Abstract
Purpose
Yearly, 600,000 people complete suicide in low- and middle-income countries, accounting for 75% of the world’s burden of suicide mortality. The highest regional rates are in South and East Asia. Nepal has one of the highest suicide rates in the world; however, few investigations exploring patterns surrounding both male and female suicides exist. This study used psychological autopsies to identify common factors, precipitating events, and warning signs in a diverse sample.
Methods
Randomly sampled from 302 police case reports over 24 months, psychological autopsies were conducted for 39 completed suicide cases in one urban and one rural region of Nepal.
Results
In the total police sample (n = 302), 57.0% of deaths were male. Over 40% of deaths were 25 years or younger, including 65% of rural and 50.8% of female suicide deaths. We estimate the crude urban and rural suicide rates to be 16.1 and 22.8 per 100,000, respectively. Within our psychological autopsy sample, 38.5% met criteria for depression and only 23.1% informants believed that the deceased had thoughts of self-harm or suicide before death. Important warning signs include recent geographic migration, alcohol abuse, and family history of suicide.
Conclusions
Suicide prevention strategies in Nepal should account for the lack of awareness about suicide risk among family members and early age of suicide completion, especially in rural and female populations. Given the low rates of ideation disclosure to friends and family, educating the general public about other signs of suicide may help prevention efforts in Nepal.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Suicide accounts for over 800,000 deaths per year, killing more than war and natural disasters combined [1]. Low and middle income countries (LMIC) hold more than 75% of the global suicide burden, but only a fraction of the research exploring risk factors and prevention strategies [1, 2]. LMIC in South–East Asia hold the largest proportion of the world’s suicides (39.1%) as well as the highest regional rate (17.7 per 100,000) [1]. In Asia, characteristics of people that die by suicide are distinctly different from other regions where the male–female ratio for suicide deaths is much closer to one (in high-income countries, this ratio is 3.5), there are lower proportions of mental disorders, differing methods, and more rural suicides [3,4,5]. Common risk factors for suicides in low-income settings include existing mental illness, history of suicide attempt, low socio-economic position, poverty, and other socio-cultural characteristics [4, 6,7,8,9]. Despite general recognition that common risk factors for suicide exist across cultures, suicide remains complex and difficult to predict. Moreover, although links between culture and suicide have been established, measures used to assess culture have been overly simplistic, often reduced to geographic origin or nationality. Thus, recent academic calls have specifically emphasized the need for broader investigations in suicide studies [10, 11]. Inquiries examining the personal lives of those that have died, their social circumstances, culture, and their interactions with broader social and political structures may be of crucial importance to better understand suicidality.
The psychological autopsy (PA) method is well suited to explore suicide from multiple dimensions. This approach will be beneficial in order to untangle disparate suicide rate estimations and severe under-reporting that is common in LMIC. Nepal is a useful example of how mismatches in suicide rate estimates confuse health and policy makers, stunting response to a potentially large burden of death [12]. In 2012, the World Health Organization estimated Nepal to have an overall age-standardized suicide rate of 24.9, ranking it the 8th highest rate in the world. The country’s estimated female suicide rate ranks 3rd highest (20.0) and male rate ranks 17th highest (30.1) [1]. However, the Global Burden of Disease estimates Nepal to have a suicide rate of just 6.21, 5.07, and 7.43 for overall, females, and males, respectively [13]. Community-based reports have purported that suicide is the leading killer among women of reproductive age [14, 15]. Police estimates are lower than both community and global estimates, but they do indicate a steady increase in suicide over the last decade [15]. To further complicate existing evidence, most suicide research in Nepal explores only female suicides or suicides that present to health institutions, leaving gaps in understanding what drives suicide in males, those in younger and older age groups, and those that do not present to health facilities [12].
This study sought to address these gaps by exploring both male and female suicides of any age through a mixed-methods modified psychological autopsy (PA) approach. To date, no studies have been published using this method in Nepal. Moreover, most suicide data for low-income countries is limited to WHO cross-national studies that include prevalence and characteristics associated with ideation and attempts [16,17,18]. Therefore, LMIC data lack information related explicitly to suicide deaths. The PA method is a resource intensive and rich source of data for people that have died by suicide. Although other larger PA case–control studies have made population-level generalizations, the following study presents rich findings on a case-series of suicides in both urban and rural Nepal, reporting on common precipitants and variations across geography and gender. We discuss the findings in the context of Nepal’s broader health system and propose prevention activities suitable for LMIC. Finally, we critically engage with the strengths and limitations of such studies in low-income settings and discuss important future research to shed more light on an often ignored public health topic.
