Abstract
Purpose
Statins, 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors have the potential to reduce acute kidney injury (AKI) after cardiac surgery through their pleiotropic properties. Here we studied the preventive effect of atorvastatin on AKI after valvular heart surgery.
Methods
Two-hundred statin-naïve patients were randomly allocated to receive either statin or placebo. Atorvastatin was administered orally to the statin group according to a dosage schedule (80 mg single dose on the evening prior to surgery; 40 mg on the morning of surgery; three further doses of 40 mg on the evenings of postoperative days 0, 1, and 2). AKI incidence was assessed during the first 48 postoperative hours on the basis of Acute Kidney Injury Network criteria.
Results
The incidence of AKI was similar in the statin and control groups (21 vs. 26 %, respectively, p = 0.404). Biomarkers of renal injury including plasma neutrophil gelatinase-associated lipocalin and interleukin-18 were also similar between the groups. The statin group required significantly less norepinephrine and vasopressin during surgery, and fewer patients in the statin group required vasopressin. There were no significant differences in postoperative outcomes.
Conclusions
Acute perioperative statin treatment was not associated with a lower incidence of AKI or improved clinical outcome in patients undergoing valvular heart surgery. (ClinicalTrials.gov NCT01909739).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiac surgery with cardiopulmonary bypass (CPB) induces decreased renal perfusion and bursts of inflammatory mediators or emboli that may lead to acute kidney injury (AKI), and its incidence still remains 30–50 % despite advances in CPB technology [1, 2]. Considering the adverse clinical impact of AKI [3, 4], clinical strategies to limit the risk of AKI seem imperative for cardiac surgical patients.
Statins, 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors, have gained attention as a way to reduce AKI after cardiovascular surgery through their anti-inflammatory and antioxidant activities [5]. Indeed, results of randomized controlled studies showed that not only continuing or postprocedural statin treatment but also short-term pretreatment with statins significantly reduced contrast-induced AKI [6] and major adverse cardiac events [7], which were also depicted by meta-analyses [8, 9].
Conversely, the effects of statins on cardiac surgery-induced AKI are inconsistent in randomized controlled [10], retrospective [11], and observational studies [12]. Above all, only a few studies evaluated the impact of statins on patient outcomes after cardiac surgery prospectively, while most studies described retrospective or observational data. So far, two randomized controlled studies prospectively investigated the effect of statins on AKI following cardiac surgery and both reported a neutral effect. Yet, both studies included statin users [10], and only a subanalysis of statin-naïve patients of a large randomized controlled trial revealed that atorvastatin did not reduce the cardiac surgery-induced AKI incidence [13]. Studies addressing the effect of short-term statin treatment on cardiac surgery-induced AKI in only statin-naïve patients is lacking heretofore.
In this prospective, double-blind, randomized, placebo-controlled trial, we investigated the effect of perioperative atorvastatin on AKI in statin-naïve patients undergoing valvular heart surgery.
Methods
Patients
This study was conducted at Severance Hospital, Yonsei University Health System, Seoul, Korea, approved by our institutional review board (IRB number, 4-2013-0334), and registered at http://www.ClinicalTrials.gov (NCT01909739). Two-hundred statin-naïve patients (older than 20 years) scheduled for elective valvular heart surgery were randomly assigned in a 1:1 ratio to either the statin or control group using a computerized randomization table. From both groups, 100 patients were randomly selected at a 1:1 ratio for the measurement of plasma neutrophil gelatinase-associated lipocalin (NGAL) and interleukin (IL)-18 levels. Exclusion criteria were pre-existing renal dysfunction (estimated glomerular filtration rate less than 15 ml/min/1.73 m2; calculated from the Modification of Diet in Renal Disease Study equation) [14], left ventricular ejection fraction less than 30 %, severe coronary artery occlusive disease, active liver disease or cirrhosis, preoperative unexplained elevation of serum transaminases, history of rhabdomyolysis, preoperative unexplained elevation of creatinine kinase, hemodynamically unstable arrhythmia, preoperative cardiogenic shock, or mechanical support.
