Abstract
Purpose
This case-series outcome study presents a surgical technique for anatomic double-bundle anterior cruciate ligament (ACL) reconstruction with 4-tunnel using two interference screws. There was a 2-year minimum follow-up.
Methods
From January to December 2009, an ACL 4-tunnel, anatomic, double-bundle reconstruction was performed on 27 patients. Double-strand hamstring tendon grafts were used in each femoral tunnel as well as two interference screws. Tibial fixation was insured through manual tension, by tying non-absorbable sutures on the bone bridge between the two tunnels at 20° of knee flexion. Clinical assessments included the International Knee Documentation Committee (IKDC) and Lysholm knee scores, range of motion (ROM), pivot-shift test, single-leg hop, and quadriceps-hamstrings strength tests using a hand-held dynamometer. Anterior knee laxity was also assessed using a rolimeter. A single examiner performed all testing pre-operatively at 6 months and during the 2-year follow-up.
Results
All patients were assessed during the 2-year follow-up. At that time, 92 % of the patients presented normal anterior laxity (average, 1.3 ± 0.5 mm) and rotational knee stability. No statistical side-to-side difference was found for ROM, muscle strength, single-leg hop, and function (n.s.). All patients presented a normal knee function according to the IKDC and the Lysholm score. In addition, no infection, graft failure, or pain were observed at the harvesting site.
Conclusion
The study shows that satisfactory results in relation to knee laxity, function, and strength can be achieved with the implant-free tibial fixation in the ACL double-bundle reconstruction with two interference screws.
Level of evidence
Therapeutic case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to the growing interest in sports participation during adulthood, the reconstruction of the anterior cruciate ligament (ACL) became a commonly performed procedure. Furthermore, good-to-excellent reconstruction results have been reported [7]. However, a critical review of the literature revealed that the success rate varies between 69 and 95 %. Conventional reconstruction techniques are more successful in limiting anterior tibial translation, but they may be insufficient in controlling combined rotatory movements of the knee [22]. Thus, ACL reconstruction with an anatomic double-bundle technique has become popular in recent years. However, the double-bundle reconstruction with four tunnels and with four implants for grafts fixation increases the cost of the surgery when compared to single-bundle reconstruction.
Several biomechanical [28–30] and clinical studies [11, 13, 19] have investigated the relevance of additional posterolateral (PL) bundle on knee transversal plane stability. Recent systematic review reported superior clinical results in relation to the anterior and rotational stability in patients who received an anatomic double-bundle technique when compared to a single-bundle technique [27]. Although there is a trend to reconstruct the ACL with the double-bundle technique, some surgeons still prefer using the single-bundle technique due to its low cost and convenience [7].
However, if the anatomic, double-bundle reconstruction is performed using the same material as the single-bundle reconstruction, patients could benefit from greater rotational stability and better function, without increasing the cost of the surgical procedure. Therefore, the purpose of this study is to present a new surgical technique and prospectively report the clinical outcomes of anatomic double-bundle ACL reconstruction with two interference screws with an evaluation at 6 months and at 2-year follow-up. The authors of the present study hypothesized that no significant side-to-side difference would be found in relation to knee stability, muscle strength, range of motion (ROM), and function.
Materials and methods
From January to December 2009, ACL reconstruction with an anatomic double-bundle using hamstring tendon grafts was performed on 27 males. All patients were evaluated pre-operatively, at 6 months and at 2 years post-operatively. Patient data are presented in Table 1. The indication for surgery was a diagnosis of ACL rupture based on clinical evaluation and magnetic resonance imaging (MRI) in a patient with marked instability who wished to regain his pre-injury level of activity. The exclusion criteria included combined collateral ligament injury, posterior cruciate ligament or PL corner injury, previous knee surgery, and grade II or III osteoarthritis. All patients had to have at least two positive tests for instability (Lachman test, anterior drawer test, or pivot-shift test).
Surgical technique
Initially, a full arthroscopic assessment was performed on each patient to confirm the ACL tear and other injuries to the meniscus and cartilage. The harvesting step for hamstring tendons was similar to the technique utilized in the single-bundle hamstring graft. The diameter of the semitendinosus and gracilis was tripled, usually 8 and 7 mm, respectively. The semitendinosus graft was used for the anteromedial (AM) bundle reconstruction, whereas the gracilis was utilized for the PL bundle. Grafts were prepared individually using No. 1-0 Vicryl suture (Ethicon, SP, BR) on both ends. At the end of the tibial grafts, three non-absorbable Ethibond wires No. 5 were sutured with a 1-cm space between each one.
