Abstract
Purpose
We assessed the effects of a protocol restricting resuscitation fluid vs. a standard care protocol after initial resuscitation in intensive care unit (ICU) patients with septic shock.
Methods
We randomised 151 adult patients with septic shock who had received initial fluid resuscitation in nine Scandinavian ICUs. In the fluid restriction group fluid boluses were permitted only if signs of severe hypoperfusion occurred, while in the standard care group fluid boluses were permitted as long as circulation continued to improve.
Results
The co-primary outcome measures, resuscitation fluid volumes at day 5 and during ICU stay, were lower in the fluid restriction group than in the standard care group [mean differences −1.2 L (95 % confidence interval −2.0 to −0.4); p < 0.001 and −1.4 L (−2.4 to −0.4) respectively; p < 0.001]. Neither total fluid inputs and balances nor serious adverse reactions differed statistically significantly between the groups. Major protocol violations occurred in 27/75 patients in the fluid restriction group. Ischaemic events occurred in 3/75 in the fluid restriction group vs. 9/76 in the standard care group (odds ratio 0.32; 0.08–1.27; p = 0.11), worsening of acute kidney injury in 27/73 vs. 39/72 (0.46; 0.23–0.92; p = 0.03), and death by 90 days in 25/75 vs. 31/76 (0.71; 0.36–1.40; p = 0.32).
Conclusions
A protocol restricting resuscitation fluid successfully reduced volumes of resuscitation fluid compared with a standard care protocol in adult ICU patients with septic shock. The patient-centred outcomes all pointed towards benefit with fluid restriction, but our trial was not powered to show differences in these exploratory outcomes.
Trial registration
NCT02079402.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fluid resuscitation is the mainstay of cardiovascular interventions for patients with septic shock [1]. Intravenous fluid may improve the circulation and organ perfusion by increasing cardiac output, but may also be associated with harmful effects through peripheral and organ oedema. The exact physiology of fluid resuscitation and the relation to patient-centred outcomes are, however, not yet fully elucidated.
In the clinical practice guideline for adults with septic shock, it is recommended to give a minimum of 30 mL/kg of crystalloid solutions during initial resuscitation and to continue to give fluids as long as the circulation improves [1]. However, there are limited high-quality data supporting these recommendations [1]; increased cumulative fluid balances at 12 h and 4 days have been associated with increased mortality in adult patients with septic shock [2] and, similarly, increased daily fluid balances from day 2 until day 7 have been associated with increased mortality in septic shock in adjusted analyses [3]. In addition, a large randomised trial showed increased mortality in febrile African children with circulatory impairment who received fluid boluses in addition to maintenance fluid as compared to those who received maintenance alone [4].
Taken together, current guidelines on volumes of resuscitation fluid in septic shock are based on low-quality evidence, and it is possible that higher fluid volumes may harm these patients. Therefore, we designed the Conservative vs. Liberal Approach to fluid therapy of Septic Shock in Intensive Care (CLASSIC) trial with the objective to assess the feasibility and effects of a protocol restricting resuscitation fluid after initial resuscitation on fluid volumes and balances and explorative outcome measures in intensive care unit (ICU) patients with septic shock. We focused on volumes of resuscitation fluid, rather than total fluid inputs or fluid balances, because resuscitation fluid is given with the specific aim to improve the circulation. Resuscitation fluid is, therefore, likely to have a different balance between benefit and harm than that of fluids given as maintenance or with nutrition and medications.
Methods
Trial design and conduct
The management committee wrote the trial protocol, which was approved by the Medicines Agency, Ethics Committee and Data Protection Agency in Denmark and the Ethics Committee in Helsinki, Finland. The protocol and the statistical analysis plan, which were written before closing the trial database, are provided in the Electronic Supplementary Material (ESM) 2. The trial was registered at http://www.clinicaltrials.gov (number NCT02079402) before enrolment of the first patient and conducted according to Good Clinical Practice (EU Directive 2001/20) including monitoring of consents and source data by external staff.
The CLASSIC trial was an investigator-initiated, multicentre, stratified (by site because these may influence volumes of resuscitation fluid [5]), parallel-group clinical trial with adequate computer generation of the allocation sequence with permuted blocks of varying sizes of 2 or 4 and allocation concealment by a Web-based, centralised randomisation system. We randomised patients with septic shock in nine general ICUs 1:1 to restrictive fluid resuscitation or standard care. The allocation was blinded for the statistician.