Treatment
Atorvastatin was administered orally for the statin group according to the following protocol: 80 mg single dose on the evening prior to surgery; 40 mg on the morning of surgery; and three further doses of 40 mg on the evenings of postoperative days (POD) 0, 1, and 2. Placebo was administered in the control group according to the same schedule. Patients received study drugs through a nasogastric tube if mechanical ventilation was continued. A nurse who was not involved in this study prepared the study drug according to the randomization table.
Clinical evaluations
The primary end point was the incidence of postoperative AKI as defined by the Acute Kidney Injury Network (AKIN) criteria [15] as an absolute increase in serum creatinine (sCr) concentration of at least 0.3 mg/dl from baseline or at least 50 % increase in sCr concentration or urine output (UO) less than 0.5 ml/kg/h for more than 6 h within 48 h after surgery. The secondary end points were changes in serum biomarkers including sCr, plasma NGAL, and IL-18 during the perioperative period. sCr was recorded 24 h before surgery; on arrival to the intensive care unit (ICU); and on POD 1, 2, 3, and 5. Plasma NGAL and IL-18 were measured in 100 randomly selected patients after anesthetic induction and at 1 and 6 h after removal of the aortic cross clamp (ACC). Plasma NGAL was measured with a human lipocalin-2/NGAL ELISA kit (R&D System Inc., Minneapolis, MN, USA). IL-18 was measured with a quantitative test for human IL-18 ELISA kit (MBL, Nagoya, Japan).
White blood cell counts (WBCs) and percentage of neutrophil counts were assessed 1 day before surgery and on POD 1, 2, 3, and 5. C-reactive protein (CRP) was measured 1 day before surgery and on POD 1. Total cholesterol and low-density lipoprotein (LDL) levels were measured 1 day before surgery and POD 5.
Preoperative variables included demographic data, type of surgery, cardiovascular risk factors [age greater than 65 years, hypertension, diabetes, smoking (current or former), and hyperlipidemia] [16], history of stroke, preoperative contrast use within 7 days, New York Heart Association Functional Classification, preoperative left ventricular ejection fraction, medications, logistic EuroSCORE, and the Cleveland Clinic Score to assess the risk of renal failure (low risk, scores 0–2; intermediate risk, 3–5; high risk, more than 6) [17]. Intraoperative variables included operation time, durations of ACC and CPB, use of vasopressors or milrinone, fluid balance, and transfusion requirement. Postoperative variables included the dose of vasopressors or milrinone, fluid balance, chest tube drainage, and transfusion requirement.
Need for renal replacement therapy, reoperation, reintubation, readmission to ICU, length of ICU and hospital stays, prolonged mechanical ventilation for more than 48 h, postoperative new-onset atrial fibrillation, stroke, in-hospital mortality, and readmission within 30 days after discharge were assessed. Significantly elevated serum transaminase levels (more than three times the upper limit of normal on two or more measurements) [18] and elevated serum creatinine kinase were assessed as safety outcomes. All assessed perioperative variables were recorded by anesthesiologists who were not involved in the study according to the prescribed case report forms.
