Abstract
Purpose
To assess the relative importance of host and bacterial factors associated with hospital mortality in patients admitted to the intensive care unit (ICU) for pneumococcal community-acquired pneumonia (PCAP).
Methods
Immunocompetent Caucasian ICU patients with PCAP documented by cultures and/or pneumococcal urinary antigen (UAg Sp) test were included in this multicenter prospective study between 2008 and 2012. All pneumococcal strains were serotyped. Logistic regression analyses were performed to identify risk factors for hospital mortality.
Results
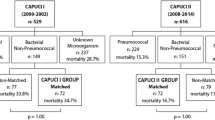
Of the 614 patients, 278 (45%) had septic shock, 270 (44%) had bacteremia, 307 (50%) required mechanical ventilation at admission, and 161 (26%) had a diagnosis based only on the UAg Sp test. No strains were penicillin-resistant, but 23% had decreased susceptibility. Of the 36 serotypes identified, 7 accounted for 72% of the isolates, with different distributions according to age. Although antibiotics were consistently appropriate and were started within 6 h after admission in 454 (74%) patients, 116 (18.9%) patients died. Independent predictors of hospital mortality in the adjusted analysis were platelets ≤ 100 × 109/L (OR, 7.7; 95% CI, 2.8–21.1), McCabe score ≥ 2 (4.58; 1.61–13), age > 65 years (2.92; 1.49–5.74), lactates > 4 mmol/L (2.41; 1.27–4.56), male gender and septic shock (2.23; 1.30–3.83 for each), invasive mechanical ventilation (1.78; 1–3.19), and bilateral pneumonia (1.59; 1.02–2.47). Women with platelets ≤ 100 × 109/L had the highest mortality risk (adjusted OR, 7.7; 2.8–21).
Conclusions
In critically ill patients with PCAP, age, gender, and organ failures at ICU admission were more strongly associated with hospital mortality than were comorbidities. Neither pneumococcal serotype nor antibiotic regimen was associated with hospital mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In immunocompetent Caucasian patients critically ill with pneumococcal pneumonia, mortality was high (18.9%). Age, gender, and organ failures at admission were more closely associated with mortality than were comorbidities, pneumococcal serotypes, and antibiotic regimens |
Introduction
Severe community-acquired pneumonia (CAP) is the most common infection requiring intensive care unit (ICU) admission and the leading cause of death from infection in Western countries [1]. Streptococcus pneumoniae is the main cause of severe CAP managed in the ICU, with 30% of microbiologically documented cases in adults [2]. Given the increased frequency of pneumococcal CAP (PCAP) with advancing age, the burden of severe PCAP can be expected to increase in the near future [3]. Despite the availability of antibiotics effective against S. pneumoniae and early ICU admission to treat organ failures, severe PCAP remains associated with high mortality rates of 15–30% [4,5,6,7].
The outcome of severe PCAP managed in the ICU depends on multiple factors including patient characteristics, pneumococcal serotype, the impact of sepsis-related organ failures, and the management strategy [8,9,10]. These factors interact with many confounders, making it difficult to determine the relative contribution of each [5, 11, 12].
The primary objective of this study was to assess the relative contributions of various factors to the outcome of severe PCAP in patients managed in French ICUs. We performed a multicenter prospective cohort study in a uniform population of immunocompetent Caucasian adults treated between 2008 and 2012. We assessed the strengths of the associations of various factors—including patient characteristics, pneumococcal serotypes, and antibiotic regimens—with hospital mortality. Our secondary objective was to obtain epidemiological and microbiological data on severe PCAP.
Materials and methods
Study design
Consecutive immunocompetent Caucasians older than 18 years and admitted to multiple French ICUs in university- and nonuniversity-affiliated hospitals between 2008 and 2012 for PCAP were included in a prospective observational study. The study sponsor registered the study database with the French Data Protection Authority (Commission Nationale Informatique et Liberté, ENRCNIL 909234). The study project was approved by the appropriate ethics committee (Comité de Protection des Personnes d’Ile de France, September 9, 2008, #2008/36NICB). Each investigator undertook to conduct the study in compliance with Good Clinical Practice guidelines and with the 1964 Declaration of Helsinki and its amendments. Written informed consent was obtained before study inclusion from patients who were competent. For patients who were not competent, written informed consent was obtained from the next-of-kin then from the patients as soon as they regained competence.
Inclusion and exclusion criteria
Patients were first screened for eligibility based on the following criteria: age ≥ 18 years, Caucasian, ICU admission for CAP, and criteria for severe CAP requiring ICU admission. S. pneumoniae CAP was defined as the presence at hospital admission or within the next 48 h of acute respiratory manifestations with a new radiological infiltrate of unknown cause combined with a positive urinary S. pneumoniae antigen test (UAg Sp; in the absence of documented pneumococcal pneumonia within the past 2 months and of pneumococcal immunization within the last 2 weeks) and/or with a sputum smear, tracheal aspirate (containing < 10 epithelial cells and > 25 neutrophils per × 10 field), distal protected airway specimen, or pleural aspirate showing Gram-positive diplococci. Criteria for severe CAP requiring ICU admission were those defined by the American Thoracic Society [13], i.e., at least one of two major criteria [invasive mechanical ventilation (IMV) or septic shock] or at least three minor criteria among the following: respiratory rate > 30/min; PaO2/FiO2 < 250 or non-invasive ventilation (NIV); multilobar infiltrates; confusion or disorientation; blood urea nitrogen > 7 mmoL/L; leukocytes < 4000/mm3; platelets < 100,000 mm3; body temperature < 36°; hypotension requiring fluid repletion; metabolic acidosis; and high serum lactate level.
