Abstract
Purpose
People with mental disorders show mortality rates up to 22.2 times higher than that of the general population. In spite of progressive increase in life expectancy observed in the general population, the mortality gap of people suffering from mental health problems has gradually widened. The aim of this paper was to study mortality rates in people suffering from mental illness in a cohort of people (16,981 subjects) in the local mental health register of the province of Modena during the decade 2006–2015.
Methods
Standardized Mortality Ratios (SMRs) were calculated to compare the mortality of people with mental disorders to the mortality of people living in the province of Modena and the excess of mortality was studied in relation to the following variables: gender, age group, diagnosis and causes of death. In addition, Poisson regression analysis was performed to study the association between patient characteristics and mortality.
Results
An overall excess mortality of 80% was found in subjects under the care of mental health services as compared to the reference population (SMR = 1.8, 95% CI 1.7–1.9). Subjects in the 15–44 year group presented the highest SMR (9.2, 95% CI 6.9–11.4). The most prevalent cause of death was cancer (28.1% of deaths). At the Poisson regression, the diagnosis “Substance abuse and dependence” showed the highest relative risk (RR) (4.00). Moreover, being male, single, unemployed and with a lower qualification was associated with higher RRs.
Conclusions
Our study confirms that subjects with mental illness have higher SMR. Noteworthy, the overall higher risk of mortality was observed in the younger age group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
People with mental disorders have mortality rates up to 22.2 times higher than that of the general population [1], both for natural (e.g., somatic diseases to chronic or acute nature) and “non-natural” (e.g., suicide, accidental traumas) causes [2,3,4,5,6,7].
The diagnosis of schizophrenia, for example, has been associated with a mean reduction in life expectancy of 18 years [8]. Up to 60% of this excess mortality is due to somatic diseases [9]. Several studies have also shown that the excess mortality rates are uniform across different diagnostic groups, including schizophrenia [10], depression [11], bipolar disorder [12, 13], and anorexia nervosa [14]; as well as across different geographic regions (Asia, Europe, America, Australia, Africa) [1]. In addition, mortality risk is increased in all mental health users and not just those who received in-patient treatment [15].
Factors leading to increased mortality rates in individuals suffering from mental illness are complex and not yet fully understood. Psychiatric conditions themselves are not a direct cause of these deaths. Rather, determinants of mortality are identified within a wide spectrum of contingent disorders (e.g., cardiovascular diseases, chronic diseases, infectious diseases) and behaviours (e.g., suicide). The presence of mental illness is also frequently associated with factors that can themselves increase mortality risk, including heritable risk factors, psychotropic treatment and unhealthy lifestyle characterized by poor diet, smoking, physical inactivity and substance abuse [16]. In addition, disparities in health care access and uptake for common conditions such as diabetes, obesity, respiratory and cardiovascular diseases contribute significantly to poorer physical health outcomes for persons with mental illness [17]. For example, individuals with mental illness may be less able to recognize, report and request the help necessary for their physical illnesses [18] and, due to the persistence of stigma and discrimination they may receive poorer medical care as compared to the general population [19]. Further, individuals with mental illness tend to be excluded from preventive medicine programmes, such as cancer screening, vaccinations, counselling for smoking cessation, etc. [18].
Finally, among people with mental illness suicide is the main cause of death, with rates from 8 to 14 times higher in persons suffering from major depression, schizophrenia or affective psychoses [20,21,22].
Since the excess mortality found in people suffering from mental illness is mainly associated with avoidable risk factors [23], it is paramount to study and better understand the relevance of these associations to formulate and implement more effective preventive strategies.
The objective of this study was to evaluate mortality rates in people suffering from mental illness within a defined geographical area, the province of Modena in Northern Italy, evaluating the phenomenon in residents who entered the local mental health register in the decade 2006–2015. Mortality rates were compared with those of the general population in the province of Modena.
Methods
The sample consisted of an open cohort of 16,981 subjects who entered the psychiatric case register of the province of Modena, followed up from 1 January 2006 to 31 December 2015. Those subjects who, during the above period, had only a single contact with a service (n = 1177) and those who turned out not to suffer from a mental disorder (n = 258) were excluded from the analyses. The province of Modena, in 2015, had a population of 702,481 people, with an average mortality rate of about 10 per 1000 residents during the second half of 2010.
