Abstract
Purpose
The intensity of procedural pain in intensive care unit (ICU) patients is well documented. However, little is known about procedural pain distress, the psychological response to pain.
Methods
Post hoc analysis of a multicenter, multinational study of procedural pain. Pain distress was measured before and during procedures (0–10 numeric rating scale). Factors that influenced procedural pain distress were identified by multivariable analyses using a hierarchical model with ICU and country as random effects.
Results
A total of 4812 procedures were recorded (3851 patients, 192 ICUs, 28 countries). Pain distress scores were highest for endotracheal suctioning (ETS) and tracheal suctioning, chest tube removal (CTR), and wound drain removal (median [IQRs] = 4 [1.6, 1.7]). Significant relative risks (RR) for a higher degree of pain distress included certain procedures: turning (RR = 1.18), ETS (RR = 1.45), tracheal suctioning (RR = 1.38), CTR (RR = 1.39), wound drain removal (RR = 1.56), and arterial line insertion (RR = 1.41); certain pain behaviors (RR = 1.19–1.28); pre-procedural pain intensity (RR = 1.15); and use of opioids (RR = 1.15–1.22). Patient-related variables that significantly increased the odds of patients having higher procedural pain distress than pain intensity were pre-procedural pain intensity (odds ratio [OR] = 1.05); pre-hospital anxiety (OR = 1.76); receiving pethidine/meperidine (OR = 4.11); or receiving haloperidol (OR = 1.77) prior to the procedure.
Conclusions
Procedural pain has both sensory and emotional dimensions. We found that, although procedural pain intensity (the sensory dimension) and distress (the emotional dimension) may closely covary, there are certain factors than can preferentially influence each of the dimensions. Clinicians are encouraged to appreciate the multidimensionality of pain when they perform procedures and use this knowledge to minimize the patient’s pain experience.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Evidence developed over the past 25 years has been overwhelming that pain is a frequent occurrence for patients in intensive care units (ICUs) [1,2,3]. Research endeavors have done well to concentrate on the intensity of pain, which is the degree of the pain sensation. As a result, we know that pain intensity is substantial and varies according to the type of injury [4], illness [5], or medical procedure [6]. Pain intensity, related to the degree of severity of the sensation, is but one of pain’s multiple dimensions. A second dimension is the affective nature of pain, or the degree of distress experienced by a patient. Pain distress is related to emotional unpleasantness and concern about threat to life or well-being [7]. In fact, a recently proposed change to the definition of pain reinforces pain as a distressing experience, which recognizes its aversive nature [8].
In non-ICU [9, 10] and ICU [11] symptom research, considerable attention has been given to the differences in patient reports of pain intensity and distress; however, ICU pain research has fallen short of addressing the psychological dimension of pain, pain distress, even though unrelieved pain is one of the main sources of psychological stress for ICU patients [12, 13].
While measures of pain intensity and pain distress are often highly correlated [14], this correlation is not 100% [15]. Pain science has clearly delineated the differences between the two. Neural mechanisms of both the sensory/intensity and affective/distress dimensions of pain have been well mapped, and brain structures that are differentially involved in pain intensity and pain distress have been identified [16, 17]. (Of note, a patient with a postcentral stroke lost pain sensation while pain affect was preserved [18].) Clinically, different types of pain have been associated with greater pain distress (e.g., cancer-related pain) or greater pain intensity (e.g., labor pain) when intensity and distress measures are compared [7]. Affective responses (i.e., distress) can be influenced by contextual factors; for example, pain associated with cancer can make a person more fearful of a poor prognosis than pain associated with labor. It has been long understood that these two dimensions of pain can covary under some conditions and not under others [19]. An empiric understanding of the distress that accompanies commonly performed procedures in ICUs can provide support for the measurement of both dimensions in clinical settings [7] and could guide selection of interventions.
The work presented here is a pre-planned sub-study from the Europain® project, with the original study previously published [20]. This was a multinational sample of ICU patients who underwent selective diagnostic or treatment-related procedures in which we concentrated on pain intensity associated with procedures. Since, in that study, we asked patients to not only report pain intensity but to also report pain distress associated with their procedure, we are able to analyze this dimension of pain in a large ICU patient population. Our purpose here is to answer the following research questions related to procedural pain distress:
-
1.
