Abstract
India launched the Safe Motherhood Scheme (Janani Suraksha Yojana or JSY) in 2005 in response to persistently high maternal and child mortality rates. JSY provides a cash incentive to socioeconomically disadvantaged women for childbirth at health facilities. This study explores some unintended consequences of JSY. Using data from two large household surveys, we examine a policy variation that exploits the differential incentive structure under JSY across states and population subgroups. We find that JSY may have resulted in a 2.5–3.5 percentage point rise in the probability of childbirth or pregnancy over a 3-year period in states already experiencing high population growth.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Since their introduction in Mexico and Brazil during the 1990s, conditional cash transfer (CCT) programs have revitalized public health service delivery mechanisms in many low- and middle-income countries. Many of these countries face challenges in building capacity through expansion and improvement of the public healthcare system, and in ensuring that the poor access free or subsidized services that could improve their health. CCTs address the latter problem through demand-side incentives that educate the poor about public health services and encourage their use (Fiszbein et al. 2009).
CCTs are a relatively new policy in India, a country that has long struggled with poor maternal and child health outcomes. India accounts for almost a fifth of the world’s maternal deaths (UNFPA 2012), and its infant mortality rate is higher than its less well off neighbors.Footnote 1 Despite recent investments in improving public health facilities, India is unlikely to reach its Millennium Development Goals on reduced child and maternal mortality.Footnote 2
In 2005, the Indian government launched the Safe Motherhood Scheme (Janani Suraksha Yojana, or JSY), a CCT that rewards pregnant women who belong to relatively poor states, are below the official poverty line, or belong to socioeconomically backward castes; benefits are conditional upon having institutional childbirth. JSY is among the world’s largest CCTs—in 2010–2011, it covered over 11.3 million beneficiaries, with an annual budget of more than US$300 million (MoHFW 2012).Footnote 3
A number of studies have looked at whether JSY has been able to achieve its stated goals of increasing institutional births and reducing maternal and child mortality, particularly among the poor. Lim et al. (2010) find that although JSY does not sufficiently cover the poorest segment of the society, and regional variation is a major concern, it had a modest effect on antenatal care usage and institutional childbirths.Footnote 4 They find that the program has led to small reductions in mortality—between 3.7 and 4.1 perinatal deaths per 1000 pregnancies, and 2.3–2.4 neonatal deaths per 1000 live births. However, Das et al. (2011) point out inconsistencies such as ambiguity and measurement errors in the Lim et al. (2010) study, and caution against prematurely calling JSY a success. In a different study, Powell-Jackson et al. (2015) do not find any effect of JSY on neonatal mortality. Das et al. (2011) and Gopalan and Durairaj (2012) also argue that JSY may be associated with higher out-of-pocket medical expenditure and impoverishment.
Although JSY has been implemented across all Indian states, the cash incentive structure varies depending on the state’s level of economic progress, and across different socioeconomic groups. Ten states, generally poor and with low rates of institutional (i.e., at healthcare facilities) childbirth, were included in the low-performing states (LPS) group. The cash incentive provided to pregnant women in these states is twice what is provided in the remaining high-performing (HPS) states.Footnote 5 In addition, the eligibility criteria are stricter in HPS, e.g., women who are above the official poverty line, or do not belong to socioeconomically disadvantaged caste groups, are not eligible for the program.
We rely on this structural difference in cash incentive across states and population subgroups as a policy variation allowing us to analyze the unintended effects of JSY. Cash incentives under JSY can be large, particularly for LPS mothers (up to INR 1400 or US$28) per birth, and health workers implementing the program can earn up to INR 600 (US$12) per birth. With a strong monetary incentive associated with childbirth, households may increase fertility (Morris et al. 2004; Stecklov et al. 2007) either on their own, or health workers who benefit from the JSY payment may be less energetic in advocating for family planning.
In many developed countries, public policies that provide financial incentives are often linked with higher fertility rates.Footnote 6 In the developing world, the evidence on the effect of financial incentives on demographic outcomes is very limited. In response to randomized CCTs for child schooling, healthcare access, and nutrition, Stecklov et al. (2007) find a 4.8 percentage point rise in fertility in Honduras, but no effect in two other countries.Footnote 7 Morris et al. (2004) also find that pregnancy decreased at a lower rate (10.4 % relative reduction) among the treatment group as compared with the control group (26.3 % relative reduction), following the Honduran program. However, Todd et al. (2011) find that a similar Nicaraguan CCT may have reduced the odds of a birth by 32 % in the longer run, indicating an increase in birth spacing.
The only contemporary study that evaluates some unintended effects of JSY is Powell-Jackson et al. (2015). In addition to finding a positive effect on the uptake of maternal care, and no impact on neonatal mortality, the authors find a 1.7 percentage point unintended rise in pregnancy rates over a baseline of 8.8 %. However, the authors use the timing of JSY introduction for statistical identification of its coverage level in a district. Program introduction may itself suffer from selection bias, i.e., it may depend upon the characteristics of districts (e.g., availability of health facilities with maternity services). Although the authors have included some covariate determinants of the introduction timing, it is not clear if the selection bias can be fully mitigated, since unobserved characteristics of the districts cannot be captured. In addition, Das et al. (2011) find that there may be measurement errors in the JSY coverage and utilization data used by the study.
Our study complements and extends the existing literature. We analyze the unintended demographic effects of JSY, one of the largest CCTs in the world. We use data from two consecutive rounds of District Level Household Survey (DLHS 2002–2004 and 2007–2008) of India to estimate the difference-in-difference (DID) effect of JSY on fertility in LPS states when compared with HPS states. In order to mitigate biases arising from measurement errors in JSY coverage or utilization data, we use an intent-to-treat approach by considering all potential beneficiaries in our analysis. We control for unobserved heterogeneity between the two groups by using an empirical approach based on state administrative borders and propensity score matching methods.
We find that the probability of a childbirth or pregnancy is significantly higher among LPS mothers after the implementation of JSY when compared with their HPS counterparts, controlling for initial conditions and other socioeconomic characteristics. Growth rates of population in these poorer LPS states were higher than those in the rest of the country even before JSY, and these states are currently the foci of aggressive family planning policies (GoI 2006). Therefore, JSY may pose a conflict with the objectives of such family planning policies.
2 About Janani Suraksha Yojana
The central government of India launched JSY in 2005 under the National Rural Health Mission (NRHM) with the objective of increasing the proportion of institutional childbirths. Although implemented across the entire country, the program was particularly targeted toward the following ten states with a higher prevalence of non-institutional births: Jammu and Kashmir, Uttar Pradesh, Uttarakhand, Bihar, Jharkhand, Madhya Pradesh, Chhattisgarh, Assam, Rajasthan, and Orissa. These states, among the poorest, are also focal points for family planning policies (empowered action group or EAG states) because of their high population growth.Footnote 8 These ten states together are classified as the low-performing states (LPS), while all the remaining states of India are known as the high-performing states (HPS) under JSY.
In LPS, all pregnant women delivering babies at a public healthcare facility or an accredited private facility are eligible for a cash benefit under JSY. This is applicable for all women in these states, irrespective of their income level or social status. In HPS, only women who are officially below the poverty line (BPL) or those who belong to government-designated socioeconomically disadvantaged scheduled caste (SC) and scheduled tribe (ST) groups are eligible for JSY benefit.Footnote 9 Eligible women in HPS can only obtain the benefit up to a lifetime maximum of two live births. There is no such restriction on the number of births for eligible LPS women.
