Abstract
Purpose
The aim of this study was to demonstrate the lower limb alignment in knee flexion position after navigation-assisted total knee arthroplasty using the gap technique and to identify the correlative factors.
Methods
One hundred and twenty consecutive osteoarthritic knees (120 patients) were prospectively enrolled for intraoperative data collection. All TKA surgeries were performed using the navigation system (OrthoPilot™, version 4.0; B. Braun Aesculap, Tuttlingen, Germany). Before and after final prosthesis implantation, the lower limb navigation alignment in both knee extension (0°) and knee flexion (90°) position was recorded. The knee flexion alignment was divided into three groups: varus, neutral and valgus alignment. To determine the factors of the alignment in knee flexion position, preoperative demographics, radiologic and intraoperative data were obtained. Pearson’s correlation (r) analysis was performed to find the correlation. The Knee Society Score and Western Ontario and McMaster Universities Osteoarthritis Index were compared between groups.
Results
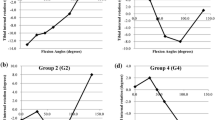
Although all postoperative extension alignment was within neutral position (between −2° and +2°), postoperative knee flexion alignment was divided into three groups: varus (≤−3°), 24 cases (20 %); neutral (between −2° and +2°), 85 cases (70.8 %) and valgus (≥+3°) alignment, 11 cases (9.2 %). There were a good correlation of alignment in knee flexion position with the rotation of femoral component relative to posterior condylar axis (r = −0.502, p = 0.000) and weak correlations with posterior femoral cut thickness (lateral condyle) (r = 0.207, p = 0.026), medial flexion (90°) gap after femoral component rotation adjustment (r = 0.276, p = 0.003). Other variables did not show correlations. There were no statistical clinical differences between varus, neutral and valgus knee flexion alignment groups.
Conclusion
About 30 % of the cases showed malalignment of more than 3° in knee flexion position although with neutral alignment in extension position. The knee flexion alignment had a good correlation with the rotation of femoral component relative to posterior condylar axis. Neutral alignment in knee flexion position may be adjusted by femoral component rotation especially by the use of navigation system.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Successful outcome of total knee arthroplasty (TKA) is dependent on the accurate implant position, restoration of limb alignment and optimal ligament balancing [5, 15, 18, 34]. A balanced extension gap is achieved by releasing structures on the tight side of the knee joint. In order to balance the knee flexion gap (90°), appropriate femoral component rotation is critical to ensure that soft tissue tension is equal between the medial and lateral compartments. Although the lower limb alignment in extension position (standing) is aimed to neutral position, the ideal lower limb alignment during knee flexion position (90°) is not known.
Femoral component rotation is an important factor that affects outcome in TKA. Multiple studies have shown that improper rotation of the femoral component can lead to patellofemoral pain, increased component wear and poor functional outcomes [27, 35]. Traditionally, four methods have been available to guide the femoral component rotation during implantation: matching rotation to the transepicondylar axis (TEA) [7], the posterior condylar axis (PCA) [20], the anteroposterior (AP) axis [32] or balancing the medial and lateral flexion gaps [15]. However, optimal femoral component rotation is achieved in only about 75 % of cases and remains a difficult challenge despite the evolution of computer-assisted navigation TKAs [12, 19, 23, 29].
The rotational relationships between the three axis (TEA, PCA and AP axis) have been studied extensively in the literature utilizing cadavers [19], intraoperative measurements [13], conventional radiography [3], computed tomography (CT) [1] and computer-assisted navigation systems [25]. However, these studies demonstrated that there was significant variability in not only the relationships of these references to one another, but also the ability to accurately identify them anatomically [36]. Rather than confining the description of knee movement to three anatomical axes, the functional flexion axis (FFA; also referred to as the helical axis) has been used to describe the instantaneous axis of primary rotation of the knee in gait studies [16] and more recently in knee arthroplasty surgical navigation studies [9, 10]. The FFA is a kinematically acquired reference related to the specific kinematics of the patient, as opposed to the conventional TKA technique, which relies on anatomical landmarks. The FFA and the TEA are reported to be coincident by some studies [4, 8, 24]. However, there are also recent studies showing these two axes to be non-coincident and non-parallel, with a mean difference of 2.9° [28]. They attributed that the difference could be from the use of TEA in other studies rather than the surgical TEA.