Methods
This particular study was situated within a larger study aimed at understanding the cultural, institutional, and social factors contributing to suicide and implications for public health practice in Nepal [12]. The authors conducted a mixed-methods PA case-series study. This culturally grounded approach allows informants to share detailed accounts of suicide circumstances including warning signs, contributing factors, help-seeking, and various impacts on the family and community. We call this approach mixed-method psychological autopsy for cross-cultural research (MPAC). The findings presented here are the quantitative results with a focus on the events and circumstances that preceded the suicide death and its variation across our sub-samples.
Informant identification and selection
A census of all deaths reported to the police in the previous 2 years was collected as a part of the larger surveillance study. After obtaining permission from police personnel at the national, district, and neighborhood levels, the authors worked alongside data managers to identify relevant information from each case identified as a suicide within hand-written investigation documents. This approach has been used in other PA studies [19, 20]. In the rural field site, the district police office houses all investigation records related to suicide cases. In Kathmandu, due to its high population, 14 police offices serve different sectors of the municipality. For feasibility, the authors randomly selected half of police offices for investigation. Following case-gathering, a list of all suicide cases in each geographic location was created and stratified based on gender. From a total of 302 suicide cases, the authors randomly selected cases to contact, ensuring an equal amount of male and female decedents were represented. To ensure geographic representation, we conducted the above procedure for each police station, randomly contacting individuals until we reached at least two cases per geographic region in Kathmandu. Identifying information for the individual that reported the case was used to contact the family. The authors worked with local community leaders and a local psychosocial organization to identify the bereaved family and invite participation.
Inclusion criteria required that the suicide occurred between 6 months and 2 years prior, participants be 18 years or older, knew the decedent well (a family member or close friend that interacted with the decedent on a regular basis), and were comfortable discussing the events surrounding the suicide. If the informant preferred, they suggested another family member that the study team should contact to request study participation. Nineteen of the 39 interviews included multiple family informants in order to triangulate information. As in common in PA studies, in instances of disagreement, the presence of a factor (e.g., the ending of a romantic relationship) or the response of more severity was retained.
Following informed consent, the survey protocol was conducted in-person by the lead author (proficient in Nepali) and one research assistant and audio recorded. Research assistants were skilled Nepali researchers fluent in both Nepali and English that worked for TPO-Nepal, a Nepali psychosocial non-governmental organization. They were trained in project aims and protocol, interviewing and active listening techniques, procedures for maintaining confidentiality, identifying distress and initiating referral pathways, and other ethical aspects of the study. Additionally, regular meetings were used to review the aforementioned concepts as well as to discuss findings. All interviews were conducted in Nepali.
Instruments and procedures
Data were collected between December 2015 and March 2016 in one rural district (Jumla) and one urban district (Kathmandu) in Nepal. These districts were selected in order to maximize variation based on geography as previous studies have suggested varying patterns. Additionally, these locations ensured that psychosocial services were accessible to participants. The questionnaire combined structured close-ended questions and psychometric instruments. The qualitative methods and findings are discussed elsewhere. The structured closed ended section followed the themes outlined in the original PA method [21] as well as more recent approaches [22, 23]. The lead author has used this method in a US-based ethnically Nepali Bhutanese refugee population experiencing high suicide rates [24]. To assess histories of depression, we used the Nepali Patient Health Questionnaire (PHQ-9), a widely used instrument around the world that has been locally validated and proven to perform well in our target population: locally validated cutoff ≥10: sensitivity = 0.94, specificity = 0.80 [25]. We also asked informants if the deceased experienced any mental illness (prompted with local terms for depression, schizophrenia, anxiety, and trauma) or if they were ever treated for one. If respondents responded yes, we asked if it was present within 3 months of the death. Abuse was assessed by asking if the deceased was ever beaten by any individual and coded as present if it occurred within 3 months of the death. Closed-ended questions also collected demographics, significant and traumatic life events including abuse, migration and household movement, social support, personal, family and social history of mental illness and suicide, and details surrounding the suicide.
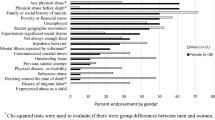
Analytic methods
Simple descriptive analyses were conducted for quantitative data stratifying by both gender and geographic region to explore significant differences in demographic and suicide-related characteristics. All quantitative data were double-entered into Excel, crosschecked, and corrected using Excel Compare v3.0.2. We used SPSS V20.0 for statistical analyses. Associations were evaluated for statistical significance at 0.05 using two-tailed tests for continuous variables and Chi-square tests for categorical variables. To calculate PHQ-9 scores, individual item scores and the percentage in which the respondent was unable to answer were reported. Mean scores were calculated only for the total reported items. The mean score was then multiplied by nine to account for responsiveness. Suicide rates were calculated according to methods used by the US Centers for Disease Control and Prevention [26].