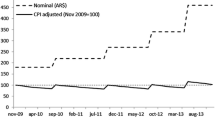
The program not only differs in its eligibility criteria across LPS and HPS but also the financial incentives for eligible women are tiered according to regional needs (see Table 1). Since the rate of non-institutional childbirth is higher in LPS, JSY provides a higher cash incentive to eligible women in these states. Then, within each state, the benefits are again higher in rural areas as compared with urban areas.
The program is administered in LPS with help from trained female health workers known as the accredited social health activists (ASHAs). An ASHA typically resides in a village and forms a health partnership with a pregnant woman—facilitating antenatal and postnatal care usage, and ushering her to a healthcare facility at the time of delivery. In HPS, these duties are performed by other health workers such as auxiliary nurse midwives (ANM), Anganwadi (nutrition) workers, or traditional birth attendants (known as dai).
Under the terms of JSY, the health worker administering the scheme delivers a one-time cash reward to the mother at the time of the institutional childbirth. The health workers themselves are eligible for a separate cash reward for a successful institutional childbirth under their supervision. Since 2013, the cash incentive for the health worker has been divided into two equal parts for facilitating antenatal care and institutional delivery. Delivery at a government health facility such as a primary health center or sub-center, community health center, and district hospital, or an accredited private health facility is considered as institutional childbirth. Private health facilities in each district are accredited under JSY by the local NRHM office.
The health worker is required to arrange and pay for transport of the pregnant woman to a health facility at the time of delivery. If the pregnant woman travels herself to a facility for delivery without any assistance from the health worker, she would receive an additional INR 250 for transport cost from funds earmarked for the health worker incentive. If the baby is delivered on the way to a health facility, the birth is eligible for JSY benefit if the mother and the child receive inpatient post-delivery care from the facility.Footnote 10
JSY also provides a separate INR 500 cash incentive for deliveries that take place at home instead of a facility. However, this incentive is only allowed to BPL mothers who are at least 19 years old (up to a lifetime maximum of two live births). No other women are eligible for this benefit. The size of the home-birth incentive is the same INR 500 for these eligible BPL mothers in LPS and HPS. The ASHA or health worker does not receive a cash incentive in case of a home birth.
For the purpose of our study, we use the differential JSY incentive structure for institutional childbirths as our identification strategy. It is obvious that an evaluation of the JSY will suffer from selective program placement bias if one were to examine its intended effect on the rate of institutional childbirths. However, our objective is to evaluate the effect of JSY on fertility rates. The placement bias is unlikely to affect secondary outcomes such as fertility. Our DID matching methodology will also reduce systematic differences between the LPS and HPS women.
3 Theoretical framework
In order to examine the dynamics of household response to the JSY cash incentive, we present a simple demand for fertility framework drawn from Arroyo and Zhang (1997) and Becker and Lewis (1973). Arroyo and Zhang (1997) developed a generalized intertemporal fertility demand model by incorporating elements from several studies—Heckman and Willis (1976), Wolpin (1984), Hotz and Miller (1984), Rosenzweig and Schultz (1985), Newman (1988), and Leung (1991).
We consider the household as a decision-making unit. The ith household’s lifetime expected value of utility is given by
Where t = τ, … … … … T is the life cycle of the representative household. The household maximizes the above utility function using all information available at time τ. The existing number of children and newborn babies in the household at time t are denoted by \( {M}_t \) and \( {N}_t \), respectively.
Economic literature following Becker and Lewis (1973) and Becker and Tomes (1976) illustrates that households jointly choose fertility (quantity) and the human capital investment (quality) on children. Q t denotes the investment in the quality of children. We assume that the household only invests in an existing child (who belongs to the M t cohort) in period τ, and the investment in a newborn child takes place from period (τ +1). Consumption of all other goods and services by the household at period t is denoted by C t (composite good).
Finally, 0 ≤ u t ≤ 1 denotes the efficiency of contraceptives usage. Higher values of \( {u}_t \) are associated with more effective contraception usage. A value of u t = 0 would typically be associated with no use of contraceptives (or, fully ineffective or improper usage), while examples of u t = 1 (completely effective contraception) may include male or female sterilization. 0 < δ < 1 is the time discount factor.
Number of children in the Arroyo and Zhang (1997) framework evolves through a continuous process. Number of children at a particular time period is determined by the cohort size and childbirths from the previous period:
The number of children born in a period is a function of three factors determining contraceptive efficiency, childbirth probability, and mortality (e.g., stillbirth, neonatal or infant mortality):
Probability of childbirth π b is an indicator of a mother’s natural fecundity, without any contraceptive usage. π m is an indicator of mortality risk of a newborn (including stillbirth). For simplicity, we assume π b and π m to be constants. The expected utility function is maximized subject to the following set of budget constraints for each period t:
Where Y t is household income, and p M t and p u t are the costs of M t and u t respectively, relative to the composite good \( {C}_t \) .
A household’s key decision variable that determines fertility is \( {u}_t \), the choice and efficiency of contraception. A lower value of \( {u}_t \) will increase childbirth or reduce the intervals between consecutive births. This will in turn increase \( {M}_t \), and if quantity-quality tradeoff is present, reduce \( {Q}_t \).
The cash incentive of JSY would reduce p M t , the cost of childbearing and child-rearing in this model. Following Arroyo and Zhang (1997), we present a partial equilibrium analysis that illustrates the analytical effect of such a cash transfer.
The value (maximized utility) function, through a choice of equilibrium levels of \( {u}_t^{*} \) (and therefore N * t ), C * t , and \( {Q}_t^{*} \) is given as follows:
The standard two-period Bellman equation that can be derived from (3) is presented as follows:
where π t = π b (1 − u t ) − π mis the survival probability of a newborn. Assuming Q t M t to be constant, and replacing C t with Y t − p M t Q t M t − p u t u t from Eq. (2), we derive the first order condition for Eq. (4) with respect to u t as:
where ΔV (•; M t + 1; t + 1) = [V (•; M t ; t + 1) − V (•; M t + 1; t + 1)]. This is the so called optimal contraception rule in Arroyo and Zhang (1997). The left-hand side of (5) is the marginal cost of contraception (MCC) and the right-hand side is its expected marginal benefit (EMBC).
With a change in p M t as a result of the JSY cash incentive, the MCC will change as below:
assuming that Q t M t > 0, and since U CC is non-positive. If the cost of childbearing reduces, the marginal cost of contraception (i.e., preventing a childbirth) should also be lower. However, \( \varDelta V \) will also change, and the final effect of p M t on the optimal level of contraception u * t is ambiguous. With reduction in childbearing cost, the household will experience an income effect which may increase the demands for both M t and C t . There may also be a substitution effect—as M t becomes relatively cheaper, households will shift some of their consumption from C t to M t . Therefore, ΔV will reduce and it will counter the fall in MCC. If the reduction in EMBC is relatively larger, the final effect of a reduction in \( {p}_t^M \) on fertility will be positive.
The health workers of JSY may also play a significant role in influencing the fertility decision of the household. The impact of p M t in the above framework holds for households with at least one previous childbirth (i.e., Q t M t > 0). This is based on the implicit assumption that only such households will know the MCC and EMBC functions and \( {p}_t^M \). However, we can generalize this framework under a scenario where households are informed about the post-JSY reduction in childbearing cost p M t by the health workers, and the knowledge on MCC and EMBC is gathered from other sources. In this case, the model will allow the health worker to persuade couples to increase fertility or reduce space between consecutive births. The health worker effect can be valid both for families with no previous children and those with at least one child.