Eligible patients were definitely included if S. pneumoniae infection was diagnosed based on the presence of any of the following: positive UAg Sp and/or positive S. pneumoniae culture of blood or pulmonary specimens.
Exclusion criteria were non-Caucasian ethnicity, pneumococcal pneumonia related to healthcare or with onset more than 72 h after hospital admission, aspiration pneumonia in a comatose or trauma patient, and immunodeficiency (asplenia or splenectomy; chemotherapy, hematological malignancy within the past 6 months and not in complete remission, solid-organ or bone marrow transplant; neutrophils < 1000/mm3 before the infection, HIV infection, Child C cirrhosis of the liver, or immunoglobulin deficiency).
Data collection
For each patient, the study data were recorded in an electronic case-report form. Demographic, epidemiological, clinical, bacteriological, laboratory and imaging data were collected prospectively upon admission and during the ICU stay. Details are reported in Electronic Supplementary Material (ESM1). We also recorded previous pneumococcal vaccination with the polysaccharide 23-valent vaccine, pre-admission exposure to antibiotics, time from hospital admission to the first dose of anti-pneumococcal antibiotic, and the nature of the antibiotics given in the ICU.
All patients were followed up until death or hospital discharge. The causes of death were recorded. After ICU discharge, patients were managed as deemed suitable by the ward physicians, who complied with French recommendations [14].
Microbiology
Susceptibility testing was performed at the French National Reference Centre for Pneumococci (FNRCP). Susceptibility to penicillin G, amoxicillin, cefotaxime, and levofloxacin was determined using the agar dilution method and susceptibility to erythromycin using the disk diffusion method. In addition, the norfloxacin screen test was used according to the European Committee on Antimicrobial Susceptibility Testing (EUCAST) [15] in order to successfully discriminate wild-type pneumococcal strains from those with any acquired mechanism of resistance to fluoroquinolones [16]. The results were interpreted according to EUCAST breakpoints [15]. Antibiotics given to treat PCAP were classified as appropriate if one or more empirical antibiotics had in vitro activity against the S. pneumoniae strain and adequate if the antibiotic had in vitro activity and was given in recommended dosage with timing of administration < 6 h. Serotyping was performed at the FNRCP with use of latex particles sensitized with pool, group, type and factor antisera provided by the Statens Serum Institut (Copenhagen, Denmark). This panel of antisera enabled recognition of 92 known serotypes. Pneumococcal strains with known serotypes from the Statens Serum Institute and from the CNRP collection were used as internal quality controls [17].
Statistical analysis
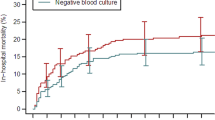
The statistical methods are detailed in the Electronic Supplementary Material (ESM2). The primary outcome was hospital mortality. The probability of hospital mortality was estimated using the cumulative incidence function estimator [18], with discharge alive as a competing risk.
Marginal associations between single variables and hospital mortality were assessed by applying Wilcoxon’s rank-sum test for quantitative variables and Fisher’s exact test for categorical variables. Some of the continuous variables were categorized according to predefined cut-offs. Variables independently associated with hospital mortality were identified by multiple logistic regression using a backward stepwise selection procedure, with P value cutoffs of 0.20 and 0.10 for considering and retaining variables, respectively. First-order interactions between selected variables were then tested. Missing data were handled through multiple imputation. Results were pooled over imputed datasets. Model performance was evaluated based on the concordance (c) index and calibration curve. As internal model validation, the final model parameters and performance were corrected for over-optimism using bootstrapping. Results of the final model are reported as odds ratios (ORs) with their 95% confidence intervals (95% CIs). In addition, a nomogram for predicting the patient-specific probability of hospital death was created.
Potential associations between pneumococcal serotypes and hospital mortality were assessed in the subgroup of patients with microbiologically documented PCAP. Individual associations were determined for the serotypes found in at least ten patients, using serotype 3 as the reference, since a strong association of serotype 3 with high mortality in adults has been reported [19]. Serotypes were then grouped according to their potential for causing invasive disease, as previously described [20,21,22,23], and their case fatality rate was determined for each group as previously reported [24, 25]. To estimate the invasiveness of serotypes for which no published data were available, invasive isolates in our patients were compared to a previously characterized sample of S. pneumoniae isolated during the study period from healthy carriers younger than 5 years of age [20].
Both unadjusted analyses and analyses adjusted on variables independent from the pathogen (age, gender, body mass index (BMI), McCabe score, and Charlson score) were performed. When no event or a single event occurred in a category, exact logistic regression was used, and the category was excluded from the adjusted analyses.
All tests were two-sided, and analyses were performed using R statistical software version 3.0.1 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Patients
We prospectively included 614 patients, including 377 (61%) males admitted to 51 French ICUs between December 2008 and February 2012. Table 1 shows that several features differed significantly across age groups. As expected, a large proportion of patients (45.1%) were older than 65 years. The Fine score, median Sepsis-Related Organ Failure (SOFA) score, and median Simplified Acute Physiology Score version II (SAPSII) indicated that most patients had severe acute illness. Most patients met major IDSA/ATS criteria for severe CAP and many patients had multiple comorbidities (ESM 3) only 2% of patients received previous pneumococcal vaccination with the polysaccharide 23-valent vaccine.
