Abstract
Purpose
The purpose of the present study was to describe the use of a novel hybrid surgical technique—arthroscopic-assisted plate fixation—and evaluate its clinical and anatomical outcomes in the management of large, displaced greater tuberosity (GT) fractures with comminution.
Methods
From 2009 to 2011, this novel technique was performed in 11 patients [2 men and 9 women; median age, 64 years (range 41–83 years)] with large, comminuted GT fractures, with fragment displacements of >5 mm. The preoperative mean posterior and superior migration of the fractured fragment, as measured on computed tomography (CT), was 19.5 and 5.5 mm, respectively. Two patients had shoulder fracture-dislocation, and three had associated undisplaced surgical neck fracture. The mean duration between injury and surgery was 4 days. The mean follow-up duration was 26 months.
Results
At the final follow-up, the mean postoperative ASES, UCLA and SST scores were 84, 29, and 8, respectively. The mean range of motion was as follows: forward flexion, 138°; abduction, 135°; external rotation at the side, 19°; and internal rotation, up to the L2 level. The mean posterior and superior displacements of fracture fragments on postoperative CT scan [0.7 ± 0.8 mm (range 0–2.1 mm) and 2.8 ± 0.5 mm (range 3.4–5.3 mm), respectively] were significantly improved (p < 0.05). On arthroscopy, a partial articular-side supraspinatus tendon avulsion lesion was identified in 10 of 11 patients (91 %), and 1 of these patients had a partial tear of the biceps and 1 had a partial subscapularis tear, respectively (9 %). Intraoperatively, 1 anchor pullout and 1 anchor protrusion through the humeral head were noted and corrected. Postoperatively, the loss of reduction in the fracture fragment was noted in 1 patient at 4 weeks, after corrective reduction and fixation surgery.
Conclusions
The novel arthroscopic-assisted anatomical plate fixation technique was found to be effective in reducing large-sized, displaced, comminuted GT fractures and in allowing concurrent management of intra-articular pathologies and early functional rehabilitation. Compared with the conventional plate fixation or arthroscopic suture anchor fixation technique, arthroscopic-assisted plate fixation enabled accurate restoration of the medial footprint of the GT fracture and provided an effective buttress to the large-sized GT fracture fragments.
Level of evidence
Retrospective clinical study, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Isolated fractures of the greater tuberosity (GT) account for approximately 17–21 % of all proximal humeral fractures [1, 2]. These fractures are often associated with anterior glenohumeral dislocation (5–30 %) and osteoporosis [3–5]. The goal of operative treatment is to restore the normal GT anatomy with stable fixation to allow for early functional range of motion (ROM). Several methods for GT fixation have been used, including suture fixation, cannulated screw fixation with or without a washer, percutaneous fixation, open reduction and internal fixation with plate and screws, and arthroscopic suture anchor fixation [3, 4, 6–14]. The size of the fragment, comminution of the GT fracture, and associated osteoporosis often influence the method of fracture fixation. The choice of treatment modality also depends on the patient’s age, activity level, and bone quality; fracture type and associated fractures; and surgeon’s preference. Recently, novel arthroscopic techniques and equipment designs have been developed for the arthroscopic fixation of GT fractures by using cannulated screws or suture anchors [11, 13, 15, 16]. However, the arthroscopic reduction in large, displaced comminuted GT fractures is not always satisfactory.
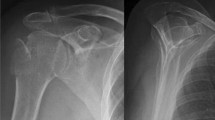
Biomechanically, the use of tension band wiring and two cancellous screws as a fixation method has been proven to provide stronger fixation for GT fractures than trans-osseous fracture fixation [17]. However, with this fixation method, it is difficult to restore the medial aspect of the GT footprint to achieve an acceptable anatomical reduction, as well as to achieve rigid fixation of the displaced large-sized GT fractures because of the strong pull of the rotator cuff muscles. When the arthroscopic suture anchor fixation technique is used, the lateral row of suture anchors can be difficult to insert into the hard cortical bone, and there is a risk that these anchor screws may be pulled out from the osteoporotic bone. Moreover, when large-sized GT fractures are comminuted, rigid fixation is difficult to achieve with an anatomical proximal humerus plate; moreover, plate fixation is associated with the risk of less reduction in fracture fragments (Fig. 1). A new hybrid technique—arthroscopic-assisted plate fixation—was introduced by the authors of the present study for the specific management of large GT fractures, especially for cases with comminution.