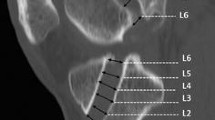
The AM femoral tunnel was created through the transportal technique on a conventional surgical table. The position of the AM tunnel was posterior to the femoral condyle wall, approximately at 11 o’clock in the right knee and 1 o’clock in the left knee. The guidewire was then drilled into the lateral femoral condyle. The AM tunnel was placed as posterior as possible without breaking the posterior wall of the femoral condyle. It was placed at the posterior part of the intercondylar notch at 120° of knee flexion. The tunnel was drilled with a cannulated drill (diameter of 4 mm) over the guidewire. The final drilling of the tunnel was made according to the diameter of the grafts obtained intraoperatively. The diameter of the AM tunnel was typically 7 mm, and the depth of the tunnel was 30 mm. Furthermore, the surgeon drilled the PL tunnel at the same position. This tunnel was performed at 130° of knee flexion at approximately 9:30 o’clock position for the right knee and 2:30 o’clock position for the left knee. The angle between the AM and PL femoral tunnels was kept at approximately 25°–30° between the AM and PL femoral tunnels. The wall between both tunnels was at least 2 mm with a tunnel depth of 30 mm. Conventional metal screws provided fixation of the grafts for both femoral tunnels.
The tibial tunnels were performed with a tibial guide, starting with the PL tunnel. This tunnel was performed with the guidewire positioned on the PL aspect of the tibial insertion of ACL. The position of the AM tibial tunnel was based on the footprint of the remaining ACL fibres. A bone bridge of approximately 1–2 mm was maintained between both tibial tunnels. The AM and PL tunnels were typically 8 and 7 mm, respectively. The grafts were passed retrograde, i.e. from the tibial tunnel to the femoral tunnel. A guidewire was used, followed by a fixation with titanium interference screws (inside out). The PL bundle was first fixed in the PL tunnel, and then, the AM bundle was fixed in the AM femoral tunnel. Afterwards, a cycling of 40 repetitions was performed.
The fixation of the tibial graft was made by lashing a non-absorbable No. 5 Ethibond suture, i.e. without using screws. In the present technique, both bundles were fixed at 20° of knee flexion. While the surgeon performed the fixation in the first pair of wires, the surgical assistant maintained a moderate traction on the other two pairs of wires. Thus, the surgeon gave the node in the second pair of wires (pair identified with two nodes), while the assistant maintaining a moderate traction on the third pair (pair identified with three nodes). Finally, the last pair of wires was fixed. Six usual nodes were made in each pair of wires, being supported and blocked with a tweezers, on the edge of the orifice of the AM bundle tibial tunnel. After the graft fixation in the tibial tunnels, the surpluses of nodes were removed with a short Kelly into the hole on the AM tibial tunnel. There was a concern to avoid friction of the subcutaneous tissue and, consequently, difficulties in subcutaneous tissue healing.
Postoperative rehabilitation
The patients were encouraged to recover ROM and to tolerate full weight bearing on the first day after surgery. Crutches were used during for 2–3 weeks. No orthotic brace was prescribed. A rehabilitation programme was prescribed that included quadriceps-strengthening exercises and ROM activities emphasizing full extension. Cycling was allowed when patient showed 100° of knee flexion. Closed kinetic chain exercises were immediately suggested. However, the open kinetic chain exercises in a full ROM (90°–0° of knee flexion) were allowed only after 9 weeks. Running was allowed at 3 months, and pivoting exercises at 6 months post-operatively [9, 20]. A therapist provided all treatment until a return to sports was possible.
Follow-up evaluation
Clinical evaluation of knee function and stability was performed pre-operatively, at 6 months and at 2 years after reconstruction during regular follow-up. All patients were evaluated regarding activity level with the International Knee Documentation Committee (IKDC), the Lysholm subjective knee evaluation forms [19, 28, 29], ROM with a goniometer [20], and the pivot-shift test [19, 28, 29].
Quadriceps and hamstring muscle strength was evaluated by measuring the maximum isometric voluntary contraction (MIVC), using a hand-held dynamometer (Lafayette Instrument Co, IL, USA) [26]. In order to measure the quadriceps, the subject was asked to sit on a table, with his arms held against his body, and his hips and knees positioned at 90° and 60° of flexion, respectively. The dynamometer was positioned 2 in. proximal to the lateral malleolus on the anterior aspect of the tibia. To measure the hamstrings, the subject was positioned in a prone position on the table, with the knee flexed at 30°. The dynamometer was placed two inches proximal to the lateral malleolus on the posterior aspect of the leg. The leg was stabilized by an inelastic band. Previous studies indicated good-to-excellent reliability and intra-class correlation coefficients (ICCs) of 0.89 and 0.92, respectively [6, 17, 23]. The single-leg hop test was also used to measure knee function. When performing the hop test, the patient was instructed to jump forward as far as possible [5].
