Abstract
Purpose
One potential way to protect patients from the physiological demands that are a consequence of fever is to aim to prevent fever and to treat it assiduously when it occurs. Our primary hypothesis was that more active fever management would increase survival among patient subgroups with limited physiological reserves such as older patients, patients with higher illness acuity, and those requiring organ support.
Methods
We conducted an individual-level patient data meta-analysis of randomised controlled trials to compare the outcomes of ICU patients who received more active fever management with the outcomes of patients who received less active fever management. The primary outcome variable of interest was the unadjusted time to death after randomisation.
Results
Of 1413 trial participants, 707 were assigned to more active fever management and 706 were assigned to less active fever management. There was no statistically significant heterogeneity in the effect of more active compared with less active fever management on survival in any of the pre-specified subgroups that were chosen to identify patients with limited physiological reserves. Overall, more active fever management did not result in a statistically significant difference in survival time compared with less active fever management [hazard ratio 0.91; (95% CI 0.75–1.10), P = 0.32].
Conclusions
Our findings do not support the hypothesis that more active fever management increases survival compared with less active fever management overall or in patients with limited physiological reserves.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
We conducted an individual level patient data meta-analysis of randomised controlled trials to compare the outcomes of ICU patients who received more active fever management with the outcomes of patients who received less active fever management. Our findings do not support the hypothesis that more active fever management increases survival compared with less active fever management overall, or in patients with limited physiological reserves. |
Introduction
Fever occurs commonly in intensive care (ICU) patients and increases metabolic demand [1]. Increasing metabolic demand has important physiological consequences on oxygen consumption and cardiac output [1]. One potential way to protect patients from the physiological demands that are a consequence of fever is to aim to prevent fever and to treat it assiduously when it develops [2]. This strategy is an attractive candidate intervention to improve outcomes in the ICU setting because patients with a range of critical illnesses including major trauma, infection, acute myocardial infarction, and pancreatitis develop fever [3,4,5], and many such patients have limited physiological reserves.
Body temperature can be manipulated in ICU patients with medicines [6, 7] and physical cooling devices [8] allowing for more or less active approaches to fever management. In a recent systematic review and aggregate data meta-analysis evaluating the effect of fever management on all-cause mortality in ICU patients, we found that more active fever management neither increased nor decreased mortality in critically ill adults compared with less active fever management [9]. However, despite these findings, it is plausible that the balance of risks and benefits of active fever management in ICU patients varies based on the physiological reserves of the patients being treated and the nature of their illness [10]. In this context, we submit that physiological reserves are reasonably defined as the capacity of a patient to cope with the physiological demands associated with fever and depend on patients’ physiology, illness severity, and the organ support they require.
Our primary hypothesis was that more active fever management would increase survival among patient subgroups with limited physiological reserves such as older patients, patients with higher illness acuity, and those with very high body temperature (≥ 39.5 °C). Because fever is part of the adaptive host response to infection [11], we further hypothesised that more active fever management would improve survival in the absence of infection but not in the presence of infection.
Methods
Study design
To address our hypotheses, we conducted an individual-level patient data meta-analysis (IPDMA) using available data from randomised controlled trials identified in our recent systematic review and aggregate data meta-analysis [9]. We contacted lead investigators for all randomised controlled trials identified in the recent systematic review and requested access to individual patient-level data (see ESM for details). The search strategy used in our systematic review has been published previously [9]; however, in brief, we searched major databases for randomised controlled trials evaluating fever management in adult ICU patients excluding trials where the intervention involved therapeutic hypothermia. We included trials that evaluated any treatment administered commonly to febrile patients to reduce body temperature. The protocol for this IPDMA was posted online on 29 June 2018 at http://wellingtonicu.com/PubResPres/Protocols/ in advance of analyses being undertaken.
Data extraction and cleaning for analysis
Pre-randomisation (baseline) data points were extracted from individual study databases. These were age, gender, invasively ventilated (yes or no), receiving inotropes and/or vasopressors at baseline (yes or no), suspected infection at baseline (yes or no), Acute Physiology And Chronic Health Evaluation (APACHE) II score [12], mean arterial pressure (mmHg), heart rate (beats per min), serum creatinine (µmol/l), and body temperature (°C).
