Abstract
Purpose
The study aimed to investigate the relationship between obesity and common mental disorders (CMD) among women.
Methods
This is a cross-sectional population-based study with a representative sample of 981 adult women (20–60 years of age) living in the urban area of the municipality of São Leopoldo, RS, Brazil, in 2015. The presence of CMD was assessed using the Self-Reporting Questionnaire (SRQ-20 ≥ 8). Obesity was defined by body mass index (BMI ≥ 30.0 kg/m2). Prevalence ratios (PRs) for the association between obesity and CMD were measured by Poisson regression with robust variance, including their respective 95% confidence intervals (CIs).
Results
The mean age of the sample was 40.3 years (standard deviation = 11.4 years). The prevalence of CMD was 33.7% (95% CI 30.8–36.7), while obesity was 31.2% (95% CI 28.3–34.1). The occurrence of CMD was higher in women with low levels of education and belonging to lower economic class, as well as smokers and those who were insufficiently active. Obesity was more prevalent in older women (50–60 years old) with less schooling, who did not consume alcohol, and those who were insufficiently active. After adjusting for potential confounding factors, women with obesity were 22% more likely to have CMD when compared to those without obesity (PR = 1.22; 95% CI 1.02–1.45; p = 0.030).
Conclusions
This study demonstrated a significant association between obesity and the presence of CMD among women. Additionally, the prevalence of obesity and CMD were high in this population group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Common mental disorders (CMD) comprise a group of non-psychotic symptoms such as fatigue, anxiety, irritability, insomnia, forgetfulness, difficulty in concentrating, depressive mood and somatic complaints [1]. CMD can cause significant psychological distress, affecting social, familial and work relationships. In addition, they contribute to increased use of health services and reduced life expectancy [2, 3]. Findings from previous studies conducted in high, middle and low income countries estimated that 17.6% of adults experienced CMD in the last 12 months and 29.2% throughout their lives [4]. In Brazil, population-based studies estimated prevalence of CMD between 14.7 and 19.7%, including a higher prevalence among women [5, 6].
Obesity, defined as an abnormal or excessive accumulation of body fat, is considered a chronic and progressive disease of complex and multifactorial etiology, resulting from the interaction of various factors such as genetics, dietary habits, environment, socioeconomic status, lifestyle and psychological factors [7]. Obesity has a high prevalence among the global population, consequent to the increase in its incidence in recent decades [8]. In addition, obesity has been associated with an increase in all-cause mortality, especially among women [9, 10].
Some studies indicated obesity as a predictor for a higher occurrence of CMD [11,12,13,14]. Moreover, this relationship has been more significant among women, considering the hypothesis that this population group is more susceptible to the influence of sociocultural factors, social dysfunction, eating disorders, and greater vulnerability to changes in hormone levels throughout life [15,16,17].
Although the association between obesity and mental disorders is established and presents a two-way relationship [18], the exploration of this relationship remains limited within the context of a developing country like Brazil. Furthermore, this association is a relevant topic in public health, considering the high rate of comorbidity between obesity and mental disorders. Thus, this study aimed to investigate the association between obesity and CMD in a sample of Brazilian women. Our hypothesis is that women with obesity tend to have a higher probability of CMD than women without it.
Methods
Design and population
This is a cross-sectional population-based study with a representative sample of adult women, between 20 and 60 years of age, living in the urban area of the municipality of São Leopoldo, RS, Brazil. The municipality of São Leopoldo belongs to the Metropolitan region of Porto Alegre, located 33 km from the state capital of Rio Grande do Sul. According to the 2010 Census, São Leopoldo has an area of 102,738 km2 and an estimated population of 214,087 inhabitants, with a predominance of females (109,845) [19]. The Human Development Index of the Municipality was 0.739, classified as high and higher than the Brazilian index (0.727).
Sampling process
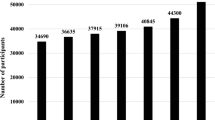
This study is part of a larger project, conducted in 2015, which sought to investigate different health outcomes in a population group of women. Multi-stage sampling was performed, in which, first, 45 census tracts were systematically drawn from the 371 in the urban region of the city. Subsequently, in each selected sector, the blocks and the corners were drawn, and from this, the domicile was identified for initiating data collection. The houses were alternately (jump of two) selected until completing 36 households in each sector. All women aged 20–69 years living in these households were invited to participate in the study; in case of refusals, two more attempts were made on different days and times. Pregnant women and those with hearing and/or cognitive impairment were excluded. Further details on the methodological procedures of the study are described in previous publications [20, 21]. The sample size was previously estimated based on the outcome that required a greater number of participants in the larger project (late cytopathological examination). Of the total number of eligible women, 1128 agreed to participate in the study, including a percentage of losses and refusals of 11.9%. Specifically for the present study, all women between 61 and 69 years of age (141) were excluded because they were considered elderly and the criteria for defining obesity differed from those used for adults [22], in addition to six women for loss of anthropometric weight and height (BMI) data. Thus, the final sample of this study totaled 981 women, allowing the detection, with 95% confidence interval (CI) and a power of 80%, a Prevalence Ratio (PR) of 1.20 for the association between obesity and CMD.