Perioperative management
Clinicians involved in the patients’ perioperative management were blinded to the patients’ groups and followed institutional standard protocols [19]. In brief, anesthesia was maintained with sevoflurane and sufentanil. CPB was instituted with a membrane oxygenator primed with 1.6 l priming solution consisting of 100 ml 20 % human albumin, 20 % mannitol (0.5 g/kg), sodium bicarbonate (20 mEq), heparin (2000 IU), and acetated Ringer’s solution (Plasma Solution A Inj.; CJ Pharma, Seoul, Korea). A non-pulsatile pump flow rate was maintained at 2.0–2.4 l/min/m2 under mild hypothermia (32–33 °C) using alpha-stat management. Ultrafiltration was applied to patients with clinical evidence of excessive body water before surgery (peripheral edema, rales, radiographic evidence of fluid overload in lung), hematocrit level less than 18 % during CPB, or expected CPB duration of longer than 2 h. After heparin was antagonized with protamine, salvaged blood from the CPB circuit was washed through a cell saver and then transfused before the end of surgery. Packed red blood cells (pRBC) were transfused when hematocrit was less than 20 % during CPB or less than 25 % before and after CPB. Fresh frozen plasma (FFP) and platelets were transfused according to the institutional guidelines [19, 20]. During the operation including CPB, mean arterial blood pressure was maintained at 60–80 mmHg using norepinephrine and vasopressin [21]. First, norepinephrine was started at 0.01 µg/kg/min (titrated to a maximum of 0.3 µg/kg/min). If the target mean arterial pressure could not be maintained with escalating doses of norepinephrine, vasopressin was added and infused at 2.4–4 unit/h. Milrinone was preferentially used if the left ventricular ejection fraction was less than 30 % or in cases of right ventricular dysfunction and/or pulmonary hypertension. For fluid resuscitation, acetated Ringer’s solution [6–8 ml/kg/h (intraoperatively) or 2–4 ml/kg/h (postoperatively)] and colloid solution (Voluven; Fresenius Kabi, Graz, Austria; to compensate for blood loss up to a maximal dose of 20 ml/kg per day) were used. All patients were transferred to the ICU. When UO decreased below 1 ml/kg/h for 30 min, 200 ml of acetated Ringer’s solution was infused first, and then a bolus of fluid was administered at most twice until the response was adequate. If UO was not recovered after the third bolus, intravenous furosemide was repeatedly administered with an escalating dose of 10–60 mg until the UO exceeded 1 ml/kg/h. Renal replacement therapy was started when fluid overload, oliguria, or hyperkalemia (plasma potassium concentration greater than 6.5 mEq/l) persisted or metabolic acidosis (pH < 7.1), rapidly rising plasma potassium levels, or signs of uremia were observed.
Statistical analysis
Sample size was calculated on the basis of the most recent published trial preformed in our institution that addressed postoperative AKI in patients undergoing valvular heart surgery when we designed the study. The incidence of AKI in patients undergoing valvular heart surgery in our institution was 36 %, and the incidence of AKI was reduced by 50 % with reported effective drugs [20]. Therefore, 94 patients were required in each group to obtain a power of 80 %, detecting a 50 % reduction in AKI considering a type I error of 0.05. Taking into consideration a 5 % dropout rate, we decided to enroll 100 patients in each group.
Continuous variables are shown as mean ± standard deviation or median (Q1–Q3). Dichotomous variables are expressed as number of patients (percentage). Continuous variables were compared using independent Student’s t tests or Mann–Whitney U tests, and dichotomous variables were compared using Chi-square or Fisher’s exact tests as appropriate. A linear mixed model with patient indicator as a random effect, and group, time, and group-by-time as fixed effects was used to analyze repeatedly measured variables such as sCr, inflammatory mediators, and neutrophil count. When the interactions of group, time, and group-by-time of the variables were statistically significant, post hoc analyses were carried out with Bonferroni correction to adjust for multiple comparisons. All data were analyzed according to the intention-to-treat principle. Additionally, per protocol analysis was done. SPSS 20 (SPSSFW, SPSS, IBM, Armonk, NY, USA) statistical software was used. P values less than 0.05 were considered statistically significant.
Results
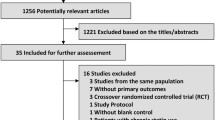
Between July 2013 and August 2015, a total of 200 patients were studied. Informed consent was obtained from all patients before study enrollment. In two patients in the statin group, one or more postoperative doses of study drug were accidentally omitted, but those patients’ data were included in the statistical analysis (Fig. 1).
The patients’ demographic data, preoperative renal function, and Cleveland Clinic Score [17] were similar between the groups (Table 1). AKI occurred in 21 (21 %) and 26 (26 %) patients in the statin and control group, respectively (p = 0.404). Of the patients with AKI, one patient in each group corresponded to AKI stage 3 and required dialysis.
sCr and plasma NGAL levels were comparable between the groups throughout the study period. No patients met the AKIN urine output criteria [15] owing to the early treatment of oliguria with diuretics, and furosemide requirements were comparable between the groups. WBCs and percentage of neutrophil were significantly increased on POD 1, 2, 3, and 5, and serum CRP levels were significantly increased on POD 1 compared to their baseline values in both groups (all p < 0.001) without intergroup differences. IL-18 levels were reduced from their corresponding baseline values 1 h after ACC off and recovered 6 h after ACC off in both groups (all p < 0.001), although all values were within the normal reference range without any intergroup differences. Total cholesterol and LDL levels were significantly reduced on POD 5 in both groups compared to their baseline value (all p < 0.001), and they were significantly lower in the statin group on POD 5 (all p < 0.001, Table 2).