Results
Police sample findings
Within the police sample, the majority of deaths were male (57%), with a male to female ratio of 1.32 overall, 1.34 in Kathmandu, and 1.21 in Jumla. Over 40% of decedents were 25 years or younger. Female deaths and rural deaths were significantly younger, compared to males and urban deaths respectively. See Fig. 1 for patterns across age groups, gender, and region. The most common method was hanging (62.9%) followed by poison (30.8%). Method did not differ by gender or location. Based on the Nepal housing census, we estimate Kathmandu’s overall annual crude rate at 18.8 per 100,000 (ranging from 16.6 to 28.2 depending on administrative area) and Jumla’s overall annual crude rate at 30.1 per 100,000 (ranging from zero to 164.1 depending on administrative area). In Jumla, rates were highest in regions with a police station, indicating possible under-reporting due factors such as access and stigma.
Psychological autopsy sub-sample findings
The majority of respondents were a male primary relative. Respondent religion and caste always matched that of the deceased. The average time between the suicide event and the interview was 18 months. Table 1 outlines the variations in case responses across study sites. There was no significant demographic variation in our consented sample compared to the police sample as a whole. There were also no differences in decedent characteristics between those who consented and those who refused participation. Refusal (n = 43) was most often due to the respondent living outside the district so that a face-to-face interview could not be conducted followed by discomfort discussing the topic. Our total sub-sample randomly selected and consented 39 cases.
The sub-sample’s characteristics are outlined in Table 2, where women were significantly younger than men, more likely to be a student, and more likely to be cited as having a mental disorder. Deceased female were significantly younger than males. Decedents were mostly married (66.7%), of Brahman or Chhetri caste (59%), Hindu (87.2%), and had no regular income (71.8%). The majority did not pass the SLC exam (53.8%), the qualifying exam to advance on to higher education (10th grade completion in the United States’ educational system). Most informants stated that the physical health of the deceased was poor (61.1%). About one-third of the male decedents were migrant workers at some point in their lives.
Jumla decedents were younger, lower caste (35%, p = 0.011), did not own their own home, and more likely to be a student. No other significant differences were found across socio-demographic characteristics.
Suicide characteristics
Across the total sample, the majority of cases died by hanging (64.1%), followed by poisoning (28.2%). Choice of method did not vary across gender. Most deaths occurred within the decedent’s own home (76.9%). On the day of the suicide, about half of the male decedents were reported to have consumed alcohol (52.4%), but very few women (16.7%). Most female decedents were reported to have endured physical abuse within 3 months of the time of suicide (61.1%), but no men. Few cases had a reported previous suicide attempt (10.3%). Many of the cases (48.7%) had relocated to a new residence within a year of their suicide. About one-third of the men (33.3%) had participated in migrant labor. More than half of the decedents had lost a family member or close friend to suicide (61.5%). All suicide characteristics stratified by gender and geography are summarized in Table 2.
Mental illness and PHQ-9 results
Reporting the presence of a mental illness varied by gender. For female cases, 22.2% were reported to have had a mental illness at the time of their death (three cases were reported to have had depression and one case had psychotic symptoms). No male cases were reported to have had a mental illness. Three of the four female cases had sought professional medical care (one a physician, one a psychiatrist, and one both a physician and a traditional healer). Within the total sample, PHQ-9 results indicated that 15 cases (38.5%) met the criteria for depression (PHQ-9 ≥10). Inventory items with the highest average scores included item 1 (feeling unhappy or not enjoying activities), item 2 (feeling frustrated or despairing), item 4 (feeling tired and lacking energy), and item 5 (blaming themselves) (Table 3). The lowest average score was for item 9 (suicidal ideation/thoughts), where only 23.1% of informants reported that the decedent expressed feelings of hurting themselves, dying, or doing suicide.
Discussion
Using an in-depth case review of police records and MPAC with a random subset of cases, we found that the greatest burden of suicide is below the age 26, accounting for 40% of suicide police reports. The burden among youth was greatest in rural areas where two out of three suicides occurred in this age-group. Similarly, half of all female suicide completions were among girls under 26 years. This proportion is large compared to 2015 suicide distributions in the US, where only 15.1% of all suicide deaths and 14.1% of female suicide deaths, occur under 26 years [26]. Nepal’s proportion is much higher. Findings revealed risk factors including geographic movement, histories of migrant labor, and family history of suicidal behavior. According to informants’ knowledge, one out of five female suicide completers had a mental illness and none of the male suicide completers did. Based on PHQ-9 scores, two out of five suicide completers would have met criteria for depression. One of the most surprising findings was that less than one-quarter of informants reported knowledge of thoughts of self-harm, death, or suicide among the completers prior to their deaths.