Does pain distress increase when ICU patients undergo frequently performed procedures and, if so, is the increase significant?
-
2.
Are there certain factors that cause ICU patients to experience a greater degree of pain distress when they undergo procedures?
-
3.
Are there certain factors that cause ICU patients to have greater pain distress than pain intensity when they undergo procedures?
Methods
Design, site, and sample
Europain® was a prospective, cross-sectional, multicenter, multinational study of procedural pain associated with 12 procedures commonly performed in ICUs. Europain® received support from the European Society of Intensive Care Medicine (ESICM). Each of the 28 participating countries had volunteer National Coordinators (NC). One or more physicians or nurses working in the 92 study ICUs volunteered to be ICU Study Coordinators. While this study was extensively described previously [20], we repeat certain information related to study subjects and procedures to offer sufficient background to evaluate this current analysis.
Patients were eligible if they were 18 years of age or older, able to speak English or their country’s primary language, and were to undergo at least one of the study procedures as part of standard care. Exclusion criteria were clinical instability, treatment with neuromuscular blockers, conditions associated with altered pain perception (e.g., Guillain–Barré disease), conditions likely to interfere with behavioral assessments of pain (e.g., decerebrate posturing), and/or a definitive or probable diagnosis of delirium by the ICU clinician. Patients with delirium were excluded because the validity of their reports could not be assured as a result of non-use of validated delirium scales in many of the ICUs.
Ethics committee approval was obtained at the study coordinating center in Paris and at the home institution of the principal investigator (KP). IRB approval which met local legislation criteria, including whether or not patient consent was required, was mandatory for study participation in all ICUs. Failure to obtain this approval (n = 9 countries) or withdrawal after IRB approval (n = 2 countries) left 28 of an original 39 participating countries.
Measures
Pain distress was measured using a horizontal 0–10 numeric rating scale (NRS), with higher numbers indicating greater distress. NRS scales have both construct [21, 22] and concurrent validity [21, 23], and pain distress has been measured in non-ICU [24] and ICU studies [25, 26]. Prior to the procedure, patients were asked the following question: “How distressful (or bothersome) is your pain right now, where 0 = no distress and 10 = very distressing?” Immediately after the procedure, patients were asked, “How distressful (or bothersome) was your pain during the procedure, where 0 = no distress and 10 = very distressing?” Pain intensity was also measured using a 0–10 NRS, with higher numbers indicating greater pain intensity. Prior to the procedure, patients were asked, “What number would you give the worst pain you have had today, where 0 = no pain and 10 = worst possible pain?” Prior to the procedure, they were also asked the following question: “How intense is your pain right now, where 0 = no pain and 10 = worst possible pain?” Immediately after the procedure, patients were asked, “How intense was your pain during the procedure, on this scale where 0 = no pain and 10 = worst possible pain?” Patients who were unable to report pain intensity/distress scores were eliminated from analyses requiring these scores. Pain behaviors were also recorded before and during the procedure, and the psychometric properties of the behavioral observation form have been published [27].
Procedures
A full description of study procedures can be found in our previous article [20]. In short, ICU coordinators selected the procedure(s) to be studied in their ICUs from a predefined list (see Electronic Supplement Table 1 for procedures and definitions), and patients could be enrolled for one or two procedures if not performed at the same time. There were two ICU clinician data collectors for each procedure; each recorded patient responses to the questions posed to the patient by one of them, as well as observing and recording pain behavior data [27], for data reliability analyses. Pain distress and intensity were assessed prior to and immediately after the procedure, with the latter being measures of procedural pain. ICU coordinators sent all completed data collection packets to the study center in Paris for data entry. For analyses in this report, we used data from patients who were able to report pain distress and intensity prior to and immediately after the procedure. Country religiosity was assessed using data from the Gallup Poll results released in 2009 (the question asked was “Is religion important in your daily life?” and religiosity was the percentage of “yes” answers per country (http://news.gallup.com/poll/13117/religion-europe-trust-filling-pews.aspx). Countries with religiosity greater than 81% who participated in the study include Romania, Brazil, India, and Tunisia.