Mortality and cause of death were verified through an electronic linkage with the local mortality register (REM: mortality register collection data) and the psychiatric case register (SISM: mental health information system). REM has been used since 1999 and collects information about mortality in the general population of Modena, whilst SISM has been available from 2005 and collects socio-demographics and clinical information of subjects under the care of community mental health services. Both registers were updated every 6 months. All deaths were identified via anonymised identification numbers.
Standardized mortality ratios (SMRs) were calculated, using the indirect method of standardisation, to compare the mortality of people with mental disorders (study population) with the mortality of people living in the province of Modena (reference population). The SMR were estimated by the ratio of observed vs expected numbers of deaths, summed across 5-year age strata. The expected number of deaths per stratum was estimated by applying the age-specific mortality rate in the reference population to the corresponding person-years at risk in the study population (e.g., the expected number of deaths per stratum in women was calculated by multiplying the mortality rate in the same stratum of the general women population by the corresponding person-years). Person-years were calculated as the time in years spent by each subject in the study period, that is before death or before being discharged by the mental health service. Mortality rates of the reference population were provided by the Epidemiology and Risk Management of Azienda Unità Sanitaria Locale (AUSL) of Modena (local public health provider). A SMR of 1 indicates that the mortality risk in the study population was equal to that in the reference (with SMR > 1 indicating an elevated risk and SMR < 1 a lower risk). Tests of the statistical significance of the SMR were established on the Poisson distribution (two-tailed), using 95% confidence intervals (CIs). If CIs do not overlap with unity are statistically significant [23].
The excess of mortality was studied in relation to the following variables: gender, age group, diagnosis and causes of death grouped in four categories (cardiovascular disease, cancer, injuries/poisoning and suicides). All causes of death were defined according to ICD-9-CM classification. Three age groups (15–44, 45–64 and 65+) were considered to assess the mortality risk at different ages. ICD-9 diagnoses were aggregated into seven diagnostic categories: Neuroses (ICD-9 codes 300.xx, 302.xx, 306.xx-316.xx); Bipolar disorders (ICD-9 codes 296.xx); Schizophrenia and other psychosis (ICD-9 codes 295.xx, 297.xx-299.xx); Personality disorders (ICD-9 codes 301.xx); Intellectual disabilities and Organic psychosis (ICD-9 codes 290.xx-294.xx, 317.xx-319.xx); Substance abuse and dependence (ICD-9 codes 303.xx-305.xx); Other diagnoses not yet classified (ICD-9 codes: V70.2 General psychiatric examination, other and unspecified; V71.0 Observation for suspected mental condition). Patients were grouped according to the following characteristics: Qualification (primary or no qualification vs higher qualification); Marital status (unmarried, divorced or widower vs married or in partnership); Occupation (unemployed, retired, disabled, student, housewife vs occupied); Housing status (live alone, residential accommodation, homeless vs subject living with family or partner).
A multivariable Poisson regression analysis was performed to analyse the combined effect of independent variables (gender, age, diagnoses, qualification, marital status, occupation and housing status) on mortality [24, 25].
The model was fit assuming a canonical log-link distribution. Using Poisson regression is possible to present the coefficients in terms of relative risk (RR). A RR < 1 means that the expected number of deaths is lower for this particular value of the variables compared with the value used as referent (protective effect); and patients with a mortality RR > 1 have an increased mortality rate. 95% CIs were also presented.
Analyses were performed using SAS Enterprise Guide, Version 5.1.
Availability of data and materials
Data were gathered from the mental health case registered of Azienda Unità Sanitaria Locale (AUSL) of Modena (local health public provider), matched with the Mortality Register of the province of Modena (REM).
Results
Patients included in the analysis were 16,981 (10,138 women and 6843 men) for a total of 50,396.5 person-years (29,976.6 for women and 20,419.9 for men). During the study period a total of 1148 individuals died (549 women and 599 men). The mean age at the entry was 48 ± 17.4 years, the mean age at death was 72.1 ± 14.6 years.
An overall excess mortality of 80% was found in subjects under the care of mental health services compared to the reference population (SMR = 1.8; 95% CI 1.7–1.9).
SMR by gender, age and diagnostic groups are shown in Table 1.