Anterior knee laxity was analysed by an arthrometer (Rolimeter TM, Aircast ® , FR). The subject was positioned in a supine position on the table, with a cushion under the knee to stabilize the joint at 25° of flexion. A Lachman test was then performed to quantify the anterior tibial translation [18]. The examiner applied the maximum manual force until the anterior endpoint was reached. The side-to-side difference below 3 mm was considered normal, between 3 and 5 mm “nearly normal”, between 6 and 10 mm “abnormal”, and above 10 mm “severely abnormal”. These factors were all rated according to the IKDC guidelines. All surgical procedures were performed by a senior orthopaedic surgeon with more than 17 years of knee surgery experience. All pre- and post-operative assessments were made by an independent examiner, not involved in the treatment.
This work received approval from The Institutional Review Board of Bandeirantes Hospital (CAAE—12233113.3.0000.5485), and all participants gave informed, written consent prior to participation.
Statistical analysis
The sample size estimation calculated was justified based on the change of anterior laxity between the injured limb and the contralateral limb. A 2.0-mm difference between limbs and the corresponding standard deviation of 2.0 mm was considered to be clinically relevant. It was determined that a sample size of 25 patients would be necessary to detect the 2.0 mm difference with 80 % power when alpha was set equal to 0.05 [12]. Data were analysed with SPSS Version 13.0 (SPSS Inc, Chicago, IL, USA). Descriptive statistics for demographic data and all outcome measures were expressed as averages and standard deviations. Chi-square test was performed to compare data from the subjective IKDC assessment, the Lysholm scale, ROM, pivot-shift test, anterior knee laxity, muscle strength, and the single-leg hop test. These analyses were categorized in accordance with the IKDC form.
Results
In the present study, no graft failure, no pain complaints, nor infection were found near the graft incision. The surgical time was on average 89.0 ± 4.0 min. Concomitant injuries such as posterior cruciate ligament, collateral ligaments, PL complex, or moderate-to-severe osteoarthritis were excluded (Table 1).
IKDC and Lysholm scores
According to the IKDC and the Lysholm final score, all patients presented a significant knee function improvement at follow-ups when compared to pre-operatively (n.s.) (Tables 2, 3).
ROM, strength, and single-hop test
Pre-operatively, a significant side-to-side deficit in ROM was found for knee extension (3.9 ± 1.2, P < 0.03) and flexion (11.0 ± 3.1, P < 0.01). However, no side-to-side difference was found at 6 months (extension, 0.8 ± 0.4; flexion, 1.0 ± 0.6; n.s.) and the 2-year follow-up (extension, 0.6 ± 0.3; flexion, 0.5 ± 0.6; n.s.). All patients showed “normal” ROM post-operatively. On average, the patients presented side-to-side quadriceps strength deficits of 9 % at the 6-month follow-up and 6 % at the 2-year follow-up. For the hamstrings strength, the deficit was 10 % at 6 months and 8 % at the 2-year follow-up. However, this side-to-side strength deficit for both muscle groups was not statistically significant (n.s.). Therefore, all patients presented “normal” or “nearly normal” strength scores at follow-up. Finally, no significant difference was found for the single-leg hop test at 6 months and at the 2-year follow-up when the injured and non-injured limbs (n.s.) were compared. No patient showed an “abnormal” or “severely abnormal” score for ROM, strength, and the hop test post-operatively (Table 4).
Anterior knee laxity and pivot-shift tests
There was a significant lower anterior displacement at the post-operative evaluation when compared to pre-operative (P < 0.05) (Table 5). A significant rotational instability was found in the injured knee pre-operatively (P < 0.001). However, there was no side-to-side difference at 6 months and at the 2-year evaluation (n.s.) (Table 6).
Discussion
The most important findings of the present study were the satisfactory clinical outcomes of double-bundle ACL reconstruction technique using two interference screws during the 2-year follow-up. Patients presented normal side-to-side rotational and anterior knee laxity, ROM, as well as satisfactory and excellent results in function, muscle strength, and subjective assessments.