In Denmark, informed consent was obtained from two physicians who were independent of the trial prior to randomisation. In Finland, deferred consent was used. In all cases informed consent was obtained from the next of kin and the patient as soon as possible after randomisation. If consent was withdrawn or not granted, permission was asked for continued registration and use of data.
Patients
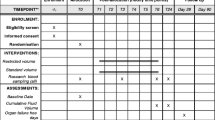
We screened patients aged 18 years or above (1) who were in the ICU, (2) who fulfilled the criteria for sepsis within the previous 24 h, (3) who had suspected or confirmed severe circulatory impairment—defined as systolic blood pressure below 90 mmHg, heart rate above 140 beats/min, lactate at least 4 mmol/L, or use of vasopressors—for no more than 12 h including the hours preceding ICU admission, (4) who had received at least 30 mL/kg ideal body weight (IBW) of fluid in the last 6 h, and (5) who had shock defined as ongoing infusion of norepinephrine to maintain blood pressure (the detailed trial definitions, including those regarding a change during trial in the definition of criterion 3, are provided in ESM 1 and ESM 2). Patients were excluded for the reasons shown in Fig. 1.
Flow of trial participants in the CLASSIC trial. Patients with septic shock assessed, excluded, randomised and followed up in the CLASSIC trial. Twelve patients fulfilled 2 or 3 exclusion criteria. Two patients were excluded post-randomisation in the recruitment period because they withdrew consent for the use of data. Two additional patients were randomised to obtain the full sample size of 150 patients. One additional patient was randomised within an hour of the randomisation of patient no. 150 before the Web-based randomisation portal was closed. RRT renal replacement therapy, PEEP positive end-expiratory pressure
Interventions
In both intervention groups, use of resuscitation fluid was per protocol and mean arterial pressure (MAP) of at least 65 mmHg (or a target decided by the clinicians) was maintained by the use of continuous infusion of norepinephrine. The choice of crystalloid solutions was at the discretion of the treating clinicians, but the use of colloid solutions for resuscitation was regarded as a protocol violation to alleviate the risk of differences in the type of fluid administered between the intervention groups. Suggestions for the use of selected co-interventions were provided, including fluid therapy for other indications than resuscitation (ESM 1); substitution of overt fluid loss was allowed in both groups.
In the fluid restriction group, isotonic crystalloid (saline or Ringer’s solutions) fluid boluses of 250–500 mL could be given intravenously during ICU stay in the case of severe hypoperfusion defined as either (1) plasma concentration of lactate of at least 4 mmol/L, (2) MAP below 50 mmHg in spite of the infusion of norepinephrine, (3) mottling beyond the edge of the kneecap (mottling score greater than 2) [6], or (4) oliguria, but only in the first 2 h after randomisation, defined as urinary output at most 0.1 mL/kg IBW in the last hour. The cut-off value of lactate was chosen on the basis of Surviving Sepsis Campaign (SSC) guidelines [1] and data indicating that a marked increase in mortality occurs at lactate values above 4 mM [7]. Fulfilment of at least one of these criteria was a prerequisite for administration of a fluid bolus, but administration was not mandated. The effect of a fluid bolus was to be assessed by re-evaluation of the four hypoperfusion criteria mentioned above before a repeated fluid bolus or after 30 min at the latest.
In the standard care group, isotonic crystalloid (saline or Ringer’s solutions) fluid boluses could be given intravenously during ICU stay as long as haemodynamic variables improved including dynamic (e.g. stroke volume variation) or static (e.g. blood pressure, heart rate) variable(s) of the clinician’s choice as outlined in the SSC guideline [1]. The effect of a fluid bolus was to be assessed by re-evaluation before a repeated fluid bolus or after 30 min at the latest.
Outcome measures
The co-primary outcomes were the amount of resuscitation fluid (defined as the cumulated volumes of 0.9 % saline, Ringer’s lactate, Ringer’s acetate and colloid solutions given in the ICU for circulatory impairment as noted by the clinicians) in the first 5 days after randomisation and the amount of resuscitation fluid given after randomisation during the entire ICU stay. The latter was promoted from a secondary outcome to a co-primary outcome during the trial so that the full intervention period was reflected in the primary outcome. This change was done before the data were available for analyses. The details about this protocol change and the full definitions of all outcomes are provided in ESM 1 and in the trial protocol (ESM 2).