We sought to compare the outcomes of patients who received more active fever management with the outcomes of patients who received less active fever management. Accordingly, where studies compared an antipyretic drug with placebo, the patients allocated to the antipyretic drug were considered to have received more active fever management. Where studies compared different thresholds for temperature treatment, patients allocated to the group with the lowest body temperature target were considered to have received more active fever management.
Time to death after randomisation was defined as the difference between time zero (T0) and the date and time of death. T0 was generally defined as the date and time of randomisation. In one study, where the date and time of randomisation were not recorded, the date and time of administration of the first dose of study medication defined T0. Where no time, only a date, was available to define either T0 or the time of death, the time(s) were be assumed to be 12:00 p.m. The time for censored participants (those who did not die) was defined as the last time of observation in relation to the time of randomisation as described above. All patients who died on or before the date of ICU discharge were defined as dead for the purposes of evaluating the end point ‘mortality at ICU discharge’. ICU and hospital length of stay were defined as the difference between T0 as described above and ICU and hospital discharge, respectively. Where no time, only a date, was available to define either T0 or the time of discharge, the time(s) were assumed to be 12:00 p.m. Body temperature at 6, 12, 24, 48, and 72 h after randomisation were included in the IPDMA database. One study reported temperature data at 4 h and 8 h after randomisation [7]. For this study, the 6-h temperature data point was calculated by averaging the values from the 4–8 h time points.
Outcomes
The primary outcome variable of interest was the time to death after randomisation. This outcome was chosen as the primary outcome because it allowed multiple trials with different durations of follow-up to be combined without loss of data. Secondary outcomes were mortality at ICU discharge, ICU and hospital length of stay, and body temperature at 6, 12, 24, 48, and 72 h following randomisation.
Statistical analyses
Data summaries by treatment group are frequency and proportions expressed as percentages for categorical data and mean ± standard deviation for continuous data.
Survival times use log-rank tests and are shown as Kaplan-Meier curves and relative survival estimated with a Cox proportional-hazards model. The primary analysis model was adjusted for study as fixed effect; however, a sensitivity analysis adjusted for baseline covariates of age, sex, and APACHE-II score was also performed incorporating individual study as a fixed effect. Because the APACHE-II score was not available for one study [8] two post hoc sensitivity analyses were used: one in which the APACHE-II score was not included in the adjusted model and another in which illness severity scores based on Simplified Acute Physiology Score (SAPS3) [13] were used in place of APACHE-II scores for the study that did not include APACHE-II data (see ESM for details).
ICU mortality was compared by treatment group using logistic regression with analyses performed in a similar fashion to those performed for survival. Mortality data by treatment group are reported as frequencies with proportions expressed as percentages with treatment effects reported as odds ratios.
ICU and hospital length of stay were highly skewed and were analysed on the logarithm transformed scale. These variables are summarised as geometric mean with treatment effects expressed as a ratio of geometric means. A post hoc analysis evaluating whether ICU length of stay differed in relation to randomised treatment for patients who did or did not die in the ICU used an ANCOVA-based interaction model.
Interaction analyses were also used to explore whether survival, ICU mortality, ICU length of stay, or hospital length of stay varied in pre-specified subgroups based on pre-randomisation characteristics. The subgroups of interest were: invasively ventilated or not; receiving inotropes and/or vasopressors or not; both invasively ventilated and receiving inotropes and/or vasopressors or not; infection present or not; high fever (≥ 39.5 °C or < 39.5 °C); age (≥ 75 years or < 75 years); APACHE-II score ≥ 25 or < 25; and physical cooling included in the study intervention or physical cooling not included in the study intervention.
Temperature was analysed using a mixed linear model with a power exponential structure for the correlation between repeated measurements and the time by randomisation interaction term used to estimate temperature differences between randomised treatments at each time point.
A two-sided P value < 0.05 was considered to indicate statistical significance and estimates are shown with 95% confidence intervals (CI). No adjustment was made for multiple comparisons.
SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) was used for analyses.