Operative data including durations of ACC and CPB, and fluid balance were similar between the groups. pRBC requirement and the number of patients transfused with FFP (18 vs. 27, p = 0.128) and platelet concentrates (21 vs. 20, p = 0.861) were comparable between the groups. The statin group required significantly less norepinephrine and vasopressin during operation, and the number of patients who required vasopressin was significantly lower in the statin group (Table 3). Postoperative fluid balance, pRBC requirement, and the number of patients transfused with FFP (26 vs. 22, p = 0.508) and platelet concentrates (14 vs. 13, p = 0.836) during the first postoperative 48 h were all similar between the groups. Hematocrit levels were not significantly different throughout the study period (p = 0.076). Vasopressor and milrinone use during the first postoperative 48 h were comparable between the groups (Table 3).
Postoperative outcomes were comparable (Table 4). One patient in the statin group died from multi-organ failure on POD 57. Eight patients in the statin group and one patient in the control group experienced significant increases in serum transaminase (p = 0.121) or serum creatinine kinase (p > 0.999) until POD 5, without statistical significance.
Finally, per protocol analysis excluding the data of two patients in the statin group in whom postoperative doses of statin were accidentally omitted yielded the same results as those of the intention-to-treat analysis mentioned above (data not shown).
Discussion
Statins are commonly used lipid-lowering drugs, and their anti-inflammatory and antioxidant effects are thought to prevent vascular events by stabilizing atherosclerotic plaques [22]. Statins can also improve endothelial function, release vasodilator substances such as nitric oxide, and reduce levels of the endothelin-1, a potent vasoconstrictor [23]. Accounting for these pleiotropic properties, clinicians hypothesized that statins could preserve major organ function in various patient subsets. In the context of contrast-induced AKI, the renoprotective effect of statins could be demonstrated in a large prospective randomized controlled trial [24]. Moreover, results of another randomized controlled study showed that short-term periprocedural treatment with statins in statin-naïve patients as well as continuing statin therapy could significantly attenuate the development of contrast-induced AKI [6].
In the cardiac surgical setting, preoperative statins protected renal function in both prospective observational [12] and retrospective studies [11] involving all types of operation. In contrast, a recent meta-analysis involving only prospective randomized controlled studies evaluating the efficacy of statins on preserving major organ function after cardiac surgery concluded that preoperative statins did not affect the incidence of postoperative AKI [25]. However, only a single randomized controlled study out of the seven included in that analysis addressed AKI as the primary end point [10], and that study reported a neutral effect.
Statins are currently recommended as a routine medication for coronary patients; thus, the clinical implication of perioperative statin treatment is difficult to evaluate in those patients undergoing surgery. Conversely, assessment of the renoprotective effect of statins in valvular heart surgery patients, who are at increased risk of postoperative AKI, would be of high priority and feasible because a large subset of these patients is statin-naïve. We, therefore, prospectively evaluated the impact of perioperative statin treatment on AKI in valvular heart surgery patients using a short-term treatment regimen to allow statins to be easily integrated into our routine clinical practice.
Among the statins, rosuvastatin has the highest potency and yet no difference could be depicted regarding the efficacy of various statins in terms of the renal function [26]. Atorvastatin has the most favorable pharmacokinetic profile rapidly achieving a peak plasma concentration within 2 h following oral intake with a longer half time (approximately 14 h) compared to other statins [27]. Atorvastatin exerted an anti-inflammatory effect shortly after treatment [28], and the highest recommended dose was preoperatively administered to maximize its effect in the current study. Still, administration of atorvastatin from the day before surgery to POD 2 did not reduce the incidence of AKI or attenuate the increase in biomarkers for renal injury including NGAL after valvular heart surgery in statin-naïve patients. We also could not observe any beneficial influence on the other major outcome variables.