Data collection
Data was obtained through face-to-face interviews conducted by interviewers. A training program was carried out with the objective of the application of standardized, pre-coded, and tested questionnaires. Quality control of data collection was performed using a random sample of 10% of the people included in the study. The present study was evaluated and approved by the Ethics and Research Committee of the University of Vale do Rio dos Sinos (protocol number 653.394). All participants signed a free and informed consent form.
Outcome: common mental disorders
The presence of CMD was assessed using the Self-Reporting Questionnaire (SRQ-20) [23]. This instrument is used to identify signs and symptoms of non-psychotic mental disorders, which consists of 20 closed questions with dichotomous answers (yes/no), including screening for depression, anxiety, insomnia, fatigue, irritability, forgetfulness, difficulty concentrating and somatic complaints in the last 30 days. This instrument is validated for the Portuguese language of Brazil, considering a cutoff point of 8 points or more (≥ 8 positive answers within a total of 20 questions) to determine the presence of CMD among adult women [23]. The internal consistency of the instrument used (SRQ-20) was adequate, considering the application of the Kuder-Richardson reliability coefficient (KR20 = 0.859).
Main exposure: obesity
The presence of obesity was evaluated by BMI (Body Mass Index), calculated by dividing body weight into kilograms by height in meters squared. Weight and body height were measured using an anthropometric scale (Omron®) with a capacity of 150 kg and resolution of 100 g, and a fixed stadiometer, with a capacity of 95–190 cm, respectively. Both measurement procedures were performed in duplicate, by previously trained personnel, and with the women wearing light clothing and no footwear. Women with BMI ≥ 30.0 kg/m2 were classified with obesity [24].
Explanatory variables (covariates)
Demographic, socioeconomic, and behavioral characteristics were collected through a standardized questionnaire to characterize the sample as well as to control potential confounding factors in multivariate analysis. Demographic characteristics included: age in age groups (20–29 years; 30–39 years; 40–49 years; 50–60 years); skin color/race (self-reported according to the categories proposed by the Brazilian Institute of Geography and Statistic) [19], and categorized as white and other (black/brown/yellow/indigenous); and marital status (with a partner [married] and without a partner [single/separated/divorced/widowed]). Socioeconomic characteristics included: complete years of study (≥ 11 years; 8–10 years; 5–7 years; ≤ 4 years) and economic class (A; B; C; D; E) classified according to the criteria proposed by the Brazilian Association of Research Companies (ABEP), based on the possession of certain material goods, schooling of the head of the family and number of employees [25]. Behavioral characteristics included: self-reported smoking status (non-smoker; former smoker; smoker); self-reported alcohol consumption in the last week (no [without consumption]; yes [consumption of some alcoholic beverage in the last 7 days], and leisure-time physical activity estimated through the International Physical Activity Questionnaire—IPAQ—adapted short version (sufficiently active [≥ 150 min/week of moderate/vigorous physical activity]; insufficiently active [< 150 min/week moderate/vigorous physical activity]) [26].
Statistical analyses
Data were entered in Epidata version 3.1, with double typing and subsequent comparison. The numerical variables were described by mean and standard deviation and categorical variables by means of absolute and relative frequencies. Pearson’s Chi-square test was used for heterogeneity of proportions (categorical variables) or linear trend (ordinal variables) to compare the prevalence of obesity and CMD according to the categories of the variables investigated. PRs for the association between obesity and CMD were obtained by Poisson regression with robust variance [27], including three multivariate analysis models: Model I (unadjusted analysis); Model II (adjusted analysis for demographic and socioeconomic characteristics); Model III (adjusted analysis for model II and behavioral characteristics) [28]. The potential confounding factors were all variables associated with outcome or exposure, with p < 0.20 in the bivariate analysis. All analyses were performed in Stata software (StataCorp, College Station, TX, USA) version 12.0 and associations with p-value lower than 5% (p < 0.05) were considered statistically significant.
Results
A total of 981 women aged between 20 and 60 years (mean of 40.3 ± 11.4 years) were included in the final analysis of this study. Regarding the general characteristics of the sample, there was a predominance of the age group from 40 to 49 years (27.9%), with white skin color (74.1%), lived with a partner (64.6%), with 11 to 14 complete years of study (34.8%) and belonged to economic class C (51.9%). Regarding behavioral characteristics, it was observed that 19.8% of the participants were smokers, 36.4% reported alcohol consumption in the last week and 85.6% were classified as insufficiently active (Table 1).
The prevalence of general obesity (BMI ≥ 30 kg/m2) was 31.2% (95% CI 28.3–34.1). Among the factors analyzed, it was observed that already from the age of 30 years about one-third of the women had obesity, a prevalence that affected 38.2% of older women in the 50–60 years age-group (Table 1). It was also observed that the lowest prevalence of obesity (~ 20%) occurred in young women (20–24 years old), with high schooling (≥ 15 years), who consumed alcohol and were physically active (Table 1).