The aim of this study focused on two parts. First was to demonstrate the lower limb alignment in knee flexion position after navigation-assisted TKA using the gap technique. Second was to identify the correlative factors which determined the lower limb alignment in knee flexion position. Since the femoral component rotation position is determined by equalized medial and lateral gap balancing, the hypothesis was that the lower limb alignment in knee flexion position would correlate with the relative femoral component rotation position from either TEA and/or PCA. If so, then the alignment in knee flexion position may be predicted by the femoral component rotation.
Materials and methods
One hundred and twenty consecutive osteoarthritic knees (120 patients) were prospectively enrolled for intraoperative data collection between May 2012 and March 2014. The inclusion criteria were primary osteoarthritic varus knees with substantial pain and loss of function. The exclusion criteria were patients with valgus knees, rheumatoid arthritis, post-traumatic osteoarthritis, previous knee joint surgeries or infection, and revisional total knee arthroplasties. The demographic and knee deformities as well as the preoperative knee function characteristics are summarized in Table 1.
Surgical technique using navigation system
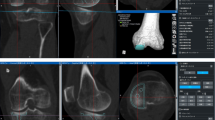
All TKA surgeries were performed by single surgeon (JHY) using the navigation system (OrthoPilot™, version 4.0; B. Braun Aesculap, Tuttlingen, Germany). All patients were implanted with full cemented type ultra-congruent fixed-bearing design (Columbus™ UC, B. Braun Aesculap, Tuttlingen, Germany). None of the patients underwent patellar resurfacing.
All 120 varus knees underwent the similar surgical approach consisting of a midline skin incision and a medial parapatellar approach under an air tourniquet at 250 mmHg. After registering the kinematic and the required anatomical selected points, the lower extremity alignment by navigation in knee extension (0°) and knee flexion (90°) position was recorded.
The osteophytes, anterior, posterior cruciate ligaments and medial meniscus were removed. A tibial cut was made perpendicular to the long axis of tibia using a cutting block positioned under navigation guidance. The offset-type force-controlled spreader system (B. Braun Aesculap, Tuttlingen, Germany) was inserted to the tibiofemoral gap at full extension position to identify the overall mechanical alignment [37]. The distraction force of the spreader system was set at 150 N. This amount of force was chosen on the basis of previous study regarding intraoperative gap measurements during surgery [22, 33]. If the alignment was not within 2° from neutral axis, further medial soft tissue release was done accordingly. Once the alignment was within 2° from neutral axis, the mediolateral gaps (in millimetres) at full extension (0°) and at 90° of knee flexion were measured with patella reduced position [37]. In previous studies assessing the intraoperative gap measurements during TKA, a difference of 2 or 3 mm in the measurements has been regarded as being clinically relevant [21, 22]. Therefore, further surgical steps were carried out after achieving the gap difference of <3 mm. To balance the discrepancies between medial and lateral gaps at 90° of knee flexion, femoral rotation was adjusted to equalize flexion gaps. However, if the femoral component rotation was beyond 0°–6°, that is <−1° or more than 7°, from the PCA, further release of the soft tissues were not performed [26]. After final prosthesis implantation, the lower extremity navigation alignment in both knee extension (0°) and knee flexion (90°) position was recorded.
Since this navigation system provides the data from registered point of posterior femoral condyles, the relative femoral component rotation position is provided from the PCA. The femoral component rotational data and the level of posterior femoral cuts were recorded. The coronal and sagittal alignment of the tibial component was also recorded.