A 54-year-old female patient with a large, displaced, comminuted greater tuberosity fracture. a Three-dimensional computed tomography scan showing the posterosuperior displacement and comminution of the fragments. b Follow-up radiograph at 6 weeks postoperatively showing the loss of reduction in the comminuted fracture fragments. The patient was treated conservatively after fracture fragment displacement, with shoulder stiffness as a residual clinical outcome. c After 9 months, the patient underwent surgery for plate removal and arthroscopic capsular release for continued shoulder pain and stiffness. Arthroscopic examination revealed an Elman, grade 3 partial tear of the articular side of the rotator cuff, and a trans-tendon rotator cuff repair was performed
The aims of this study were to describe the use of this new surgical technique and to evaluate the clinical results of its application for the management of displaced, large-sized GT fractures with comminution. It was hypothesized that arthroscopic-assisted plate fixation would be a good alternative to achieve an accurate reduction and restoration of the medial footprint of the GT and will also provide a buttress to large fracture fragments in order to improve stability in the treatment of large, comminuted GT fractures.
Materials and methods
From 2009 to 2011, arthroscopic-assisted plate fixation was performed for displaced, large-sized comminuted GT fractures of the proximal humerus in 11 patients (Table 1). The inclusion criteria were as follows: >5 mm posterior or superior displacement of the GT fracture fragment; comminution of >2 fragments; and a fracture line extending distally up to, or beyond, the surgical neck of the humerus (Fig. 2). Patients with GT fractures meeting the inclusion criteria but with an associated anatomical fracture or surgical neck fracture, with minimal displacement, or a fracture-dislocation of the shoulder, were also included in the analysis.
All patients had sustained a direct-impact injury. Two patients had shoulder fracture-dislocation, and 3 had a non-displaced fracture of the proximal surgical neck of the humerus, combined with a large, comminuted GT fracture. The study group consisted of 2 male and 9 female patients [median age, 64 years (range 41–83 years)]. The mean duration between initial trauma and surgery was 4 days (range 2–7 days). The mean follow-up duration was 26 months (range 18–40 months). Routine preoperative shoulder radiographs included anteroposterior, axillary, lateral, and supraspinatus outlet views. For further evaluation of the fracture configuration, three-dimensional (3D) computed tomography (CT) scanning was performed. The amount of posterior and superior displacement of the fracture fragment was determined from axial and coronal CT images. The mean preoperative posterior migration of the fracture fragment in all patients was 19.5 mm (range 6.0–40.0 mm), and the mean amount of superior migration was 5.5 mm (range 3.2–10.0 mm). Preoperative measures of shoulder ROM and clinical scores from the American Shoulder and Elbow Surgeons (ASES), University of California, Los Angeles (UCLA), and Simple Shoulder Test (SST) assessments could not be obtained because of severe pain resulting from the fracture.
Each patient initially underwent arthroscopic-assisted GT fracture reduction, by using medial-row suture anchors, similar to the trans-tendon repair technique for rotator cuff tears. After this initial step, a minimally invasive surgical technique was used to buttress the fracture fragments with an anatomical proximal humerus locking plate. During the arthroscopic examination, any associated intra-articular pathologies identified were treated concurrently. All patients were regularly followed in the outpatient clinic. At 3 months postoperatively, a 2D CT scan was obtained to evaluate the accuracy of the fracture reduction and to measure the amount of residual posterior and superior displacement of the fracture fragments. It was sometimes difficult to measure the amount of residual posterior displacement on the CT scan image because of implant artefacts. At the final follow-up, clinical scores from the ASES, UCLA, and SST assessments were obtained, and passive ROM of the shoulder was measured, with a handheld goniometer, in forward flexion, abduction, and external rotation, with the shoulder in the neutral position at the side of the trunk, and internal rotation at the back (L2 level). All ROM measurements were performed by a single examiner to avoid interobserver bias.