The prevalence of CMD (SRQ ≥ 8) was 33.7% (95% CI 30.8–36.7) in the total sample, and, regardless of age group, skin color and marital status, the prevalence of CMD was at least 30%. There was a disparity in the prevalence of CMD, and women with high schooling and belonging to upper economic class had a lower prevalence of CMD (14.6% and 12.8%, respectively) compared to those with low schooling and belonging to lower economic class (45.3% and 43.7%, respectively). In addition, women who were smokers and insufficiently active had a higher prevalence of CMD compared to those who were non-smokers and physically active; on the other hand, women who reported no alcohol consumption had a higher prevalence of CMD compared to those who reported alcohol consumption (Table 1).
Table 2 presents the PRs for the association between obesity and CMD. There was a prevalence of 39.9% of CMD among women with obesity, while among women without obesity it was 31%. In the unadjusted analysis (Model I), it was observed that women with obesity had a 29% higher probability of having CMD (PR = 1.29; 95% CI 1.08–1.54; p = 0.005), when compared to women without obesity. After adjusting for potential confounding factors (Model III), it was observed that this association remained significant, with a 22% higher probability of occurrence of CMD among women with obesity (PR = 1.22%; 95% CI 1.02–1.45; p = 0.030), compared to those without obesity (Table 2).
Discussion
This study aimed to investigate the relationship between obesity and CMD among women. The findings showed a significant association, and women with obesity were 22% more likely to have CMD when compared to women without obesity. In this population-based study with a representative sample of adult women from southern Brazil, a high prevalence of obesity and the presence of CMD were observed.
Previous studies have also indicated a possible association between obesity and CMD. A cross-sectional study with 6079 Latin American women aged 40 to 59 years showed that women with obesity had a 57% and 21% higher chance of having depression and anxiety, respectively [29]. A similar finding was observed in a Mexican study conducted on 45,052 people, in which women with obesity had a 28% higher chance of having depression [30]. In the United States, a greater magnitude of association was observed, and women with obesity had 73% [31] and 218% [32] higher chance for depression, for example. In addition, a longitudinal study found that women with obesity had a 14% higher risk of developing depression [33], while the final result of a meta-analysis of observational studies indicated a 36% higher probability of depression among women with obesity [12].
Although treated as unrelated diseases, obesity and CMD share some possible mechanisms. Among biological factors, some gain greater relevance and justify much of this association, such as the presence of systemic inflammation, dysregulation of the hypothalamus–pituitary–adrenal axis, oxidative stress, and interruption of neuroendocrine regulators (leptin and insulin resistance) [34, 35]. Moreover, there is a hormonal issue: obesity usually induces a greater irregularity in menstrual cycles, as well as causing oscillations in the production of female sex hormones throughout the reproductive life [36]. This hormonal imbalance can influence mechanisms that contribute directly or indirectly to the occurrence of CMD [15]. It is also prospected that shared genetic factors are involved in the development of obesity and CMD, particularly depression [37, 38]. Features related to the intestinal microbiota are also identified among the possible common mechanisms between obesity and CMD [39, 40]. The accumulation of adipose tissue tends to increase the secretion of pro-inflammatory cytokines, such as TNF-α and IL-6 by adipocytes, which, aided by intestinal dysbiosis, can develop a chronic inflammatory state, contributing to neuroinflammation and neuroplasticity in mood and behavior networks [34, 41]. Finally, psychosocial factors, such as stigmatization of obesity and low self-esteem, can also contribute to significant psychological consequences, being a more evident problem in women [34, 42]. A study conducted with 1238 Brazilian adults showed that the relationship between obesity and depression was mediated by the perception of body weight. Thus, people with obesity were more prone to body dissatisfaction, leading to low self-esteem, and consequently, increase the chances of depression [43].
Our findings showed a high prevalence of CMD in the group of women who were investigated. Previous studies have found similar results for the occurrence of CMD, including prevalences of 18.7% [44] and 29.7% [45]. In addition, a systematic review study revealed that the overall prevalence of CMD among adult women ranges from 9.6 to 69.3% [2]. This heterogeneity in prevalence may be related to the choice of the screening instrument and socioeconomic and cultural conditions of the population investigated [2, 46]. Although our findings did not identify an association with age, it was observed that CMD affected women homogeneously in all age groups, particularly those between 30 and 39 years (35.1%); that is, aside from the high prevalence, the presence of CMD among young women should be highlighted.
In the present study, socioeconomic conditions presented an inverse association with CMD. These results are similar to previous studies that indicated low schooling associated with higher occurrence of CMD [6, 44, 47], as well as an association between less favored economic classes and CMD [48, 49]. Unhealthy habits such as smoking tend to be related to the presence of CMD [50, 51]. Our analysis showed higher prevalence of CMD among smokers, similar to a study in southern Brazil, where 50.8% of female smokers had anxiety disorder [52]. According to the findings of a meta-analysis, it is difficult to infer causality between smoking and CMD in observational studies, because the possible confounding factors are not fully elucidated. Additionally, when a causal association is evidenced, bidirectionality should be considered [51]. Insufficient physical activity was related to CMD. As described in the literature, higher levels of physical activity are positively associated with a decreased chances of developing depression and future anxiety [53, 54].