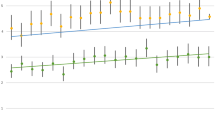
SMR by gender and age group
The mortality risk was 2.1 times that expected in men (95% CI 1.9–2.3) and 1.7 times that expected in women (95% CI 1.6–1.8). SMR decreased with age in both sexes. Those in the 15–44-year group presented the highest risk of death compared to the general age matched population (SMR = 9.2; 95% CI 6.9–11.4).
SMR by diagnosis
SMRs were significantly higher across all the diagnostic groups (see Table 1). However, SMR was particularly high in those with a diagnosis of substance abuse (5.8 times greater than that of the general population). Considering diagnoses by gender, the greatest risk elevation for females was associated with a diagnosis of intellectual disabilities and organic psychiatric conditions (SMR = 2.9, 95% CI 2.4–3.4), and, for males, a diagnosis of substance abuse (SMR = 5.7, 95% CI 3.2–8.3). Moreover, 21.7% of deaths of patients with substance abuse were found in the 15–44 age group.
SMR by causes of death
The most prevalent cause of death was cancer (28.1% of deaths), followed by cardiovascular diseases (25.3%) and injuries/poisoning (9.3%). The number of suicides registered during the decade of the study was 61 (5.3% of total deaths and 57% of deaths from injury and poisoning); 75.4% of suicides were completed by male subjects.
Among natural causes of death an excess mortality was found for cancer (SMR = 1.7; 95% CI 1.5–1.9); this was 1.8 (95% CI 1.5–2.1) in men and 1.7 (95% CI 1.4–2.0) in women. The SMR for cardiovascular diseases was 1.3 (95% CI 1.1–1.4).
In terms of external causes of death (i.e., non-natural) high SMR was observed with respect to suicide (SMR = 12.1, 95% CI 9.1–15.2).
Analysis by age group
The mortality rate was higher in the 15–44 age group for causes of death, psychiatric diagnosis and sex (see Tables 2, 3, 4). SMRs were: 6.4 for cardiovascular diseases, 5.1 for cancer and 25.3 for suicides. Regarding diagnoses, the highest SMR was found in subjects with a diagnosis of substance abuse (SMR = 37.2). Noteworthy, one in five deaths of patients with a diagnosis of substance abuse occurred in the 15–44 age group. Very high mortality excess rates were found also in subjects with intellectual disabilities and personality disorders.
Multivariate analysis
All factors entered in the Poisson regression showed significant RRs except for “housing situation”, namely “living alone, in residential accommodation, homeless” which showed a lower RR as compared to the reference category (i.e., subjects “living with family or partner”). Taking as a reference the category “other non-psychiatric diagnoses”, the RRs was significantly higher with respect to all the diagnoses considered: “substance abuse” (RR 4.00), “personality disorders” (RR 2.75), “intellectual disabilities“(RR 2.74), “neuroses” (RR 1.52), “bipolar disorders” (RR 1.65) and “schizophrenia and other psychoses” (RR 2.29). Other factors associated with significantly greater risk of mortality (Table 5) included: male gender (RR 1.55), unemployment (i.e., “unemployed, retired, disabled, student or housewife”) (RR 1.67), low education (i.e., “primary or no qualification”) (RR 1.31) and civil status (i.e., “unmarried, divorced, widower”) (RR 1.31).
Discussion and conclusions
Despite progressive increases in life expectancy in the general population, the mortality gap of people suffering from mental illness has gradually widened: this is true for a large number of psychopathological conditions [1]. Even in countries with a comprehensive, accessible welfare system, with an overall high quality of public health services, the risk of mortality from cardiovascular disease in people with severe mental illness has risen by five times for men and three times for women during the last decades as compared to general population [24]. The increase in mortality risk for people with mental illness is even larger when looking at younger age groups.
Our study confirms these data: people with mental disorders have higher SMR than other members of the general population. A major concern is that the overall higher risk of mortality was observed in the younger age group: the 15–44 age group showed the highest SMR: 9.2 (versus 2.9 of 45–64 group, and 1.4 of 65+ group). Suicide rates found in younger patients were extremely elevated compared to their peers (SMR: 25.3). Increased mortality in the younger population was more pronounced in individuals with substance use disorders, personality disorders and intellectual disabilities. These findings confirm that young people suffering from mental illness present highest relative risk of mortality [1].
