Abstract
Purpose
The range of motion of the knee is a critical element of clinical assessment. The tested hypothesis was that the measurement of the knee flexion angle measured with two specific smartphone applications using either inclinometer or camera technology was different from the reference measurement with a navigation system designed for total knee arthroplasty (TKA).
Methods
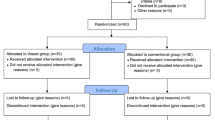
Ten consecutive patients were selected for navigation-assisted TKA. Five navigated, five inclinometer and five camera measurements of knee flexion angle were obtained for each patient throughout the complete range of motion. The difference, the correlation and the coherence between all measurements and all paired sub-groups were analysed.
Results
There was a strong correlation and a good coherence between the three techniques of measurements, but the knee flexion angle reported by the inclinometer differed substantially from the camera- and navigation-based measurements. The camera-based measurement was clinically identical to the navigated data, with a mean difference of <1° and only 1/50 difference >3°.
Conclusion
Camera-based smartphone measurement of the knee range of motion is fit for purpose in a routine clinical setting. The accuracy may be higher than other conventional measurement techniques, allowing a more precise rating of the clinical outcomes after TKA.
Level of evidence
II.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is a successful treatment for end-stage osteoarthritis. One of the major goals of this procedure is to restore an adequate range of motion. Therefore, measurement of range of motion is clinically relevant and an important element or item of most clinical knee scoring systems [8, 10].
Smartphone technology may currently be used in many ways, but its use in the medical field is not yet widespread. An inclinometer application has been shown to be an accurate and precise tool to measure the knee flexion angle [12], with virtually no additional cost when compared to more sophisticated techniques such as gait analysis [6, 17] or image analysis [3, 9]. Another possible smartphone technology is based on photographic analysis [7]. No comparative analysis between these two techniques has been previously performed. The goal of the present study was to compare these two technologies to the navigated measurement considered as the gold standard, suggesting to use the more precise one.
The basic hypothesis of this study was that measurements of the knee flexion angle taken with the inclinometer and camera applications on a smartphone would differ from each other and from the reference measurement with a navigation system designed for TKA.
Materials and methods
The study was approved by the institutional review committee of the University Hospital Strasbourg, and respects the ethical standards in the Helsinki Declaration of 1975, as revised in 2000. Ten consecutive patients with end-stage osteoarthritis were selected for navigation-assisted TKA and included in the present study after giving their informed consent. The following pre-operative items were recorded: age, gender, body mass index (BMI), knee assessment by the Knee Society Score (KSS) [10], severity of the degenerative changes according to Ahlback [1] and mechanical femoro-tibial angle measured on full leg radiographs with unipodal support (varus angles were considered as positive and valgus angles as negative values). The navigation system used (OrthoPilot®, Aesculap, Tuttlingen, FRG) and the technique of navigation has been described elsewhere [11]. The data registration for the present study was performed after the TKA implantation.
Two free angle measurement applications were downloaded to the smartphone from the Apple Application store: one using inclinometer technology (Goniometer Pro, 5fuf5) and the other using camera technology (Dr. Goniometer, CDM S.r.L.). After navigation-assisted TKA and just before wound closure, the operated knee was positioned at full extension, 30 ± 2°, 60 ± 2°, 90 ± 2° and 120 ± 2° according to the navigated measurement. At each step, the knee flexion angle was measured with both smartphone applications:
-
1.
Inclinometer application the precise measurement technique has been described elsewhere [12]. Briefly, the device was put on the anterior surface of the thigh proximal to the skin incision, and on the anterior surface of the distal tibia distal to the skin incision; the device displayed the angle compared to the horizontal line in both positions, and knee flexion angle was calculated as the sum of the two measurements.
-
2.
Camera application a picture was taken from the lateral side of the operated knee; markers were virtually placed at the level of the greater trochanter, the knee joint and the ankle joint, and the application displayed the knee flexion angle calculated.
Statistical analysis
For each of the ten patients, five navigated, five inclinometer and five camera measurements were obtained for each patient, giving three sets of 50 repeat measurements. The sample size was calculated with the ANOVA test to get a significance level of 0.05 and a power of 0.8 to detect a 10° difference: a minimal group size of 42 measures was required, and 50 measures were actually included in each group. The paired difference between each pair of measurements was calculated. The homogenicity of the variance of the three sets of measurements was tested with a Levene test to validate the use of parametric tests. The difference between the three sets of measurements was analysed with an ANOVA test for repeat measurements, with post hoc comparisons with a paired Wilcoxon test. The correlation between the three sets of measurements was analysed with a Kendall test, with post hoc comparisons with a Spearman test. The coherence between each pair of data was analysed according to Bland–Altman. The influence of all registered pre-operative items was analysed with the appropriate statistical test. All tests were performed at a 0.05 level of significance, and post hoc comparisons were performed at a 0.01 level of significance.