In relation to obesity, a higher prevalence was observed among older women with lower schooling and insufficient activity. It is noteworthy that according to data on obesity trends in the world, between 1975 and 2014 the prevalence of obesity increased from 3.2 to 10.8% among male adults, and from 6.4 to 14.9% among female adults [8]. In Brazil, in a study involving data from 59,402 individuals, the prevalence of obesity was 20.8% among the adult population, being higher in women (24.3% versus 16.8%) who were middle-aged (increasing prevalence from 30 years), and those with lower schooling [55]. It is hypothesized that this more pronounced prevalence in women is due to a greater vulnerability regarding biological (hormonal fluctuation, particularly in menopause) and behavioral (insufficient physical activity and sedentary lifestyle) factors, in addition to a gender-related social disparity, in which socioeconomic and cultural variables play an important role [29, 56, 57]. Corroborating other studies, there was also a higher prevalence of obesity in insufficiently active women, considering that more than 85% of the participants said they practiced less than 150 min of intense/moderate activity. There is consensus in the literature that inadequate patterns of physical activity are associated with health problems such as obesity [58]. Moreover, vigorous physical activity seems to play an important role in regulating fat percentage in women, and can prevent fat mass gains over time [59].
Regarding alcohol consumption, it was observed in this study that the prevalence of CMD and obesity was higher among women who did not use alcohol in the last 7 days. In relation to CMD, this finding is contrary to scientific literature that has associated alcohol use with mental disorders [60,61,62]. Evidence points out that women are less predisposed to excessive alcohol use, since they have less social support and greater social stigma compared to men [63]. Regarding obesity, the scientific literature is controversial about this relationship, because epidemiological studies generally tend to demonstrate that mild to moderate alcohol consumption is not associated with adiposity gain, while excessive consumption is associated with a higher occurrence of obesity [64]. Considering these findings in relation to alcohol consumption with the occurrence of CMD and obesity, it is worth noting that previous studies indicate a possible J-shaped relationship between these factors [64, 65]. The higher prevalence of CMD and obesity among women who do not use alcohol can be influenced by various factors. In this study, we hypothesize that the observed higher prevalence of CMD and obesity among women who do not consume alcohol can be attributed to their lower alcohol consumption. This hypothesis is supported by the fact that more than 60% of the women who participated in the study reported abstaining from alcohol in the past 7 days. Women who do not consume alcohol may experience diverse lifestyle or social factors, as well as underlying health conditions or genetic predispositions, which can contribute to both CMD and obesity. Thus, further research and analysis would be needed to fully understand the specific reasons behind the higher prevalence of CMD and obesity among non-alcohol-consuming women.
Compared to the previously published studies in the literature, this study explored the association between obesity and CMD within the specific context of a developing country. The strengths of this study included a representative population-based sample of Brazilian adult women, the use of instruments tested and validated for the assessment/screening of the presence of CMD (SRQ-20), and a standardized collection of anthropometric measurements for measuring weight and height to determine the presence of obesity. The SRQ-20 is advantageous for evaluating CMD due to its practicality, simplicity, and efficiency. It is a widely used screening tool that assesses the presence of non-psychotic psychiatric symptoms commonly associated with CMD. Additionally, the use of the SRQ-20 is cost-effective compared to a comprehensive clinical evaluation performed by professionals. These factors make the SRQ-20 a valuable tool for identifying individuals in need of further diagnostic evaluation or intervention. It is also noteworthy that multivariate analyses were performed for observing the association between obesity and CMD, including control for potential confounding factors, which reinforces the methodological rigor of the present study. However, some limitations should be highlighted and mentioned. A limitation of the present study is its design, considering that studies with cross-sectional design are limited in the establishment of causality between exposure and outcome. On the association between obesity and CMD, previous studies have shown that this relationship can be bidirectional, where people with CMD may also develop obesity [18, 66, 67]. Evidence suggests that this association is more significant among women. For example, a study that evaluated the relationship between depression and obesity among 7108 Americans over 18 years showed that only among women did depression predict increased obesity, and vice versa [16]. The SRQ-20 instrument is composed of questions related to depressive symptoms, anxiety, and psychosomatic complaints that reflect probable cases of CMD—i.e., this instrument is used for screening and does not allow specific diagnoses of mental disorders. Finally, the external validity of this study was established; that is, it was conducted on a sample of adult women living in a city in southern Brazil. Therefore, the findings can be generalized within similar population groups.
The association between obesity and CMD is a relevant topic in public health, considering the high rate of comorbidity between these two diseases. The coexistence of multifactorial diseases, such as obesity and CMD, is one of the points to be highlighted among the implications of the present study since both health conditions had a high prevalence. Both obesity and CMD are related to unfavorable and severe health consequences, including emotional distress and dissatisfaction with life, combined with social determinants, such as lack of resources for food and housing. In addition, they generate significant economic impacts due to the high use of health services and the commitment of work activities [68, 69]. Thus, given the relevance of both conditions for public health, exploring the nature of this association may contribute to the implementation of preventive strategies of CMD associated with obesity, especially among the female population.