Overall, our findings indicate that the Nepali suicide profile is similar to patterns found in India and China. While the majority of individuals used hanging, one-third of the suicide deaths in our Nepal sample were due to poison. This highly lethal method is also common in low-income settings due to accessibility and little regulation [27]. In our sample, when compared to estimated populations in Kathmandu, higher castes (Brahman/Chhetri) were over-represented [28]. In Nepal, caste is often associated with social capital where high-caste individuals are more likely to be educated, employed, and economically productive [29]. This might indicate important differences in suicide patterns marked by geography and development. In India, in highly developed areas where individuals have high education and wealth, but low opportunity, suicide rates are highest [30]. This conflict is theorized to justify and propel suicidal behaviors, as aspirations are impossible to attain [31]. Other low-income studies also found that those with higher education had higher rates of depression, suggesting that when high academic achievement does not result in economic prosperity, mental health suffers [32, 33]. This may also be the case in urban Kathmandu, although we do not see similar patterns with education. In fact, across sites, only one-quarter of decedents achieved high-school level education. In Jumla, low-caste individuals were over-represented, suggesting that in severely low-resourced rural areas, the development expectation theory may not hold.
The majority of suicides in our sample cited stressors of poverty and unemployment. In other low-income countries, stressful life events such as crop failure, debt, and loss of control were connected to suicidal behavior [20, 34,35,36,37]. Contextualizing suicide in a broader socio-political milieu emphasizes how social conditions and expectations may be important contributors, and should be considered alongside mental health status [38].
In high-income countries, marriage and having children is a protective factor for both men and women [39]. In our findings, the majority were married with children, indicating such risk factors do not hold across cultures and countries. In Nepal, marriage and family bring additional social problems. Men must provide for their families, while women endure pressure to have sons, endure abuse, and often live with difficult expectations and pressure from extended household members [40, 41]. Moreover, many female cases had reports of physical abuse, but no men. Nepal’s 2011 DHS study found 22% of women and 28% of married women experienced physical and spousal violence in their lifetime, respectively [42]. Qualitative studies found that Nepali women often attribute spousal violence to alcohol, but it is a wife’s duty to endure and remain supportive and loyal to her husband [43, 44]. Our findings echo these studies and perhaps highlight the difficulty women face when negotiating their personal wellbeing with pervasive social expectations. Other studies from LMIC found that suicide attempts were significantly associated with domestic violence [45] and, contrasting to US evidence, marriage was a risk factor for completed suicide, especially among women [46, 47]. Other factors, such as alcohol consumption, previous suicide attempts, and family history of suicide seem to be universal risk factors [48,49,50]. However, in our findings, suicide attempts were rarely mentioned. This may be due to method lethality, where attempt survival is rare.
Geographic migration emerged as another important factor in our results. For men, returning from a migrant labor job overseas or moving for school caused most relocation. For women, following patrilocal tradition, movement into the husband’s house after marriage was most often the reason for migration. Nepal is a highly collective society, and individuals typically live in multigenerational households. Migration often meant moving to a single room, resulting in isolation. In India, researchers found that nearly 60% of suicides were migrants from other countries [51]. Additional investigations exploring associations between geographic movements and suicidal behavior are limited. The authors recommend further investigation into this topic, particularly as it may be a viable screening item in both clinical and community settings.
Much of the PA literature focuses on findings related to mental disorders. We found few descriptions of mental disorders, particularly among men. However, deceased individuals were commonly described as ‘impulsive,’ ‘aggressive,’ and had difficulties controlling their emotions, indicating emotional dysregulation. Aggressiveness and impulsivity have consistently been associated with increased risk of suicidal behavior [52,53,54]. Lower levels of mental illness have been found among individuals that died by suicide in China [23, 55, 56]. One potential reason for few PAs documenting mental illness in our study and other low- and middle-income countries is the low level of mental health literacy, which is associated with limited awareness and recognition of mental illness. For example, in a cross-national study of 21 countries, 65% of persons meeting criteria for depression in high-income countries endorsed need for treatment of a disorder compared with 35% in lower-middle income countries [57]. In India, the VISHRAM project, an 18-month community-based program to enhance mental health literacy as pathway to reduce suicide risk, resulted in increased conceptualization of depression as a mental health problem and greater intention to seek care for depression, with a sixfold increase in contact coverage (treatment seeking) [58].
Most individuals in our study were poor and economic stressors were commonly mentioned. Only 15% of our informants mentioned that economic concerns were not present. Previous evidence in Nepal indicated that caste was significantly associated with higher depression and anxiety scores, with the majority of caste-differences in depression mediated by socio-economic deprivation [59, 60]. We found no distinct patterns related to caste (although our study is not a population generalizable sample). Larger reviews have found that social position and poverty seemed to contribute to suicide at the individual level, but differences at the country level are difficult to decipher [4, 5, 61].