The secondary outcome measures were total fluid input given in the ICU at day 5 after randomisation and during the entire ICU stay, fluid balance in ICU at day 5 after randomisation and for entire ICU stay, number of patients with violations of the fluid resuscitation protocol, and rates of serious adverse reactions for isotonic crystalloids or norepinephrine in the ICU.
Exploratory outcomes were death within 90 days after randomisation, time to death with censoring 90 days after the last patient had been randomised, days alive without the use of mechanical ventilation or renal replacement therapy in the 90-day period, the number of patients with ischaemic events during the ICU stay, maximum change in plasma creatinine during the ICU stay, and number of patients with worsening of acute kidney injury (AKI) according to the KDIGO criteria [8] (values of plasma creatinine were assessed in ICU and the use of renal replacement therapy in the 90 days after randomisation; the urinary output criteria were not assessed). For patients without AKI at baseline, development of AKI after randomisation was regarded as worsening of AKI.
Statistical analysis
One hundred and fifty patients were needed to show a 1.7-L difference in volumes of resuscitation fluid within the first 5 days between the groups on the basis of the mean volume of resuscitation fluid observed in the 6S trial [5.3 L (standard deviation 3.7 L)] [9], an alpha of 5 % (two-sided) and a power of 80 %. The implications for the sample size estimation of the change from one to two co-primary outcomes are provided in the statistical analysis plan in the trial protocol (ESM 2).
In the recruitment period we excluded two patients after randomisation because they withdrew consent for the use of data. We randomised two additional patients to obtain the full sample size. One additional patient was randomised within an hour of patient no. 150 before the randomisation portal was closed (Fig. 1).
The statistician (P.W.) performed all the analyses blinded for the intervention and according to the ICH-GCP guidelines E9 [10] and the statistical analysis plan, in which the handling of missing data is also described (ESM 2). We performed the analyses in the intention-to-treat population defined as all randomised patients except those who withdrew consent for the use of data. We defined the per-protocol population as all patients in the intention-to-treat population except those who had a protocol violation (Table S1 in ESM 1).
In the primary analyses, we compared data in the two groups by the non-parametric van Elteren test or the general linear model for ordinal and rate data adjusted for the stratification variable (trial site) [10], logistic regression analysis for binary outcome measures adjusted for site and by logrank test and Cox analysis (adjusted for site) for time to death. Sites including less than 10 patients were grouped in the adjusted analyses. We also compared the co-primary outcomes in an analysis adjusted for predefined risk factors at baseline (age, weight, norepinephrine dose at randomisation, surgery prior to randomization and more than 5 L of fluid given prior to randomization), in the per-protocol population and in the predefined subgroup analysis of patients who had received more than 5 L of fluid (crystalloids, colloids, and blood products) in the 24-h prior to randomisation. We performed all analyses using SAS software, version 9.3, and SPSS software, version 17.0. Multiplicity issues were addressed for the co-primary outcomes. We adjusted the level of significance by a factor in between a full Bonferroni adjustment and no adjustment at all, because we expected a degree of correlation between the two outcomes; thus, we considered a two-sided P value of 0.05/1.5 = 0.033 to indicate statistical significance. For the remaining outcome measures, we considered a two-sided P value of less than 0.05 to indicate statistical significance.
Results
Patients
Between September 2014 and August 2015 we assessed 203 patients who fulfilled the inclusion criteria and randomised 153 (75 %) of those (Fig. 1; Fig. 4 in ESM 1); 76 patients were allocated to the fluid restriction group and 77 to the standard care group. One patient in each group withdrew consent for the use of data, thus we analysed data from 151 patients (99 %). Patient characteristics and fluid administration are presented in Table 1 and Table S2 in ESM 1; there appeared to be a degree of imbalance between the two groups for some characteristics, including the rates of pulmonary focus of sepsis and AKI and patient weight.