Despite the fact that the double-bundle ACL reconstruction has become popular in recent years, the cost of the procedure can increase the cost of surgery more than ten times due to the material and surgical time required when compared to the single-bundle technique [7]. However, this study presents a technique using two metallic interference screws, which costs less than conventional double-bundle technique with four bioabsorbable screws, or four metallic interference screws, or endobutton, or even two bioabsorbable interference screws [8, 15]. These findings imply additional direct costs to the health system of emerging countries. As aforementioned, the patients in the present study were submitted to femoral fixation with metallic screws, despite the fact that some biomechanical studies have shown that bioabsorbable screws are stronger than metallic screws in the single-cycle load-to-failure test [3, 16, 21]. The initial doubt was in relation to loss of graft fixation due to using a tibial fixation by tying. However, it is important to highlight that no patient experienced any “giving way” episodes during the rehabilitation protocol or even during the 2-year follow-up.
Many researchers have focused on replicating anatomic ACL reconstruction studies in order to reproduce similar kinematics of the injured knee when compared to the healthy knee [1, 2, 4, 8, 10, 14, 24, 25]. The patients in the present study showed no side-to-side difference for the anterior and rotational clinical knee stability. In addition, no patients presented “abnormal” or “severely abnormal” knee laxity or graft failures at the 2-year follow-up. These data corroborate previous studies that showed low graft failure incidence in patients submitted to double-bundle reconstruction [13, 25]. Moreover, the present outcomes referring to normal function, satisfactory stability, and an absence of post-operative complications allow the authors of this study to affirm that double-bundle reconstruction without tibial implants is a safe technique and provides similar outcomes than other technique with four implants.
The limitations of this case-series study include a small number of patients, no comparison group treated with the single-bundle reconstruction, or other double-bundle reconstruction. However, when considering the comparison with the healthy knee, the results were satisfactory in all clinical measurements. There was also a lack of comparison between “aggressive” and “nonaggressive” rehabilitation protocols for evaluation of the effect of implant-free tibial fixation. Another possible bias was the fact that both bundles were fixed simultaneously at 20 degrees of knee flexion. While some studies have suggested a fixation at approximately 45°–60° of knee flexion [2, 28], the authors of the present study believe that both bundles fixed at 20° of knee flexion can restore relatively normal tension curves in each bundle, thus avoiding excessive stress in the graft. Another limitation of this fixation is the fact that it was not possible to apply quantitative force to the grafts. The clinical relevance of this study is the determination that satisfactory results can be achieved with double-bundle, ACL reconstruction while using the same surgical material as is utilized in single-bundle reconstruction. Biomechanical studies are also needed to evaluate the dynamic rotational stability of the knee between the tibial implant-free double-bundle and conventional double-bundle, as well as the tibiofemoral and patellofemoral stress.
Conclusion
The study demonstrated satisfactory results in relation to knee stability, function, and strength. This was achieved with an implant-free tibial fixation of a double-bundle ACL reconstruction with two interference screws.
References
Adachi N, Ochi M, Uchio Y et al (2004) Reconstruction of the anterior cruciate ligament single- versus double-bundle multistranded hamstring tendons. J Bone Joint Surg Br 86(4):515–520
Aglietti P, Giron F, Losco M, Cuomo P, Ciardullo A, Mondanelli N (2010) Comparison between single- and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized, single-blinded clinical trial. Am J Sports Med 38(1):25–34
Alexander JW, Gold JE, Icenogle KD, Noble PC, Lowe WR (2010) Anatomic double-bundle anterior cruciate ligament reconstruction: kinematics and knee flexion angle-graft tension relation. Arthroscopy 26:202–213
Asagumo H, Kimura M, Kobayashi Y et al (2007) Anatomic reconstruction of the anterior cruciate ligament using double-bundle hamstring tendons: surgical techniques, clinical outcomes, and complications. Arthroscopy 23(6):602–606
Augustsson J, Thomee R, Karlsson J (2004) Ability of a new hop test to determine functional déficits after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 12:350–355
Bohannon RW (1990) Hand-held compared with isokinetic dynamometry for measurement of static knee extension torque (parallel reliability of dynamometers. Clin Phys Physiol Meas 11:217–222
Brophy RH, Wright RW, Matava M (2010) Cost analysis of converting from single to double anterior cruciate ligament reconstruction. Am J Sports Med 37(4):683–687