Few individuals in our sample had sought care for any kind of mental disorder. Particularly in settings where mental health care is inadequate, pairing community-based strategies for prevention with simple clinical screening may be most effective [62,63,64]. Integrating police, health professionals, and community health workers in crisis response teams has shown early efficacy in LMIC [65], along with strategies for integrating mental health into primary care [66], and controlling access to means [67, 68].
In Nepal, a recent study found suicide disclosure to family/friends and help-seeking to be very low, suggesting that active clinical screening maybe a useful strategy for prevention [69]. Compared to depression, a more sensitive marker of risk in Nepal may include having a family member or close friend that recently engaged in suicidal behavior. Based on our findings, screening and detection in clinical settings could address the following risk factors: (1) If a family/social history of suicide is endorsed, the individual should automatically receive suicide prevention support. (2) If an individual has two of the following: recent geographic movement, extensive alcohol use, or symptoms of depression, the individual should receive suicide prevention support. Because individuals seem to be unlikely to disclose suicidal ideation to family members, asking the aforementioned questions during clinical and community health encounters would be vital for detection and risk assessment of an individual’s propensity for suicidal behavior.
Limitations
General limitations of the psychological autopsy method have been previously documented [11, 20, 70] and results should be interpreted with caution. For example, due to the sensitive content and reliance on verbal interviewing methods, respondent bias may have influenced informant responses due to guilt or shame. Additionally, as our respondent sample includes a variety of relationships to the deceased, the content and quality of information regarding the suicide death may be quite varied and limit the accuracy, depth, and breadth of recall for each case. Moreover, a prolonged time period between the death and the interview may have hindered the ability to recall information. Although our results have generalizability to the police sample from which they were randomly sampled, their generalizability to the population as a whole should be undertaken with caution. There may be biases between the types of deaths classified as suicide within police records versus deaths documented differently based on socio-political-economic factors that impact family’s disclosure preferences [12]. Finally, it is likely that stigmatized and sensitive factors, such as alcohol consumption and previous suicide attempts, are under-reported in our community sample. Additionally, suicides are underestimated as they are commonly misclassified or unreported [47, 71, 72]. Despite these limitations, the PA method remains a robust strategy to assemble a complex array of events and contexts that may have influenced suicidal behavior [73, 74].
Conclusion
Suicide remains a leading cause of death around the world, with urgent needs for prevention and intervention in LMIC. This study sheds new light on suicide in Nepal, pointing to potential important warning signs such as migrant labor, recent geographic movement, and family history of suicide. Findings demonstrate that male suicides are also a major public health issue, despite their neglect in public health and development discourse and literature in Nepal. Results reinforce the necessity for prevention programs to work with young people, especially to prevent suicide in rural areas and among girls. We suggest indicators that can be screened at both clinical and community-levels, and future research can explore its application and efficacy. Developing communication pathways by which persons with suicidal ideation can disclose to family, friends, or health workers will be indispensable to prevent suicide from being a silent public health crisis. Community-level interventions such as poison safes, policy to limit available pesticides and poisons, and decreasing stigma, while increasing awareness of warning signs for those with thoughts of suicide show great promise in Nepal, and other similar LMIC settings.
References
World Health Organization (2014) Preventing suicide: a global imperative. World Health Organization, Geneva, Switzerland
Bertolote JM, Fleischmann A, Butchart A, Besbelli N (2006) Suicide, suicide attempts and pesticides: a major hidden public health problem. Bull World Health Org 84:260
Phillips MR (2010) Rethinking the role of mental illness in suicide. Am J Psychiatry 167:731–733