JSY may have an additional effect in our model. The main purpose of the program is to improve institutional childbirth rates and thereby increase survival probabilities of the newborn child and the mother. As Lim et al. (2010) show, JSY may have been successful in reducing perinatal and neonatal death rates by small magnitudes. This is equivalent to a reduction in child mortality risk (π m) or an increase in the survival probability π t = π b (1 − u t ) − π m in our model. As Arroyo and Zhang (1997) discuss, this could increase EMBC and reduce fertility rates due to the so called hoarding effect, i.e., positive relationship between child mortality risk and birth hazard in the current period. Furthermore, JSY might reduce the mortality risks of older children, i.e., children born under JSY may have lower infant or under five mortality rates in the future. In such a case, there could be a reduction in child replacement motive of families, i.e., parents may reduce their future fertility if a child born in the current period is more likely to survive. However, the magnitude of the impact of a change in child mortality on future fertility is known to be generally very small (Arroyo and Zhang 1997).
Therefore, the final effect of JSY on fertility will depend on the relative strengths of the counteracting factors described above.
4 Data and descriptive statistics
We use data from the second and third waves of the District Level Household Surveys (DLHS) of India. The DLHS are independent cross-sectional socioeconomic household surveys covering 601 districts of India, with a special focus on reproductive and child health. The second survey (DLHS-2) was conducted from 2002 to 2004 on a total of 620,107 households, two-thirds of which were from rural areas. DLHS-3 (2007–2008) covered 559,663 rural households and 160,657 urban households. The main respondents of both surveys were currently married women of reproductive age (15- to 44-year-olds in DLHS-2 and 15- to 49-year-olds in DLHS-3).Footnote 11 The samples in both surveys were representative of the population at the district level or above.
The DLHS surveys used a household questionnaire on household characteristics such as location, caste, and religion, along with demographic and educational attainment information for all members. Household’s standard of living was assessed in the form of ownership of various assets including TV, radio, or vehicle, and indicators of living condition such as building material, electrification, and availability of toilets. Furthermore, detailed data on topics such as short-term morbidity of household members, deaths, use of health facilities, maternal health, family planning, and immunization and nutrition of children were collected.
A separate questionnaire administered to married women of reproductive age collected information on birth history. A truncated history of births that occurred only since 2004 was collected by DLHS-3, as compared with a complete lifetime birth history of women in DLHS-2.
In order to prevent any overlap between the pre- and post-JSY years, we consider a subsample of births that includes a baseline of births between 2001 and 2003 from DLHS-2, along with post-JSY births during 2006–2008 from DLHS-3. We create a woman level repeated cross-sectional dataset that contains these births along with the background characteristics of the woman, her husband, and the household.
The DLHS-2 survey was conducted during years 2002–2004. Therefore, the annual birth history of most interviewed women during these years is incomplete. In particular, the lowest number of births reported in DLHS-2 data was from 2004. Therefore, in order to avoid any idiosyncrasies due to incomplete birth history reporting, we exclude births during 2004 from our analysis.
After the introduction of JSY in April 2005, potential beneficiaries would have required some time to become aware of the program, followed by the decision to have a child and pregnancy. Due to lack of data, we cannot incorporate the exact timeframe of this decision process for each beneficiary. Therefore, for simplicity, we ignore all births during 2005 from our analysis.Footnote 12
Our outcome variable of interest is an indicator of fertility—the probability of at least one childbirth or an ongoing pregnancy during 3-year study periods pre- and post-JSY. While some ongoing pregnancies may eventually be unsuccessful (e.g., a stillbirth or an abortion), we are only interested in assessing the impact of JSY on fertility decision and not the final outcome. Therefore, we include ongoing pregnancies in our analysis. Our objective is to evaluate the DID effect of JSY, e.g., whether the probability of childbirth or pregnancy among LPS mothers increased after JSY, as compared with that among the HPS mothers over time.
Pregnant women in HPS who are above the official poverty line, or do not belong to scheduled caste or scheduled tribe groups, are not eligible for JSY. We consider these women as the main control group of our analysis. Similar non-poor and non-SC/ST women in LPS are eligible for the full cash incentive of up to INR 1400, and are considered as our treatment group.Footnote 13
Since the program provides monetary incentive also to poor (BPL) or SC/ST women in HPS, we conduct additional analysis that exploits the tiered incentive structure. This allows us to ex-amine any possible heterogeneous treatment effects. For this second type of analysis, we consider poor or SC/ST LPS women as the strongly treated group (eligible for an incentive of INR 1400), and compare them with poor or SC/ST HPS women, i.e., the weakly treated group (eligible for an incentive of INR 700).
5 Empirical approach: border districts and propensity score matching
A typical treatment-effect analysis framework may suffer from two types of dissimilarities between the comparison groups. First, there may be systematic differences in the initial characteristics of the two groups (e.g., LPS mothers may be generally poorer than HPS mothers). These differences may also be correlated with program placement (e.g., states with high non-institutional childbirth rates were designated as LPS). Second, there may also be heterogeneity in time-varying factors, i.e., socioeconomic conditions may change differently over time across the two groups. If we ignore these differences between the LPS and HPS, least squares estimation of the impact of JSY will produce biased results. Therefore, in order to mitigate such differences, we use an empirical strategy involving a two-stage matching of localities and individuals.
Since there is a wide variation in socioeconomic and cultural factors across India, including all states in our analysis will likely produce large time-invariant differences across the treatment (or strongly treated) and control (or weakly treated) groups. Therefore, at the first step, we restrict our analysis only to women from districts located along the administrative border of LPS and HPS. We assume that these women would be similar in both time-invariant and time-varying characteristics due to their geographic proximity. Figure 1 shows the border districts which we include in our analysis.Footnote 14
A problem with choosing the border district sample is that pregnant mothers from LPS may travel to a nearby HPS area to receive higher monetary benefits. However, JSY is implemented in a very localized way with the help of health workers. It may be difficult for expectant mothers to establish themselves in a new community to receive JSY benefits. Moving across state borders, especially to deliver a baby, may be costly in terms of both time and money and a deterrent to benefit seeking.Footnote 15
However, even after restricting our analysis to the border districts, there may still be systematic differences between LPS and HPS women. Therefore, at the second step, we use propensity score matching (PSM) method to match LPS women with similar HPS women within the border district sample. Following Rosenbaum and Rubin (1983), Heckman et al. (1997), and Dehejia and Wahba (1999), the methodology is briefly described below.
Let Y i1 and Y i0 denote the outcomes of observation i under treatment and control, respectively.