Antibiotic susceptibility and treatment
Of the 614 patients, 449 (73.1%) had positive cultures for S. pneumoniae and 270 (44%) had bacteremia. The diagnosis relied solely on the UAg Sp in 161 (26.2%) patients (Table 1). Susceptibility testing and serotyping were performed for 349 isolates, of which 56.7% were from blood, 40.9% from lung specimens, and 2.3% from pleural fluid. Of these 349 isolates, 5 were not viable and 5 were not S. pneumoniae strains, leaving 339 isolates for the study. Of these, 23.3, 10.0, and 2.9% exhibited decreased susceptibility to penicillin, amoxicillin, or cefotaxime, respectively. No strain was resistant to any of these antibiotics. Resistance to erythromycin was noted for 24.5% of strains and to levofloxacin for 2 (0.6%) strains. In addition, among levofloxacin-susceptible strains, one (0.3%) was detected as a topoisomerase IV first-step mutant. The proportion of isolates with a decreased susceptibility to beta-lactams declined over the 3-year study period (Electronic Supplementary Material 4).
Mean time from hospital admission to the first antibiotic dose was 6.8 ± 5.5 h (Table 1). The antibiotics were appropriate in all patients and adequate in 63.3% of patients. A beta-lactam active against S. pneumoniae was used alone in 22.6% of patients, with a macrolide in 36.3% of patients, and with a fluoroquinolone in 34.2% of patients (Electronic Supplementary Material 5).
Serotypes
Of the 36 capsular serotypes identified (Fig. 1), serotype 3 was the most common (23.9% of isolates), followed by serotypes 7F, 19A, 12F, 1, 6C, and 11A. These seven serotypes, each found for over 10 isolates, accounted for 72.2% of all isolates. PCV13 serotypes accounted for 69.6% of isolates overall, with a decrease from 71.8% in the first to 64.2% in the third study year. Most (84.8%) of the isolates with decreased susceptibility to penicillin had PCV13 serotypes, mainly 19A (59.5%). Among the non-PCV13 serotypes, the most prevalent was the emerging 12F serotype (6.5%), which was fully susceptible to beta-lactams (Fig. 1) and covered by the 23-valent polysaccharide vaccine.
Serotype distribution differed significantly across age groups (Electronic Supplementary Material 5). The prevalence of serotype 3 increased with age, accounting for 29% of serotypes after 65 years. Serotype 7F was found chiefly between 18 and 50 years of age and serotype 19A between 51 and 65 years of age. Serotypes known to have a highly invasive potential or associated with high mortality rates accounted for 72% and 55.5% of strains, respectively (Table 2). The frequency of these serotypes was significantly higher in the oldest group than in the younger groups (P = 0.011; Electronic Supplementary Material 6).
Hospital mortality
Overall, 116 (18.9%) patients died. Mortality increased with age for 27.1% in the group older than 65 years (P < 0.0001; Table 3). Mortality was 23.8% in patients who met major IDSA/ATS criteria at ICU admission and 31.3% in patients with septic shock. In the group of patients who died, mean age was 70 ± 15 years, mean SAPSII was 61 ± 18, mean SOFA score was 11.2 ± 4, and mean Fine score was 163 ± 35. Multiorgan failure was the main cause of death (45.7%). Of the patients who died, 32% died within the first 5 days. Day-5 mortality was similar across age groups, but differed according to ICU admission criteria (P = 0.0008) and presence of septic shock (P < 0.0001).
Factors associated with hospital mortality are reported in Table 4 (data pooled over imputed datasets) and Electronic Supplementary Material 7 (patients with no missing data). In the adjusted analysis, factors independently associated with hospital mortality were age > 65 years, male gender, McCabe score ≥ 2, higher SAPSII, platelets ≤ 100 × 109/L, lactates > 4 mmol/L, bilateral pneumonia, septic shock, and IMV. Interactions were found between gender and platelets: mortality was considerably higher in women with ≤ 100 × 109/L platelets than in women with higher platelet counts (adjusted OR, 7.70; 95% CI, 2.80–21), whereas men, regardless of their platelet count, were at greater risk for death compared to women with platelet counts > 100 × 109/L.
Figure 2 is the nomogram for predicting hospital death. The model was well calibrated, with a calibration curve showing no major deviations from the reference line (Electronic Supplementary Material 8) and an optimism-corrected c index of 0.841 (95% CI, 0.809–0.872).
Nomogram for predicting hospital death. The nomogram provides an estimate of the probability of death according to patient characteristics. For each characteristic listed, locate the relevant value on the horizontal line, and draw the vertical line from that value to the points line at the top of the figure. Sum the points for each characteristic and locate this number on the total points line at the bottom of the figure. Draw a straight line down from the number on the total points line to the probability of hospital death line just below it
After adjustment on the multivariable score predicting hospital death, no difference was found between beta-lactam therapy alone (19.4%) or with a macrolide (19.9%) or fluoroquinolone (15.1%) started within 24 h after ICU admission (Electronic Supplementary Material 4).
Serotype 3 was the serotype associated with the highest mortality rate (23.5%). However, this rate was not significantly different from the mortality rates for the other serotypes, with only the exception of serotype 12F, which was responsible for no deaths. In the unadjusted analysis, mortality was significantly higher for serotypes known to have low invasiveness and for those known to be associated with high mortality rates. However, after adjustment on host variables not affected by the pathogen, only low-invasiveness serotypes were significantly associated with higher mortality (Table 2).