Clinical and radiologic evaluation
Symptom severity was assessed at preoperative and at latest follow-up using the Knee Society Score (KSS) [15] and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score [6]. Passive maximum knee range of motion (ROM) was measured using a goniometer. At these evaluations, assessments were performed by a physician assistant not directly involved in the surgical procedures. The WOMAC system involves the completion of a 24-item questionnaire with three sections, namely pain, stiffness and function [6]. Five response options are possible (none, mild, moderate, severe and extreme), which are scored from 0 to 4 to yield subtotal scores for pain (5 items; possible total score range 0–20), stiffness (2 items; possible score range 0–8) and function (17 items; possible score range 0–68).
The standing anteroposterior, lateral, Merchant’s views of the patellofemoral joint were taken pre- and postoperatively. Mechanical limb alignment was checked using a standing radiograph of the entire lower extremity. To analyse the femoral component rotation from clinical epicondylar axis (CEA), postoperative radiographs were taken according to Kanekasu’s technique (femur axial view) (Fig. 1) [17]. Patients sat on the wooden table with their lower legs in hanging position. Knees were flexed at an angle of 90° in neutral and relaxed position. The central ray was aimed in an upward angle of 15° at a distance of 1 m from X-ray tube to film cassette. The angle between the CEA and the PCA (of prosthesis) was measured for femoral component rotational position. Radiographs were stored into PACS (Picture Archiving Communications System, Maroview®, Marotch, Seoul, Korea) in the format of DICOM (digital imaging and communications in medicine) files. Angular measurements were taken using protractor function in Maroview® PACS. All radiologic measurements were taken by two physicians: one orthopaedic surgeon specialized in knee surgery blinded to the study and a senior orthopaedic resident. Measurements were taken at two separate times 2 weeks apart. Average of three measurements at each session was recorded to reduce the random errors. The study protocol was approved by the Institutional Review Board of Veterans Health Service Medical Center, Seoul, Korea (VHS 2012-35), and all included patients provided written informed consent.
Statistical analysis
The study numbers were sufficient to satisfy the power calculation. The sample size was calculated to detect a significance of correlative factors with power of 80 % with an α value of 0.05. The arithmetic mean, standard deviation and the distribution of values were determined for each radiologic and intraoperative data. The post-implantation alignment in knee flexion position was divided into three groups: varus (≤−3°), neutral (between −2° and +2°) and valgus (≥+3°) alignment (Table 2).
To determine the predictive factor of the alignment in knee flexion position, preoperative demographics, radiologic data [pre- and postoperative coronal alignment including prosthesis position, angle between CEA and PCA (of prosthesis)] and intraoperative data (preoperative navigation knee flexion alignment, femoral component rotation, posterior femoral cut thickness, gaps of initial measurements and after femoral component adjustment, tibia coronal and sagittal alignment) were analysed. Pearson’s correlation analysis was performed to find the correlation between the lower extremity navigation alignment in knee flexion (90°) position and each measurement. The gap difference between medial and lateral compartment in knee flexion position after femoral component adjustment was also analysed with the alignment in knee flexion position. Correlation coefficient (r) ranges from −1 (negative correlation) to +1 (positive correlation). If p < 0.05 and 0.1 < |r| < 0.4, there is a weak positive correlation between the two variables; if 0.4 < |r| < 0.7, there is good positive correlation; and if 0.7 < |r| < 1, there is strong positive correlation.
The reliability of each radiologic measurement was assessed using the intraclass correlation coefficient, which quantifies what proportion of the difference is due to measurement variability. The intraclass correlation coefficient can assume any value from 0 to 1, where >0.80 represents good agreement, between 0.60 and 0.79 represents moderate agreement, and <0.59 represents poor agreement. All radiologic measurements in this study showed good reliability (all values >0.9). The Statistical Package for Social Science, version 10.1 (SPSS Inc., Chicago, IL, USA) was used, and p value <0.05 was considered statistically significant.