Statistical analyses
A Bland–Altman analysis was conducted to determine the levels of agreement between pain intensity and pain distress. Other results are expressed as numbers (%) for categorical variables and medians [interquartile range, IQR] for continuous variables, unless stated otherwise. The primary outcome measure for this report was procedural pain distress, which was studied using negative binomial regression in a hierarchical model with ICU and country as random effects. Multivariate models adjusting for potential confounding factors were built. Variables associated with P values less than 0.20 by univariate analysis were entered into the multivariate model and kept if the P value was less than 0.05. Adjusted relative risks and 95% confidence intervals (95% CI) were calculated for each parameter estimate. P values less than 0.05 were considered significant. Analyses were computed using the SAS 9.3 software package (SAS Institute, Cary, NC, USA).
Although there were two simultaneous data collectors, in order to test reliability of the data collected, a single observation data point per procedure was used to avoid creating an additional level in the final hierarchical model. For NRS values, this observation was the mean of the values recorded by the two data collectors. For binary variables, when data from one observer were missing, the data from the other observer were used. Concordance between the two observers for pain scores was excellent (kappa > 0.90).
Results
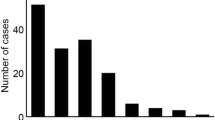
A total of 192 ICUs in 28 countries participated in the study. Of the 5107 procedures in 4080 ICU patients observed for the study, 4812 procedures (94%) in 3851 patients were evaluable (Fig. 1). Data on patient characteristics have been previously published [20]. Briefly, 61% of patients were male; the median age was 62 [50–73]; 37.2% of patients were mechanically ventilated during the procedure; and 65% patients were able to speak or otherwise communicate. The median admission SOFA score was 3.7 [2–6.1], and median procedure day RASS score was 0 [− 1 to 0]. ICU mortality rate was 10.3%.
Patient flow chart. N = 261 procedures (215 patients) did not meet inclusion and/or exclusion criteria: 37 patients (52 procedures) younger than 18 years; 72 patients (82 procedures) did not speak the country language; did not meet IRB requirements (12 patients, 19 procedures); did not undergo procedures of interest (17 patients, 24 procedures); 67 patients (76 procedures) were unstable at the time of procedure; 16 patients (16 procedures) were receiving neuromuscular blocking medication; 20 patients (21 procedures) had disease or condition that alters sensory transmission; 28 patients (32 procedures) had disease or condition that would confuse the behavioral assessment (i.e., decerebrate posturing); 51 patients (62 procedures) were delirious
The most common procedure was turning (n = 873), and the least common was wound drain removal (n = 75). Median/[IQR] procedural pain distress scores on the 0–10 NRS were highest for endotracheal (ET) (4 [1–7]) and tracheal (4 [2–6]) suctioning, chest tube removal (4 [2–6.5]), and wound drain removal (4 [1–7]) (Table 1). Pain distress scores increased significantly from before the procedure (from a median of 0 [0–4] to 3 [0–5] depending on procedure) to during the procedure (from 2 [0–5] to 4 [1–7], P < 0.00 depending on the procedure) (P < 0.001–0.005) for all procedures except for wound care.
The Bland–Altman analysis shown in Fig. 2 demonstrates that, while there was a high degree of agreement between pain intensity and pain distress, there was variability between the two measures. In fact, Pearson’s correlation between the two was 0.79. This finding reinforces that, while pain intensity and pain distress can be highly correlated [14, 15], the correlation was not 100%. Subsequent analyses identified where differences existed in patients, i.e., where pain intensity and pain distress were different for the patient.
Several risk factors independently predicted that patients would have a higher degree of procedural pain distress (Table 2). These included certain procedures: turning [relative risk/confidence interval = 1.18/1.02–1.37), ETS (1.45/1.14–1.66), tracheal suctioning (1.38/1.14–1.66), CTR (1.39/1.16–1.66), wound drain removal (1.56/1.23–1.99), and arterial line insertion (1.41/1.15–1.73). Certain pain behaviors exhibited by the patient prior to the procedure predicted that the patient’s pain distress would be higher during the procedure: grimacing (RR/CI = 1.19/1.09–1.31), eyes closed (RR/CI = 1.11/1.02–1.20), and moaning (RR/CI = 1.28/1.12–1.48). The higher the patient’s “worst pain intensity” score on the procedure day was also a significant risk for them having higher procedural pain distress (RR/CI = 1.15/1/13–1.16).