The treatment status is denoted by a binary variable T, where T = 1 for the group which receives the treatment. The treatment effect of interest of a particular observation is denoted by τi = (Y i1 − Y i0). The estimated average treatment effect on the treated (ATT) is given as:
Since a particular sample observation cannot exhibit Y i1 and Y i0 both at the same time (“missing data” problem), simple mean-difference estimation of the treatment effect suffers from bias due to the differences in characteristics between the two groups. Let X denote a vector of covariates (characteristics of sample observations). Matching estimators compare the outcomes of the treatment and control observations that possess similar X covariate values. Estimated propensity scores provide a way of reducing the comparison from over a range of covariates to a single dimension. Let us suppose that π(X) = P(T = 1|X) denotes the probability of treatment conditional on the covariates (i.e., the propensity score). Following (Rosenbaum and Rubin 1983), the unconfoundedness assumption along with the overlap assumption 0 < π(X) < 1∀X imply that the outcomes are orthogonal to the treatment not only conditional on the set X but also conditional on the estimated propensity score:
Therefore, a matching estimator of the average treatment effect on the treated (ATT) can be written as follows:
We conduct two sets of PSM analysis, using the 2001–2003 birth data (pre-JSY) and 2006–2008 birth data (post-JSY), respectively. The propensity score estimation equation is a probit model of the probability of a woman belonging to LPS. It is regressed upon a range of socioeconomic characteristics of the household, the woman, and the neighborhood. Included are the indicators for religion (Muslim/Christian/Sikh), caste group (scheduled caste/scheduled tribe/other backward classes), and age and gender of the household head. We also include variables for husband’s education and woman’s age. The demographic composition of the household is incorporated by including variables for the share of members in various age and gender groups (males and females in the age groups 5–14, 15–24, 25–44, 45–59, and 60 years and above). To capture the effect of a household’s standard of living, we include a series of binary variables related to asset ownership, such as the possession of a radio, sewing machine, TV, bicycle, car, and so on—and indicators of housing condition such as construction quality, availability of toilet and electricity, sources of drinking water, and the type of cooking fuel used.Footnote 16
In addition to household and individual level factors, there may be differences in access to healthcare between LPS and HPS women which affect reproductive care seeking decision. The DLHS surveys collected some data on the availability of health facilities and other amenities in rural areas. From these data, we include the following indicators of access to healthcare—share of villages in a district with at least one public health facility, at least one private health facility, a mother-child welfare center (known as Anganwadi), and a traditional birth attendant (dai)—among the explanatory variables in the propensity score equation.Footnote 17 Also included is the average distance from a village to the nearest town (in kilometers). Finally, since both the DLHS surveys were conducted over multiple years, mothers interviewed later experienced a longer reporting period for childbirth, which could affect fertility rates. Therefore, we include a control for months elapsed since the beginning of the reporting period (January 1, 2004 for DLHS-3, and to maintain consistency, January 1, 2000 for DLHS-2) in the regression.
We divide the border district households into two subsamples and analyze separately, as mentioned earlier (Fig. 2). The first subsample (subsample 1) contains women from the border districts who are neither poor nor SC/ST. Separately within each of the pre- and post-JSY datasets, these women from LPS are matched with similar non-poor and non-SC/ST women from HPS on the basis of estimated propensity scores. We take the difference in childbirth or pregnancy probability (LPS − HPS) between the matched women in the pre-JSY data to create the ATT estimator ATT1 pre−JSY. Similarly, using the post-JSY data, we create ATT1 post−JSY. Then, we calculate the DID estimator of the impact of JSY on childbirth or pregnancy probability (DATT 1) from the pre- to the post-JSY period as follows:
The second subsample (subsample 2) contains the other part of the border district population, i.e., poor or SC/ST women. Again, we produce two ATT estimators separately by matching the LPS women with HPS women within the pre-JSY and post-JSY datasets, denoted by ATT 2 pre−JSY and ATT 2 post−JSY respectively, leading to the estimation of the DID effect of JSY as follows:
We adjust the standard errors of all ATT estimators by using the bias-correction method of Abadie and Imbens (2006). The bias corrected ATT estimators and DATT’s are asymptotically normally distributed.
6 Results
6.1 Evaluation of parallel trends
For a DID analysis to be valid, the “parallel trends” assumption has to be satisfied, i.e., time trends of outcomes across two comparison groups should be statistically indistinguishable until the introduction of the treatment (although levels can be different). In order to test this hypothesis, we first create a woman-year panel dataset from 1993 to 2003 using DLHS-2 data. We then restrict the sample to women only in the bordering districts of LPS and HPS, and analyze their annual probability of childbirth or pregnancy.
The residual average annual probability of birth or pregnancy of these women, after controlling for state fixed effects, are presented in Figs. 3 and 4. We find that during the period leading up to the introduction of JSY, the fertility rates of LPS and HPS women generally followed a parallel trend. However, the trend in fertility among LPS women shows more fluctuations over time. In both the graphs, there is a sharp drop in fertility from 2002 due to a smaller number of reported births or pregnancies. This is due to the incomplete annual birth history during 2002–2004 in DLHS-2 data, as mentioned earlier. However, this discrepancy does not affect our DID analysis since these initial conditions (i.e., lower reported fertility) were similar in LPS and HPS.
We evaluate the trends in fertility in another way. We regress the annual probability of childbirth or pregnancy of each woman on a similar set of explanatory variables as in the propensity score estimation equation—socioeconomic characteristics, demographic composition, asset ownership and living condition of the household, characteristics of the woman and her husband, and access to healthcare. Also included are indicators for LPS, binary variables for years, and the interaction between LPS and year indicators. The coefficients of the LPS-year interaction and their 95 % confidence intervals are presented in Figs. 5 and 6. The results show that starting in 1998, LPS women saw a small decline in fertility rates as compared with HPS women, presumably due to stronger family planning policies (GoI 2006). However, the reduction was often statistically insignificant, satisfying the parallel trends assumption.
Finally, we also use PSM to test the parallel trends assumption. We use the same probit model of propensity score estimation as discussed earlier—including socioeconomic characteristics, demographic composition, asset ownership and living condition of the household, characteristics of the woman and her husband, and access to healthcare as explanatory variables. Then, LPS women are matched with similar HPS women based on the estimated propensity score (nearest-neighbor matching with replacement and within a radius of 0.01). The annual average childbirth or pregnancy probabilities of the two groups of women are presented in Figs. 7 and 8. We find that the movements of these trend lines are very similar to those in Figs. 3 and 4, and they satisfy the parallel trends assumption.
6.2 Propensity score estimation and covariate balancing
We use a probit regression framework to estimate the propensity score of a woman belonging to LPS. Results from the estimation in our two subsamples and two time periods are presented in Table 2. We find most regression coefficients to be highly statistically significant, exhibiting their strong association with the LPS status of a woman.
However, strong relationship between LPS status and the covariates alone is not sufficient to ensure good quality matches based on propensity scores. We use a nearest-neighbor matching (with replacement) algorithm within a radius of 0.01 to match LPS and HPS women. In order to improve the quality of matching, we only consider observations with overlapping propensity scores (more than 99.5 % of the sample), i.e., those which belong to the common support. After matching, we check the balance of the covariates and reduction in bias across the two groups. The results are presented in Tables 3 and 4. We find that the raw percentage bias, which measures the difference in the average value of a covariate between unmatched LPS and HPS women, is reduced by a large amount after matching on estimated propensity scores. The mean biases in the two pre-JSY analysis subsamples reduce by 41 and 84 % respectively after matching, while the reduction in the post-JSY subsamples are 61 and 79 % respectively.
Additional tests of the quality of matching can be done following Sianesi (2004). If the matching quality is good, then the value of pseudo-R 2 after matching should be much lower than the pseudo-R 2 before matching. Results in Tables 3 and 4 show large reductions (by up to 90 %) in the pseudo-R 2 value from pre-matching to post-matching, indicating that our propensity score matching framework is valid.
6.3 Treatment effect results
Our main estimates of the impact of JSY are provided in Table 5. We present three sets of estimates—those from the raw data, PSM estimates using nearest-neighbor matching algorithm, and PSM estimates from an alternative five-nearest-neighbors matching algorithm (with replacement). In the first subsample of non-poor and non-SC/ST women from the border districts of LPS and HPS, we find that the raw DID rise in the probability of childbirth or pregnancy from pre-JSY to post-JSY is 2.5 percentage points (statistically significant at 5 % level) over a 3-year period. In comparison, the DID impact of JSY over the same period shows a significant 3.5 and 3.3 percentage point increase, respectively after nearest-neighbor and five-nearest-neighbors propensity score matching, from a pre-JSY childbirth probability of 29.1 %. In the second subsample of poor or SC/ST mothers from the border districts, we also find significant positive effects of JSY on the probability of at least one childbirth or pregnancy. The raw DID, PSM nearest-neighbor, and PSM five-nearest-neighbors DID estimates in this subsample are 1.4, 2.7, and 2.5 percentage point increases (all significant at 5 % level), respectively, from a pre-JSY childbirth probability of 37.2 %.