Iemmi V, Bantjes J, Coast E, Channer K, Leone T, McDaid D et al (2016) Suicide and poverty in low-income and middle-income countries: a systematic review. Lancet Psychiatry 3(8):774–783
Knipe DW, Carroll R, Thomas KH, Pease A, Gunnell D, Metcalfe C (2015) Association of socio-economic position and suicide/attempted suicide in low and middle income countries in South and South-East Asia—a systematic review. BMC Public Health 15:1055
Hendin H, Phillips MR, Vijayakumar L, Pirkis J, Wang H, Yip P, Wasserman D, Bertolote JM, Fleischmann A (2008) Suicide and suicide prevention in Asia. Mental Health and Substance Abuse, World Health Organization, Geneva, Switzerland
Vijayakumar L, Pirkis J, Huong TT, Yip P, Seneviratne RDA, Hendin H (2008) Socio-economic, cultural and religious factors affecting suicide prevention in Asia. Suicide and Suicide Prevention in Asia. World Health Organization, Geneva, pp 19–30
Vijayakumar L, John S, Pirkis J, Whiteford H (2005) Suicide in developing countries (2): risk factors. Crisis 26(3):112–119
Bertolote JM, Fleischmann A, De Leo D, Bolhari J, Botega N, De Silva D et al (2005) Suicide attempts, plans, and ideation in culturally diverse sites: the WHO SUPRE-MISS community survey. Psychol Med 35(10):1457–1465
Kral MJ, Links PS, Bergmans Y (2012) Suicide studies and the need for mixed methods research. J Mixed Methods Res 6(3):236–249
Hjelmeland H, Knizek BL (2010) Why we need qualitative research in suicidology. Suicide Life Threat Behav 40(1):74–80
Hagaman AK, Maharjan U, Kohrt BA (2016) Suicide surveillance and health systems in Nepal: a qualitative and social network analysis. Int J Mental Health Syst 10:46
Institute for Health Metrics and Evaluation. GBD Compare Data Visualization. Retrieved from http://vizhub.healthdata.org/gbd-compare. Accessed 21 Dec 2016
Suvedi BK, Pradhan A, Barnett S, Puri M, Chitrakar SR, Poudel P et al (2009) Nepal maternal mortality and morbidity study 2008/2009: summary of preliminary findings. Kathmandu, Nepal: Family Health Division, Department of Health Services, Ministry of Health, Government of Nepal
Pradhan A, Poudel P, Thomas D, Barnett S (2011) A review of the evidence: suicide among women in Nepal. Kathmandu: National Health Sector Support Program, Ministry of Health and Population
Borges G, Nock MK, Abad JMH, Hwang I, Sampson NA, Alonso J et al (2010) Twelve month prevalence of and risk factors for suicide attempts in the WHO World Mental Health Surveys. J Clin Psychiatry 71(12):1617
Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A et al (2009) Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Med 6(8):e1000123
Fleischmann A, Bertolote JM, De Leo D, Botega N, Phillips M, Sisask M et al (2005) Characteristics of attempted suicides seen in emergency-care settings of general hospitals in eight low- and middle-income countries. Psychol Med 35(10):1467–1474
Kizza D, Hjelmeland H, Kinyanda E, Knizek BL (2012) Alcohol and suicide in postconflict Northern Uganda: A qualitative psychological autopsy study. Crisis 33(2):95–105
Hjelmeland H, Knizek BL (2016) Qualitative evidence in suicide: findings from qualitative psychological autopsy studies. In: Handbook of qualitative health research for evidence-based practice. Springer, New York, NY, pp 355–371
Shneidman ES (1994) The psychological autopsy. Am Psychol 49(1):75–76
Appleby L, Cooper J, Amos T, Faragher B (1999) Psychological autopsy study of suicides by people aged under 35. Br J Psychiatry 175(2):168–174
Phillips MR, Yang G, Zhang Y, Wang L, Ji H, Zhou M (2002) Risk factors for suicide in China: a national case-control psychological autopsy study. Lancet 360(9347):1728–1736
Hagaman AK, Sivilli TI, Ao T, Blanton C, Ellis H, Cardozo BL et al (2016) An investigation into suicides among bhutanese refugees resettled in the United States between 2008 and 2011. J Immigr Minor Health 18(4):819–827
Kohrt BA, Luitel NP, Acharya P, Jordans MJ (2016) Detection of depression in low resource settings: validation of the Patient Health Questionnaire (PHQ-9) and cultural concepts of distress in Nepal. BMC Psychiatry 16(1):58
CDC (2005) Web-based injury statistics query and reporting system (WISQARS) [online]. In: Control. NCfIPa, editor
Gunnell D, Eddleston M, Phillips MR, Konradsen F (2007) The global distribution of fatal pesticide self-poisoning: systematic review. BMC Public Health 7:357
Nepal Central Bureau of Statistics (2012) National population and housing census 2011. Kathmandu, Nepal: Government of Nepal, National Planning Commission Secretariat, Central Bureau of Statistics
Cameron MM (1998) On the edge of the auspicious: gender and caste in Nepal. University of Illinois Press, Illinois