Our results contrast with the beneficial effects observed regarding the contrast-induced AKI, but are in agreement with the result of a recent large prospective randomized controlled trial showing that a short-term perioperative atorvastatin treatment could not prevent AKI after cardiac surgery regardless of the statin-naïve nature of the patients [13]. This discrepancy might be related to differences in the degree of inflammatory reaction. Short-term statin treatment alone might not be sufficient to ameliorate the renal insult from CPB accompanied by marked systemic inflammation and oxidative stress. Similar randomized controlled studies were published with N-acetylcysteine [29] and sodium bicarbonate [30], both of which failed to prevent AKI after CPB, despite their proven efficacies in contrast-induced AKI in a randomized controlled trial [31] or meta-analysis [32], respectively. It is also possible that statins might be less effective in patients undergoing valvular heart surgery compared to those with established vascular disease. In a meta-analysis of observational studies [33] and a retrospective study [34], preoperative statin failed to exert a renoprotective effect in isolated valve surgery. Moreover, results of an observational study showed that statins exerted better organ-protective effects in patients at high cardiovascular risk [35], whereas results of a retrospective study showed that statin-naïve patients undergoing valvular heart surgery had fewer cardiovascular morbidities than statin-treated patients [34]. Indeed, more than 60 % of patients had none or just one cardiovascular risk factor in the present study, suggesting that they had a relatively lower potential of benefitting from statins. Also, considering that the positive effects of statins are related to the stabilization of atherosclerotic plaque and a subsequent reduction of cholesterol emboli, statin-naïve patients potentially possessing less cholesterol embolic load might get limited benefit from statins. Finally, given the inconsistencies in the relationship between statin therapy and postoperative AKI, the benefits of statins may be overestimated in the literature.
In this study, atorvastatin did not influence the plasma concentration of IL-18, which plays a pivotal role in a various renal disease processes including ischemia–reperfusion injury [36]. IL-18 levels are significantly increased in patients with vascular events [37] or severe cardiovascular risk [38], and statins have been shown to exert anti-inflammatory effects by attenuating the increase in IL-18 [38]. Nevertheless, IL-18 levels were consistently within the normal range in both groups in the current study. Although IL-18 is an immunomodulatory cytokine in innate and adaptive inflammatory reactions, its levels seem to be more closely related to atherosclerotic and vascular events rather than inflammatory reactions following cardiac surgery.
Notably, intraoperative requirements for vasopressors were significantly lower in the statin group. Since all patients were managed to meet certain hemodynamic goals and the use of vasopressor was done in stepwise fashion, the lack of difference in fluid balance or hemodynamic variables indicates that the vascular tone may be better preserved with statins in the present study. Similar results showed that statin therapy increased vasopressor-free days in patients with sepsis-associated acute respiratory distress syndrome [39]. This observation might be related to decreased nitric oxide production and attenuation of vascular hyporeactivity to vasopressors following statin therapy [40, 41]. Although less vasopressor requirements may lead towards a lower incidence of AKI, its effect on cardiac surgery-induced AKI remains to be proven.
The strengths of the present study are that it was conducted prospectively and employed a double-blinded, randomized, placebo-controlled design. Moreover, we included statin-naïve patients to specifically assess the effect of statin on AKI after CPB.
The limitations of this study are as follows. Although we included a fairly large number of patients compared to previous prospective studies, the power of this study is insufficient since the actual incidence of AKI was less than we predicted. Additionally, measurements of urinary NGAL and IL-18 instead of serum for longer postoperative days would have been more helpful for evaluation of the changes in renal function [42, 43]. Finally, as patients with low UO were given diuretics, the incidence of AKI might have been underestimated using the AKIN criteria.
In conclusion, acute perioperative statin treatment was not associated with a lower incidence of AKI or attenuation of biomarkers related to renal injury in patients undergoing valvular heart surgery. The actual incidence of AKI was less than expected in both groups and this limited the statistical power.