Finally, if patients had received morphine (RR/CI = 1.12/1.02–1.23) or tramadol (1.17/1.05–1.30) or other opioids on the procedure day (RR/CI = 1.22/1.06–1.40), prior to the procedure, or if they received opioids specifically for the procedure (RR/CI = 1.15/1.02–1.28) they were more likely to be at risk for higher procedural pain distress. The country did not have a significant effect on pain distress; however, there was a significant ICU effect.
For our third analysis, we conducted multivariate modeling to identify factors that would put patients at risk for experiencing greater pain distress than pain intensity. (Pain intensity scores are reported in Table 2 of our previous publication [20], and pain distress scores are found here in Table 1.) With tracheal suctioning as the comparator, the odds were that most of the procedures would be associated with less pain distress than intensity (Table 3). Conversely, for chest tube removal, wound drain removal, and mobilization, degrees of pain intensity and pain distress were similar. However, the odds of patients having greater pain distress than intensity during the procedure were if the patient’s pre-procedural pain intensity score were significantly higher [odds ratio (OR)/CI 1.05/1.01–1.09] or if patients had pre-hospital anxiety (OR/CI 1.76/1.29–2.41).
Finally, if patients received pethidine/meperidine (RR/CI 4.12/1.05–16.07) or haloperidol (RR/CI 1.77/1.01–3.12) before the procedure, the odds for patients experiencing greater pain distress than intensity were higher.
Discussion
To our knowledge, this is the first extensive report on ICU patients’ experiences of pain distress and the only ICU study to investigate this pain distress using a model of procedural pain. We found that patient-reported pain distress increased significantly from the pre-procedure time to the time of the procedure for all procedures except for wound care. While not surprising, this has not been documented previously. We also found that half of the procedures increased the risk of patients having higher degrees of pain distress by at least 30%: ET and tracheal suctioning, chest tube removal, wound drain removal, turning, and arterial line insertion. There may be some factors unique to these procedures that may account for the higher distress. The first two procedures, ET and tracheal suctioning, can not only cause pain but also a decrease of oxygenation levels, choking, gagging, and shortness of breath. Chest tube removal also affects the pulmonary system, as the tube is moved from the interpleural space through pulmonary and chest wall tissues. These actions, which many patients have described as fearful [25], may be seen as an intrinsic emotional threat due to the interference with breathing. It is unclear why drain removal is associated with a risk of higher pain distress, but the movement of drains through body parts may feel like a threat to a person’s tissue integrity. Another risk for higher procedural pain distress was when patients had reported a higher degree of “worst pain intensity” on the day of, but previous to, the procedure. It may be that their pain during the day had been more bothersome to them because they had “hurt more”, causing them more distress when they were subjected to additional, procedural pain. This distress may have been reflected in certain behaviors exhibited prior to the procedure (eyes closed, grimacing, and moaning), also risk factors for higher procedural pain distress. Taken together, these findings of higher pain levels the day of, but prior to, the procedure and behaviors of distress that they were exhibiting could increase a clinician’s “index of suspicion” that the pain that patients were about to experience during the procedure could cause them increased distress. Attending to the distress of patients undergoing procedures may be as important to the patient as attending to the intensity of the experience. Clinicians could consider using analgesics to decrease the procedural pain intensity and non-pharmacological interventions such as providing information [24] and soothing talk or music [26] to decrease the procedural distress.