Fluid protocol
Fifty-five of 75 patients (73 %) in the fluid restriction group vs. 70 of 76 patients (92 %) in the standard care group (P = 0.002) received resuscitation fluid during 286 vs. 464 episodes (P = 0.003) after randomisation. In the fluid restriction group, the resuscitation fluids were administered mainly on the first day after randomisation; in the standard care group, the majority of patients received resuscitation fluid until day 4 (Tables S3, S4 in ESM 1). Resuscitation fluid was given as Ringer’s solutions rather than saline in the majority of patients in both groups (Table S4 in ESM 1).
No patients had the fluid resuscitation protocol temporarily suspended (Table S5 in ESM 1), but two patients in each group had the protocol discontinued on the request of surrogates (Fig. 1). Additional details regarding fluid indications, types and timing, co-interventions, haemodynamic variables, and urinary outputs are provided in Tables S3–S11 and Figs. 5–7 in ESM 1.
Primary outcome measures
Cumulated resuscitation fluid volumes given in the ICU at day 5 after randomisation and during the entire ICU stay (the co-primary outcomes) were lower in the fluid restriction group vs. the standard care group [mean differences −1.2 L (95 % CI −2.0 to −0.4); P < 0.001 and −1.4 L (95 % CI −2.4 to −0.4); P < 0.001, respectively (Table 2; Fig. 2)]. We obtained similar results in the analyses adjusted for the predefined risk factors at baseline, in the per-protocol population (Tables S12, S13 in ESM 1), and in the subgroup analysis of patients who had received more than 5 L of fluid in the 24 h prior to randomisation (P = 0.91 for interaction between subgroup and intervention).
Percentiles of resuscitations fluids (the primary outcome) given in the restriction group and standard care group after randomisation. Resuscitation fluid was defined as the cumulated volumes of 0.9 % saline, Ringer’s lactate, Ringer’s acetate and colloid solutions given for circulatory impairment as noted by the clinicians. Lower volumes of resuscitation fluid were given after randomisation in the first 5 days in ICU (p < 0.001) and during the entire ICU stay (p < 0.001) in the fluid restriction group vs. the standard care group. More detailed analyses are presented in Table 2
Secondary outcome measures
Total fluid inputs and balances in the ICU did not differ with statistical significance between groups either at day 5 after randomisation or during the entire ICU stay (Table 2; Figs. 5, 6 in ESM 1). In the fluid restriction group, 27 of the 75 patients (36 %, 95 % CI 25–47) had a total of 80 violations of the fluid resuscitation protocol (Fig. 8 in ESM 1). The rates of serious adverse reactions to fluids or norepinephrine did not differ between the two intervention groups (Table 2; Table S14 in ESM 1).
Exploratory outcome measures
Death at day 90 (Fig. 3), time to death at latest follow-up (Fig. 3), number of patients with ischaemic events in ICU (Fig. 3; Table S15 in ESM 1), days alive without mechanical ventilation (mean 79 vs. 72 %, P = 0.48) or renal replacement therapy (92 vs. 92 %, P = 0.70) in the 90-day follow-up period or maximum changes in plasma creatinine in the ICU (median 9 (IQR −13 to 47) vs. 15 (−4 to 62) µmol/L, P = 0.36) did not differ with statistical significance between the fluid restriction group and the standard care group. The number of patients with worsening of acute kidney injury in the 90-day period was lower in the fluid restriction group than in the standard care group (Fig. 3; Fig. 10 in ESM 1).