Halliburton M (1998) Suicide: a paradox of development in Kerala. Economic and political weekly, pp 2341–2345
Chua JL (2014) In pursuit of the good life: aspiration and suicide in globalizing south India. University of California Press, California
Wagenaar B, Hagaman A, Kaiser B, McLean K, Kohrt B (2012) Depression, suicidal ideation, and associated factors: a cross-sectional study in rural Haiti. BMC Psychiatry 12(1):149
Eggerman M, Panter-Brick C (2010) Suffering, hope, and entrapment: resilience and cultural values in Afghanistan. Soc Sci Med 71(1):71–83
Munster DN (2015) Farmers’ suicides as public death: politics, agency and statistics in a suicide-prone district (South India). Mod Asian Stud 49(5):1580–1605
Bhise MC, Behere PB (2016) Risk factors for farmers’ suicides in central rural India: matched case–control psychological autopsy study. Indian J Psychol Med 38(6):560
Meltzer H, Bebbington P, Brugha T, Jenkins R, McManus S, Dennis M (2011) Personal debt and suicidal ideation. Psychol Med 41(04):771–778
Chavez-Hernandez AM, Macias-Garcia LF (2016) Understanding suicide in socially vulnerable contexts: psychological autopsy in a small town in Mexico. Suicide Life Threat Behav 46(1):3–12
Vijayakumar L (2016) Suicide prevention: beyond mental disorder. Indian J Psychol Med 38(6):514
Qin P, Agerbo E, Mortensen PB (2003) Suicide risk in relation to socioeconomic, demographic, psychiatric, and familial factors: a national register—based study of all suicides in Denmark, 1981–1997. Am J Psychiatry 160(4):765–772
Paudel GS (2007) Domestic violence against women in Nepal. Gender Technol Dev 11(2):199–233
Bradley F, Smith M, Long J, O’dowd T (2002) Reported frequency of domestic violence: cross sectional survey of women attending general practice. BMJ 324(7332):271
Tuladhar S, Khanal KR, Lila K, Ghimire PK, Onta K (2013) Womens empowerment and spousal violence in relation to health outcomes in Nepal: further analysis of the 2011 Nepal Demographic and Health Survey
Pun KD, Infanti JJ, Koju R, Schei B, Darj E, Group AS (2016) Community perceptions on domestic violence against pregnant women in Nepal: a qualitative study. Global Health Act 9(1):31964
Kohrt BA, Bourey C (2016) Culture and comorbidity: intimate partner violence as a common risk factor for maternal mental illness and reproductive health problems among former child soldiers in Nepal. Med Anthropol Q 30(4):515–535
Devries K, Watts C, Yoshihama M, Kiss L, Schraiber LB, Deyessa N et al (2011) Violence against women is strongly associated with suicide attempts: evidence from the WHO multi-country study on women’s health and domestic violence against women. Soc Sci Med 73(1):79–86
Mohanty S, Sahu G, Mohanty MK, Patnaik M (2007) Suicide in India—a four year retrospective study. J Forensic Leg Med 14(4):185–189
Patel V, Ramasundarahettige C, Vijayakumar L, Thakur JS, Gajalakshmi V, Gururaj G et al (2012) Suicide mortality in India: a nationally representative survey. Lancet 379(9834):2343–2351
Kolves K, Värnik A, Tooding L-M, Wasserman D (2006) The role of alcohol in suicide: a case-control psychological autopsy study. Psychol Med 36(07):923–930
Vijayakumar L, Kumar MS, Vijayakumar V (2011) Substance use and suicide. Curr Opin Psychiatry 24(3):197–202
Pompili M, Murri MB, Patti S, Innamorati M, Lester D, Girardi P et al (2016) The communication of suicidal intentions: a meta-analysis. Psychol Med 46(11):2239–2253
Chavan B, Singh GP, Kaur J, Kochar R (2008) Psychological autopsy of 101 suicide cases from northwest region of India. Indian J Psychiatry 50(1):34
Conner KR, Duberstein PR, Conwell Y, Caine ED (2003) Reactive aggression and suicide: theory and evidence. Aggress Violent Beh 8(4):413–432
Chachamovich E, Ding Y, Turecki G (2012) Levels of aggressiveness are higher among alcohol-related suicides: results from a psychological autopsy study. Alcohol 46(6):529–536
Rajappa K, Gallagher M, Miranda R (2012) Emotion dysregulation and vulnerability to suicidal ideation and attempts. Cognit Ther Res 36(6):833–839
Yang GH, Phillips MR, Zhou MG, Wang LJ, Zhang YP, Xu D (2005) Understanding the unique characteristics of suicide in China: national psychological autopsy study. Biomed Environ Sci 18(6):379–389
Ji J, Kleinman A, Becker AE (2001) Suicide in contemporary China: a review of China’s distinctive suicide demographics in their sociocultural context. Harv Rev Psychiatry 9(1):1–12
Thornicroft G, Chatterji S, Evans-Lacko S, Gruber M, Sampson N, Aguilar-Gaxiola S et al (2017) Undertreatment of people with major depressive disorder in 21 countries. Br J Psychiatry 210(2):119–124
Shidhaye R, Murhar V, Gangale S, Aldridge L, Shastri R, Parikh R et al (2017) The effect of VISHRAM, a grass-roots community-based mental health programme, on the treatment gap for depression in rural communities in India: a population-based study. Lancet Psychiatry 4(2):128–135