Discussion
This study of a large prospective cohort of immunocompetent Caucasian adults admitted to the ICU for PCAP showed that hospital mortality was high, at nearly one in five, although all patients received appropriate antibiotics from the outset, usually within 6 h after ICU admission. The main factors assessable at admission and independently associated with hospital mortality were older age, male gender, worse McCabe score, worse SAPSII, septic shock, and markers of organ failure (serum lactate elevation, thrombocytopenia, bilateral pulmonary infiltrates, and IMV). Seven pneumococcal serotypes accounted for nearly three-fourths of all isolates. Serotype distribution varied significantly across age groups. Serotype was not independently associated with hospital mortality.
Our mortality rate of 18.9% is high. Several ICU studies found mortality rates of 16–20%, but included patients with immunodeficiencies [5,6,7, 11]. However, a study of two prospective databases of patients managed in 2001–2008 found a higher hospital mortality rate of 29% [4]. The introduction in recent years of care protocols for septic shock has led to a steady decrease in mortality throughout the world [26]. Nevertheless, septic shock was an independent risk factor for death in our study. The 31% hospital mortality rate in our subgroup with septic shock is lower than the 40–50% rates reported in the past [8, 9], but higher than in recent studies [6, 10]. These discrepancies are probably due to differences in case mix and treatment strategies. Day-5 mortality was very high, at 43%, in the youngest age group and was 35.7% in the subgroup with septic shock, perhaps due to a massive and deleterious proinflammatory response in these specific populations [12].
Mortality was very low in the subgroup admitted to the ICU with minor but no major IDSA/ATS criteria, in keeping with earlier data [27]. These patients may have been admitted earlier in the course of their disease then benefited from the close monitoring provided in the ICU. Minor criteria do not seem to be strong risk factors for death and may deserve to be used only as an aid to clinical judgment when making ICU admission decisions [28].
Mortality increased with age in our study, in keeping with earlier data [5, 29], an effect probably ascribable to immunosenescence. Age older than 65 years was an independent risk factor for death. The lower mortality in patients aged 18–50 years might be ascribable to herd immunity provided by childhood vaccination with pneumococcal conjugate vaccines (PCVs) [30]. Males predominated in our population, and male gender was independently associated with death, as reported previously [29,30,31,32]. The poorer prognosis in males versus females has been ascribed to differences in hormonal status and in inflammatory and immune responses, as well as to the higher prevalence of cardiovascular disease and exposure to toxic agents among males [33]. A recent study in a mouse model of pneumococcal infection also found that mortality was higher in males than in females (stronger proinflammatory response, faster rate of bacterial proliferation, slower clearance of lung bacteria) [34]. In contrast, in a vast retrospective study of patients with CAP managed in 17 countries between 2001 and 2011, after adjustment on a propensity score, 28-day mortality was higher in females [35]. However, the difference was small (absolute difference with males, 5%; hazard ratio, 1.15; 95% CI, 1.02–1.30) and the study was not confined to ICU patients. Thrombocytopenia was an independent risk factor for death in our study and in earlier work in an ICU population [36]. In a mouse model of pneumococcal pneumonia with bacteremia, induced thrombocytopenia was followed by decreased survival [37]. S. pneumoniae can bind to type 2 toll-like receptors on platelets, thereby inducing platelet activation and thrombocytopenia, which contributes to thrombosis, bleeding, and excessive inflammation in patients with severe PCAP [38]). The platelet count showed a strong interaction with gender in our study. Mortality was highest in women with thrombocytopenia, whereas the higher mortality rate in males versus females was independent from the platelet count. The platelet serotonin content is higher and is metabolized more slowly in females [39, 40]. Thrombocytopenia during PCAP is accompanied with the release of serotonin in the bloodstream. Serotonin not only exerts multiple vascular and hemodynamic effects, but also has major effects on immune cells [41]. However, it remains unclear why thrombocytopenia was associated with mortality in females but not in males in our study.
An unexpected finding from our study was that a longer than 6-h time from ICU admission to initiation of appropriate antibiotics was not associated with hospital mortality in the adjusted analyses, in contrast with an old study [6]. This finding may be ascribable to the small proportion of patients (26%) who did not receive antibiotics within 6 h. In other observational studies in critically ill patients with pneumonia due to various microorganisms, antibiotic therapy within 4–8 h was associated with survival [42, 43]. In non-randomized studies, adding a macrolide to a beta-lactam was associated with lower mortality [5, 42], although this result was not replicated in other work [12, 43,44,45], and all these studies had methodological weaknesses. In a mouse model of pneumococcal pneumonia, macrolides modulated the inflammatory response, as well as S. pneumoniae virulence [46]. Mortality was not lower in the patients given macrolides in our study. Similarly, in a recent cluster-randomized crossover trial in patients with severe CAP, after adjustment on a multivariable mortality prediction score, beta-lactam therapy alone was not inferior to beta-lactam therapy with a macrolide in terms of 90-day mortality [47]. Conceivably, the antiinflammatory effect of macrolides may be insufficient to induce clinical benefits in patients with the most severe forms of PCAP [45].