The magnitude of the impact of JSY in the two subsamples depends on several factors such as the relative size of the cash incentive, knowledge about the program among women, and program coverage rate. The non-poor and non-SC/ST mothers in LPS are eligible for a maximum of INR 1400 cash incentive under JSY (in comparison with no incentive in HPS), possibly resulting in a higher demand or uptake rate of the program. In comparison, for the poor or SC/ST women in LPS, the relative cash incentive is only up to INR 700 (i.e., INR 1400 benefit in LPS as compared with INR 700 benefit in HPS). Therefore, the differential effect of the program may be smaller among these women, as seen in our results. Furthermore, for poor (BPL) women delivering babies at home, the JSY incentive available to LPS and HPS women is an equal INR 500. Considering that poor women also generally have lower access to health facilities, if they choose to deliver babies at home even after JSY, there will likely be no differential fertility effect of the program in LPS. Finally, health workers in LPS areas can earn up to INR 600 for childbirth under JSY among the non-poor and non-SC/ST subpopulation, while health workers in HPS receive no incentive for such births. In comparison, for childbirth among the poor or SC/ST subsamples, health workers in both LPS and HPS can earn up to INR 600. Considering that health workers may be able to influence fertility decisions of couples, this may further explain the larger fertility effect of JSY in the non-poor and non-SC/ST subsample.
Knowledge about the program may also determine the fertility effect. While the pace of JSY implementation varied across districts, the official DLHS-3 report shows that by 2008, 79 % of women of reproductive age across India knew about the program, and 74 % of villages had access to it (IIPS 2014).Footnote 18 Availability of JSY reached over 90 % in rural areas of states such as Punjab, Rajasthan, West Bengal, Madhya Pradesh, Andhra Pradesh, and Kerala.
The longer-term effect of JSY on fertility would depend on uptake rates and administrative efficiency, including the success of women in actually obtaining the cash benefit. However, during the early years, the introduction of the program may trigger higher fertility rates in anticipation of the cash incentive. The incentive can be substantially large when compared with the standard of living in India. During 2007–2008, the median monthly per capita expenditure among rural Indian families was just INR 649, and among the poorest 10 % of families, it was less than INR 400 (MoSPI 2010). In comparison, the maximum possible JSY benefit of INR 1400 is indeed large. It is well known that credit constraints and the lack of robust social safety nets in India and other developing countries often lead to higher fertility rates among the poor (Cain 1981; Schultz 1993). Therefore, it is no surprise that the high availability of JSY and its large cash benefit can induce the fertility effects seen in our results. Our findings are similar to Stecklov et al. (2007) who find a 4.8 percentage point rise in fertility as an unintended consequence of a CCT in Honduras.
The rise in childbirth probability as a result of JSY is a remarkable finding. The low-performing states are characterized by worse socioeconomic outcomes and high initial fertility rates. The problem of high population growth may be exacerbated under JSY if the monetary incentive is inducing LPS couples to have additional children or is hastening their fertility decisions. The health workers implementing JSY may also persuade couples to have more children, since they themselves are entitled to cash incentives for institutional deliveries. They may be less enthusiastic about delivering family planning services.Footnote 19 The fertility effect of JSY echoes Stecklov et al. (2007) and Morris et al. (2004), who find an impeded demographic transition as a result of cash incentives in Honduras. If the rise in childbirth probability reflects a rise in the overall demand for fertility (i.e., over a mother’s lifetime), this finding is additionally important for India. The unintended demographic impact of JSY may present a conflict with the objectives of population control, especially in the high-fertility LPS states.Footnote 20 Since JSY is a new program, its utilization rates are yet to reach the optimal level. Therefore, with rise in uptake rates of JSY, the fertility effect may strengthen in the near future.
Alternatively, the rise in fertility may be a short-term phenomenon, and it may subside in the long run. In such as case, the unintended demographic expansion will not be a matter of concern. Also, our analysis cannot distinguish between a true rise in overall fertility demand and a hastening of the next fertility decision. It is possible that the perceived rise in childbirth probability is a result of couples reducing birth spacing in response to the cash incentive.Footnote 21 However, a reduction in the space between two consecutive births may be associated with higher neonatal mortality, or worse health outcomes for the second-born baby (Rutstein 2005; Conde-Agudelo et al. 2006; Dewey and Cohen 2007; Bhalotra and van Soest 2008). Therefore, the neonatal health gains from JSY (Lim et al. 2010)—which have been already challenged by Das et al. (2011) and Powell-Jackson et al. (2015)—may be much lower, or even negative.
6.4 Robustness check, sensitivity analysis, and heterogeneous treatment effects
We check the robustness of our results in three ways. First, we check the robustness of our underlying propensity score estimation technique and matching algorithms. We estimate the DID PSM effect of JSY using two alternative matching methods—local linear regression matching and Kernel matching. Then, we also replace the probit model of propensity score with a logit model, and re-estimate the effect under nearest-neighbor (with replacement and within 0.01 radius) and five-nearest-neighbors (with replacement) matching scenarios. In another alternative scenario, we use the original probit model of propensity score, but modify the regression specification by replacing all asset ownership and housing condition variables with binary indicators of five quintiles of the wealth index (as discussed in footnote 16). These scenarios allow us to test whether our results vary substantially across different model specifications.
A second type of robustness check involves testing if our results are dependent upon the choice of study periods. We repeat our PSM analysis with three more time periods. First, we consider births during 2005–2008 (from DLHS-3) in our post-JSY data and compare them with pre-JSY births during 2001–2004 (from DLHS-2). Then, we also compare the post-JSY period of 2006–2008 (from DLHS-3) separately with DLHS-2 data from pre-JSY periods 1999–2001 and 1996–1998.
As another robustness check, we use an alternative regression-based DID framework to evaluate the impact of JSY on childbirth probability.
for the ith woman in the dth district. t denotes the time periods 2001–2003 or 2006–2008. The outcome variable \( \mathrm{Birt}{\mathrm{h}}_{idt}=1 \) if the woman had at least one childbirth or pregnancy during period t, or 0 otherwise. \( \mathrm{P}\mathrm{o}\mathrm{s}{\mathrm{t}}_t=1 \) for the post-JSY period of 2006–2008 and 0 for the pre-JSY period of 2001–2006. \( \mathrm{J}\mathrm{S}{\mathrm{Y}}_d=1 \) for the LPS districts and 0 otherwise. The iid error term of the regression is \( {\epsilon}_{idt} \). \( X \) is the same set of time-varying explanatory variables which were used in the original propensity score estimation equation. It includes household, woman, and husband characteristics. In order to preserve sample size, household standard of living is captured by binary indicators of five quintiles of the wealth index (as discussed in footnote 14) instead of individual asset ownership and housing condition indicators. \( X \) also includes the number of children born to a woman prior to the study period, average distance from a village to the nearest town, and the share of villages in the district with at least one public health facility, at least one private health facility, an Anganwadi center and a dai. We use a linear probability model to estimate Eq. (9). The coefficient of the interaction between \( \mathrm{P}\mathrm{o}\mathrm{s}{\mathrm{t}}_t \) and \( \mathrm{J}\mathrm{S}{\mathrm{Y}}_d \) is the estimated DID effect of JSY on the fertility.