When patients were receiving opioids on the day of the procedure or received opioids specifically for the procedure, they, too, were at risk for higher degree of procedural pain distress. It is perplexing why opioids received before a procedure would be a risk factor for increased procedural pain distress. The reasons for these patients receiving opioids are unknown. Perhaps, they received opioids for the procedure but the drug had not reached peak effect at procedure time. Perhaps the amount of opioid administered was insufficient to relieve the pain, leading to increased procedural pain distress. It is also possible that patients who had been receiving opioids during their ICU stay were experiencing opioid-induced hyperalgesia (OIH), a state of enhanced pain sensitivity [28]. OIH may occur when there is an increase in perceived pain with an increase in opioid use and has been identified in postoperative patient populations [29]. Investigating the reason(s) for our finding is beyond the scope of our study. Yet, this finding was similar to that found in our previous report [20], in that patients who received opioids prior to the procedure reported greater procedural pain intensity. Future research is warranted to discern the intriguing relationship among opioid administration for a procedure and pre-procedural and procedural pain intensity and distress. In the meantime, as we are currently concerned about potential short- and long-term adverse effects from use of opioids, a multimodal approach to procedural pain management through use of non-opioid analgesics alone or concurrent with use of (lower) opioid doses may be considered [30].
Some of the significant risk factors for higher procedural pain distress (i.e., certain procedures, receiving opioids, and a higher degree of “worst” pain intensity prior to the procedure) were treatment-related not intrinsically patient-related. Thus, these factors may be under the control of clinicians who can influence the procedural pain experience of patients, either positively or negatively. As noted by others [7], the emotional dimension of pain does not depend solely on how much tissue is damaged or how intense the pain is; it is greatly influenced by the psychological context in which pain occurs.
In another analysis, we asked: Are there certain factors that cause ICU patients to have greater pain distress than pain intensity when they undergo procedures?” We found that for half of the procedures, the risk for patients was to experience higher pain intensity than pain distress. Yet for chest tube removal, wound drain removal, and mobilization, the differences between procedural pain intensity and distress were not significant. These findings accentuate the fact that pain is multidimensional and what is done to a patient can be both intense (invasive) and distressful (emotionally unpleasant) and, in a certain situation, one can predominate [7]. What is essential is that both are assessed by clinicians in order to individualize treatment approaches in a particular situation.
We also found that patients with higher pre-procedural pain intensity were at risk for having greater procedural pain distress than pain intensity during the procedure. It may be that patients with a high degree of pain intensity prior to the procedure experienced the procedure as a “threat to life or well-being” [7], causing them greater distress. Indeed, there is evidence for a unilateral direction of causation: pain sensation causes pain unpleasantness, not vice versa [16], an experience that we may have seen in our study. Thus, lowering the patient’s pain intensity before a procedure begins could make the procedure less distressful.
Those who had pre-existing anxiety also had greater procedural distress than intensity. Anxiety has long been known to be an important psychological correlate of pain and plays an important role in pain affect/distress [15].
Regarding medications, surprisingly, if patients received pethidine/meperidine prior to the procedure, they reported significantly greater pain distress than intensity during the procedure. This is a counterintuitive finding, as discussed earlier. As noted earlier, we found that when patients received opioids before the procedure, they reported greater pain distress during the procedure.
As noted in our previous report on pain intensity [20], our study had limitations: convenience enrollment, a low acuity ICU sample, considerable variability of sample sizes across the represented countries, and lack of randomization of patients, ICUs, or countries. Our exclusion of patients with delirium, while increasing internal validity, decreases external validity because of the high proportion of ICU patients with delirium [31]. The validity of pain reports from patients with delirium is a very important area for future research focus. Strengths of this study were its prospective design and rigorous standardization of date collection procedures, and it was the largest multinational study of ICU procedural pain conducted. Furthermore, we were able to include patients who were mechanically ventilated which allowed them to be represented in our findings about procedural pain. Indeed, our 37% sample of ventilated patients is actually representative of the percentage of ICU patients, in general, who receive invasive ventilation (approximately 33%) [32]. We found, for the first time, that pain distress, a salient dimension of a person’s pain experience, during procedures is prevalent and that certain procedures cause the greatest distress: ET and tracheal aspiration, chest tube, and wound drain removal, turning, and arterial line insertion. Thus, asking patients to rate their pain distress as well as pain intensity is warranted. Future research is needed that examines interventions to relieve both the intensity and the distress caused by procedural pain. Perhaps a more important first step is to ensure that clinicians understand that assessing pain, including its severity and distress, is the essential first step in managing pain, procedural or otherwise. Many clinicians, including those in ICU, are not receiving adequate pain assessment education [33,34,35], including the important component of pain distress. Clinician recognition of pain distress, as a companion to pain intensity, could serve ICU patients well and negate at least part of the stress of being a patient in an ICU.