We found a broad diversity of pneumococcal serotypes reflecting the indirect herd effect of universal childhood immunization with PCV7 starting in 2005 then PCV13 starting in 2010 in France. Most of the patients enrolled during the first 2 study years had replacement serotypes such as 3, 7F, and 19A, whereas after the introduction of PCV13, the main serotypes were 3, 12F, 19A, and 7F, in descending order, with a decrease in the last two serotypes. The decline in the proportion of S. pneumoniae strains with decreased beta-lactam susceptibility over the 3-year study period is ascribable to the decrease in PCV13 vaccine serotypes, mainly 19A, combined with an increase in serotype 12F. In our study, serotypes 1 and 12F, which are known to be highly invasive [20,21,22, 42], were more common in younger patients and were associated with lower mortality, as reported previously [24, 25]. Although PCV13 includes serotype 3, the frequency of this serotype did not decrease during the study, suggesting absence of a herd effect [48]. Serotypes 3 and 19A have been reported to be associated with respiratory failure and mortality [10, 49], as well as to cause severe pneumonia in the elderly more often than serotypes 1, 7F, and 12F [24, 25]. However, in our study, serotypes 3 and 19A were not associated with hospital mortality. In the analyses adjusted for factors independent from the pathogen, no serotype was associated with hospital mortality. Thus, in patients with severe PCAP, host-related factors or other S. pneumoniae-related factors affecting virulence may have a greater effect on the risk of death compared to capsular polysaccharides, as suggested by a study in a murine model [50].
One limitation of our study is that, despite the large number of patients, only 349 isolates were serotyped, possibly limiting our ability to detect associations between serotype and mortality. The nomogram for predicting the risk of hospital mortality 24 h after ICU admission needs to be validated in large prospective studies of other cohorts of severe PCAP. Potential associations with viral co-infections and biomarkers such as C-reactive protein and procalcitonin were not assessed. Finally, we did not record mortality after hospital discharge, which has been reported to be about 40% after 1 year due, in particular, to a cardiovascular risk increase in the oldest patients [51].
In conclusion, in a large population of immunocompetent Caucasian adults managed in the ICU for severe PCAP, hospital mortality remained high, particularly in the oldest patients, although appropriate antibiotic therapy was consistently given, usually within 6 h after ICU admission. Older age, male gender, and organ failures at admission were more strongly associated with hospital mortality than were comorbidities, pneumococcal serotypes, and antibiotic regimens. Improvements in our understanding of interactions between host factors and S. pneumoniae virulence factors are needed to improve survival. New pneumococcal vaccines targets should be designed to match the continuous changes in pneumococcal serotypes and provide much broader and longer protective coverage.
References
Marrie TJ, Shariatzadeh MR (2007) Community-acquired pneumonia requiring admission to an intensive care unit: a descriptive study. Medicine (Baltimore) 86:103–111. https://doi.org/10.1097/MD.0b013e3180421c16
Walden AP, Clarke GM, McKechnie S et al (2014) Patients with community acquired pneumonia admitted to European intensive care units: an epidemiological survey of the GenOSept cohort. Crit Care Lond Engl 18:R58. https://doi.org/10.1186/cc13812
Drijkoningen JJC, Rohde GGU (2014) Pneumococcal infection in adults: burden of disease. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis 20(Suppl 5):45–51. https://doi.org/10.1111/1469-0691.12461
Mongardon N, Max A, Bouglé A et al (2012) Epidemiology and outcome of severe pneumococcal pneumonia admitted to intensive care unit: a multicenter study. Crit Care Lond Engl 16:R155. https://doi.org/10.1186/cc11471
Naucler P, Darenberg J, Morfeldt E et al (2013) Contribution of host, bacterial factors and antibiotic treatment to mortality in adult patients with bacteraemic pneumococcal pneumonia. Thorax 68:571–579. https://doi.org/10.1136/thoraxjnl-2012-203106
Gattarello S, Borgatta B, Solé-Violán J et al (2014) Decrease in mortality in severe community-acquired pneumococcal pneumonia: impact of improving antibiotic strategies (2000–2013). Chest 146:22–31. https://doi.org/10.1378/chest.13-1531
Que Y-A, Virgini V, Lozeron ED et al (2015) Low C-reactive protein values at admission predict mortality in patients with severe community-acquired pneumonia caused by Streptococcus pneumoniae that require intensive care management. Infection 43:193–199. https://doi.org/10.1007/s15010-015-0755-0
Moine P, Vercken JB, Chevret S, Gajdos P, The French Study Group of Community-Acquired Pneumonia in ICU (1995) Severe community-acquired pneumococcal pneumonia. Scand J Infect Dis 27:201–206
Georges H, Leroy O, Vandenbussche C et al (1999) Epidemiological features and prognosis of severe community-acquired pneumococcal pneumonia. Intensive Care Med 25:198–206