Kohrt BA, Speckman RA, Kunz RD, Baldwin JL, Upadhaya N, Acharya NR et al (2009) Culture in psychiatric epidemiology: using ethnography and multiple mediator models to assess the relationship of caste with depression and anxiety in Nepal. Ann Hum Biol 36(3):261–280
Kohrt BA, Worthman CM (2009) Gender and anxiety in Nepal: the role of social support, stressful life events, and structural violence. CNS Neurosci Ther 15(3):237–248
Milner A, Hjelmeland H, Arensman E, De Leo D (2013) Social-environmental factors and suicide mortality: a narrative review of over 200 articles. Sociol Mind 3(2):137
Fleischmann A, Arensman E, Berman A, Carli V, De Leo D, Hadlaczky G et al. (2016) Overview evidence on interventions for population suicide with an eye to identifying best-supported strategies for LMICs. Glob Ment Health 3:e5
Zalsman G, Hawton K, Wasserman D, van Heeringen K, Arensman E, Sarchiapone M et al (2016) Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry 3(7):646–659
Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A et al (2005) Suicide prevention strategies—a systematic review. JAMA J Am Med Assoc 294(16):2064–2074
Kohrt BA, Blasingame E, Compton MT, Dakana SF, Dossen B, Lang F et al (2015) Adapting the crisis intervention team (CIT) Model of police–mental health collaboration in a low-income, post-conflict country: curriculum development in liberia, West Africa. Am J Public Health 105(3):e73–e80
Lund C, Tomlinson M, Patel V (2016) Integration of mental health into primary care in low-and middle-income countries: the PRIME mental healthcare plans. Br J Psychiatry 208(Suppl 56):s1–s3
Vijayakumar L, Jeyaseelan L, Kumar S, Mohanraj R, Devika S, Manikandan S (2013) A central storage facility to reduce pesticide suicides—a feasibility study from India. BMC Public Health 13(1):850
Gunnell D, Fernando R, Hewagama M, Priyangika W, Konradsen F, Eddleston M (2007) The impact of pesticide regulations on suicide in Sri Lanka. Int J Epidemiol 36(6):1235–1242
Jordans MRS, Fekadu A, Medhin G, Kigozi F, Kohrt BA, Luitel N, Petersen I, Shidhaye R, Ssebunnya J, Patel V, Lund C (2017) Suicidal ideation and behaviour among community and health care seeking populations in five low and middle-income countries: a cross-sectional study. Epidemiol Psychiatri Sci. doi:10.1017/S2045796017000038
Pouliot L, De Leo D (2006) Critical issues in psychological autopsy studies. Suicide Life Threat Behav 36(5):491–510
Phillips DP, Ruth TE (1993) Adequacy of official suicide statistics for scientific-research and public-policy. Suicide Life Threat Behav 23(4):307–319
Rockett I, Kapusta ND, Bhandari R (2011) Suicide misclassification in an international context: revisitation and update. Suicidol Online 2:48–61
Conner KR, Beautrais AL, Brent DA, Conwell Y, Phillips MR, Schneider B (2012) The next generation of psychological autopsy studies. Suicide Life Threat Behav 42(1):86–103
Cavanagh JT, Carson AJ, Sharpe M, Lawrie S (2003) Psychological autopsy studies of suicide: a systematic review. Psychol Med 33(3):395–405
Acknowledgements
The authors are deeply grateful for the valuable support and mentorship of Transcultural Psychosocial Organization (TPO) Nepal, particularly Mr. Nandaraj Acharya, Mr. Safar Bikram Adhikari, Mr. Nagendra Luitel, and Mr. Suraj Koirala. We are also gracious for the assistance of Jumla District and Kathmandu District police officers as well as Action Works Nepal staff and community leaders.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial support
AH was supported by US Fulbright Student Research Program and the National Science Foundation Cultural Anthropology Doctoral Dissertation Research Improvement Grant (Award 1459811). BAK was supported by the U.S. National Institute of Mental Health (K01MH104310).
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Availability of data and materials
Quantitative data resulting from the psychological autopsies and qualitative coding queries and code book information may be requested from the first author. Institutional suicide surveillance and reporting data are not available from the authors. For this information, researchers are encouraged to directly contact law enforcement and health institutions in Nepal.
Rights and permissions
About this article
Cite this article
Hagaman, A.K., Khadka, S., Lohani, S. et al. Suicide in Nepal: a modified psychological autopsy investigation from randomly selected police cases between 2013 and 2015. Soc Psychiatry Psychiatr Epidemiol 52, 1483–1494 (2017). https://doi.org/10.1007/s00127-017-1433-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-017-1433-6