Results
Ten patients participated in the study. There were five men and five women, with a mean age of 69 years (SD 10.8 years) and a mean BMI of 30 (SD 5.7). The mean KSS was 88 points (range 31–148 points). There were six grade 2 and four grade 3 cases according to Ahlback. The mean mechanical femoro-tibial angle was 2° (range −1–5°).
The mean paired difference between navigated and camera measurements was 0.7° (SD 1.5°), with one difference >3°. The mean paired difference between navigated and inclinometer measurements was 7.5° (SD 5.3°), with 16 differences >10°. The mean paired difference between inclinometer and camera measurements was −6.8° (SD5.2°), with 7 differences >10°.
The Levene test showed that the variances of the three sets of measurements were not inhomogeneous (n.s.), allowing using parametric tests for further analysis. The ANOVA test for repeat measurements showed a significant difference between the three sets of measurements (p < 0.001). The post hoc paired comparisons with the Wilcoxon test showed a significant difference between all pairs of measurements (p < 0.001). The Kendall test showed no difference in the distribution of the three sets of measurements (n.s.). The post hoc paired correlations with the Spearman test showed a good coherence between all pairs of measurements (R 2 between 0.02 and 0.12). No pre-operative criteria showed a significant influence on the differences observed.
Discussion
The most important finding of the present study was that the measurement of the knee flexion angle measured with the inclinometer application and the camera application were substantially different, and were each different from the reference measurement with a navigation system designed for TKA. The basic hypothesis of the present study was therefore confirmed. However, there was a strong correlation and a good coherence between the three techniques of measurements, suggesting that the differences were not random.
The inclinometer application showed differences of a size which may be clinically relevant: the mean difference was 7°, and 16/50 differences were >10° (32 %). A random fluctuation which was not related to the degree of extension or flexion measured was observed using this technology. The inclinometry application used in the present study seems to be less accurate than a previously documented application with the same hardware [12]. Accordingly, this application should not be used for measurement of the knee flexion angle.
Measurements taken with the camera application were clinically identical to those obtained using navigation, although the difference of <1° with 1 of 50 with difference was >3° (2 %) reached statistical significance. The size of these differences is clinically irrelevant. This application seems to be more accurate than a previously documented application with another technology [12]. His application seems fit for the purpose measuring the knee flexion angle in a clinical setting, and the image can be simply retained for further use, however, while the less accurate inclinometer could be used by the patient alone, for the camera-based application to be used by the patient alone, a ‘selfie’ in a mirror would be required. This possibility has not yet be explored.
The precise and accurate measurement of the knee range of motion is a critical point during the clinical evaluation of TKA patients. Flexion angles measured by visual evaluation and/or mechanical goniometers are fast, easy to perform and inexpensive, but involve a significant inaccuracy [13, 14]. Radiographic evaluation is accepted as the reference technique [5], but the additional exposure prevents its widespread use. Digital goniometers [4, 17], gait analysis [6, 9] or digital imaging with computer image analysis are too expensive or time-consuming to be used on a routine basis [3, 15, 16].
Navigation systems are accurate and precise measurement tools for the assessment of the three-dimensional positioning of the knee joint, including the angle of knee flexion [2]. It is therefore reasonable to use these systems as a reference technique to test for precision and accuracy of other measurement tools. However, such systems are invasive needing to be pinned to the bones, so cannot be used outside the operating room.
There are some limitations in this study. Although the total number of measurements is high, only ten patients have been included, and the results might not be extended to the general population. Body habitus, knee malalignment or abnormal knee mechanics may affect the accuracy and reliability of measurement. Results might be significantly different for different-sized legs such as a competitive runner versus a large power lifter or even a more common obsess individual. A larger study with more repetition would more fully validate this technology. The measurement was taken under passive conditions, and the results might be altered in the office environment where patients may actively bend the knee or even squat down. Specifically, flexion angle may be thrown off with any measurement technique if there is a component of rotation when a patient attempts an active knee flexion or squat. However, the use of navigation is not possible under this office condition, and there is actually no gold standard non-invasive technique to perform further validation. The accepted reference for similar works, i.e. radiographic measurement, has not been performed; however, the bias is probably limited, as navigation systems may be more precise and accurate than radiographic measurement. The repeatability studies have already been published elsewhere, showing that a similar inclinometer application had a high accuracy with intraclass correlation coefficient around 0.8 for both intra- and inter-observer reproducibility [12]. This study involved only one surgeon, but we see no reason why the results should not be extended to any orthopaedic surgeon. However, our results may be specific to the specific applications used on one specific smartphone. Our findings suggest that any other hardware and software combinations should be validated before clinical use.