The results from robustness checks are presented in Tables 6, 7, and 8. In the first set of checks where we vary the underlying matching methods and propensity score models (Tables 6 and 7), the DID PSM effect of JSY remains statistically significant. The magnitude of the effect is similar to our original results, and in the range of 3.7–5.9 percentage points for the first subsample (non-poor and non-SC/ST), and 2.1–2.9 percentage points for the second subsample (poor or SC/ST). Results from the DID regression analysis (Eq. 9) are presented in the last row of Table 7. We find that JSY had a weakly significant positive effect of 1.4 percentage points in the first subsample but no impact on the second subsample. As discussed in Section 6.2, there are systematic differences between the treatment (strongly treated) and control (weakly treated) groups which might bias regression-based DID estimates. Therefore, it is not surprising that the effect of JSY is weaker in the regression model as compared with PSM.
Our results are also robust to the choice of time period (see Table 8). When comparing the 2005–2008 post-JSY data with 2001–2004 pre-JSY data, we find DID PSM effects of 2.9 (significant at 10 % level) and 3.4 (significant at 5 % level) percentage point increase in childbirth probability in the first and second subsamples respectively. If we choose years 1999–2001 as the pre-JSY period, the DID PSM effect of JSY is 5.4 and 3.6 percentage points (both significant at 5 % level) in the first and second subsamples respectively. If we further go back in time and choose 1996–1998 as the pre-JSY period, the DID PSM effect is 4.7 and 2.6 percentage points (both significant at 5 % level) in the two subsamples.
However, PSM only reduces the disparities in observable characteristics of LPS and HPS women. It may fail to incorporate any unobservable factors that are systematically different between the two groups of women. For example, the quality of the implementation of the program may be different across LPS and HPS, or HPS women may generally be better informed about government programs and thus more likely to participate in JSY. Matching on observable characteristics will not correct for such differences. Therefore, following Rosenbaum (2002) and Becker and Caliendo (2007), we calculate the Mantel-Haenszel (Mantel and Haenszel 1959) bounds to test the sensitivity of our main PSM estimators (i.e., probit model with nearest-neighbor matching) for any possible unobserved bias. We consider the odds of differential treatment assignment due to unobserved factors (Γ) over a range of 1–3 with 0.02 increments. Under the scenario of no hidden bias (Γ = 1), the Qmh statistic shows that the probability of childbirth is significantly higher among LPS women in both the non-poor and non-SC/ST subsample and the poor or SC/ST subsample. The bounds of the statistic are interpreted in the following way. If there exists positive selection bias, such that women who are likely to be eligible for JSY also have higher fertility rates even without treatment, then the Qmh statistic is too high and needs to be adjusted downward. On the other hand, in case of negative selection bias, the Qmh statistic is too low and needs to be adjusted upward. The statistics p + mh and p − mh indicate the significance levels for rejecting the null hypothesis of over- or under-estimation of Qmh.
Results from the sensitivity analysis are presented in Table 9. We find that the presence of unobservable factors do not affect our PSM estimates. Even with increasing odds of differential treatment assignment (i.e., higher values of Γ), the values of the p + mh and p − mh statistics remain very low, indicating that the effect of the treatment in the post-JSY data is not over- or under-estimated.
Due to lack of space, we do not present the results from covariate balancing and Mantel-Haenszel tests from the additional PSM models shown in Tables 6, 7, and 8. The outcomes of the balancing and sensitivity tests in these additional models are highly similar to the original nearest-neighbor PSM probit model.
Finally, we explore the possibility of heterogeneous treatment effects. We divide our two subsamples further by woman’s age (less than 20 years, 20–30 years, and 30 years and above), location (rural or urban), and educational attainment of the woman and her husband (less than grade 1, grades 1–5, grades 6–11, and grades 12 or above). We estimate the DID effect of JSY using the original probit PSM method (nearest-neighbor matching with replacement within a radius of 0.01) for each of these subgroups. However, in order to preserve sample size and reduce the dimensionality problem arising from a large number of asset ownership and housing condition variables in the probit model, we replace those covariates with the indicators of the five quintiles of the wealth index.
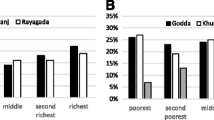
The results are presented in Table 10. We find that the positive effect of JSY on fertility is largest among women in the 20–30-year-old age group in the non-poor and non-SC/ST subsample. There is no significant effect of JSY for the same age group in the poor or SC/ST subsample, while women of age 30 years and above experience significantly positive fertility effects in both the subsamples. For rural women, the fertility effect is larger in the first subsample, while for urban women, it is the stronger in the second subsample. We also find that the effects are consistently bigger among uneducated (<grade 1) women and husbands, expect for women with grades 6–11 in the poor or SC/ST subsample, who experience a relatively larger fertility effect as compared with other educated women.
Before concluding, we should mention the possible limitations of our analysis. First, in the absence of long-term data, our analysis is only restricted to the post-JSY years of 2006–2008. It is difficult to predict whether the fertility effect of JSY will strengthen or subside in the medium to long run. As knowledge about JSY and its utilization increases with time, and the fertility effect may continue for a few years beyond our study period. On contrary, as the quantity-quality theory (Becker and Lewis 1973; Becker and Tomes 1976) suggests, with improvements in child quality (e.g., reduction in neonatal mortality as a result of JSY), fertility rates (quantity) may fall in the future. Alternatively, since JSY benefits are restricted to up to two births per woman in HPS, the relative fertility effect among LPS women may continue even in the longer run. This will also apply to the cash incentive separately received by JSY health workers in LPS. Not only their benefits are higher but they can earn them for longer since there is no restriction on the number of births per woman. If the health workers coerce couples into increasing fertility rates (or de-emphasize family planning services), the effect of JSY may continue in the future.
Second, the lack of long-term data also prevents us from effectively analyzing births and pregnancies separately. Since the two DLHS surveys were conducted over the years 2002–2004 and 2007–2008, which overlapped with our study periods of 2001–2003 and 2006–2008, respectively, a large number of women reported ongoing pregnancies. We find that if such pregnancies are excluded, the estimated fertility effect of JSY on childbirths is significantly weaker or nonexistent.
Third, our estimation techniques are internally valid, i.e., they produce reliable estimates of the effect of JSY on fertility rates among the two subsamples in the border districts of LPS and HPS. The impact of the program at the national level may be affected by the widespread regional disparities in socioeconomic indicators and access to healthcare. In addition, there is no information on the quality of the program, including the efficiency of cash payment process, coercion by health workers, leakages, fraud, and other irregularities across regions. Therefore, it is difficult to predict the external validity of our findings.
Fourth, an analysis of the unintended effects should also take into account the later life outcomes of the children born due to JSY. More children may lead to lower per capita availability of nutrition and healthcare resources in a household, thereby either increasing child mortality rates or reducing the levels of human development of children. Unfortunately, such longer-term analysis is beyond the scope of this study.
Finally, NRHM is an umbrella program which included other health policies in addition to JSY. For example, while ASHAs were introduced primarily for JSY, they were also given the responsibility of delivering immunization or other early childhood care in some areas. JSY is the only program under NRHM which could have a large fertility effect. However, if there is any small fertility or health impact from these other components of NRHM, we cannot capture that in our study.
7 Conclusion
JSY is one of the world’s largest conditional cash transfer schemes, with more than 11.3 million beneficiaries. With an expanding network of public health facilities in India, JSY appears to be a correct and timely tool that will encourage uptake of public healthcare. Although it is hampered by the poor quality of facilities for institutional births, JSY could potentially offer significant health and economic benefits where good-quality facilities are available.