In terms of SMR by cause of death our sample showed a smaller increase of risk for cardiovascular diseases (SMR: 1.3) as compared with previous studies: [6, 25]. However, cardiovascular risk found in our sample was particularly high in younger subjects (SMR: 6.4). This is consistent with Osborn et al. [26] and Foley et al. [27]. The lower SMR found in our sample might be explained, at least in part, by the relatively high prevalence of patients with diagnosis of neuroses (52.4% of the sample), a diagnostic group whose lifestyle is generally less pervasively affected by unhealthy behaviours and less exposed to antipsychotic medications iatrogenic effects.
There is broad consensus regarding increased mortality for cancer in the population suffering from mental illness, although with some variability with respect to type and site of cancer [28, 29]. Several factors have been associated with the risk for developing malignancies and receiving late diagnosis: unhealthy lifestyle (e.g., smoking, substance/alcohol abuse), underestimation of somatic morbidity, such as blood-borne viral infections (e.g., hepatitis B or C) [30] and interpreting physical complaints as “psychosomatic” by health professionals. As a matter of fact, a comparative meta-analysis showed significant disparity, with regards to rates of mammography screening, in women with mental disorders compared to the general population [31]. Not least, physical problems may be underreported by individuals with mental illness [32]. Cancer SMRs in our sample, were consistent with available data, representing the most frequent natural cause of death (28.1%); interestingly, the analysis showed highest SMR for cancer in younger subjects.
A diagnosis of substance abuse disorder showed the highest SMR among all diagnostic groups; SMRs were higher both in the whole sample and in each age group with the only exception of the 65+ subjects. Non-accidental poisoning, traffic related-accidents and suicide are highly represented in people with drug abuse, despite they may be under-estimated (e.g., drug intoxications might be reported as “overdose” and therefore may not appear as suicide attempts in the statistics) [33]. People suffering from substance abuse are 10 times more likely to commit suicide in case of alcohol abuse and 14 times higher in case of intravenous drug use compared to the general population [34]. Up to 40% of patients requesting access to drug abuse services have been reported as having a history of suicide attempts.
Our results make the case that attention and prevention efforts should deal with the high mortality rate observed in the 15–44 age group with personality disorders as well as intellectual disabilities/organic disorders. Large population studies, recently provided evidence of substantially increased SMRs across all clusters of personality disorders [35] along with sub-optimal assessment of physical health [36]. Less information is available regarding the health status of people with intellectual disabilities [37, 38]. This requires more systematic investigation, as this group shows a trend toward premature and avoidable deaths [39].
Relative risk of mortality was significantly elevated in subjects outside the labour market, who were unmarried, divorced, or widowed and with low levels of education. These findings could be interpreted as the negative additional effect exerted by social determinants of mental health on mortality risk. However, it is not possible to rule out a reversal causality, i.e., the conditions considered (marital status, unemployment, low education) being an effect, rather than a consequence, of mental illness.
There are some limitations of this study. Our sample was represented by subjects in the register of general psychiatric services and did not include individuals whose conditions were managed solely by general practitioners or by drug and alcohol services. This is likely to have resulted in underestimating the scale of the problem. Second, the use of medication was not included in the analysis. Controversy is ongoing regarding the impact of psychotropic medication on mortality in people with mental illness, especially concerning antipsychotic medication. While there is increasing evidence suggesting a protective effect of antipsychotic and antidepressants on mortality in people suffering from severe mental illness [40], for schizophrenia in particular [41, 42], it is widely acknowledged that several psychotropic treatments, with particular reference to antipsychotic drugs, increase the incidence of metabolic disturbances linked to the risk of cardiovascular complications [43, 44].
The mortality gap between people suffering from mental illness and the general population, as found in the current study, reinforces the notion of inequitable access to physical care for users of mental health services [45]. If the goal is indeed to reduce the mortality gap, equity of access to all levels of care and intervention (acute and long-term care, preventive medicine and health promotion) should be guaranteed. The available evidence, instead, suggests that interventions such as smoking cessation, which are effective also in people suffering from severe mental illness are not given the appropriate priority and resources in clinical practice [46, 47].