Garcia-Vidal C, Ardanuy C, Tubau F et al (2010) Pneumococcal pneumonia presenting with septic shock: host- and pathogen-related factors and outcomes. Thorax 65:77–81. https://doi.org/10.1136/thx.2009.123612
Cillóniz C, Polverino E, Ewig S et al (2013) Impact of age and comorbidity on cause and outcome in community-acquired pneumonia. Chest 144:999–1007. https://doi.org/10.1378/chest.13-0062
Burgos J, Luján M, Larrosa MN et al (2015) The problem of early mortality in pneumococcal pneumonia: a study of risk factors. Eur Respir J 46:561–564. https://doi.org/10.1183/09031936.00034415
Mandell LA (2009) Severe community-acquired pneumonia (CAP) and the Infectious Diseases Society of America/American Thoracic Society CAP guidelines prediction rule: validated or not. Clin Infect Dis 48:386–388. https://doi.org/10.1086/596308
Société de Pathologie Infectieuse de Langue Française (2006) 15th consensus conference about management of lower respiratory tract infections in immunocompetent adult. Med Mal Infect 36:235–244
The European Committe on Antimicrobial Susceptibility Testing. (2015) Breakpoints tables for interpretation of MICs and zone diameters. Version 5.0, 2015. http://www.eucast.org. Accessed 24 Oct 2018
Varon E, Houssaye S, Grondin S et al (2006) Nonmolecular test for detection of low-level resistance to fluoroquinolones in Streptococcus pneumoniae. Antimicrob Agents Chemother 50:572–579. https://doi.org/10.1128/AAC.50.2.572-579.2006
Auburtin M, Wolff M, Charpentier J et al (2006) Detrimental role of delayed antibiotic administration and penicillin-nonsusceptible strains in adult intensive care unit patients with pneumococcal meningitis: the PNEUMOREA prospective multicenter study. Crit Care Med 34:2758–2765. https://doi.org/10.1097/01.CCM.0000239434.26669.65
Kalbfleisch J (1980) The statistical analysis of failure time data. Wiley, New York
Grabenstein JD, Musey LK (2014) Differences in serious clinical outcomes of infection caused by specific pneumococcal serotypes among adults. Vaccine 32:2399–2405. https://doi.org/10.1016/j.vaccine.2014.02.096
Varon E, Cohen R, Béchet S et al (2015) Invasive disease potential of pneumococci before and after the 13-valent pneumococcal conjugate vaccine implementation in children. Vaccine 33:6178–6185. https://doi.org/10.1016/j.vaccine.2015.10.015
Brueggemann AB, Griffiths DT, Meats E et al (2003) Clonal relationships between invasive and carriage Streptococcus pneumoniae and serotype- and clone-specific differences in invasive disease potential. J Infect Dis 187:1424–1432. https://doi.org/10.1086/374624
Hanage WP, Kaijalainen TH, Syrjänen RK et al (2005) Invasiveness of serotypes and clones of Streptococcus pneumoniae among children in Finland. Infect Immun 73:431–435. https://doi.org/10.1128/IAI.73.1.431-435.2005
Sá-Leão R, Pinto F, Aguiar S et al (2011) Analysis of invasiveness of pneumococcal serotypes and clones circulating in Portugal before widespread use of conjugate vaccines reveals heterogeneous behavior of clones expressing the same serotype. J Clin Microbiol 49:1369–1375. https://doi.org/10.1128/JCM.01763-10
Harboe ZB, Thomsen RW, Riis A et al (2009) Pneumococcal serotypes and mortality following invasive pneumococcal disease: a population-based cohort study. PLoS Med 6:e1000081. https://doi.org/10.1371/journal.pmed.1000081
Weinberger DM, Harboe ZB, Sanders EAM et al (2010) Association of serotype with risk of death due to pneumococcal pneumonia: a meta-analysis. Clin Infect Dis 51:692–699. https://doi.org/10.1086/655828
Coz Yataco A, Jaehne AK, Rivers EP (2017) Protocolized early sepsis care is not only helpful for patients: it prevents medical errors. Crit Care Med 45:464–472. https://doi.org/10.1097/CCM.0000000000002237
Liapikou A, Ferrer M, Polverino E et al (2009) Severe community-acquired pneumonia: validation of the Infectious Diseases Society of America/American Thoracic Society guidelines to predict an intensive care unit admission. Clin Infect Dis 48:377–385. https://doi.org/10.1086/596307
Ewig S (2011) Gains and limitations of predictive rules for severe community-acquired pneumonia. Clin Infect Dis 53:512–514. https://doi.org/10.1093/cid/cir469
Krone CL, van de Groep K, Trzciński K et al (2014) Immunosenescence and pneumococcal disease: an imbalance in host–pathogen interactions. Lancet Respir Med 2:141–153. https://doi.org/10.1016/S2213-2600(13)70165-6
Grau I, Ardanuy C, Cubero M et al (2016) Declining mortality from adult pneumococcal infections linked to children’s vaccination. J Infect 72:439–449. https://doi.org/10.1016/j.jinf.2016.01.011
Gutiérrez F, Masiá M, Mirete C et al (2006) The influence of age and gender on the population-based incidence of community-acquired pneumonia caused by different microbial pathogens. J Infect 53:166–174. https://doi.org/10.1016/j.jinf.2005.11.006
Kaplan V, Clermont G, Griffin MF et al (2003) Pneumonia: still the old man’s friend? Arch Intern Med 163:317–323
Angele MK, Schwacha MG, Ayala A, Chaudry IH (2000) Effect of gender and sex hormones on immune responses following shock. Shock Augusta Ga 14:81–90
Kadioglu A, Cuppone AM, Trappetti C et al (2011) Sex-based differences in susceptibility to respiratory and systemic pneumococcal disease in mice. J Infect Dis 204:1971–1979. https://doi.org/10.1093/infdis/jir657