Conclusion
In measuring the negative emotional experience of pain during ICU procedures, we found that patients reported more pain distress during procedures than before the procedures. In addition, there are certain factors that increase pain distress and sometimes make distress greater than pain intensity. Although pain intensity and distress may closely covary [7], as we found, there are certain factors than can powerfully and preferentially influence each of the dimensions. Clearly, procedural pain is both a sensory and emotional phenomenon affected by many clinical conditions. While it is impossible to avoid procedures in ICU, it may be possible to decrease the level of associated distress [36] through such simple intervention as providing information to the patient about the procedure they are to undergo [24]. Clinicians are encouraged to appreciate the multidimensionality of pain when they assess their patients’ pain and perform procedures, and to use this knowledge to minimize the pain experiences of their patients.
References
Cazorla C, Cravoisy A, Gibot S, Nace L, Levy B, Bollaert P (2007) Patients’ perception of their experience in the intensive care unit. Presse Med 36(2 Pt 1):211–216
Gelinas C (2007) Management of pain in cardiac surgery ICU patients: have we improved over time? Intensive Crit Care Nurs 3:298–303
Puntillo K, Weiss SJ (1994) Pain: its mediators and associated morbidity in critically ill cardiovascular surgical patients. Nurs Res 43:31–36
Stanik-Hutt JA, Soeken KL, Fontaine DK, Gift AG (2001) Pain experiences of traumatically injured patients in a critical care setting. Am J Crit Care 10:252–259
Chanques G, Sebbane M, Barbotte E, Viel E, Eledjam JJ, Jaber S (2007) A prospective study of pain at rest: incidence and characteristics of an unrecognized symptom in surgical and trauma versus medical intensive care unit patients. J Am Soc Anesthesiol 107:858–860
Puntillo KA, White C, Morris AB, Perdue ST, Stanik-Hutt J, Thompson CL, Wild LR (2001) Patients’ perceptions and responses to procedural pain: results from Thunder Project II. Am J Crit Care 10:238–251
Price DD, Harkins SW, Baker C (1987) Sensory-affective relationships among different types of clinical and experimental pain. Pain 28:297–307
Williams AC, Craig KD (2016) Updating the definition of pain. Pain 157:2420–2423
Henoch I, Sawatyzky R, Falk H, Fridh I, Ung EJ, Sarenmalm EK, Ozanne A, Ohlen J, Falk K (2014) Symptom distress profiles in hospitalized patients in Sweden: a cross-sectional study. Res Nurs Health 37:512–523
Tishelman C, Degner LF, Rudman A, Bertilsson K, Bond R, Broberger E, Dukkali E, Levealahti H (2005) Symptoms in patients with lung carcinoma: distinguishing distress from intensity. Cancer 104:2013–2021
Puntillo KA, Arai S, Cohen NH, Gropper MA, Neuhaus J, Paul SM, Miaskowski C (2010) Symptoms experienced by intensive care unit patients at high risk of dying. Crit Care Med 38:2155–2160
Rotondi AJ, Chelluri L, Sirio C, Mendelsohn A, Schultz R, Belle S, Im K, Donahoe M, Pinsky MR (2002) Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Crit Care Med 30:746–752
Granja C, Gomes E, Amaro A, Ribeiro O, Jones C, Carneiro A, Costa-Pereira A, the JJMIP Study Group (2008) Understanding posttraumatic stress disorder-related symptoms after critical care: the early illness amnesia hypothesis. Crit Care Med 36:2801–2809
Kunz M, Lautenbacher S, LeBlanc N, Rainville P (2012) Are both the sensory and the affective dimensions of pain encoded in the face? Pain 153:350–358
Hemington KS, Cheng JC, Bosma RL, Rogachov A, Kim JA, Davis KD (2017) Beyond negative pain-related psychological factors: resilience is related to lower pain affect in healthy adults. J Pain 18:1117–1128