Carneiro M, Navarro RD, Nakama GY, Barreto JM, Queiroz AAB, Luzo MVM (2009) Arthroscopy double-bundle reconstruction of anterior cruciate ligament using hamstring tendon grafts fixation with two interference screws. Rev Bras Ortop 44:441–445
Fukuda TY, Fingerhut D, Moreira VC et al (2013) Open kinetic chain exercises in a restricted range of motion after anterior cruciate ligament reconstruction: a randomized clinical trial. Am J Sports Med 41(4):788–794
Georgoulis AD, Papadonikolakis A, Papageorgiou CD et al (2003) Three-dimensional tibiofemoral kinematics of the anterior cruciate ligament-deficient and reconstructed knee during walking. Am J Sports Med 31(1):75–79
Izawa T, Okazaki K, Tashiro Y, Matsubara H, Miura H, Matsuda S, Hashizume M, Iwamoto Y (2011) Comparison of rotatory stability after anterior cruciate ligament reconstruction between single-bundle and double-bundle techniques. Am J Sports Med 39:1470–1477
Keays SL, Bullock-Saxton JE, Keays AC, Newcombe PA, Bullock MI (2007) A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and gracilis tendon graft. Am J Sports Med 35(5):729–739
Komzák M, Hart R, Okál F, Safi A (2012) Does the posterolateral bundle influence rotational movement more than the anteromedial bundle in anterior cruciate ligament reconstruction?: A clinical study. J Bone Joint Surg Br 94(10):1372–1376
Kondo E, Yasuda K, Azuma H, Tanabe Y, Yagi T (2008) Prospective clinical comparisons of anatomic double-bundle versus single-bundle anterior cruciate ligament reconstruction procedures in 328 consecutive patients. Am J Sports Med 36:1675–1687
Kondo E, Yasuda K, Miyatake S, Kitamura N, Tohyama H, Yagi T (2012) Clinical comparison of two suspensory fixation devices for anatomic double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20(7):1261–1267
Kousa P, Järvinen TLN, Vihavainen M, Kannus P, Järvinen M (2003) The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part I: femoral site. Am J Sports Med 31:174–181
Magalhães E, Fukuda TY, Sacramento SN, Forgas A, Cohen M, Abdalla RJ (2010) A comparison of hip strength between sedentary females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther 40(10):641–647
Muellner T, Bugge W, Johansen S, Holtan C, Engebretsen L (2001) Inter- and intratester comparison of the rolimeter knee tester: effect of tester’s experience and the examination technique. Knee Surg Sports Traumatol Arthrosc 9:302–306
Muneta T, Koga H, Mochizuki T et al (2007) A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and doublebundle techniques. Arthroscopy 23(6):618–628
Myer GD, Paterno MV, Ford KR, Hewett TE (2006) Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther 36:385–402
Pinczewski LA, Deehan DJ, Salmon LJ, Russell VJ, Clingeleffer A (2002) A five-year comparison of patellar tendon versus four-strand hamstring tendon autograft for arthroscopic reconstruction of the anterior cruciate ligament. Am J Sports Med 30:523–536
Ristanis S, Giakas G, Papageorgiou CD et al (2003) The effects of anterior cruciate ligament reconstruction on tibial rotation during pivoting after descending stairs. Knee Surg Sports Traumatol Arthrosc 11(6):360–365
Robinson RL, Nee RJ (2007) Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J Orthop Sports Phys Ther 37:232–238
Seon JK, Gadikota HR, Wu JL, Sutton K, Gill TJ, Li G (2010) Comparison of single- and double-bundle anterior cruciate ligament reconstructions in restoration of knee kinematics and anterior cruciate ligament forces. Am J Sports Med 38(7):1359–1367
Suomalainen P, Järvelä T, Paakkala A, Kannus P, Järvinen M (2012) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 5-year results. Am J Sports Med 40:1511–1518
Trudelle-Jackson E, Jackson AW, Frankowski CM, Long KM, Meske NB (1994) Interdevice reliability and validity assessment of the nicholas hand-held dynamometer. J Orthop Sports Phys Ther 20(6):302–306
Van Eck CF, Kopf S, Irrgang JJ, Blankevoort L, Bhandari M, Fu FH, Poolman RW (2012) Single-bundle versus double-bundle reconstruction for anterior cruciate ligament rupture: a meta-analysis—does anatomy matter? Arthroscopy 28:405–424
Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL (2002) Biomechanical analysis of anatomic anterior cruciate ligament reconstruction. Am J Sports Med 30:660–666
Yamamoto Y, Hsu WH, Woo SL, Van Scyoc AH, Takakura Y, Debski RE (2004) Knee stability and graft function after anterior cruciate ligament reconstruction a comparison of a lateral and an anatomic femoral tunnel placement. Am J Sports Med 32:1825–1832
Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W (2007) The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med 35:223–227
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sacramento, S.N., Magalhães, E., Christel, P. et al. A new technique in double-bundle anterior cruciate ligament reconstruction with implant-free tibial fixation. Knee Surg Sports Traumatol Arthrosc 24, 2831–2837 (2016). https://doi.org/10.1007/s00167-014-3430-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3430-6