However, policymakers must be aware of the possible unintended consequences of JSY, as shown in this paper. We used a policy variation arising from the differential incentive structure across two groups of states—poorer and initial-high-fertility states (LPS), and the rest of the country (HPS)—to study the potential unintended consequences of JSY on birth rates.
The results are very intriguing. The probability of childbirth among LPS mothers significantly increased by as much as 3.5 percentage points over a 3-year period. If the increased number of births post-JSY is a result of an increase in the lifetime demand for fertility (i.e., a couple’s desire to increase the size of the family, instead of simply moving the next fertility decision forward in time), this unintended effect of JSY will pose a conflict with the family planning objectives of the poorer states. This effect may even strengthen with increasing JSY utilization rates in the near future. However, this may also be a short-run phenomenon, and the fertility demand may stabilize in the longer run.
The rise in fertility also casts further doubts on the health gains from JSY. The validity of the reduction in mortality shown by Lim et al. (2010) has already been challenged by others. If there is indeed no such effect, then a reduction in birth spacing due to rising fertility rates may worsen child health outcomes. Longer-term studies will be necessary to ascertain the true health impact of JSY.
The fertility effect of JSY could be reduced by removing the threshold effect of the bulk cash payment at the time of delivery. For example, instead of providing INR 1400 as a one-time payment, it could be divided into a few small payments (e.g., not more than INR 200) that are delivered at each prenatal and postnatal care visit, child delivery, and immunization. Since 2013, the cash benefit of the ASHA or health worker has already been divided equally between prenatal and delivery care. The benefit for the pregnant woman should be divided in a similar manner. The program could also stipulate a minimum waiting period for the cash benefit between two consecutive eligible births of a woman. Finally, family planning policies could be strengthened further to normalize the demographic expansion created by JSY.
JSY is undoubtedly India’s most ambitious maternal and child health scheme. However, to unlock its full potential, supplementary healthcare infrastructure, continued evaluation, and evidence-based program modifications are required. In addition, the possibly damaging unintended consequences discussed in this paper should be considered at the policy-making stage.
Notes
For example, the infant mortality rates of India, Nepal, Bangladesh, and Sri Lanka were 47, 39, 37, and 11 per 1000 live births in 2011, respectively. Source: Level and Trends in Child Mortality. Report 2011. Estimates Developed by the UN Inter-agency Group for Child Estimation (UNICEF, WHO, World Bank, UN DESA, UNPD).
Source: MDGMonitor, United Nations Development Programme, http://www.mdgmonitor.org.
Assuming US$1 = INR 60, approximately. The annual budget of JSY in 2010–11 was INR 16.18 billion. INR = Indian rupees.
Randive et al. (2013) also find a positive association between JSY and institutional deliveries.
The phrases “low-performing states” and “high-performing states” are official JSY terms for describing these two groups of states.
See Hotz et al. (1993) for a review of the literature on economics of fertility. Del Boca (2002) finds that the availability of publicly funded child care increased fertility in Italy. Milligan (2005) finds that pronatalist tax benefits may have increased childbirth probability in Canada, while Laroque and Salanié (2013) estimate that child benefits might increase total fertility in France. Cohen et al. (2007) and Mörk et al. (2013) find similar effects of fiscal benefits on fertility in Israel and Sweden respectively.
The Honduran Programa de Asignación Familiar (PRAF-II) CCT provides two different cash incentives for schooling and health. One of them is a US$48 cash incentive, per person per year, provided for health care and nutrition of pregnant and nursing mothers, and young children (Moore 2008).
Except Jammu & Kashmir and Assam, the rest are EAG states.
Before 2013, the BPL women in HPS needed to be at least 19 years old to be eligible for JSY. This restriction has been now abolished.
In DLHS 2007–2008 data, 41, 12.9, and 19 % of villages in India had a primary health sub-center, a primary health center, and a private clinic, respectively. The availability of other types of facilities, such as community health center or private hospital, was even lower. The average distance from a village to a primary health center and a private clinic was 9 and 10 km respectively (IIPS 2014).
The state of Nagaland was not surveyed in DLHS-3.
Our results are robust to the inclusion of births during 2004 and 2005 in our analysis, as discussed later (also see Table 8).
In the absence of a below-poverty-line indicator in DLHS-2, we use an approximate measure for poverty. First, we use principal-component analysis to create an household-level wealth index following Filmer and Pritchett (2001). Only variables that are common to both DLHS rounds are considered in this index—for example, the possession of a radio, sewing machine, TV, bicycle, car, and so on—and indicators of housing condition such as construction quality, availability of toilets, sources of drinking water, and the type of cooking fuel used. Then, we consider households on or below the 30th percentile of the wealth index distribution, separately in DLHS-2 and DLHS-3, as approximately poor. For comparison, the national poverty headcount rate was 33.8 % in India in 2009 (Source: World Bank data, http://data.worldbank.org/indicator/SI.POV.RUHC?page=1, accessed May 5, 2015)
We use maps from the 2001 Indian census, and the GADM (http://gadm.org) database, to identify the districts along state borders. There are several extra districts in the DLHS-3 data. A new district in DLHS-3 was typically created by carving out from a parent district in DLHS-2. In such cases, we mapped the DLHS-3 district back to the parent district. However, one particular border district in DLHS-3, Mewat in the state of Haryana, was created from more than one parent DLHS-2 districts. We exclude these parent districts and Mewat from our analysis. Also excluded from analysis is the state of Nagaland which was surveyed in DLHS-2 but not in DLHS-3. Figures 1 and 2 in the appendix present the district maps.
For example, pregnant women may visit or temporarily live at their natal home for the purpose of childbirth. However, DLHS-3 data show that less than 1 % of pregnant women who reported receiving antenatal care did so at their natal homes, and only 3.75 % of the most recent child deliveries took place in natal homes.
17 We include 26 indicators of household asset ownership and housing condition in the pre-JSY (2001–2003) propensity score estimation, and 46 such indicators in the post-JSY (2006–2008) propensity score estimation. The difference is a result of DLHS-3 collecting data on more such indicators as compared with DLHS-2.
The availability of a dai may be associated with the rollout of JSY in a village. According to official JSY documents, traditional birth attendants are often trained and converted into ASHAs. Anganwadi centers operate under the Integrated Child Development Services (ICDS) of India, a large national program providing supplemental nutrition, immunization, health check-up and education, and preschool education to over 90 million women and children. See http://wcd.nic.in/icds.htm, accessed April 29, 2015.
Powell-Jackson et al. (2015) use a different way of estimating the coverage of JSY. They consider the proportion of women giving birth at a public facility who receive the cash benefit as an indicator of coverage. This method ignores births at accredited private health facilities. In addition, the inconsistencies in JSY uptake and usage data at the level of the mother from DLHS-3 have been already pointed out by Das et al. (2011).
Past experience from India’s coercive fertility control policy (abolished in 1996) show that minorities and the poor were disproportionately targeted by health workers seeking to meet contraceptive targets mandated by the government (Sangwan and Maru 1999). These groups may be similarly vulnerable to coercion by health workers under JSY.
One possible confounding factor for the fertility effect of JSY seen in our results is a change in the family planning policy. If the family planning policy was relaxed in LPS at the same time as the introduction of JSY, the effect of JSY will be overestimated. However, both the National Population Policy of 2000 and the Working Group on Population Stabilization for the Eleventh Year Plan (2007–2012) of India vigorously emphasized the need for family planning particularly in LPS states (GoI 2006). Therefore, any concurrent relaxation of family planning policies is highly unlikely.