Price DD (2000) Psychological and neural mechanisms of the affective dimension of pain. Science 288(5472):1769–1772
Rainville P (2002) Brain mechanisms of pain affect and pain modulation. Curr Opin Neurobiol 12:195–204
Ploner M, Freund HJ, Schnitzler A (1999) Pain affect without pain sensation in a patient with a postcentral lesion. Pain 81:211–214
Jensen MP, Karoly P, O’Riordan EF, Bland F, Burns RS et al (1989) The subjective experience of acute pain. An assessment of the utility of 10 indices. Clin J Pain 5:153–159
Puntillo KA, Max A, Timsit JF, Vignoud L, Chaques G, Robleda G et al (2014) Determinants of procedural pain intensity in the intensive care unit. The Europain® study. Am J Respir Crit Care Med 189:39–47
Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA (1978) Studies with pain rating scales. Ann Rheum Dis 37:378–381
Jensen MP, Karoly P, Braver S (1986) The measurement of clinical pain intensity: a comparison of six methods. Pain 27:117–126
Reading AE (1980) A comparison of pain rating scales. J Psychosom Res 24(3–4):119–124
Johnson JE, Rice VH (1974) Sensory and distress components of pain: implications for the study of clinical pain. Nurs Res 23:203–209
Puntillo K, Ley SJ (2004) Appropriately timed analgesics control pain due to chest tube removal. Am J Crit Care 13:292–301 (discussion 302; quiz 303–4)
Voss JA, Good M, Yates B, Baun MM, Thompson A, Hertzog M (2004) Sedative music reduces anxiety and pain during chair rest after open-heart surgery. Pain 112:197–203
Gelinas C, Puntillo KA, Levin P, Azoulay E (2017) The Behavior Pain Assessment Tool for critically ill adults: a validation study in 28 countries. Pain 158:811–821
Yi P, Pryzbylkowski P (2015) Opioid induced hyperalgesia. Pain Med 16(Suppl 1):S32–S36
Guignard B, Bossard AE, Coste C, Sessler DI, Lebrault C (2000) Acute opioid tolerance: intraoperative remifentanil increases postoperative pain and morphine requirement. Anesthesiology 93:409–417
Puntillo K, Gelinas C, Chanques G (2017) Next steps in ICU pain research. Intensive Care Med 43:1386–1388
Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, Truman B et al (2001) Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 286:2703–2710
Canadian Institute for Health Information (2016) Care in Canadian ICU. CIHI, Ottowa
Hoang HT, Sabia M, Torjman M, Goldberg ME (2014) The importance of medical education in the changing field of pain medicine. Pain Manag 4:437–443
Sabia M, Weaver M, Gessman R, Kalariya J (2017) Update on the importance of medical education if the changing field of pain medicine. J Anesth Patient Care 2:1–5
Seers T, Derry S, Kate Seers K, Moore RA (2018) Professionals underestimate patients’ pain: a comprehensive review. Pain 159:811–818
Shaw S, Lamdin R (2011) Nurses have an ethical imperative to minimise procedural pain. Nurs N Z 17:12–14
Acknowledgements
Contributors: We recognize and thank patients and clinicians from the following ICUs who were involved in the Europain® study. (1) Medical Intensive Care Unit, University of Paris-Diderot, Saint Louis Hospital, Paris, France; (2) Medical Intensive Care Unit, Bichat University Hospital, France; (3) Institut Albert Bonniot, INSERM U823, Grenoble, France; (4) Département d’Anesthésie-Réanimation, Hôpital Saint Eloi, France; (5) Unite U1046 de l’Institut National de la Sante et de la Recherche, University of Montpellier, Montpellier, France; (6) Servei de Medicina Intensiva, Hospital de Sant Pau, Barcelona, Spain; (7) Anaesthesia, Critical Care and Pain, Tata Memorial Hospital, Mumbai, India; (8) D’Or Institute for Research Education, Postgraduate Program, Instituto Nacional de Cancer, Rio de Janeiro, Brazil; (9) Department of Anesthesia and Intensive Care I, Iuliu