Exploratory outcome measures. a Odds ratios (black boxes) with 95 % confidence intervals (horizontal lines) for the binary explorative outcomes in the fluid restriction group vs. the standard care group as assessed by logistic regression analyses with adjustment for the stratification variable (trial site). Ischaemic events were defined as at least one of the following during ICU stay: intestinal, limb, ischaemia or myocardial ischaemia. Worsening acute kidney injury (AKI) was defined as worsening of the KDIGO stage (plasma creatinine criteria or use of renal replacement therapy). A total of 6 patients (4 %) had either missing baseline plasma creatinine or did not have any plasma creatinine measurements during ICU stay—these patients were not included in the above complete case analysis. Since p of Little’s test was less than 0.001 and one auxiliary variable (rate of serious adverse reactions) was highly correlated (|r| = 0.53) with worsening of KDIGO we did multiple (monotone) imputation. The results were comparable to that of the complete case analysis including that of the inference (p = 0.03). On the request of reviewers, we conducted a post hoc sensitivity analysis excluding patients with KDIGO stage 3 at baseline from the analysis of worsening of AKI; excluding these patients, 27/66 vs. 39/68 had worsening of AKI in the fluid restriction group vs. standard care group [odds ratio 0.52 (95 % confidence interval (CI) 0.26–1.02; p = 0.058)]. b Survival curves and the number of patients at risk censored at the time of follow-up of the last randomised patient (4 November 2015) for the two intervention groups. The median time of follow-up was 262 days (interquartile range 173–326). P of the logrank test was 0.77. Using the Cox analysis adjusted by the stratification variable (site) the hazard ratio between the fluid restriction group and the standard care group was 0.89 (CI 0.54–1.45; p = 0.64)
Discussion
We observed that a protocol aimed at restricting resuscitation fluid vs. a protocol aimed at standard care after initial resuscitation of ICU patients with septic shock resulted in lower volumes of resuscitation fluid in the first 5 days and during the entire ICU stay in this binational, multicentre randomised trial. This difference in volumes of resuscitation fluid did not affect fluid balances or rates of serious adverse reactions, use of mechanical ventilation or renal replacement therapy, ischaemia, or death with statistical significance. The number of patients with worsening acute kidney injury appeared to be lower in the fluid restriction group as compared to the standard care group. However, our trial was not powered to show differences in any of these outcomes.
Fluid resuscitation is complex in patients with septic shock and may be influenced by setting, timing, use of haemodynamic triggers and targets and co-interventions as well as focus of infection and co-morbidities [11–13]. The current guideline is based on low level of evidence and recommends a minimum of 30 mL/kg followed by continued fluid resuscitation as long as haemodynamic variables improve [1]. Our fluid restriction protocol challenged in particular the latter part of the guideline. We enrolled ICU patients who had received the 30 mL/kg and observed a median 4.5 L of fluid given prior to randomisation, volumes that are similar to the total fluid volumes given at the end of the 6-h intervention period in the recent early goal-directed therapy trials [14–17]. The patients in those trials were enrolled in emergency departments before any transfer to ICU. In the ICU setting after the initial resuscitation, our fluid restriction protocol resulted in marked reduction in volumes of resuscitation fluid as compared with our standard care protocol where use of resuscitation fluids was continued for some days after randomisation.
We observed lower numbers of patients with worsening acute kidney injury in the fluid restriction group as compared with the standard care group in the exploratory analyses. This may seem counterintuitive; fluids are, in fact, often given by ICU clinicians for oliguria [18]. Our trial was relatively small, and chance or baseline imbalance, including the rates of pulmonary focus of sepsis and AKI at baseline, may have contributed to our results. On the other hand, the results of the recent PROCESS (Protocol-based Care for Early Septic Shock) trial indicated higher volumes of resuscitation fluid given and higher rates of new-onset acute kidney injury in the protocol-based standard therapy group as compared with the early goal-directed therapy group and the usual care group [14]. In two recent cohort studies adherence to the SSC resuscitation bundle, which included administration of a minimum of 30 mL/kg of crystalloids early in septic shock, was associated with improved survival [19, 20]. The interpretation of these data may not conflict that of our data, because our patients had received 30 mL/kg of fluid at enrolment. The results of other cohort studies have associated higher fluid balances in the first days of ICU stay with worse outcomes in patients with sepsis, including those with acute kidney injury [2, 21, 22]. We did not observe statistically significant differences in total fluid input or balances at day 5 most likely because of the large variations in these volumes. Of note, the pretrial power estimation for the detectable difference in total fluid input was more than twofold higher than that of resuscitation fluid. Because we only intervened in administration of resuscitation fluids, statistically significant differences in total fluid inputs were not expected. Also, the observed point estimates for total inputs were similar to those for the volumes of resuscitation fluids. In any case, it is difficult to compare the potential benefits and harms of fluids given for resuscitation and mainly given early with fluids as maintenance and with nutrition and medications during the entire ICU stay. Taken together there is evidence to suggest that lower volumes of resuscitation fluid improve outcomes as compared to higher fluid volumes in patients with septic shock, and to our knowledge there are no high-quality data supporting use of higher fluid volumes in these patients. Given these uncertainties and the abundant use of fluid in patients with septic shock, additional high-quality trials are needed to assess the effects on patient-centred outcomes of protocols aimed at restricting volumes of resuscitation fluid in these patients. Our results indicate that it is feasible to protocolize and restrict resuscitation fluids across multiple ICUs.