Conclusions
This study revealed a significant association between obesity and CMD. Women with obesity were more likely to have CMD (almost 40%). In addition, the prevalence of obesity and CMD were high in this population group (~ 30%). However, we highlight the need for further longitudinal studies that elucidate the causative mechanisms of this association, so that preventive strategies can be implemented and prevalence of both these conditions can be reduced.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Goldberg DP, Huxley P (1992) Common mental disorders: a bio-social model. Tavistock/Routledge, New York
Bezerra HS, Alves RM, Nunes ADD, Barbosa IR (2021) Prevalence and associated factors of common mental disorders in women: a systematic review. Public Health Rev 42:1604234. https://doi.org/10.3389/phrs.2021.1604234
Ormel J, VonKorff M (2021) Reducing common mental disorder prevalence in populations. JAMA Psychiat 78(4):359–360. https://doi.org/10.1001/jamapsychiatry.2020.3443
Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, Silove D (2014) The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int J Epidemiol 43(2):476–493. https://doi.org/10.1093/ije/dyu038
Moraes RSM, Silva DAS, Oliveira WF, Peres MA (2017) Social inequalities in the prevalence of common mental disorders in adults: a population-based study in Southern Brazil. Rev Bras Epidemiol 20(1):43–56. https://doi.org/10.1590/1980-5497201700010004
Santos G, Alves M, Goldbaum M, Cesar CLG, Gianini RJ (2019) Prevalence of common mental disorders and associated factors in urban residents of Sao Paulo, Brazil. Cad Saude Publica 35(11):e00236318. https://doi.org/10.1590/0102-311X00236318
Gonzalez-Muniesa P, Martinez-Gonzalez MA, Hu FB, Despres JP, Matsuzawa Y, Loos RJF, Moreno LA, Bray GA, Martinez JA (2017) Obesity. Nat Rev Dis Primers 3:17034. https://doi.org/10.1038/nrdp.2017.34
NCDRF Collaboration (2017) Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 387(10026):1377–1396. https://doi.org/10.1016/S0140-6736(16)30054-X
Collaborators GBDO, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M et al (2017) Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 377(1):13–27. https://doi.org/10.1056/NEJMoa1614362
Colpani V, Baena CP, Jaspers L, van Dijk GM, Farajzadegan Z, Dhana K, Tielemans MJ, Voortman T, Freak-Poli R, Veloso GGV et al (2018) Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and meta-analysis. Eur J Epidemiol 33(9):831–845. https://doi.org/10.1007/s10654-018-0374-z
Alshehri T, Boone S, de Mutsert R, Penninx B, Rosendaal F, le Cessie S, Milaneschi Y, Mook-Kanamori D (2019) The association between overall and abdominal adiposity and depressive mood: a cross-sectional analysis in 6459 participants. Psychoneuroendocrinology 110:104429. https://doi.org/10.1016/j.psyneuen.2019.104429
Pereira-Miranda E, Costa PRF, Queiroz VAO, Pereira-Santos M, Santana MLP (2017) Overweight and obesity associated with higher depression prevalence in adults: a systematic review and meta-analysis. J Am Coll Nutr 36(3):223–233. https://doi.org/10.1080/07315724.2016.1261053
Husky MM, Mazure CM, Ruffault A, Flahault C, Kovess-Masfety V (2018) Differential associations between excess body weight and psychiatric disorders in men and women. J Womens Health (Larchmt) 27(2):183–190. https://doi.org/10.1089/jwh.2016.6248
McCrea RL, Berger YG, King MB (2012) Body mass index and common mental disorders: exploring the shape of the association and its moderation by age, gender and education. Int J Obes (Lond) 36(3):414–421. https://doi.org/10.1038/ijo.2011.65
Baldini I, Casagrande BP, Estadella D (2021) Depression and obesity among females, are sex specificities considered? Arch Womens Ment Health 24(6):851–866. https://doi.org/10.1007/s00737-021-01123-6
Vittengl JR (2018) Mediation of the bidirectional relations between obesity and depression among women. Psychiatry Res 264:254–259. https://doi.org/10.1016/j.psychres.2018.03.023
de Wit L, Luppino F, van Straten A, Penninx B, Zitman F, Cuijpers P (2010) Depression and obesity: a meta-analysis of community-based studies. Psychiatry Res 178(2):230–235. https://doi.org/10.1016/j.psychres.2009.04.015
Mannan M, Mamun A, Doi S, Clavarino A (2010) Is there a bi-directional relationship between depression and obesity among adult men and women? Systematic review and bias-adjusted meta analysis. Asian J Psychiatry 21:51–66. https://doi.org/10.1016/j.ajp.2015.12.008