References
Parida S, Badhe AS (2013) Cardiac surgery-associated acute kidney injury. J Anesth 27:433–446
Tuttle KR, Worrall NK, Dahlstrom LR, Nandagopal R, Kausz AT, Davis CL (2003) Predictors of ARF after cardiac surgical procedures. Am J Kidney Dis 41:76–83
Druml W, Lenz K, Laggner AN (2015) Our paper 20 years later: from acute renal failure to acute kidney injury—the metamorphosis of a syndrome. Intensive Care Med 41:1941–1949
Hoste EA, Bagshaw SM, Bellomo R, Cely CM, Colman R, Cruz DN, Edipidis K, Forni LG, Gomersall CD, Govil D, Honore PM, Joannes-Boyau O, Joannidis M, Korhonen AM, Lavrentieva A, Mehta RL, Palevsky P, Roessler E, Ronco C, Uchino S, Vazquez JA, Vidal Andrade E, Webb S, Kellum JA (2015) Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med 41:1411–1423
Shishehbor MH, Brennan ML, Aviles RJ, Fu X, Penn MS, Sprecher DL, Hazen SL (2003) Statins promote potent systemic antioxidant effects through specific inflammatory pathways. Circulation 108:426–431
Patti G, Ricottini E, Nusca A, Colonna G, Pasceri V, D’Ambrosio A, Montinaro A, Di Sciascio G (2011) Short-term, high-dose atorvastatin pretreatment to prevent contrast-induced nephropathy in patients with acute coronary syndromes undergoing percutaneous coronary intervention (from the ARMYDA-CIN [atorvastatin for reduction of myocardial damage during angioplasty–contrast-induced nephropathy] trial. Am J Cardiol 108:1–7
Patti G, Pasceri V, Colonna G, Miglionico M, Fischetti D, Sardella G, Montinaro A, Di Sciascio G (2007) Atorvastatin pretreatment improves outcomes in patients with acute coronary syndromes undergoing early percutaneous coronary intervention: results of the ARMYDA-ACS randomized trial. J Am Coll Cardiol 49:1272–1278
Singh N, Lee JZ, Huang JJ, Low SW, Howe C, Pandit A, Suryanarayana P, Lee KS (2014) Benefit of statin pretreatment in prevention of contrast-induced nephropathy in different adult patient population: systematic review and meta-analysis. Open Heart 1:e000127
Liu Y, Su Q, Li L (2013) Efficacy of short-term high-dose atorvastatin pretreatment in patients with acute coronary syndrome undergoing percutaneous coronary intervention: a meta-analysis of nine randomized controlled trials. Clin Cardiol 36:E41–E48
Prowle JR, Calzavacca P, Licari E, Ligabo EV, Echeverri JE, Haase M, Haase-Fielitz A, Bagshaw SM, Devarajan P, Bellomo R (2012) Pilot double-blind, randomized controlled trial of short-term atorvastatin for prevention of acute kidney injury after cardiac surgery. Nephrology (Carlton) 17:215–224
Layton JB, Kshirsagar AV, Simpson RJ Jr, Pate V, Jonsson Funk M, Sturmer T, Brookhart MA (2013) Effect of statin use on acute kidney injury risk following coronary artery bypass grafting. Am J Cardiol 111:823–828
Molnar AO, Parikh CR, Coca SG, Thiessen-Philbrook H, Koyner JL, Shlipak MG, Myers ML, Garg AX, TRIBE-AKI Consortium (2014) Association between preoperative statin use and acute kidney injury biomarkers in cardiac surgical procedures. Ann Thorac Surg 97:2081–2087
Billings FT, Hendricks PA, Schildcrout JS, Shi Y, Petracek MR, Byrne JG, Brown NJ (2016) High-dose perioperative atorvastatin and acute kidney injury following cardiac surgery: a randomized clinical trial. JAMA 315:877–888
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in renal disease study group. Ann Intern Med 130:461–470
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A, Acute Kidney Injury Network (2007) Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 11:R31