Surgical technique
Patients were placed in the lateral decubitus position by using lateral arm traction. Intra-articular arthroscopic examination was performed through a conventional posterior portal. The articular side of the fracture in the glenohumeral joint was debrided, and reduction in the fracture was attempted by using a probe. Metal anchors (TwinFix Ti; Smith & Nephew Endoscopy, Andover, MA, USA) were inserted into the medial (i.e. intra-articular) aspect of the GT fracture. A trans-tendon repair through the rotator cuff attached to the GT fracture fragment was then performed. Similar to the trans-tendon repair technique for rotator cuff tears, threads of double-loaded suture anchors, inserted at the fracture site, were retrieved through the rotator cuff and passed through the skin by using a suture shuttle technique. Thereafter, the arthroscope was inserted into the subacromial space, and a medial-row, trans-tendon repair was performed. The arthroscope was then again inserted into the glenohumeral joint to evaluate the accuracy of the restoration of the medial footprint of the GT. Thus, the superior displacement of the fracture fragment was corrected. After completion of the arthroscopic procedure, the lateral traction was removed. Correction of the posterior migration of the severely displaced GT fracture was attempted in the last step through an open procedure, due to the difficulty of restoring posterior migration via an arthroscopic procedure. Open reduction in the posteriorly displaced GT fracture was performed by using a 5-cm deltoid-splitting approach. The suture threads of the previously inserted suture anchors were pulled anteriorly to correct the superior and posterior displacement of the fracture fragments. An anatomical proximal humerus locking plate (Zimmer Inc. Warsaw, IN, USA) was applied to buttress the fracture fragments, and rigid fixation was performed by inserting locking screws through the plate. Finally, threads from the suture anchors were tied to the available holes on the plate. On postoperative 2 day, passive ROM exercises were permitted, and active-assisted ROM exercises were advised at postoperative 4 week.
Institutional Review Board approval (Daejeon St. Mary’s Hospital, Catholic University of Korea; No. DC14RISE0011) was obtained for our retrospective study before the inclusion of patients in our review and analysis.
Statistical analysis
All statistical analyses were performed with the SPSS 20.0 software (IBM Corp., Armonk, NY, USA). The results of fracture reduction status (preoperative and postoperative fracture displacement: mm) were compared by using the Wilcoxon test. A p value of <0.05 was considered significant.
Results
At the final follow-up, all patients showed satisfactory clinical scores and shoulder ROM (Table 2). Most patients returned to daily life activities by 10 weeks postoperatively. Postoperative radiographs confirmed acceptable reduction and rigid fixation of the GT fragments (Fig. 3a). Radiological union was obtained in 10 of the 11 patients within 6–12 weeks. In 1 patient (83-year-old woman with severe osteoporosis), loss of the reduction in the GT fracture after falling down injury, without pullout of a suture anchor, developed, and revision surgery was performed. On follow-up 2D CT scan at 3 months postoperatively, maintenance of acceptable reduction in the fracture fragments was observed (Fig. 3b). The mean posterior and superior displacement of fracture fragments on postoperative CT scan was significantly improved, respectively (p < 0.05) (Table 2).
During the arthroscopic procedure, a partial articular-side supraspinatus tendon avulsion lesion was identified in 10 of the 11 patients (91 %); the lesion was repaired by using medial suture anchors and a trans-tendon repair technique. One of these patients also had an associated partial biceps tear with a thickness that was <20 % of the biceps tendon thickness (1 case), whereas another patient had a partial subscapularis tendon tear with a thickness that was <50 % of the tendon thickness (1 case).
None of the patients developed wound infection or any neurological complications. Two intraoperative complications were noted. In the first case, anchor protrusion from the humeral head developed as the medial anchor was inserted too deep, such that the tip of the metal anchor protruded from the articular surface of the humeral head. The protruding tip was removed by using an arthroscopic burr. In the second case, pull-out of the metal anchor was observed, and it was localized and removed after the arthroscopic procedure, under C-arm fluoroscopy.
Discussion
The most important finding of the present study was that for displaced large-sized, comminuted GT fractures of the proximal humerus, arthroscopic-assisted plate fixation was found to provide satisfactory anatomical reduction in the comminuted GT fracture, rigid fixation of the large-sized GT fracture, and early ROM and rehabilitation compared to open plate fixation or arthroscopic suture anchor fixation.