Results
Data sources
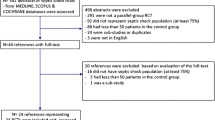
Individual-level patient data were obtained for 5 [6,7,8, 14, 15] of 13 randomised controlled trials identified in the systematic review conducted for our aggregate data meta-analysis [9]. This included the three largest trials [6,7,8] and resulted in data from 1413 of 1780 (79.4%) of the participants in the original trials being included in this analysis. Details of included trials and those trials from which data could not be obtained are shown in the ESM.
Patient characteristics
Of the 1413 participants included in this analysis, 707 were assigned to more active fever management and 706 were assigned to less active fever management. The study groups had similar characteristics at baseline (Table 1). More than 95% of participants were suspected to have an infection at baseline.
Effects of fever management on body temperature
Patients assigned to more active fever management had statistically significantly lower body temperature than patients assigned to less active fever management (Fig. 1). The effect of study treatment on body temperature varied with time with a maximum temperature difference of 0.73 °C (95% CI 0.63–0.83 °C) between temperature groups evident at 12 h post randomisation.
Body temperature over time with more active fever management vs. less active fever management. *P value for the interaction term evaluating temperature difference by time from randomisation was < 0.001 indicating a statistically significant variation in the temperature difference by treatment over time
Survival and mortality
In the analysis addressing the primary hypothesis that more active fever management would increase survival among patient subgroups with limited physiological reserves such as older patients, patients with higher illness acuity, and those requiring organ support, we found no statistically significant heterogeneity of treatment effect in any of the pre-specified subgroups (Fig. 2). Similarly, there was no heterogeneity of survival response by treatment allocation in patients with and without infections (Fig. 2). Overall, more active fever management did not result in a statistically significant difference in survival time compared with less active fever management [hazard ratio; 0.91; (95% CI 0.75–1.10), P = 0.32] (Table 2, Fig. 3, Fig. S1 ESM). Findings were similar in analyses adjusting for pre-specified baseline covariates (Table 2 and Fig. 3) and in sensitivity analyses (ESM). Moreover, the estimates of the hazard ratios related to survival from the sensitivity analyses were more-or-less identical treating the studies as fixed effects (as was pre-specified) or as random effects.
Kaplan-Meier survival estimates of the probability of survival. Because the number of observations beyond day 90 is small, this figure is truncated at day 90 with data censored at day 90 if death had not occurred by then. An expanded Kaplan-Meier survival plot including all available data points is provided with the electronic supplementary material
There was no statistically significant heterogeneity in the effect of more active compared with less active fever management on ICU mortality in any of the pre-specified subgroups (Fig. 4). A total of 98 of 707 patients (13.9%) assigned to more active fever management and 121 of 706 patients (17.1%) assigned to less active fever management died in the ICU [absolute mortality difference, − 3.3% points (95% CI − 7.1 to 0.5% points); odds ratio, 0.78 (95% CI 0.58–1.04), P = 0.09] (Table 2). Findings were similar in analyses adjusting for pre-specified baseline covariates (Table 2) and in sensitivity analyses (ESM).
Length of stay
Overall, ICU length of stay and hospital length of stay were similar between treatment groups (Table 2). However, there was statistically significant heterogeneity of response to treatment in relation to length of stay variables in some subgroups (Fig. 5 and Fig. S2, ESM). In each case where significant heterogeneity in response to treatment was observed, the length of stay was statistically significantly shorter in a subgroup where the point estimate for ICU mortality risk favoured more active fever management. In a post hoc interaction analysis of ICU and hospital length of stay by treatment allocation, there was statistically significant heterogeneity in response in survivors compared with non-survivors (ESM). Compared with less active fever management, more active fever management was associated with longer ICU and hospital length of stay in patients who died in ICU and with shorter ICU and hospital length of stay in patients who survived ICU.