Results
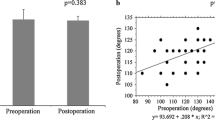
All patients were managed to be followed up (mean 25 ± 8 months). The mean preoperative KSS knee score improved from 50 ± 6 to 93 ± 4 at latest follow-up. The mean preoperative KSS functional score improved from 46 ± 10 to 93 ± 3 at latest follow-up. The mean preoperative total WOMAC score improved from 68 ± 5 to 16 ± 4 at latest follow-up. The mean preoperative mechanical axis was −6.4° ± 3.6°. All knees were in varus alignment preoperatively. The mean postoperative mechanical axis was improved to a value of 0.2° ± 1.3°. There were no other minor or major complications directly related to TKA.
Although all postoperative navigation mechanical alignment was within neutral position (between −2° and +2°) in 0° of knee flexion, postoperative 90° flexion alignment was divided into three groups: varus (≤−3°), neutral (between −2° and +2°) and valgus (≥+3°) alignment. Eighty-five cases (70.8 %) were in neutral knee flexion alignment. However, the conventional knee scoring system (KSS, WOMAC) did not show statistical difference between these varus, neutral and valgus groups (Table 2).
The intraoperative data obtained by the navigation system are demonstrated in Table 3 . The mean coronal and sagittal alignment for tibia component was 0° ± 1° and 1° ± 1°, respectively. The intraoperative gap measurements of each medial and lateral compartment in knee extension and flexion positions are demonstrated in Table 4 (before and after femoral component adjustment). All gaps were maintained in rectangular gaps both in extension and knee flexion position (<3 mm difference) after femoral component adjustment. However, each gap measurement had no correlation with the alignment in knee flexion position (−0.1 < r < 0.1).
The navigation system used in this study provides the relative femoral component rotation according to the PCA. The mean femoral component rotation from the PCA was 3° ± 2°. Additionally, to measure the femoral component rotational position from CEA, femur axial view was taken postoperatively. The mean angle of femoral component rotation (PCA of prosthesis) relative to CEA was −2° ± 2°.
The radiologic and intraoperative data with the correlation coefficient values are demonstrated in Table 3. The alignment in knee flexion position had a good correlation with the rotation of femoral component (relative angle to PCA) and weak correlations with posterior femoral cut thickness (lateral condyle) and medial flexion (90°) gap after femoral component rotation adjustment (p < 0.05). There was no correlation with the CEA (r = −0.052, n.s.). No correlations were observed with the preoperative demographic parameters such as height, weight and body mass index (−0.1 < r < 0.1). Other variables did not show correlations. Using the rotation of femoral component from PCA which was the good correlative, regression analysis was performed to figure out the best fit equation to predict the knee flexion alignment. The formula was as follows: (knee flexion alignment = −2 × femoral component rotation from PCA + 4.8).
Discussion
The important finding of this study was that there were variable ranges of lower limb alignment (varus, neutral and valgus) in knee flexion position although acceptable knee extension alignment was achieved. Another finding was that out of demographic, radiologic and intraoperative parameters, knee flexion alignment had a good correlation with the femoral component rotational position relative to the PCA.
There were variable ranges of lower limb alignment in knee flexion position. While 85 cases (70.8 %) were in neutral knee flexion alignment, there were 24 cases (20 %) with varus (≤−3°) alignment and 11 cases (9.2 %) with valgus alignment. Although conventional clinical evaluation system (KSS, WOMAC) has failed to demonstrate the significance of these findings, patients with valgus alignment in knee flexion position may have difficulty in cross-leg position and/or figure-4 position, which is important in Asian lifestyle. Other meticulous clinical evaluation system may be needed in future studies.