Arnold FW, Wiemken TL, Peyrani P et al (2013) Outcomes in females hospitalised with community-acquired pneumonia are worse than in males. Eur Respir J 41:1135–1140. https://doi.org/10.1183/09031936.00046212
Brogly N, Devos P, Boussekey N et al (2007) Impact of thrombocytopenia on outcome of patients admitted to ICU for severe community-acquired pneumonia. J Infect 55:136–140. https://doi.org/10.1016/j.jinf.2007.01.011
van den Boogaard FE, Schouten M, de Stoppelaar SF et al (2015) Thrombocytopenia impairs host defense during murine Streptococcus pneumoniae pneumonia. Crit Care Med 43:e75–e83. https://doi.org/10.1097/CCM.0000000000000853
Keane C, Tilley D, Cunningham A et al (2010) Invasive Streptococcus pneumoniae trigger platelet activation via Toll-like receptor 2. J Thromb Haemost JTH 8:2757–2765. https://doi.org/10.1111/j.1538-7836.2010.04093.x
Costa JL, Reese TS, Murphy DL (1974) Serotonin storage in platelets: estimation of storage-packet size. Science 183:537–538
Snell LD, Glanz J, Tabakoff B, WHO/ISBRA Study on State and Trait Markers ofAlcohol Use and Dependence Investigators (2002) Relationships between effects of smoking, gender, and alcohol dependence on platelet monoamine oxidase-B: activity, affinity labeling, and protein measurements. Alcohol Clin Exp Res 26:1105–1113
Buckley NA, Dawson AH, Isbister GK (2014) Serotonin syndrome. BMJ 348:g1626
Lee JS, Giesler DL, Gellad WF, Fine MJ (2016) Antibiotic therapy for adults hospitalized with community-acquired pneumonia: a systematic review. JAMA 315:593–602. https://doi.org/10.1001/jama.2016.0115
Sligl WI, Hoang H, Eurich DT et al (2013) Macrolide use in the treatment of critically ill patients with pneumonia: incidence, correlates, timing and outcomes. Can J Infect Dis Med Microbiol J Can Mal Infect Microbiol Medicale 24:e107–e112
Paul M, Nielsen AD, Gafter-Gvili A et al (2007) The need for macrolides in hospitalised community-acquired pneumonia: propensity analysis. Eur Respir J 30:525–531. https://doi.org/10.1183/09031936.00031007
Sligl WI, Asadi L, Eurich DT et al (2014) Macrolides and mortality in critically ill patients with community-acquired pneumonia: a systematic review and meta-analysis. Crit Care Med 42:420–432. https://doi.org/10.1097/CCM.0b013e3182a66b9b
Yoshioka D, Kajiwara C, Ishii Y et al (2016) Efficacy of β-lactam-plus-macrolide combination therapy in a mouse model of lethal pneumococcal pneumonia. Antimicrob Agents Chemother 60:6146–6154. https://doi.org/10.1128/AAC.01024-16
Postma DF, van Werkhoven CH, van Elden LJR et al (2015) Antibiotic treatment strategies for community-acquired pneumonia in adults. N Engl J Med 372:1312–1323. https://doi.org/10.1056/NEJMoa1406330
Slotved H-C, Dalby T, Harboe ZB et al (2016) The incidence of invasive pneumococcal serotype 3 disease in the Danish population is not reduced by PCV-13 vaccination. Heliyon 2:e00198. https://doi.org/10.1016/j.heliyon.2016.e00198
Burgos J, Luján M, Larrosa MN et al (2014) Risk factors for respiratory failure in pneumococcal pneumonia: the importance of pneumococcal serotypes. Eur Respir J 43:545–553. https://doi.org/10.1183/09031936.00050413
Mohler J, Azoulay-Dupuis E, Amory-Rivier C et al (2003) Streptococcus pneumoniae strain-dependent lung inflammatory responses in a murine model of pneumococcal pneumonia. Intensive Care Med 29:808–816. https://doi.org/10.1007/s00134-003-1699-x
Corrales-Medina VF, Musher DM, Shachkina S, Chirinos JA (2013) Acute pneumonia and the cardiovascular system. Lancet Lond Engl 381:496–505. https://doi.org/10.1016/S0140-6736(12)61266-5
Acknowledgements
We thank the ICU physicians who contributed to collect data for the study: Nadia Anguel (CHU Bicêtre, Le Kremlin-Bicêtre, France); Christian Brun-Buisson (Hôpital H. Mondor, Créteil, France); M. Castaner (Hôpital Sud-Sainte Marguerite, Marseille, France); Charles Cerf (Hôpital Foch, Suresnes, France); Christine Cheval (CH Hyères, France); Bernard Clair (Hôpital R. Poincaré, Garches, France); Yves Cohen (Hôpital Avicenne, Bobigny, France); Jean-Michel Constantin (CHU Hôtel Dieu, Clermont Ferrand, France); Aurélie Cravoisy-Brovic (Hôpital Central, Nancy, France); Arnaud Delahaye (CH Rodez, France); N. Fadel (CH Rambouillet, France); Muriel Fartoukh and Antoine Parrot (Hôpital Tenon, Paris, France); Christian Floriot and Christophe Bein (CHI Haute Saône, Vesoul, France); Hugues Georges (CH Tourcoing, France); Claude Gervais (Hôpital Caremeau, Nîmes, France); Dany Goldran-Toledano (Hôpital de Gonesse, France); Jan Hayon and Jean-Claude Lacherade (CHI Poissy-Saint Germain en Laye, France); Kada Klouche (CHU Lapeyronie, Montpellier, France); Sophie Marqué (CHU Rennes, France); Jean-Marc Mazou (CH Dax, France); Hervé Mentec (CH V. Dupouy, Argenteuil, France); Joy Yoganaden Mootien (CH Mulhouse, France); Bruno Mourvillier (GH Bichat, Paris, France); Jean Nouveau (Hôpital Monod, Le Havre, France); Ana Novara (HEGP, Paris, France); Bernard Page (Hôpital A. Paré, Boulogne, France); Antoine Rabbat (Hôtel Dieu, Paris, France); Marie Thuong (CH Delafontaine, Saint-Denis, France); Martial Thyrault (CHG Longjumeau, France); Jean-François Timsit (CHU A. Michaillon, Grenoble, France); Jean-Marie Tonnelier (CHU La Cavale Blanche, Brest, France); and Olivier Zambon (CHU, Nantes, France).