ICU length of stay with more active fever management vs. less active fever management by subgroup. *Unadjusted P value for overall comparison, 0.92; P value adjusted for age, sex, study, and APACHE-II score (excluding Schortgen et al. trial), 0.52; P value adjusted for age, sex, study, and APACHE-II score (including Schortgen et al. trial with SAPS III data from that trial rescaled to give the same range as APACHE-II data), 0.29; P value adjusted for age, sex, and study, 0.94
Discussion
In this individual-level patient data meta-analysis of randomised controlled trials, more active fever management did not increase survival compared with less active fever management in critically ill adults either overall or in those with limited physiological reserves. Survival by treatment group was similar in a range of subgroup pairs that divided the study population into groups based on age, illness severity, on receipt of specific organ supports, and in the presence or absence of high fever at baseline.
Overall, effect size estimates in relation to ICU mortality based on the 95% CI were consistent with an absolute effect on ICU mortality with active fever management ranging from a decrease of 7.1% points to an increase of 0.5% points. Although we observed statistically significant heterogeneity of treatment effect in relation to ICU and hospital length of stay effects, the interpretation of these findings is complicated because length of stay can be reduced by more rapid recovery or by early death. Moreover, a reduction in mortality, even a non-statistically significant one, can be associated with a statistically significant increase in length of stay when survivors have longer average lengths of stay than non-survivors. In patients who were receiving invasive mechanical ventilation, those receiving inotropes and/or vasopressors, or those receiving both of these, a relative increase in hospital length of stay was associated with lower ICU mortality based on point estimates. We also found that, compared with less active temperature management, more active temperature was associated with reduced ICU and hospital length of stay in patients who survived ICU and with increased length of stay in patients who died in ICU.
Our study is consistent with two recent aggregate data metaanalyses [9, 16] evaluating fever control in adult ICU patients; however, it extends their findings because the use of individual-level patient data allowed us to conduct analyses adjusting for important baseline covariates and to accurately evaluate subgroups of interest defined based on pre-randomisation characteristics.
Our study has a number of limitations. Because our analyses were not adjusted for multiple comparisons, they should be considered exploratory and should not be used to infer definitive treatment effects. Although we did not demonstrate statistically significant heterogeneity of treatment effect on survival for subgroups of interest, confidence intervals around hazard ratios were generally wide and the possibility of clinically important differences in survival responses by subgroup cannot be excluded. In particular, as nearly all patients were suspected of having an infection at baseline, our findings effectively neither confirm nor refute the hypothesis that the presence of infection is an important factor in determining the efficacy of active fever management [17]. We were only able to obtain data from 5 out of 13 trials identified in our recent systematic review. However, the three largest trials [6,7,8] conducted were included in our analysis and 79.4% of all potential data from prior randomised controlled trials were analysed. Most of the studies where data were not available were small single-centre studies. The studies included in our analysis used a variety of different therapies and it is not known whether these therapies have equivalent effects on patient outcomes. Nevertheless, as all therapies evaluated are given to patients to treat fever, we submit that combining trials in an IPDMA has both face validity and clinical relevance.
In conclusion, our findings do not support the hypothesis that more active fever management increases survival compared with less active fever management in patients with limited physiological reserves. However, as point estimates for the effect of active fever management on ICU mortality encompass potentially clinically important effects, further clinical trials are justified. The significant heterogeneity in treatment effects on length of stay in subgroups based on the receipt of organ support, combined with the finding that more active fever management increases ICU and hospital length in patients who die in ICU, and reduces length of stay in patient who survive ICU, suggests that further research in patients receiving organ support may be of interest.