Owing to the increasing age of the general population, and the associated risk of osteoporosis with ageing, the incidence of GT fractures has been increasing [18]. GT fractures may be associated with partial-thickness rotator cuff tears and with labral tears. Late complications of isolated GT fractures include partial rotator cuff tears and malunions due to the traction force of the attached rotator cuff tendon, which may be a cause of persistent pain after fracture healing [19–22]. Most minimally displaced, 2-part GT fractures heal well without operative treatment. Recently, in the study of Verdano et al. [23], it was shown that posterosuperior displacement of the GT fracture fragment led to poorer surgical outcomes as compared to undisplaced fractures or fractures displaced in other directions. Several surgical techniques can be used to manage minimally displaced GT fractures, such as arthroscopic-cannulated screw fixation with washer or suture anchor fixation [7, 10]. However, it is difficult to achieve anatomical reduction and rigid fixation for large, displaced GT fractures by using cannulated screws with washer or suture anchors.
The most important factors to consider in the surgical treatment for large, displaced GT fractures are the size of the fragment, fracture comminution, and amount of fracture displacement [11, 24]. In several previous studies, the operative indication of GT fracture has been reported [25–27]. The indication for surgery for fracture displacements of >5 mm in any plane, used by the authors of the present study, is based on several anatomical, biomechanical, and clinical studies in the literature [5, 28, 29]. The direction of displacement of the tuberosity is as important to consider as the degree of displacement. Generally, a superior displacement results in subacromial impingement, whereas a posterior displacement can limit external rotation. Correction of a superior displacement is a more important factor for good clinical outcomes, as even a small amount of superior displacement can result in subacromial impingement and shoulder dysfunction, and limit abduction and external rotation [30]. In our procedure, an effective correction of superior displacement of the GT fragment was achieved by using medial-row fixation. However, correction of a large amount of the posterior displacement of the large-sized GT fragment was difficult with an arthroscopic procedure.
Large GT fractures can be stabilized with trans-osseous sutures or, occasionally, with cannulated screws or plates. A locking plate provides increased stability and thus allows for immediate postoperative rehabilitation. However, in patients with a comminuted GT fracture, there is risk of a loss of reduction with plate fixation (Fig. 1). Biomechanical studies have shown that screws should be oriented perpendicular to the fracture line. However, to resist the posteriorly directed pulling forces of the infraspinatus and the teres minor muscles on the GT fracture fragment and to reduce the fragment to its anatomical site, an anterior traction force is needed. The screw orientation of the conventional locking plate cannot resist this traction force of the infraspinatus and the teres minor muscles, which may be the cause for the common loss of reduction in comminuted GT fractures when using only the conventional plate fixation method. Arthroscopic-assisted fixation with cannulated screws and washer is also not effective in reducing a posterosuperior displacement of large-sized fracture fragments and in restoring the medial footprint of the GT. In Lin et al.’s [31] report, it was suggested that suture anchor constructs, such as the double-row suture anchor fixation, suture-bridge technique, and use of suture anchors and knotless suture anchors, would be stronger than a rigid fixation construct, such as 2 screws, to achieve rigid fixation of a GT fracture. However, an arthroscopic, double-row suture anchor fixation construct cannot rigidly and effectively fix large, comminuted GT fractures or reduce a large amount of posterior displacement of the fracture fragments. Moreover, if the fracture line extends distally up to or beyond the surgical neck, it is difficult to insert lateral row anchors in hard cortical bone. With large GT fractures, the fracture line commonly extends distally beyond the surgical neck, making it difficult to reduce and fix the fracture arthroscopically because the capsular attachment diverges from the anatomical neck and descends 1 cm or more onto the shaft of the humerus [32]. Also, if the GT fracture involves the bicipital groove anteriorly, subacromial bursal reflection prevents the arthroscopic visualization of this fragment. Because of the posterior pulling force of the infraspinatus and the teres minor, accurate arthroscopic visualization of fractures involving surgical neck and bicipital groove is difficult.
Our new hybrid technique has several advantages. The arthroscopic anchor fixation method can effectively restore the medial footprint of the GT and, for comminuted GT fractures, the threads of the suture anchors can decrease the risk of pull-out of the comminuted fragments, which would result in a loss of fracture reduction [8, 33]. In combination with the arthroscopic medial-row repair, open plate fixation was used to provide rigid fixation and lateral buttress for large fragments of the GT fracture. This hybrid method allowed rapid rehabilitation owing to the rigid fixation. Arthroscopic suture anchor fixation provides stable fixation only for minimally displaced comminuted GT fractures [11]. However, if the GT fragments are too large, comminuted, or markedly displaced, it is extremely difficult to achieve an accurate reduction and stable fixation by using the arthroscopic technique alone.