From the demographic, radiologic and intraoperative parameters, there was a good negative correlation of alignment in knee flexion position with the rotation of femoral component (relative angle to PCA). The best fit formula was as follows: (knee flexion alignment = −2 × femoral component rotation from PCA + 4.8). Since the femoral component rotation relative to the PCA can be identified during the femoral adjustment stage in navigation-assisted gap balancing before the femoral bone chamber cutting, the final knee flexion alignment may be anticipated using this formula.
Axial rotation of the femoral component is crucial for obtaining well-balanced flexion gaps and tibiofemoral and patellofemoral congruency through flexion [35]. However, the ideal referencing choice to determine the femoral component rotation in TKA has not been definitively determined. No single referencing technique has been shown to be superior to another [30, 31]. The disadvantage of bone referencing of femoral rotation is that the capsuloligamentous situation is not taken into account and the flexion gap symmetry has to be achieved by soft tissue balancing alone. Meanwhile, the disadvantage of the tibia-first technique, where the femoral component is adjusted according to the flexion gap, may have a malpositioned femoral component. Throughout the surgery in this study, the femoral component rotation to balance the flexion gap was dependent on the soft tissue releases that were performed, resulting in a variable relationship between the PCA and the amount of rotation necessary to appropriately balance the knee. The mean femoral component rotation from the PCA was 2.7° ± 1.8°.
Berger et al. [7] have proposed two transepicondylar axes: the surgical epicondylar axis, which is a line connecting the lateral epicondylar prominence and the medial sulcus of the medial epicondyle, and the CEA, which is a line connecting the lateral epicondylar prominence and the most prominent point of the medial epicondyle. Yoshino et al. [38] demonstrated that the CEA was more reproducible than the surgical one. In order to identify the relative femoral component rotation from CEA, femur axial view was taken postoperatively [17]. The mean angle of femoral component rotation relative to CEA was −1.8° ± 1.9°. However, this relative position had no correlation with the knee flexion alignment (r = −0.052, n.s.). Although the femoral component was situated in rather internal rotation from CEA, none of the patients demonstrated problem in patella tracking position. One possible explanation could be from bias of evaluation by difference methods. The CEA was measured from the postoperative radiographs, while other parameters were from navigation data.
Normal knee kinematics can be expressed simply as three fixed axes (flexion–extension, axial rotation and abduction–adduction). In this model of knee kinematics, the flexion motion of the tibia and femur relative to one another occurs around the functional flexion axis [8]. The FFA is a strictly kinematic measure and is not determined by anatomical landmarks, but the relationship of such landmarks to the FFA is of great interest in TKA [9]. The problem of defining the flexion axis of the knee and relating it to the anatomy has led to differing results reported in the literature. Churchill et al. [8] suggested that matching the femoral rotation to the TEA most closely matched the mean flexion axis of the knee in 15 cadaveric specimens. Hollister et al. [14] claimed that the flexion axis found by their ‘‘axis finder’’ passes through the posterior femoral condyles at the attachment of the medial and lateral collateral ligaments. In contrary, Eckhoff et al. [11] define the cylindrical axis as the FFA and demonstrate that the TEA is not truly an approximation to the cylindrical axis. There are yet no clear studies regarding the issue between the ideal flexion axis and the knee flexion alignment. From this study, 85/120 cases (70.8 %) were in neutral knee flexion alignment, while 24/120 cases (20 %) were varus (≤−3°) alignment and 11/120 cases (9.2 %) were valgus alignment even after using the navigation-assisted strict gap-balancing technique. By the correlation analysis, the femoral component rotation for the PCA had a good correlation while other parameters showed either weak or no correlation. These results may also mean that there are no single anatomical or other parameters which can determine the knee flexion alignment. Further studies are required whether the flexion axis or the ideal knee flexion alignment should be “patient specific”.
Limitations of this study should be noted. First, this is rather short-term follow-up study. Clinical significance regarding the alignment in knee flexion position may need longer follow-up period. Second, preoperative valgus knees were not included. As suggested by Akagi et al. [2], in valgus knees, hypoplasia of the lateral femoral condyle exists and modifies the femoral rotation throughout the ROM. For valgus knees, the correlative factors for knee flexion alignment may be different. Third, radiographic measurements and navigation data were used to correlate with the alignment in knee flexion position. There might have been a bias since different methods were used.