Our trial has limitations. The trial was designed to show differences in volumes of resuscitation fluid and was, therefore, relatively small; we could not mask the intervention for investigators, clinicians and patients; and there may have been some baseline imbalance and differences in co-interventions between the two groups. All these factors may have affected the results. Administration of at least 30 mL/kg of fluid had to be documented prior to inclusion, which may have resulted in selection of specific patient groups. Thus, we may have included more surgical patients than was done in other recent ICU trials in septic shock [23–25]. Use of colloids for circulatory impairment was not allowed in both groups, which might have reduced the external validity of our results. Additionally, we observed a relatively high number of protocol violations, including the administration of resuscitation fluid to patients who did not fulfil the criteria in the fluid restriction group, which reduces the internal and external validity of our results. Also, albumin was administered for circulatory impairment in both groups. In general, protocol violations may be difficult to avoid in trials of complex interventions in ICU [9, 23, 25], and despite these protocol violations we observed separation in resuscitation fluid volumes between the two intervention groups. Potential measures to lessen the number protocol violations in a large-scale trial include promoting the results of the present trial, which did not indicate safety concerns, and allowing resuscitation fluid in the restriction group on the basis of tachycardia and a lower lactate threshold.
The strengths of our trial include lower risk of bias as group allocation was concealed and the statistician adhered to the predefined statistical analysis plan while blinded to the intervention. It is reasonable to assume that our results are generalizable, because patients were recruited in both university and non-university hospitals and the majority of patients screened were included. In addition, most patient characteristics and outcome rates were comparable to those of some recent trials in ICU patients with septic shock [23–25].
In conclusion, a protocol aimed at restricting resuscitation fluid was feasible and resulted in reduced volumes of resuscitation fluid as compared with a protocol aimed at standard care in ICU patients with septic shock who had undergone initial resuscitation. As the exploratory outcomes suggested benefit from fluid restriction and fluid is abundantly used in septic shock, we need large, high-quality trials assessing benefits vs. harms of lower vs. higher volumes of resuscitation fluid in these patients.
References
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R (2013) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39:165–228
Boyd JH, Forbes J, Nakada TA, Walley KR, Russell JA (2011) Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med 39:259–265
Acheampong A, Vincent JL (2015) A positive fluid balance is an independent prognostic factor in patients with sepsis. Crit Care 19:251
Maitland K, Kiguli S, Opoka RO, Engoru C, Olupot-Olupot P, Akech SO, Nyeko R, Mtove G, Reyburn H, Lang T, Brent B, Evans JA, Tibenderana JK, Crawley J, Russell EC, Levin M, Babiker AG, Gibb DM (2011) Mortality after fluid bolus in African children with severe infection. N Engl J Med 364:2483–2495
Hjortrup PB, Haase N, Wetterslev J, Perner A (2016) Associations of hospital and patient characteristics with fluid resuscitation volumes in patients with severe sepsis: post hoc analyses of data from a multicentre randomised clinical trial. PLoS One 11:e0155767
Ait-Oufella H, Lemoinne S, Boelle PY, Galbois A, Baudel JL, Lemant J, Joffre J, Margetis D, Guidet B, Maury E, Offenstadt G (2011) Mottling score predicts survival in septic shock. Intensive Care Med 37:801–807