IBGE (2001) Brazilian Institute of Geography and Statistics. 2010 Population Census—Characteristics of Population and Households: Results of the Universe/[Censo demográfico 2000: características da população e dos domicílios: resultados do universo]. Instituto Brasileiro de Geografia Estatística. IBGE, Rio de Janeiro. https://biblioteca.ibge.gov.br/visualizacao/periodicos/93/cd_2010_caracteristicas_populacao_domicilios.pdf. Accessed 23 Sep 2021
Cafruni CB, Pattussi MP, Backes V, da Costa JD, Olinto MTA, de Bairros FS, Henn RL (2019) Neighbourhood environment and transport-related and leisure-time sedentary behaviour amongst women in a city in Southern Brazil: a multilevel analysis. Int J Public Health 64(4):511–522. https://doi.org/10.1007/s00038-019-01229-w
Dias-da-Costa JS, Mattos CNB, Leite HM, Theodoro H, Acosta LMW, Freitas MW, Bordin RB, Bairros F, Goncalves TR, Olinto MTA (2019) Factors associated with not having Pap Smears in Sao Leopoldo, Rio Grande do Sul, Brazil, 2015: a cross-sectional population-based study. Epidemiol Serv Saude 28(1):e2018203. https://doi.org/10.5123/S1679-49742019000100011
Silveira EA, Pagotto V, Barbosa LS, Oliveira C, Pena GDG, Velasquez-Melendez G (2020) Accuracy of BMI and waist circumference cut-off points to predict obesity in older adults. Cien Saude Colet 25(3):1073–1082. https://doi.org/10.1590/1413-81232020253.13762018
Mari JJ, Williams P (1986) A validity study of a psychiatric screening questionnaire (SRQ-20) in primary care in the city of Sao Paulo. Br J Psychiatry 148:23–26. https://doi.org/10.1192/bjp.148.1.23
WHO (2000) World Health Organization. Obesity: preventing and managing the global epidemic. WHO, Geneva. https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/. Accessed 13 Sep 2021
ABEP (2015) Brazilian Association of Research Companies. Brazil Economic Classification Criterion/[Critério de Classificação Econômica Brasil]. Associação Brasileira de Empresas de Pesquisa. ABEP, São Paulo. http://www.abep.org/novo/critério-brasil. Accessed 22 Sep 2021
Matsudo S, Araújo T, Matsudo V, Andrade D, Andrade E, Oliveira L, Braggion G (2001) International physical activity questionnaire (IPAQ): study of validity and reliability in Brazil. Rev Bras Ativ Fis Saude 6(2):5–18. https://doi.org/10.12820/rbafs.v.6n2p5-18
Barros AJ, Hirakata VN (2003) Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 3:21. https://doi.org/10.1186/1471-2288-3-21
Victora CG, Huttly SR, Fuchs SC, Olinto MT (1997) The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol 26(1):224–227. https://doi.org/10.1093/ije/26.1.224
Blumel JE, Chedraui P, Aedo S, Fica J, Mezones-Holguin E, Baron G, Bencosme A, Benitez Z, Bravo LM, Calle A et al (2015) Obesity and its relation to depressive symptoms and sedentary lifestyle in middle-aged women. Maturitas 80(1):100–105. https://doi.org/10.1016/j.maturitas.2014.10.007
Zavala GA, Kolovos S, Chiarotto A, Bosmans JE, Campos-Ponce M, Rosado JL, Garcia OP (2018) Association between obesity and depressive symptoms in Mexican population. Soc Psychiatry Psychiatr Epidemiol 53(6):639–646. https://doi.org/10.1007/s00127-018-1517-y
Hicken MT, Lee H, Mezuk B, Kershaw KN, Rafferty J, Jackson JS (2013) Racial and ethnic differences in the association between obesity and depression in women. J Womens Health (Larchmt) 22(5):445–452. https://doi.org/10.1089/jwh.2012.4111
Ma J, Xiao L (2010) Obesity and depression in US women: results from the 2005–2006 National Health and Nutritional Examination Survey. Obesity (Silver Spring) 18(2):347–353. https://doi.org/10.1038/oby.2009.213
Martin-Rodriguez E, Guillen-Grima F, Auba E, Marti A, Brugos-Larumbe A (2016) Relationship between body mass index and depression in women: a 7-year prospective cohort study. The APNA study. Eur Psychiatry 32:55–60. https://doi.org/10.1016/j.eurpsy.2015.11.003
Fulton S, Decarie-Spain L, Fioramonti X, Guiard B, Nakajima S (2022) The menace of obesity to depression and anxiety prevalence. Trends Endocrinol Metab 33(1):18–35. https://doi.org/10.1016/j.tem.2021.10.005
Capuron L, Lasselin J, Castanon N (2017) Role of adiposity-driven inflammation in depressive morbidity. Neuropsychopharmacology 42(1):115–128. https://doi.org/10.1038/npp.2016.123
Pasquali R, Oriolo C (2019) Obesity and androgens in women. Front Horm Res 53:120–134. https://doi.org/10.1159/000494908
Kleinendorst L, Massink MPG, Cooiman MI, Savas M, van der Baan-Slootweg OH, Roelants RJ, Janssen ICM, Meijers-Heijboer HJ, Knoers N, Ploos van Amstel HK et al (2018) Genetic obesity: next-generation sequencing results of 1230 patients with obesity. J Med Genet 55(9):578–586. https://doi.org/10.1136/jmedgenet-2018-105315
Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, Powell C, Vedantam S, Buchkovich ML, Yang J et al (2015) Genetic studies of body mass index yield new insights for obesity biology. Nature 518(7538):197–206. https://doi.org/10.1038/nature14177
Simpson CA, Diaz-Arteche C, Eliby D, Schwartz OS, Simmons JG, Cowan CSM (2021) The gut microbiota in anxiety and depression—a systematic review. Clin Psychol Rev 83:101943. https://doi.org/10.1016/j.cpr.2020.101943
Torres-Fuentes C, Schellekens H, Dinan TG, Cryan JF (2017) The microbiota–gut–brain axis in obesity. Lancet Gastroenterol Hepatol 2(10):747–756. https://doi.org/10.1016/S2468-1253(17)30147-4
Spichak S, Bastiaanssen TFS, Berding K, Vlckova K, Clarke G, Dinan TG, Cryan JF (2021) Mining microbes for mental health: determining the role of microbial metabolic pathways in human brain health and disease. Neurosci Biobehav Rev 125:698–761. https://doi.org/10.1016/j.neubiorev.2021.02.044
Preiss K, Brennan L, Clarke D (2013) A systematic review of variables associated with the relationship between obesity and depression. Obes Rev 14(11):906–918. https://doi.org/10.1111/obr.12052
Paulitsch RG, Demenech LM, Dumith SC (2021) Association of depression and obesity is mediated by weight perception. J Health Psychol 26(11):2020–2030. https://doi.org/10.1177/1359105319897778
Senicato C, Azevedo RCS, Barros MBA (2018) Common mental disorders in adult women: identifying the most vulnerable segments. Cien Saude Colet 23(8):2543–2554. https://doi.org/10.1590/1413-81232018238.13652016
Henriques IF, Walsh IAPD, Meirelles MCCC, Pereira GDA, Castro SSD (2017) Relation of common mental disorder, physical activity and body mass index in women, population-based study. J Phys Educ 28:e2819. https://doi.org/10.4025/jphyseduc.v28i1.2819
Kagee A, Tsai AC, Lund C, Tomlinson M (2013) Screening for common mental disorders in low resource settings: reasons for caution and a way forward. Int Health 5(1):11–14. https://doi.org/10.1093/inthealth/ihs004
Quadros LCM, Quevedo LA, Goncalves HD, Horta BL, Motta J, Gigante DP (2020) Common mental disorders and contemporary factors: 1982 birth cohort. Rev Bras Enferm 73(1):e20180162. https://doi.org/10.1590/0034-7167-2018-0162
de Vries YA, Ten Have M, de Graaf R, van Dorsselaer S, de Ruiter NMP, de Jonge P (2019) The relationship between mental disorders and actual and desired subjective social status. Epidemiol Psychiatr Sci 29:e83. https://doi.org/10.1017/S2045796019000805
Costa JSDd, Menezes AMB, Olinto MTA, Gigante DP, Macedo S, Britto MAPd, Fuchs SC (2002) [Prevalence of minor psychiatric disorders in the City of Pelotas, RS] (Prevalência de distúrbios psiquiátricos menores na cidade de Pelotas, RS). Rev Bras Epidemiol 5(2):164–173. https://doi.org/10.1590/S1415-790X2002000200004
Tayefi M, Shafiee M, Kazemi-Bajestani SMR, Esmaeili H, Darroudi S, Khakpouri S, Mohammadi M, Ghaneifar Z, Azarpajouh MR, Moohebati M et al (2017) Depression and anxiety both associate with serum level of hs-CRP: a gender-stratified analysis in a population-based study. Psychoneuroendocrinology 81:63–69. https://doi.org/10.1016/j.psyneuen.2017.02.035
Taylor AE, Fluharty ME, Bjorngaard JH, Gabrielsen ME, Skorpen F, Marioni RE, Campbell A, Engmann J, Mirza SS, Loukola A et al (2014) Investigating the possible causal association of smoking with depression and anxiety using Mendelian randomisation meta-analysis: the CARTA consortium. BMJ Open 4(10):e006141. https://doi.org/10.1136/bmjopen-2014-006141
Costa CO, Branco JC, Vieira IS, Souza LDdM, Silva RA (2019) [Prevalence of anxiety and associated factors in adults] (Prevalência de ansiedade e fatores associados em adultos). J Bras Psiquiatr 68(2):92–100. https://doi.org/10.1590/0047-2085000000232
Schuch FB, Stubbs B, Meyer J, Heissel A, Zech P, Vancampfort D, Rosenbaum S, Deenik J, Firth J, Ward PB et al (2019) Physical activity protects from incident anxiety: a meta-analysis of prospective cohort studies. Depress Anxiety 36(9):846–858. https://doi.org/10.1002/da.22915
Schuch FB, Vancampfort D, Firth J, Rosenbaum S, Ward PB, Silva ES, Hallgren M, Ponce De Leon A, Dunn AL, Deslandes AC et al (2018) Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiatry 175(7):631–648. https://doi.org/10.1176/appi.ajp.2018.17111194
Rimes-Dias KA, Canella DS (2020) Medication use and obesity in Brazil: results from the National Health Survey. Sci Rep 10(1):18856. https://doi.org/10.1038/s41598-020-76058-6