Ohman EM, Bhatt DL, Steg PG, Goto S, Hirsch AT, Liau CS, Mas JL, Richard AJ, Rother J, Wilson PW, REACH Registry Investigators (2006) The REduction of Atherothrombosis for Continued Health (REACH) Registry: an international, prospective, observational investigation in subjects at risk for atherothrombotic events-study design. Am Heart J 151:786.e1–10
Thakar CV, Arrigain S, Worley S, Yared JP, Paganini EP (2005) A clinical score to predict acute renal failure after cardiac surgery. J Am Soc Nephrol 16:162–168
Chalasani N (2005) Statins and hepatotoxicity: focus on patients with fatty liver. Hepatology 41:690–695
Cho JS, Shim JK, Soh S, Kim MK, Kwak YL (2016) Perioperative dexmedetomidine reduces the incidence and severity of acute kidney injury following valvular heart surgery. Kidney Int 89:693–700
Yoo YC, Shim JK, Kim JC, Jo YY, Lee JH, Kwak YL (2011) Effect of single recombinant human erythropoietin injection on transfusion requirements in preoperatively anemic patients undergoing valvular heart surgery. Anesthesiology 115:929–937
Antonelli M, Bonten M, Chastre J, Citerio G, Conti G, Curtis JR, De Backer D, Hedenstierna G, Joannidis M, Macrae D, Mancebo J, Maggiore SM, Mebazaa A, Preiser JC, Rocco P, Timsit JF, Wernerman J, Zhang H (2012) Year in review in Intensive Care Medicine 2011: I. Nephrology, epidemiology, nutrition and therapeutics, neurology, ethical and legal issues, experimentals. Intensive Care Med 38:192–209
Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA, Neil HA, Livingstone SJ, Thomason MJ, Mackness MI, Charlton-Menys V, Fuller JH, investigators C (2004) Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet 364:685–696
Epstein M, Campese VM (2005) Pleiotropic effects of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors on renal function. Am J Kidney Dis 45:2–14
Han Y, Zhu G, Han L, Hou F, Huang W, Liu H, Gan J, Jiang T, Li X, Wang W, Ding S, Jia S, Shen W, Wang D, Sun L, Qiu J, Wang X, Li Y, Deng J, Li J, Xu K, Xu B, Mehran R, Huo Y (2014) Short-term rosuvastatin therapy for prevention of contrast-induced acute kidney injury in patients with diabetes and chronic kidney disease. J Am Coll Cardiol 63:62–70
Lewicki M, Ng I, Schneider AG (2015) HMG CoA reductase inhibitors (statins) for preventing acute kidney injury after surgical procedures requiring cardiac bypass. Cochrane Database Syst Rev 3:CD010480
García Rodríguez LA, Herings R, Johansson S (2010) Use of multiple international healthcare databases for the detection of rare drug-associated outcomes: a pharmacoepidemiological programme comparing rosuvastatin with other marketed statins. Pharmacoepidemiol Drug Saf 19:1218–1224
Florens E, Salvi S, Peynet J, Elbim C, Mallat Z, Bel A, Nguyen A, Tedgui A, Pasquier C, Menasche P (2001) Can statins reduce the inflammatory response to cardiopulmonary bypass? A clinical study. J Card Surg 16:232–239
Bustos C, Hernandez-Presa MA, Ortego M, Tunon J, Ortega L, Perez F, Diaz C, Hernandez G, Egido J (1998) HMG-CoA reductase inhibition by atorvastatin reduces neointimal inflammation in a rabbit model of atherosclerosis. J Am Coll Cardiol 32:2057–2064
Adabag AS, Ishani A, Koneswaran S, Johnson DJ, Kelly RF, Ward HB, McFalls EO, Bloomfield HE, Chandrashekhar Y (2008) Utility of N-acetylcysteine to prevent acute kidney injury after cardiac surgery: a randomized controlled trial. Am Heart J 155:1143–1149
Haase M, Haase-Fielitz A, Plass M, Kuppe H, Hetzer R, Hannon C, Murray PT, Bailey MJ, Bellomo R, Bagshaw SM (2013) Prophylactic perioperative sodium bicarbonate to prevent acute kidney injury following open heart surgery: a multicenter double-blinded randomized controlled trial. PLoS Med 10:e1001426