Our findings confirm the importance of overcoming institutional barriers to equitable access, particularly in younger subjects, who are at very substantial higher risk of mortality compared to their peers. In addition, the very high mortality excess found in people with substance use disorders, demands the rethinking of policies addressing the way the health system (and, possibly, society as a whole) interact with this vulnerable group.
At policy level, to arrest the excess mortality of people suffering from mental illness, it seems necessary to broaden the availability of preventive medicine and achieve a better integration between mental health and primary care services. These interventions must be universal and include individuals with high mortality risk. In our opinion, this is the only way to overturn the ongoing disparities faced by people with mental illness.
References
Walker ER, McGee RE, Druss BG (2015) Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry 72(4):334–341. https://doi.org/10.1001/jamapsychiatry.2014.2502
Chesney E, Goodwin GM, Fazel S (2014) Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry 13(2):153–160. https://doi.org/10.1002/wps.20128
Harris EC, Barraclough B (1998) Excess mortality of mental disorder. Br J Psychiatry 173:11–53
Charlson FJ, Baxter AJ, Dua T, Degenhardt L, Whiteford HA, Vos T (2016) Excess mortality from mental, neurological, and substance use disorders in the global burden of disease study 2010. In: Patel V, Chisholm D, Dua T, Laxminarayan R, Medina-Mora ME (eds) Mental, neurological, and substance use disorders: disease control priorities, 3rd edn (vol 4). The International Bank for Reconstruction and Development / The World Bank, Washington (DC). https://doi.org/10.1596/978-1-4648-0426-7_ch3
Nordentoft M, Wahlbeck K, Hallgren J, Westman J, Osby U, Alinaghizadeh H, Gissler M, Laursen TM (2013) Excess mortality, causes of death and life expectancy in 270,770 patients with recent onset of mental disorders in Denmark, Finland and Sweden. PLoS One 8(1):e55176. https://doi.org/10.1371/journal.pone.0055176
Hoye A, Nesvag R, Reichborn-Kjennerud T, Jacobsen BK (2016) Sex differences in mortality among patients admitted with affective disorders in North Norway: a 33-year prospective register study. Bipolar Disord 18(3):272–281. https://doi.org/10.1111/bdi.12389
Lawrence D, Jablensky AV, Holman CD, Pinder TJ (2000) Mortality in Western Australian psychiatric patients. Soc Psychiatry Psychiatr Epidemiol 35(8):341–347
Chang CK, Hayes RD, Perera G, Broadbent MT, Fernandes AC, Lee WE, Hotopf M, Stewart R (2011) Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS One 6(5):e19590. https://doi.org/10.1371/journal.pone.0019590
Doherty AM, Gaughran F (2014) The interface of physical and mental health. Soc Psychiatry Psychiatr Epidemiol 49(5):673–682. https://doi.org/10.1007/s00127-014-0847-7
Saha S, Chant D, McGrath J (2007) A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry 64(10):1123–1131. https://doi.org/10.1001/archpsyc.64.10.1123
Cuijpers P, Vogelzangs N, Twisk J, Kleiboer A, Li J, Penninx BW (2014) Comprehensive meta-analysis of excess mortality in depression in the general community versus patients with specific illnesses. Am J Psychiatry 171(4):453–462. https://doi.org/10.1176/appi.ajp.2013.13030325
Roshanaei-Moghaddam B, Katon W (2009) Premature mortality from general medical illnesses among persons with bipolar disorder: a review. Psychiatr Serv 60(2):147–156. https://doi.org/10.1176/appi.ps.60.2.147
Hayes JF, Miles J, Walters K, King M, Osborn DP (2015) A systematic review and meta-analysis of premature mortality in bipolar affective disorder. Acta Psychiatr Scand 131(6):417–425. https://doi.org/10.1111/acps.12408
Keshaviah A, Edkins K, Hastings ER, Krishna M, Franko DL, Herzog DB, Thomas JJ, Murray HB, Eddy KT (2014) Re-examining premature mortality in anorexia nervosa: a meta-analysis redux. Compr Psychiatry 55(8):1773–1784. https://doi.org/10.1016/j.comppsych.2014.07.017