References
Golding R, Taylor D, Gardner H, Wilkinson JN (2016) Targeted temperature management in intensive care—do we let nature take its course? JICS 17:154–159
Manthous CA, Hall JB, Olson D, Singh M, Chatila W, Pohlman A, Kushner R, Schmidt GA, Wood LD (1995) Effect of cooling on oxygen consumption in febrile critically ill patients. Am J Respir Crit Care Med 151:10–14
Laupland KB, Shahpori R, Kirkpatrick AW, Ross T, Gregson DB, Stelfox HT (2008) Occurrence and outcome of fever in critically ill adults. Crit Care Med 36:1531–1535
Laupland KB, Zahar JR, Adrie C, Schwebel C, Goldgran-Toledano D, Azoulay E, Garrouste-Orgeas M, Cohen Y, Jamali S, Souweine B, Darmon M, Timsit JF (2012) Determinants of temperature abnormalities and influence on outcome of critical illness. Crit Care Med 40:145–151
Niven DJ, Stelfox HT, Shahpori R, Laupland KB (2013) Fever in adult ICUs: an interrupted time series analysis. Crit Care Med 41:1863–1869
Young P, Saxena M, Bellomo R, Freebairn R, Hammond N, van Haren F, Holliday M, Henderson S, Mackle D, McArthur C, McGuinness S, Myburgh J, Weatherall M, Webb S, Beasley R (2015) Acetaminophen for fever in critically ill patients with suspected infection. N Engl J Med 373:2215–2224
Bernard GR, Wheeler AP, Russell JA, Schein R, Summer WR, Steinberg KP, Fulkerson WJ, Wright PE, Christman BW, Dupont WD, Higgins SB, Swindell BB (1997) The effects of ibuprofen on the physiology and survival of patients with sepsis. The Ibuprofen in Sepsis Study Group. N Engl J Med 336:912–918
Schortgen F, Clabault K, Katsahian S, Devaquet J, Mercat A, Deye N, Dellamonica J, Bouadma L, Cook F, Beji O, Brun-Buisson C, Lemaire F, Brochard L (2012) Fever control using external cooling in septic shock: a randomized controlled trial. Am J Respir Crit Care Med 185:1088–1095
Dallimore J, Ebmeier S, Thayabaran D, Bellomo R, Bernard G, Schortgen F, Saxena M, Beasley R, Weatherall M, Young P (2018) Effect of active temperature management on mortality in intensive care unit patients. Crit Care Resusc 20:150–163
Young PJ, Nielsen N, Saxena M (2017) Fever control. Intensive Care Med 44:227–230
Young PJ, Saxena M (2014) Fever management in intensive care patients with infections. Crit Care 18:206
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Metnitz PG, Moreno RP, Almeida E, Jordan B, Bauer P, Campos RA, Iapichino G, Edbrooke D, Capuzzo M, Le Gall JR (2005) SAPS 3—from evaluation of the patient to evaluation of the intensive care unit. Part 1: Objectives, methods and cohort description. Intensive Care Med 31:1336–1344
Niven DJ, Stelfox HT, Leger C, Kubes P, Laupland KB (2013) Assessment of the safety and feasibility of administering antipyretic therapy in critically ill adults: a pilot randomized clinical trial. J Crit Care 28:296–302
Saxena MK, Taylor C, Billot L, Bompoint S, Gowardman J, Roberts JA, Lipman J, Myburgh J (2015) The effect of paracetamol on core body temperature in acute traumatic brain injury: a randomised, controlled clinical trial. PLoS One 10:e0144740
Drewry AM, Ablordeppey EA, Murray ET, Stoll CRT, Izadi SR, Dalton CM, Hardi AC, Fowler SA, Fuller BM, Colditz GA (2017) Antipyretic therapy in critically ill septic patients: a systematic review and meta-analysis. Crit Care Med 45:806–813
Young PJ, Saxena M, Beasley R, Bellomo R, Bailey M, Pilcher D, Finfer S, Harrison D, Myburgh J, Rowan K (2012) Early peak temperature and mortality in critically ill patients with or without infection. Intensive Care Med 38:437–444
Acknowledgements
This research was conducted during the tenure of a Clinical Practitioner Research Fellowship from the Health Research Council of New Zealand held by PY. The Medical Research Institute of New Zealand is supported by independent research organisation funding from the Health Research Council of New Zealand.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Paul Young and Dr. Manoj Saxena report receiving speaker’s fees from Bard Medical Pty. Dr. Gordon Bernard reports having an equity stake and is on the Board of Directors for Cumberland Pharmaceuticals, Nashville, TN, makers of intravenous ibuprofen (Caldolor).
Ethical approval
An approval by an ethics committee was not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Young, P.J., Bellomo, R., Bernard, G.R. et al. Fever control in critically ill adults. An individual patient data meta-analysis of randomised controlled trials. Intensive Care Med 45, 468–476 (2019). https://doi.org/10.1007/s00134-019-05553-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-019-05553-w