Hatieganu University of Medicine and Pharmacy, Cluj-Napoca, Romania; (10) Anesthesia and Intensive Care Department, Clinical Emergency Hospital, Bucharest, Romania; (11) Department of Anesthesiology and Intensive Care, Policlinico A. Gemelli, Università Cattolica del Sacro Cuore, Rome, Italy; (12) Department of Anaesthesiology and Intensive Care, General University Hospital, First Faculty of Medicine of Charles University, Prague, Czech Republic; (13) Department of Anaesthesiology and Intensive Therapy, Medical University of Gdansk, Gdansk, Poland; (14) Trauma Centre, Copenhagen University Hospital Rigshospitalet, Copenhagen, Denmark; (15) Department of Nursing, Cyprus University of Technology, Nicosia, Cyprus; (16) Nursing Department, Papageorgiou Hospital, Thessaloniki, Greece; (17) The Chinese University of Hong Kong, Department of Anaesthesia and Intensive Care, Prince of Wales Hospital, Shatin, Hong Kong; (18) Intensive Care Unit, Hospital Maciel, Santorio Americano and Sanatorio Hospital in Montevideo, Montevideo, Uruguay; (19) Intensive Care Services, Hawke’s Bay Hospital, Hastings, New Zealand; (20) Department of Intensive Care Medicine and School of Population Health, Royal Perth Hospital and University of Western Australia, Perth, Australia; (21) Trauma ICU and CCU of Helsinki University Hospital, Helsinki, Finland; ICU of Kuopio University Hospital, Finland; ICU of Oulu University Hospital, Finland; (22) Department of Intensive Care, Medical Centre Leeuwarden, Netherlands; (23) Department of Intensive Care Medicine, University Medical Center, Utrecht, Netherlands; (24) Clinic of Anesthesiology and Intensive Medicine, Jessenius Faculty of Medicine in Martin-Comenius University in Bratislava, University Hospital Martin, Martin, Slovakia; (25) Intensive Care Unit Department, Erasme Hospital, Belgium; (26) Department of Intensive Care, Erasme University Hospital, Université Libre de Bruxelles, Brussels, Belgium; (27) ICU Maennedorf, Spital Maennedorf, Maennedorf, Switzerland; (28) ICU Department, Khoula Hospital, Muscat, Sultanate of Oman; (29) Intensive Care Unit of Clinica Las Americas, Medellin, Columbia; (30) ICU, Neurosurgery, Medical ICU, Hadassah Hebrew University Hospital, Jerusalem, Israel; (31) Intensive Care Unit, CHU F. Bourguiba, Monastir, Tunisia; (32) Department of Anaesthesia and Intensive Care, Mater Dei Hospital, Msida, Malta; (33) Servico Cuidados Intensivos, Hospital Santo Antonio, Centro Hospitalar do Porto, Porto, Portugal; and (34) Department of Critical Care Medicine, Peking University People’s Hospital, Beijing, China.
Funding
Supported by a grant from the European Society of Intensive Care Medicine/European Critical Care Research Network Award (ECCRN Established Investigator Award, 2009) and by an academic grant from AP-HP, Hôpital Saint-Louis, Paris, France.
Author information
Authors and Affiliations
Contributions
KAP, EA, AM, study concept and design. KAP, AM, EA, training materials. KAP, EA, JFT, SR, data analysis and interpretation. KAP, EA, JFT, SR, manuscript preparation and drafting. KAP, EA, JFT, SR, statistical methods, statistical data analysis. AM, GC, GR, JM, FRC, JVD, MS, DCI, IMG, SMM, KR, RO, IE, EDEP, MK, GMJ, GB, RCF, KMH, AK, RTG, JK, MMSS, MN, DDB, MSGS, AH, FJP, JSB, FA, AA, JRCM, YA, acquisition of the data and manuscript critique and review. All authors approved the manuscript submitted.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Puntillo, K.A., Max, A., Timsit, JF. et al. Pain distress: the negative emotion associated with procedures in ICU patients. Intensive Care Med 44, 1493–1501 (2018). https://doi.org/10.1007/s00134-018-5344-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-018-5344-0