Kisely S, Smith M, Lawrence D, Maaten S (2005) Mortality in individuals who have had psychiatric treatment: population-based study in Nova Scotia. Br J Psychiatry 187:552–558. https://doi.org/10.1192/bjp.187.6.552
Brown S, Inskip H, Barraclough B (2000) Causes of the excess mortality of schizophrenia. Br J Psychiatry 177:212–217
Hert DE, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, Detraux J, Gautam S, Moller HJ, Ndetei DM, Newcomer JW, Uwakwe R, Leucht S (2011) Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry 10(1):52–77
Druss BG, Bradford WD, Rosenheck RA, Radford MJ, Krumholz HM (2001) Quality of medical care and excess mortality in older patients with mental disorders. Arch Gen Psychiatry 58(6):565–572
Henderson C, Noblett J, Parke H, Clement S, Caffrey A, Gale-Grant O, Schulze B, Druss B, Thornicroft G (2014) Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry 1(6):467–482. https://doi.org/10.1016/S2215-0366(14)00023-6
Lawrence D, Kisely S, Pais J (2010) The epidemiology of excess mortality in people with mental illness. Can J Psychiatry 55(12):752–760
Pan CH, Jhong JR, Tsai SY, Lin SK, Chen CC, Kuo CJ (2014) Excessive suicide mortality and risk factors for suicide among patients with heroin dependence. Drug Alcohol Depend 145:224–230. https://doi.org/10.1016/j.drugalcdep.2014.10.021
Harris EC, Barraclough B (1997) Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry 170:205–228
Crompton D, Groves A, McGrath J (2010) What can we do to reduce the burden of avoidable deaths in those with serious mental illness? Epidemiol Psichiatr Soc 19(1):4–7
Osby U, Correia N, Brandt L, Ekbom A, Sparen P (2000) Time trends in schizophrenia mortality in Stockholm county, Sweden: cohort study. BMJ 321(7259):483–484
Amaddeo F, Bisoffi G, Bonizzato P, Micciolo R, Tansella M (1995) Mortality among patients with psychiatric illness. A ten-year case register study in an area with a community-based system of care. Br J Psychiatry 166(6):783–788
Osborn DP, Levy G, Nazareth I, Petersen I, Islam A, King MB (2007) Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s General Practice Rsearch Database. Arch Gen Psychiatry 64(2):242–249. https://doi.org/10.1001/archpsyc.64.2.242
Foley DL, Mackinnon A, Watts GF, Shaw JE, Magliano DJ, Castle DJ, McGrath JJ, Waterreus A, Morgan VA, Galletly CA (2013) Cardiometabolic risk indicators that distinguish adults with psychosis from the general population, by age and gender. PLoS One 8(12):e82606. https://doi.org/10.1371/journal.pone.0082606
Biggeri A, Catelan D (2010) The methodological and conceptual aspects of mortality studies in psychiatry. Epidemiol Psichiatr Soc 19(1):16–20
Guan NC, Termorshuizen F, Laan W, Smeets HM, Zainal NZ, Kahn RS, De Wit NJ, Boks MP (2013) Cancer mortality in patients with psychiatric diagnoses: a higher hazard of cancer death does not lead to a higher cumulative risk of dying from cancer. Soc Psychiatry Psychiatr Epidemiol 48(8):1289–1295. https://doi.org/10.1007/s00127-012-0612-8
Hughes E, Bassi S, Gilbody S, Bland M, Martin F (2016) Prevalence of HIV, hepatitis B, and hepatitis C in people with severe mental illness: a systematic review and meta-analysis. Lancet Psychiatry 3(1):40–48. https://doi.org/10.1016/S2215-0366(15)00357-0
Mitchell AJ, Pereira IE, Yadegarfar M, Pepereke S, Mugadza V, Stubbs B (2014) Breast cancer screening in women with mental illness: comparative meta-analysis of mammography uptake. Br J Psychiatry 205(6):428–435. https://doi.org/10.1192/bjp.bp.114.147629
Musuuza JS, Sherman ME, Knudsen KJ, Sweeney HA, Tyler CV, Koroukian SM (2013) Analyzing excess mortality from cancer among individuals with mental illness. Cancer 119(13):2469–2476. https://doi.org/10.1002/cncr.28091
Delaveris GJ, Konstantinova-Larsen S, Rogde S (2014) Unnatural deaths among drug abusers. Tidsskr Nor Laegeforen 134(6):615–619. https://doi.org/10.4045/tidsskr.13.0884