Garawi F, Devries K, Thorogood N, Uauy R (2014) Global differences between women and men in the prevalence of obesity: is there an association with gender inequality? Eur J Clin Nutr 68(10):1101–1106. https://doi.org/10.1038/ejcn.2014.86
Wells JC, Marphatia AA, Cole TJ, McCoy D (2012) Associations of economic and gender inequality with global obesity prevalence: understanding the female excess. Soc Sci Med 75(3):482–490. https://doi.org/10.1016/j.socscimed.2012.03.029
Must A, Tybor DJ (2005) Physical activity and sedentary behavior: a review of longitudinal studies of weight and adiposity in youth. Int J Obes (Lond) 29(Suppl 2):S84–S96. https://doi.org/10.1038/sj.ijo.0803064
Bailey BW, Tucker LA, Peterson TR, LeCheminant JD (2007) A prospective study of physical activity intensity and change in adiposity in middle-aged women. Am J Health Promot 21(6):492–497. https://doi.org/10.4278/0890-1171-21.6.492
Macedo JP, Dimenstein M, Silva BÍdBdM, Sousa HR, Costa APA (2018) Social support, common mental disorder and abusive use of alcohol in rural settlements. Trends Psychol 26(3):1123–1137. https://doi.org/10.9788/TP2018.3-01Pt
Jansen K, Mondin TC, Ores Lda C, Souza LD, Konradt CE, Pinheiro RT, Silva RA (2011) Mental common disorders and quality of life in young adulthoods: a population-based sample in Pelotas, Rio Grande do Sul State, Brazil. Cad Saude Publica 27(3):440–448. https://doi.org/10.1590/s0102-311x2011000300005
Bolton JM, Robinson J, Sareen J (2009) Self-medication of mood disorders with alcohol and drugs in the National Epidemiologic Survey on Alcohol and Related Conditions. J Affect Disord 115(3):367–375. https://doi.org/10.1016/j.jad.2008.10.003
Shield K, Manthey J, Rylett M, Probst C, Wettlaufer A, Parry CDH, Rehm J (2020) National, regional, and global burdens of disease from 2000 to 2016 attributable to alcohol use: a comparative risk assessment study. Lancet Public Health 5(1):e51–e61. https://doi.org/10.1016/S2468-2667(19)30231-2
Traversy G, Chaput JP (2015) Alcohol consumption and obesity: an update. Curr Obes Rep 4(1):122–130. https://doi.org/10.1007/s13679-014-0129-4
Boden JM, Foulds JA, Horwood LJ (2016) Examination of a possible J-shaped relationship between alcohol consumption and internalizing disorders in a longitudinal birth cohort. Drug Alcohol Depend 162:88–91. https://doi.org/10.1016/j.drugalcdep.2016.02.032
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG (2010) Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 67(3):220–229. https://doi.org/10.1001/archgenpsychiatry.2010.2
Gomes AP, Soares ALG, Menezes AMB, Assuncao MC, Wehrmeister FC, Howe LD, Goncalves H (2019) Adiposity, depression and anxiety: interrelationship and possible mediators. Rev Saude Publica 53:103. https://doi.org/10.11606/S1518-8787.2019053001119
Zarza-Rebollo JA, Molina E, Rivera M (2021) The role of the FTO gene in the relationship between depression and obesity. A systematic review. Neurosci Biobehav Rev 127:630–637. https://doi.org/10.1016/j.neubiorev.2021.05.013
Milano W, Ambrosio P, Carizzone F, De Biasio V, Di Munzio W, Foia MG, Capasso A (2020) Depression and obesity: analysis of common biomarkers. Diseases 8(2). https://doi.org/10.3390/diseases8020023
Acknowledgements
M.T.A.O. received research productivity grants from the Brazilian Council for Scientific and Technological Development—CNPq (process n. 307257/2013-4 e 307175/2017-0). J.S.D.C. received research productivity grants from CNPq (process n. 310595/2018-0). A.G. received a post-doctoral fellowship from CNPq (process n. 150215/2021-5).
Funding
This work was supported by the National Council of Technological and Scientific Development (CNPq, grant no. 457235/2014-4). The funder had no role in study design, data collection and analysis, decision to publish and the preparation or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
DGO, AG, JSDC, and MTAO conceived the objective and processed data of this study; DGO, AG, and MTAO analyzed data and drafted the manuscript; DGO, AG, JSDC, and MTAO interpreted the findings and reviewed manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest declared.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of University of Vale do Rio dos Sinos (UNISINOS) (Ethics approval number: 653.394).
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Osmari, D.G., Garcez, A., Dias-da-Costa, J.S. et al. Association between obesity and common mental disorders in women: a population-based study in Southern Brazil. Soc Psychiatry Psychiatr Epidemiol 59, 1577–1585 (2024). https://doi.org/10.1007/s00127-023-02530-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-023-02530-z