Despite these limitations, these results offer a simple and practical way of improving the precision and accuracy of the clinical examination of a TKAR and of its scoring. Using this technology to assess the knee range of motion allows an accurate assessment of this clinically relevant item. The precision and accuracy we report is be higher than published conventional measurement techniques, and especially visual assessment which is most commonly used in the routine practice. Furthermore, this cheap and widely available technology may be used to monitor the rehabilitation course by the physiotherapist or even the patient himself or herself (with help). Access to information on range of motion might avoid unnecessary post-operative visits or validate the necessity for further follow-up. The simple storage and transmission of images by smartphones are further advantages of this method.
Conclusion
The camera smartphone application used in this study is fit for the purpose of measurement of the knee range of motion in a routine clinical setting and is substantially superior to inclinometer-based measurement. Camera-based measurement allows a precise, accurate rating of knee range of motion, a key element of clinical scoring systems. The accuracy may be higher than other conventional measurement techniques.
References
Ahlbäck S (1968) Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) Suppl. 277:1–72
Austin MS, Ghanem E, Joshi A, Trappler R, Parvizi J, Hozack WJ (2008) The assessment of intraoperative prosthetic knee range of motion using two methods. J Arthroplast 23:515–521
Bennett D, Hanratty B, Thompson N, Beverland D (2009) Measurement of knee joint motion using digital imaging. Int Orthop 33:1627–1631
Cleffken B, van Breukelen G, Brink P, van Mameren H, Damink SO (2007) Digital goniometric measurement of knee joint motion. Evaluation of usefulness for research settings and clinical practice. Knee 14:385–389
Edwards JZ, Greene KA, Davis RS, Kovacik MW, Noe DA, Askew MJ (2004) Measuring flexion in knee arthroplasty patients. J Arthroplast 19:369–372
Favre J, Jolles BM, Aissaoui R, Aminian K (2008) Ambulatory measurement of 3D knee joint angle. J Biomech 41:1029–1035
Ferriero G, Vercelli S, Sartorio F, Lasa SM, Ilieva E, Brigatti E, Ruella C, Foti C (2013) Reliability of a smartphone-based goniometer for knee joint goniometry. Int J Rehabil Res 36:146–151
Hefti F, Müller W, Jakob RP, Stäubli HU (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc 1:226–234
Huddleston J, Alaiti A, Goldvasser D, Scarborough D, Freiberg A, Rubash H, Malchau H, Harris W, Krebs D (2006) Ambulatory measurement of knee motion and physical activity: preliminary evaluation of a smart activity monitor. J Neuroeng Rehabil 3:21
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Jenny JY, Clemens U, Kohler S, Kiefer H, Konermann W, Miehlke RK (2005) Consistency of implantation of a total knee arthroplasty with a non-image-based navigation system: a case-control study of 235 cases compared with 235 conventionally implanted prostheses. J Arthroplasty 20:832–839
Jenny JY (2013) Measurement of the knee flexion angle with a Smartphone-application is precise and accurate. J Arthroplast 28:784–787
Lavernia C, D’Apuzzo M, Rossi MD, Lee D (2008) Accuracy of knee range of motion assessment after total knee arthroplasty. J Arthroplast 23(Suppl 1):85–91
Lenssen AF, van Dam EM, Crijns YH, Verhey M, Geesink RJ, van den Brandt PA, de Bie RA (2007) Reproducibility of goniometric measurement of the knee in the in-hospital phase following total knee arthroplasty. BMC Musculoskelet Disord 8:83
Naylor JM, Ko V, Adie S, Gaskin C, Walker R, Harris IA, Mittal R (2011) Validity and reliability of using photography for measuring knee range of motion: a methodological study. BMC Musculoskelet Disord 12:77
Russell TG, Jull GA, Wootton R (2003) Can the Internet be used as a medium to evaluate knee angle? Man Ther 8:242–246
Yaikwawongs N, Limpaphayom N, Wilairatana V (2009) Reliability of digital compass goniometer in knee joint range of motion measurement. J Med Assoc Thai 92:517–522
Acknowledgments
The authors thank gratefully Prof. Justin Cobb for having reviewed the final version of the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jenny, JY., Bureggah, A. & Diesinger, Y. Measurement of the knee flexion angle with smartphone applications: Which technology is better?. Knee Surg Sports Traumatol Arthrosc 24, 2874–2877 (2016). https://doi.org/10.1007/s00167-015-3537-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3537-4