Wacharasint P, Nakada TA, Boyd JH, Russell JA, Walley KR (2012) Normal-range blood lactate concentration in septic shock is prognostic and predictive. Shock 38:4–10
Kellum JA, Lameire N (2013) Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit Care 17:204
Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Aneman A, Madsen KR, Moller MH, Elkjaer JM, Poulsen LM, Bendtsen A, Winding R, Steensen M, Berezowicz P, Soe-Jensen P, Bestle M, Strand K, Wiis J, White JO, Thornberg KJ, Quist L, Nielsen J, Andersen LH, Holst LB, Thormar K, Kjaeldgaard AL, Fabritius ML, Mondrup F, Pott FC, Moller TP, Winkel P, Wetterslev J (2012) Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med 367:124–134
ICH Steering Committee (1998) International conference on harmonisation of technical requirements for registration of pharmaceuticals for human use. ICH Harmonised Tripartite Guideline for Statistical Principles for Clinical Trials, 3rd edn. Brookwood Medical Publications, London
Seymour CW, Rosengart MR (2015) Septic shock: advances in diagnosis and treatment. JAMA 314:708–717
Perner A, Vieillard-Baron A, Bakker J (2015) Fluid resuscitation in ICU patients: quo vadis? Intensive Care Med 41:1667–1669
Myburgh JA, Mythen MG (2013) Resuscitation fluids. N Engl J Med 369:1243–1251
Yealy DM, Kellum JA, Huang DT, Barnato AE, Weissfeld LA, Pike F, Terndrup T, Wang HE, Hou PC, LoVecchio F, Filbin MR, Shapiro NI, Angus DC (2014) A randomized trial of protocol-based care for early septic shock. N Engl J Med 370:1683–1693
Peake SL, Delaney A, Bailey M, Bellomo R, Cameron PA, Cooper DJ, Higgins AM, Holdgate A, Howe BD, Webb SA, Williams P (2014) Goal-directed resuscitation for patients with early septic shock. N Engl J Med 371:1496–1506
Mouncey PR, Osborn TM, Power GS, Harrison DA, Sadique MZ, Grieve RD, Jahan R, Harvey SE, Bell D, Bion JF, Coats TJ, Singer M, Young JD, Rowan KM (2015) Trial of early, goal-directed resuscitation for septic shock. N Engl J Med 372:1301–1311
Angus DC, Barnato AE, Bell D, Bellomo R, Chong CR, Coats TJ, Davies A, Delaney A, Harrison DA, Holdgate A, Howe B, Huang DT, Iwashyna T, Kellum JA, Peake SL, Pike F, Reade MC, Rowan KM, Singer M, Webb SA, Weissfeld LA, Yealy DM, Young JD (2015) A systematic review and meta-analysis of early goal-directed therapy for septic shock: the ARISE, ProCESS and ProMISe Investigators. Intensive Care Med 41:1549–1560
Cecconi M, Hofer C, Teboul JL, Pettila V, Wilkman E, Molnar Z, Della RG, Aldecoa C, Artigas A, Jog S, Sander M, Spies C, Lefrant JY, De BD (2015) Fluid challenges in intensive care: the FENICE study: a global inception cohort study. Intensive Care Med 41:1529–1537
Levy MM, Rhodes A, Phillips GS, Townsend SR, Schorr CA, Beale R, Osborn T, Lemeshow S, Chiche JD, Artigas A, Dellinger RP (2014) Surviving Sepsis Campaign: association between performance metrics and outcomes in a 7.5-year study. Intensive Care Med 40:1623–1633
Rhodes A, Phillips G, Beale R, Cecconi M, Chiche JD, De Backer D, Divatia J, Du B, Evans L, Ferrer R, Girardis M, Koulenti D, Machado F, Simpson SQ, Tan CC, Wittebole X, Levy M (2015) The Surviving Sepsis Campaign bundles and outcome: results from the International Multicentre Prevalence Study on Sepsis (the IMPreSS study). Intensive Care Med 41:1620–1628
Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Jr Le Gall, Payen D (2006) Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 34:344–353
Vaara ST, Korhonen AM, Kaukonen KM, Nisula S, Inkinen O, Hoppu S, Laurila JJ, Mildh L, Reinikainen M, Lund V, Parviainen I, Pettila V (2012) Fluid overload is associated with an increased risk for 90-day mortality in critically ill patients with renal replacement therapy: data from the prospective FINNAKI study. Crit Care 16:R197