Conclusion
There were variable ranges of lower limb alignment (varus, neutral and valgus) in knee flexion position although acceptable knee extension alignment was achieved using the navigation-assisted gap-balancing technique. Out of demographic, radiologic and intraoperative parameters, knee flexion alignment had a good correlation with the femoral component rotational position relative to the PCA. Neutral alignment in knee flexion position may be adjusted by femoral component rotation especially by the use of navigation system.
References
Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, Nakamura T (1999) Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res 366:155–163
Akagi M, Yamashita E, Nakagawa T, Asano T, Nakamura T (2001) Relationship between frontal knee alignment and reference axes in the distal femur. Clin Orthop Relat Res 388:147–156
Arima J, Whiteside LA, McCarthy DS, White SE (1995) Femoral rotational alignment, based on the anteroposterior axis, in total knee arthroplasty in a valgus knee. A technical note. J Bone Joint Surg Am 77:1331–1334
Asano T, Akagi M, Nakamura T (2005) The functional flexion-extension axis of the knee corresponds to the surgical epicondylar axis: in vivo analysis using a biplanar image-matching technique. J Arthroplasty 20:1060–1067
Bae DK, Song SJ, Heo DB, Tak DH (2013) Does the severity of preoperative varus deformity influence postoperative alignment in both conventional and computer-assisted total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 21:2248–2254
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15:1833–1840
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47
Churchill DL, Incavo SJ, Johnson CC, Beynnon BD (1998) The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res 356:111–118
Colle F, Bignozzi S, Lopomo N, Zaffagnini S, Sun L, Marcacci M (2012) Knee functional flexion axis in osteoarthritic patients: comparison in vivo with transepicondylar axis using a navigation system. Knee Surg Sports Traumatol Arthrosc 20:552–558
Colle F, Lopomo N, Bruni D, Visani A, Iacono F, Zaffagnini S, Marcacci M (2014) Analysis of knee functional flexion axis in navigated TKA: identification and repeatability before and after implant positioning. Knee Surg Sports Traumatol Arthrosc 22:694–702
Eckhoff DG, Bach JM, Spitzer VM, Reinig KD, Bagur MM, Baldini TH, Flannery NM (2005) Three-dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg Am 87(Suppl 2):71–80
Garvin KL, Barrera A, Mahoney CR, Hartman CW, Haider H (2013) Total knee arthroplasty with a computer-navigated saw: a pilot study. Clin Orthop Relat Res 471:155–161
Griffin FM, Insall JN, Scuderi GR (1998) The posterior condylar angle in osteoarthritic knees. J Arthroplasty 13:812–815
Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG (1993) The axes of rotation of the knee. Clin Orthop Relat Res 290:259–268
Insall JN, Binazzi R, Soudry M, Mestriner LA (1985) Total knee arthroplasty. Clin Orthop Relat Res 192:13–22
Johnson TS, Andriacchi TP, Erdman AG (2004) Sensitivity of finite helical axis parameters to temporally varying realistic motion utilizing an idealized knee model. Proc Inst Mech Eng H 218:89–100
Kanekasu K, Kondo M, Kadoya Y (2005) Axial radiography of the distal femur to assess rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 434:193–197
Kang CH, Lee KJ, Bae KC, Cho CH, Lee SW, Shin HK, Lee YK, Bae JS (2012) Results of total knee arthroplasty with NexGen LPS-flex implant using navigation system (brain lab): results with a 5-year follow-up. Knee Surg Relat Res 24:208–213
Kinzel V, Ledger M, Shakespeare D (2005) Can the epicondylar axis be defined accurately in total knee arthroplasty? Knee 12:293–296
Laskin RS (1995) Flexion space configuration in total knee arthroplasty. J Arthroplasty 10:657–660