Our study has several limitations. First, this is a retrospective study, and hence, has all the inherent limitations of this research design. There was no control group to permit head-to-head comparison with other surgical techniques. Moreover, the outcomes of only 11 patients were included. Prospective, randomized controlled trials, with inclusion of a sufficient number of patients for statistical power, are needed to validate the clinical effectiveness of our technique. The currently available locking plates are too large to manage GT fractures that may have large fragments but that extend only to the surgical neck area. There is a need for the development of a low-profile short-length plate specifically designed for the reduction in large-sized GT fractures. For example, in Schoffl et al.’s [34] report, the use of the “Bamberg” plate for isolated GT fractures was described. However, this new hybrid GT fixation technique could be a good alternative for the treatment of large, comminuted GT fractures that are difficult to manage with the conventional plate fixation or arthroscopic suture anchor fixation technique.
Conclusions
A new hybrid technique—arthroscopic-assisted plate fixation—is effective in achieving anatomical reduction and rigid fixation of large, displaced, comminuted GT fractures, and can ultimately help in achieving satisfactory clinical outcomes and early rehabilitation, with an early return to the activities of daily living.
References
Bahrs C, Lingenfelter E, Fischer F, Walters EM, Schnabel M (2006) Mechanism of injury and morphology of the greater tuberosity fracture. J Shoulder Elbow Surg 15:140–147
Kim E, Shin HK, Kim CH (2005) Characteristics of an isolated greater tuberosity fracture of the humerus. J Orthop Sci 10:441–444
Bhatia DN, van Rooyen KS, du Toit DF, de Beer JF (2006) Surgical treatment of comminuted, displaced fractures of the greater tuberosity of the proximal humerus: a new technique of double-row suture-anchor fixation and long-term results. Injury 37:946–952
Bigliani LU, Flatow EL, Pollock R (1998) Fractures of the proximal humerus. In: Rackwood CA, Matsen FA (eds) The shoulder. WB Saunders, Philadelphia, pp 337–389
Green A, Izzi J Jr (2003) Isolated fractures of the greater tuberosity of the proximal humerus. J Shoulder Elbow Surg 12:641–649
Gartsman GM (2003) Calcific tendinitis. In: Gartsman G (ed) Shoulder arthroscopy. Elsevier Science, Philadelphia, pp 271–275
Bonsell S, Buford DA Jr (2003) Arthroscopic reduction and internal fixation of a greater tuberosity fracture of the shoulder: a case report. J Shoulder Elbow Surg 12:397–400
Flatow EL, Cuomo F, Maday MG, Miller SR, McIlveen SJ, Bigliani LU (1991) Open reduction and internal fixation of two-part displaced fractures of the greater tuberosity of the proximal part of the humerus. J Bone Joint Surg Am 73:1213–1218
Gartsman GM, Taverna E, Hammerman SM (1999) Arthroscopic treatment of acute traumatic anterior glenohumeral dislocation and greater tuberosity fracture. Arthroscopy 15:648–650
Herscovici D Jr, Saunders DT, Johnson MP, Sanders R, DiPasquale T (2000) Percutaneous fixation of proximal humeral fractures. Clin Orthop Relat Res 375:97–104
Ji JH, Shafi M, Song IS, Kim YY, McFarland EG, Moon CY (2010) Arthroscopic fixation technique for comminuted, displaced greater tuberosity fracture. Arthroscopy 26:600–609
Kim KC, Rhee KJ, Shin HD (2010) Arthroscopic treatment of symptomatic malunion of the greater tuberosity of the humerus using the suture-bridge technique. Orthopedics 33:242–245
Song HS, Williams GR Jr (2008) Arthroscopic reduction and fixation with suture-bridge technique for displaced or comminuted greater tuberosity fractures. Arthroscopy 24:956–960
Taverna E, Sansone V, Battistella F (2004) Arthroscopic treatment for greater tuberosity fractures: rationale and surgical technique. Arthroscopy 20:e53–e57
Ji JH, Kim WY, Ra KH (2007) Arthroscopic double-row suture anchor fixation of minimally displaced greater tuberosity fractures. Arthroscopy 23:1133.e1-4