Holst LB, Haase N, Wetterslev J, Wernerman J, Guttormsen AB, Karlsson S, Johansson PI, Aneman A, Vang ML, Winding R, Nebrich L, Nibro HL, Rasmussen BS, Lauridsen JR, Nielsen JS, Oldner A, Pettila V, Cronhjort MB, Andersen LH, Pedersen UG, Reiter N, Wiis J, White JO, Russell L, Thornberg KJ, Hjortrup PB, Muller RG, Moller MH, Steensen M, Tjader I, Kilsand K, Odeberg-Wernerman S, Sjobo B, Bundgaard H, Thyo MA, Lodahl D, Maerkedahl R, Albeck C, Illum D, Kruse M, Winkel P, Perner A (2014) Lower versus higher hemoglobin threshold for transfusion in septic shock. N Engl J Med 371:1381–1391
Caironi P, Tognoni G, Masson S, Fumagalli R, Pesenti A, Romero M, Fanizza C, Caspani L, Faenza S, Grasselli G, Iapichino G, Antonelli M, Parrini V, Fiore G, Latini R, Gattinoni L (2014) Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med 370:1412–1421
Asfar P, Meziani F, Hamel JF, Grelon F, Megarbane B, Anguel N, Mira JP, Dequin PF, Gergaud S, Weiss N, Legay F, Le TY, Conrad M, Robert R, Gonzalez F, Guitton C, Tamion F, Tonnelier JM, Guezennec P, Van Der Linden T, Vieillard-Baron A, Mariotte E, Pradel G, Lesieur O, Ricard JD, Herve F, du CD, Guerin C, Mercat A, Teboul JL, Radermacher P (2014) High versus low blood-pressure target in patients with septic shock. N Engl J Med 370:1583–1593
Acknowledgments
The CLASSIC trial was funded by the Danish Medical Research Council (09-066938) and supported by Rigshospitalets Research Council, the Scandinavian Society of Anaesthesiology and Intensive Care Medicine (the ACTA Foundation) and the Ehrenreich Foundation. The funders of the study had no influence on the design or conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. We are grateful to the clinical staff of doctors and nurses at the participating ICUs for their important contribution and to patients and relatives for their consent to participate.
The CLASSIC trial investigators
Management Committee: Peter B. Hjortrup, Anders Perner (Chair), Nicolai Haase and Jørn Wetterslev.
Trial site investigators (in Denmark unless otherwise specified): Rigshospitalet: P.B. Hjortrup, A. Perner, N. Haase, K.R. Uhre, L.H. Nislev, L. Russell, C. Claudius, U.G. Pedersen, M.B. Madsen, M.H. Møller, M. Ibsen, K. Thornberg, F. Sjövall, F. Mondrup, H.C. Thorsen-Meyer, L. Quist, L. Vestergaard, C. Lund, J. Wiis, R. Hein-Rasmussen, C.P. Holler, J.O. White, S. Asghar; Randers Hospital: H. Bundgaard, D. Flye, K. Knudsen, B. Hougaard; Aalborg Hospital: B.S. Rasmussen, S.L. Thomsen, S.N. Granum; Herning Hospital: R. Winding, S. Haubjerg, L. Friholdt, N. Dey, M. Nygaard; Holbæk Hospital: H.H. Bülow, J.M. Elkjær, A. Aaen, S. Grangaard, L. Christensen, M. Hjort, S. Larsen; Helsinki University Hospital, Finland: V. Pettilä, E. Wilkman, M. Valkonen, S. Sutinen, L. Pettilä; Holstebro Hospital: D. Lodahl, R.V.M. Andersen; Nordsjællands Hospital: R.E. Berthelsen, M. Bestle, S. Lauritzen, L. Valbjørn; Herlev Hospital: H. Christensen.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
The Department of Intensive Care, Rigshospitalet receives research funds from CSL Behring, Switzerland, Fresenius Kabi, Germany, and Ferring Pharmaceuticals, Denmark.
Additional information
The members of the CLASSIC Trial Group are listed in the Acknowledgments.
Take-home message: A fluid restriction protocol in septic shock resulted in less resuscitation fluid being given to fewer patients. The patient-centred outcomes all pointed towards benefit with fluid restriction, but our trial was not powered to show differences in these exploratory outcomes.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hjortrup, P.B., Haase, N., Bundgaard, H. et al. Restricting volumes of resuscitation fluid in adults with septic shock after initial management: the CLASSIC randomised, parallel-group, multicentre feasibility trial. Intensive Care Med 42, 1695–1705 (2016). https://doi.org/10.1007/s00134-016-4500-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-016-4500-7