Marenzi G, Assanelli E, Marana I, Lauri G, Campodonico J, Grazi M, De Metrio M, Galli S, Fabbiocchi F, Montorsi P, Veglia F, Bartorelli AL (2006) N-acetylcysteine and contrast-induced nephropathy in primary angioplasty. N Engl J Med 354:2773–2782
Jang JS, Jin HY, Seo JS, Yang TH, Kim DK, Kim TH, Urm SH, Kim DS, Kim DK, Seol SH, Kim DI, Cho KI, Kim BH, Park YH, Je HG, Ahn JM, Kim WJ, Lee JY, Lee SW (2012) Sodium bicarbonate therapy for the prevention of contrast-induced acute kidney injury—a systematic review and meta-analysis. Circ J 76:2255–2265
Singh I, Rajagopalan S, Srinivasan A, Achuthan S, Dhamija P, Hota D, Chakrabarti A (2013) Preoperative statin therapy is associated with lower requirement of renal replacement therapy in patients undergoing cardiac surgery: a meta-analysis of observational studies. Interact CardioVasc Thorac Surg 17:345–352
Borger MA, Seeburger J, Walther T, Borger F, Rastan A, Doenst T, Mohr FW (2010) Effect of preoperative statin therapy on patients undergoing isolated and combined valvular heart surgery. Ann Thorac Surg 89:773–780
Allou N, Augustin P, Dufour G, Tini L, Ibrahim H, Dilly MP, Montravers P, Wallace J, Provenchere S, Philip I (2010) Preoperative statin treatment is associated with reduced postoperative mortality after isolated cardiac valve surgery in high-risk patients. J Cardiothorac Vasc Anesth 24:921–926
Leslie JA, Meldrum KK (2008) The role of interleukin-18 in renal injury. J Surg Res 145:170–175
Kumar RA, Cann C, Hall JE, Sudheer PS, Wilkes AR (2007) Predictive value of IL-18 and SC5b-9 for neurocognitive dysfunction after cardiopulmonary bypass. Br J Anaesth 98:317–322
Liu Y, Jiang H, Liu W, Shang H, Tang Y, Zhu R, Li B (2010) Effects of fluvastatin therapy on serum interleukin-18 and interleukin-10 levels in patients with acute coronary syndrome. Acta Cardiol 65:285–289
Mansur A, Steinau M, Popov AF, Ghadimi M, Beissbarth T, Bauer M, Hinz J (2015) Impact of statin therapy on mortality in patients with sepsis-associated acute respiratory distress syndrome (ARDS) depends on ARDS severity: a prospective observational cohort study. BMC Med 13:128
Giusti-Paiva A, Martinez MR, Felix JV, da Rocha MJ, Carnio EC, Elias LL, Antunes-Rodrigues J (2004) Simvastatin decreases nitric oxide overproduction and reverts the impaired vascular responsiveness induced by endotoxic shock in rats. Shock 21:271–275
Kandasamy K, Prawez S, Choudhury S, More AS, Ahanger AA, Singh TU, Parida S, Mishra SK (2011) Atorvastatin prevents vascular hyporeactivity to norepinephrine in sepsis: role of nitric oxide and alpha(1)-adrenoceptor mRNA expression. Shock 36:76–82
Ostermann M, Joannidis M (2015) Biomarkers for AKI improve clinical practice: no. Intensive Care Med 41:618–622
Legrand M, Darmon M (2015) Biomarkers for AKI improve clinical practice: yes. Intensive Care Med 41:615–617
Acknowledgments
No financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflicts of interest
The authors declare that they have no conflict of list.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Take-home message: The effect of statin in ameliorating acute kidney injury induced by valvular heart surgery with cardiopulmonary bypass was studied. Acute perioperative statin treatment was not associated with the reduction of incidence of acute kidney injury.
Rights and permissions
About this article
Cite this article
Park, J.H., Shim, JK., Song, JW. et al. Effect of atorvastatin on the incidence of acute kidney injury following valvular heart surgery: a randomized, placebo-controlled trial. Intensive Care Med 42, 1398–1407 (2016). https://doi.org/10.1007/s00134-016-4358-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-016-4358-8