Kim KC, Rhee KJ, Shin HD, Kim YM (2008) Arthroscopic fixation for displaced greater tuberosity fracture using the suture-bridge technique. Arthroscopy 24:120
Braunstein V, Wiedemann E, Plitz W, Muensterer OJ, Mutschler W, Hinterwimmer S (2007) Operative treatment of greater tuberosity fractures of the humerus—a biomechanical analysis. Clin Biomech 2:652–657
Cadossi M, Mazzotti A, Capra C, Persiani V, Luciani D, Pungetti C (2013) Proximal humeral fractures in elderly patients. Aging Clin Exp Res 25(Suppl 1):S85–S87
Calvo E, Merino-Gutierrez I, Lagunes I (2010) Arthroscopic tuberoplasty for subacromial impingement secondary to proximal humeral malunion. Knee Surg Sports Traumatol Arthrosc 18:988–991
Hinov V, Wilson F, Adams G (2002) Arthroscopically treated proximal humeral fracture malunion. Arthroscopy 18:1020–1023
Ladermann A, Denard PJ, Burkhart SS (2012) Arthroscopic management of proximal humerus malunion with tuberoplasty and rotator cuff retensioning. Arthroscopy 28:1220–1229
Martinez AA, Calvo A, Domingo J, Cuenca J, Herrera A (2010) Arthroscopic treatment for malunions of the proximal humeral greater tuberosity. Int Orthop 34:1207–1211
Verdano MA, Aliani D, Pellegrini A, Baudi P, Pedrazzi G, Ceccarelli F (2013) Isolated fractures of the greater tuberosity in proximal humerus: does the direction of displacement influence functional outcome? An analysis of displacement in greater tuberosity fractures. Acta Biomed 84:219–228
Yin B, Moen TC, Thompson SA, Bigliani LU, Ahmad CS, Levine WN (2012) Operative treatment of isolated greater tuberosity fractures: retrospective review of clinical and functional outcomes. Orthopedics 35:e807–e814
Bigliani LU, Flatow EL, Pollock R (1998) Fractures of the proximal humerus. In: Rockwood C, MatBen F (eds) The shoulder. WB Saunders, Philadelphia, pp 337–389
Neer CS 2nd (1970) Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 52:1077–1089
Park TS, Choi IY, Kim YH, Park MR, Shon JH, Kim SI (1997) A new suggestion for the treatment of minimally displaced fractures of the greater tuberosity of the proximal humerus. Bull Hosp Jt Dis 56:171–176
Bono CM, Renard R, Levine RG, Levy AS (2001) Effect of displacement of fractures of the greater tuberosity on the mechanics of the shoulder. J Bone Joint Surg Br 83:1056–1062
Iannotti JP, Gabriel JP, Schneck SL, Evans BG, Misra S (1992) The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. J Bone Joint Surg Am 74:491–500
Park MC, Murthi AM, Roth NS, Blaine TA, Levine WN, Bigliani LU (2003) Two-part and three-part fractures of the proximal humerus treated with suture fixation. J Orthop Trauma 17:319–325
Lin CL, Hong CK, Jou IM, Lin CJ, Su FC, Su WR (2012) Suture anchor versus screw fixation for greater tuberosity fractures of the humerus—a biomechanical study. J Orthop Res 30:423–428
Johnson D (2008) Pectoral girdle and upper limb. In: Standring S, Borley NR, Gray H (eds) Gray’s anatomy: the anatomical basis of clinical practice. Churchill Livingston/Elsevier, Philadelphia, pp 796–806
Zuckerman JD, Checroun AJ (1999) Fractures of the proximal humerus: diagnosis and management. In: Iannotti JP, Williams GR (eds) Disorders of the shoulder: diagnosis and management. Lippincott, Philadelphia, pp 639–685
Schoffl V, Popp D, Strecker W (2011) A simple and effective implant for displaced fractures of the greater tuberosity: the “Bamberg” plate. Arch Orthop Trauma Surg 131:509–512
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No author or related institute has received any financial benefit from research in this study. The authors report no conflict of interest. Institutional Review Board: approved by Daejeon St. Mary’s Hospital (DC14RISE0011).
Rights and permissions
About this article
Cite this article
Park, SE., Jeong, JJ., Panchal, K. et al. Arthroscopic-assisted plate fixation for displaced large-sized comminuted greater tuberosity fractures of proximal humerus: a novel surgical technique. Knee Surg Sports Traumatol Arthrosc 24, 3892–3898 (2016). https://doi.org/10.1007/s00167-015-3805-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3805-3