Yuodelis-Flores C, Ries RK (2015) Addiction and suicide: a review. Am J Addict 24(2):98–104. https://doi.org/10.1111/ajad.12185
Bjorkenstam E, Bjorkenstam C, Holm H, Gerdin B, Ekselius L (2015) Excess cause-specific mortality in in-patient-treated individuals with personality disorder: 25-year nationwide population-based study. Br J Psychiatry 207(4):339–345. https://doi.org/10.1192/bjp.bp.114.149583
Sanatinia R, Middleton SM, Lin T, Dale O, Crawford MJ (2015) Quality of physical health care among patients with personality disorder. Personal Ment Health 9(4):319–329. https://doi.org/10.1002/pmh.1303
Robertson J, Hatton C, Emerson E, Baines S (2015) Mortality in people with intellectual disabilities and epilepsy: a systematic review. Seizure 29:123–133. https://doi.org/10.1016/j.seizure.2015.04.004
Heslop P, Blair PS, Fleming P, Hoghton M, Marriott A, Russ L (2014) The confidential inquiry into premature deaths of people with intellectual disabilities in the UK: a population-based study. Lancet 383(9920):889–895. https://doi.org/10.1016/S0140-6736(13)62026-7
Robertson J, Baines S, Emerson E, Hatton C (2017) Service responses to people with intellectual disabilities and epilepsy: a systematic review. J Appl Res Intellect Disabil 30(1):1–32. https://doi.org/10.1111/jar.12228
Baxter AJ, Harris MG, Khatib Y, Brugha TS, Bien H, Bhui K (2016) Reducing excess mortality due to chronic disease in people with severe mental illness: meta-review of health interventions. Br J Psychiatry 208(4):322–329. https://doi.org/10.1192/bjp.bp.115.163170
Tiihonen J, Mittendorfer-Rutz E, Torniainen M, Alexanderson K, Tanskanen A (2016) Mortality and cumulative exposure to antipsychotics, antidepressants, and benzodiazepines in patients with schizophrenia: an observational follow-up study. Am J Psychiatry 173(6):600–606. https://doi.org/10.1176/appi.ajp.2015.15050618
Vanasse A, Blais L, Courteau J, Cohen AA, Roberge P, Larouche A, Grignon S, Fleury MJ, Lesage A, Demers MF, Roy MA, Carrier JD, Delorme A (2016) Comparative effectiveness and safety of antipsychotic drugs in schizophrenia treatment: a real-world observational study. Acta Psychiatr Scand 134(5):374–384. https://doi.org/10.1111/acps.12621
De Hert M, Cohen D, Bobes J, Cetkovich-Bakmas M, Leucht S, Ndetei DM, Newcomer JW, Uwakwe R, Asai I, Moller HJ, Gautam S, Detraux J, Correll CU (2011) Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry 10(2):138–151
Zhang Q, Deng C, Huang XF (2013) The role of ghrelin signalling in second-generation antipsychotic-induced weight gain. Psychoneuroendocrinology 38(11):2423–2438. https://doi.org/10.1016/j.psyneuen.2013.07.010
Moore S, Shiers D, Daly B, Mitchell AJ, Gaughran F (2015) Promoting physical health for people with schizophrenia by reducing disparities in medical and dental care. Acta Psychiatr Scand 132(2):109–121. https://doi.org/10.1111/acps.12431
Stubbs B, Vancampfort D, Bobes J, De Hert M, Mitchell AJ (2015) How can we promote smoking cessation in people with schizophrenia in practice? A clinical overview. Acta Psychiatr Scand 132(2):122–130. https://doi.org/10.1111/acps.12412
Mitchell AJ, Vancampfort D, De Hert M, Stubbs B (2015) Do people with mental illness receive adequate smoking cessation advice? A systematic review and meta-analysis. Gen Hosp Psychiatry 37(1):14–23. https://doi.org/10.1016/j.genhosppsych.2014.11.006
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Ethics statement
Ethical approval was not required as this study was performed as secondary data analysis on anonymous datasets.
Rights and permissions
About this article
Cite this article
Starace, F., Mungai, F., Baccari, F. et al. Excess mortality in people with mental illness: findings from a Northern Italy psychiatric case register. Soc Psychiatry Psychiatr Epidemiol 53, 249–257 (2018). https://doi.org/10.1007/s00127-017-1468-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-017-1468-8