Matsumoto T, Kuroda R, Kubo S, Muratsu H, Mizuno K, Kurosaka M (2009) The intra-operative joint gap in cruciate-retaining compared with posterior-stabilised total knee replacement. J Bone Joint Surg Br 91:475–480
Matsumoto T, Muratsu H, Tsumura N, Mizuno K, Kuroda R, Yoshiya S, Kurosaka M (2006) Joint gap kinematics in posterior-stabilized total knee arthroplasty measured by a new tensor with the navigation system. J Biomech Eng 128:867–871
Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C (2007) A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am 89:236–243
Matziolis G, Pfiel S, Wassilew G, Boenicke H, Perka C (2011) Kinematic analysis of the flexion axis for correct femoral component placement. Knee Surg Sports Traumatol Arthrosc 19:1504–1509
Moon YW, Seo JG, Lim SJ, Yang JH (2010) Variability in femoral component rotation reference axes measured during navigation-assisted total knee arthroplasty using gap technique. J Arthroplasty 25:238–243
Moon YW, Seo JG, Yang JH, Shon MS (2008) Analysis of the patellofemoral congruence angle according to the rotational alignment of the femoral component in navigation-guided TKA. Orthopedics 31:62–67
Moyad TF, Hughes RE, Urquhart A (2011) “Grand piano sign,” a marker for proper femoral component rotation during total knee arthroplasty. Am J Orthop 40:348–352
Oussedik S, Scholes C, Ferguson D, Roe J, Parker D (2012) Is femoral component rotation in a TKA reliably guided by the functional flexion axis? Clin Orthop Relat Res 470:3227–3232
Schlatterer B, Linares JM, Chabrand P, Sprauel JM, Argenson JN (2014) Influence of the optical system and anatomic points on computer-assisted total knee arthroplasty. Orthop Traumatol Surg Res 100:395–402
Siston RA, Cromie MJ, Gold GE, Goodman SB, Delp SL, Maloney WJ, Giori NJ (2008) Averaging different alignment axes improves femoral rotational alignment in computer-navigated total knee arthroplasty. J Bone Joint Surg Am 90:2098–2104
Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ (2005) The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am 87:2276–2280
Suter T, Zanetti M, Schmid M, Romero J (2006) Reproducibility of measurement of femoral component rotation after total knee arthroplasty using computer tomography. J Arthroplasty 21:744–748
Tanaka K, Muratsu H, Mizuno K, Kuroda R, Yoshiya S, Kurosaka M (2007) Soft tissue balance measurement in anterior cruciate ligament-resected knee joint: cadaveric study as a model for cruciate-retaining total knee arthroplasty. J Orthop Sci 12:149–153
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 21:2325–2330
Verlinden C, Uvin P, Labey L, Luyckx JP, Bellemans J, Vandenneucker H (2010) The influence of malrotation of the femoral component in total knee replacement on the mechanics of patellofemoral contact during gait: an in vitro biomechanical study. J Bone Joint Surg Br 92:737–742
Wai Hung CL, Wai Pan Y, Kwong Yuen C, Hon Bong L, Lei Sha LW, Ho Man SW (2009) Interobserver and intraobserver error in distal femur transepicondylar axis measurement with computed tomography. J Arthroplasty 24:96–100
Yoon J-R, Oh K-J, Wang JH, Yang J-H (2014) Does patella position influence ligament balancing in total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-2879-7
Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y (2001) Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty 16:493–497
Acknowledgments
The authors would like to thank Ms. Min-Jung Lee for statistical analysis, Ms. Kyoung-Jong Bong and Mr. Ho-Woo Kim for data collection of this manuscript.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, JH., Dahuja, A., Kim, JK. et al. Alignment in knee flexion position during navigation-assisted total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24, 2422–2429 (2016). https://doi.org/10.1007/s00167-015-3589-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3589-5