We are grateful to the microbiologists who sent the pneumococcal strains to the French National Reference Centre for Pneumococci (FNRCP): Guillaume Arlet (Hôpital Tenon, Paris, France); Laurence Armand-Lefevre (Hôpital Bichat, Paris, France); Régine Baraduc (CHU Gabriel Montpied, Clermont Ferrand, France); Gilles Berthelot (CH Dieppe, France); Martine Bingen (Hôpital de Gonesse, France); Michel Brun and Christian Carrière (CHU Lapeyronie, Montpellier, France); Annie Buu-Hoi and Emmanuelle Varon (Hôpital Européen Georges Pompidou, Paris, France); Violaine Caillaux (CH Tourcoing, France); Christian Cattoen (CH Valenciennes, France); Guy Chambreuil (CHD Les Oudairies, La Roche sur Yon, France); Chantal Chaplain (CH Delafontaine, Saint-Denis, France); Hubert Chardon (CH du Pays d’Aix, Aix en Provence, France); Mireille Cheron, Michel Leneveu, and Eric Vallée (CHI Poissy, St Germain en Laye, France); Vincent Chieux (Hôpital L. Pasteur, Chartres, France); M.D. Conroy (Hôpital Central, Nancy, France); Jacques Croizé (CHU A. Michaillon, Grenoble, France); Alexandre Doloy and Hélène Poupet (Hôpital Cochin, Paris, France); Pierre-Yves Donnio (CHU, Rennes, France); Florence Doucet-Populaire (Hôpital A. Béclère, Clamart, France); AnneFarges (CHG Longjumeau, France); Jean-Louis Gaillard (Hôpital R. Poincaré, Garches, France); Alain Gravet (CH Mulhouse, France); Bernadette Grignon (CHU J. Bernard, Poitiers, France); Patrick Honderlick (Hôpital Foch, Suresnes, France); Françoise Jaureguy (Hôpital Avicenne, Bobigny, France); Marie-Emmanuelle Juvin (CHU Nantes, France); Marie Kempf (CHU, Angers, France); Marie-Dominique Kitzis (Hôpital St Joseph, Paris, France); Jean-Pierre Laffargue (CH Dax, France); Jean-Philippe Lavigne (Hôpital Caremeau, Nîmes, Frances); Alban Le Monnier (CH Mignot, Le Chesnay, France); Françoise Le Turdu (CH V. Dupouy, Argenteuil, France); P. Legrand (Hôpital H. Mondor, Créteil, France); PierreYves Levy (Hôpital La Timone, Marseille, France); Julien Loubinoux (Hôpital Hôtel Dieu, Paris, France); Morel (Hôpital Monod, Le Havre, France); M.C. Ploy and Delphine Chainier (CHU Dupuytren, Limoges, France); Patrick Pina (CH Rambouillet, France); Didier Poisson (Hôpital La Source, Orléans, France); Annie Raoult (CH Hyères, France); Laurent Raskine (Hôpital Lariboisière, Paris, France); Micheline Roussel-Delvallez (Hôpital A. Calmette, Lille, France); Royer (CHI Haute Saône, Vesoul, France); Cyril Serizer (CH Sud Essonne, Etampes, France); V. Sivadon-Tardy (Hôpital A. Paré, Boulogne, France); Colette Spicq (CHU Bicêtre, Le Kremlin Bicêtre, France); Didier Tandet (CHU La Cavale Blanche, Brest, France); Jacques Tankovic (Hôpital St Antoine, Paris, France); Véronique Vernet-Garnier (Hôpital R. Debré, Reims, France); and Joseph Wattine (CH Rodez, France).
We are indebted to Nathalie Marin and the Clinical Research Unit at the Cochin Teaching Hospital (Paris, France) for centralizing and processing the study data and to A. Wolfe, MD, for helping to prepare the manuscript.
Funding
This study was funded by a 2006 grant from the French public research agency PHRC (#07/061). The study sponsors were two public healthcare and research agencies, namely, the Assistance Publique Hôpitaux de Paris (AP-HP) and the Délégation à la Recherche Clinique et au Développement (DRCD).
Author information
Authors and Affiliations
Contributions
JPB, EV and JPM are the study guarantors and designed the study; EV and RP extracted and managed the data; RP performed the statistical analysis; and JPB, EV, RP, and JPM wrote the manuscript. All authors included more than 10 patients in the study. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None of the authors have any conflicts of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bedos, JP., Varon, E., Porcher, R. et al. Host–pathogen interactions and prognosis of critically ill immunocompetent patients with pneumococcal pneumonia: the nationwide prospective observational STREPTOGENE study. Intensive Care Med 44, 2162–2173 (2018). https://doi.org/10.1007/s00134-018-5444-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-018-5444-x