In additional analyses, we examined the space between two most recent births during the study period for women with multiple births in the data. We do not find any statistically significant effect of JSY on birth spacing. This could be either due to the small sample size of women with multiple births during the 3-year study period, or an indication of JSY’s positive effect on total fertility. Powell-Jackson et al. (2015) also suggest that the fertility effect of JSY may not be temporary, as it increased with the program’s age. However, longer-term data are required for more research on such effect.
References
Abadie A, Imbens GW (2006) Large sample properties of matching estimators for average treatment effects. Econometrica 74:235–267
Arroyo CR, Zhang J (1997) Dynamic microeconomic models of fertility choice: a survey. J Popul Econ 10:23–65
Becker GS, Lewis HG (1973) On the interaction between the quantity and quality of children. J Polit Econ 81:S279–88
Becker GS, Tomes N (1976) Child endowments and the quantity and quality of children. J Polit Econ 84:S143–S162
Becker SO, Caliendo M (2007) Sensitivity analysis for average treatment effects. Stata J 7:71–83
Bhalotra S, van Soest A (2008) Birth-spacing, fertility and neonatal mortality in India: dynamics, frailty, and fecundity. J Econ 143:274–290
Cain M (1981) Risk and insurance: perspectives on fertility and agrarian change in India and Bangladesh. Popul Dev Rev 7:435–474
Cohen A, Dehejia R, Romanov D (2007) Do Financial Incentives Affect Fertility?
Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC (2006) Birth spacing and risk of adverse perinatal outcomes. J Am Med Assoc 295:1809–1823
Das A, Rao D, Hagopian A (2011) India’s Janani Suraksha Yojana: further review needed. Lancet 377:295–6
Dehejia RH, Wahba S (1999) Causal effects in nonexperimental studies: reevaluating the evaluation of training programs. J Am Stat Assoc 94:1053–1062
Del Boca D (2002) The effect of child care and part time opportunities on participation and fertility decisions in Italy. J Popul Econ 15:549–573
Dewey KG, Cohen RJ (2007) Does birth spacing affect maternal or child nutritional status? A systematic literature review. Matern Child Nutr 3:151–173
Filmer D, Pritchett LH (2001) Estimating wealth effects without expenditure data-or-tears: an application to educational enrollments in States of India. Demography 38:115–132
Fiszbein A, Schady N, Ferreira FHG et al (2009) Conditional cash transfers: reducing present and future poverty. The World Bank, Washington DC
GoI (2006) Report Of The Working Group On Population Stabilization For The Eleventh Five Year Plan (2007–2012). The Planning Commission, Government of India
Gopalan SS, Durairaj V (2012) Addressing maternal healthcare through demand side financial incentives: experience of Janani Suraksha Yojana program in India. BMC Heal Serv Res. doi:10.1186/1472-6963-12-319
Heckman JJ, Ichimura H, Todd PE (1997) Matching as an econometric evaluation estimator: evidence from evaluating a job training programme. Rev Econ Stud 64:605–654
Heckman JJ, Willis RJ (1976) Estimation of a stochastic model of reproduction an econometric approach. Household Production and Consumption. National Bureau of Economic Research, In, pp 99–146
Hotz VJ, Klerman JA, Willis RJ (1993) The economics of fertility in developed countries. In: Stark O (ed) Rosenzweig MR. Elsevier, Handbook of Population and Family Economics, pp 275–347
Hotz VJ, Miller RA (1984) The Economics of Family Planning. University of Chicago - Population Research Center
IIPS (2014) District Level Household and Facility Survey (DLHS-4), 2012–13. IIPS, International Institute of Population Sciences, Mumbai, India
Laroque G, Salanié B (2013) Identifying the response of fertility to financial incentives. J Appl Econ 29:314–332
Leung SF (1991) A stochastic dynamic analysis of parental sex preferences and fertility. Q J Econ 106:1063–1088
Lim SS, Dandona L, Hoisington JA et al (2010) India’s Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. Lancet 375:2009–2023
Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22:719–784
Milligan K (2005) Subsidizing the stork: new evidence on tax incentives and fertility. Rev Econ Stat 87:1–39
MoHFW (2012) Annual Report 2011–12: Ministry of Health and Family Welfare. Government of India, New Delhi, India
Moore C (2008) Assessing Honduras? CCT Programme PRAF, Programa de Asignación Familiar: Expected and Unexpected Realities. International Policy Centre for Inclusive Growth, Country Study 01/2008
Mörk E, Sjögren A, Svaleryd H (2013) Childcare costs and the demand for children—evidence from a nationwide reform. J Popul Econ 26:33–65
Morris SS, Flores R, Olinto P, Medina JM (2004) Monetary incentives in primary health care and effects on use and coverage of preventive health care interventions in rural Honduras: cluster randomised trial. Lancet 364:2030–7. doi:10.1016/S0140-6736(04)17515-6
MoSPI (2010) Household Consumer Expenditure in India, 2007–08. Government of India, New Delhi, India
Newman JL (1988) Research in Population Economics. In: Schultz TP (ed). JAI Press, London,
Powell-Jackson T, Mazumdar S, Mills A (2015) Financial incentives in health: new evidence from India’s Janani Suraksha Yojana. J Health Econ. doi:10.1016/j.jhealeco.2015.07.001
Randive B, Diwan V, Costa A (2013) india’s conditional cash transfer programme (the JSY) to promote institutional birth: is there an association between institutional birth proportion and maternal mortality? PLoS One 8:e67452
Rosenbaum PR (2002) Observational Studies, 2nd edn. Springer, New York
Rosenbaum PR, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70:41–55
Rosenzweig MR, Schultz TP (1985) The demand for and supply of births: fertility and its life cycle consequences. Am Econ Rev 75:992–1015
Rutstein SO (2005) Effects of preceding birth intervals on neonatal, infant and under-five years mortality and nutritional status in developing countries: evidence from the demographic and health surveys. Int J Gynecol Obstet 89:S7–S24
Sangwan N, Maru RM (1999) The target-free approach: an overview. J Health Manag 1:71–96
Schultz TP (1993) Demand for children in low income countries. Handbook of Population and Family Economics. Elsevier, In, pp 349–430
Sianesi B (2004) An evaluation of the swedish system of active labor market programs in the 1990s. Rev Econ Stat 86:133–155
Stecklov G, Winters P, Todd J, Regalia F (2007) Unintended effects of poverty programmes on childbearing in less developed countries: experimental evidence from Latin America. Popul Stud 61:125–140
Todd J, Winters P, Stecklov G (2011) Evaluating the impact of conditional cash transfer programs on fertility: the case of the Red de Proteccion Social in Nicaragua. J Popul Econ 25:267–290
UNFPA (2012) Trends in Maternal Mortality:1990–2010. United Nations Population Fund (with UNICEF, WHO, World Bank)
Wolpin KI (1984) An estimable dynamic stochastic model of fertility and child mortality. J Polit Econ 92:852–874
Acknowledgments
We thank the two anonymous reviewers for their very helpful comments, and Ashvin Ashok, Nikolay Braykov, and Nestor Mojica for their research assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible editor: Junsen Zhang
Rights and permissions
About this article
Cite this article
Nandi, A., Laxminarayan, R. The unintended effects of cash transfers on fertility: evidence from the Safe Motherhood Scheme in India. J Popul Econ 29, 457–491 (2016). https://doi.org/10.1007/s00148-015-0576-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00148-015-0576-6