Abstract
Purpose
Macau is a Special Administrative Region in China that has experienced tremendous development in its gambling industry during its post-colonial years. To inform mental health planning, this study presents the first population estimates and correlates of the current depression in Macau.
Methods
A population-representative sample of 1068 Macau Chinese citizens aged 18 or above responded to a household telephone survey in January, 2015. The Patient Health Questionnaire-9 measured the current depression. Logistic regression models assessed the association between depression and potential correlates.
Results
Overall, 8.0% (95% CI 6.3–9.7) of persons reported the current depression. A higher but non-significant proportion of women reported depression than men (9.3 vs. 6.6%) and older women reported higher prevalence (13.4%) than other demographic groups. Persons who were unemployed (OR = 4.9, 2.3–10.5), separated or divorced (OR = 3.1, 1.1–8.9), and reported poor self-rated health (OR = 5.0, 2.8–9.0), low quality of life (OR = 6.2, 3.1–12.7), lower social standing (OR = 2.4, 1.4–4.0), lower community trust (OR = 1.9, 1.2–3.1), lower perceived fairness (OR = 2.3, 1.4–3.8), lower social cohesion (OR = 3.8, 2.3–6.2), and lower social integration (OR = 3.0, 1.9–5.0) had greater odds of depression than their comparison group.
Conclusions
The current study demonstrated the burden of depression among Macau adults disproportionately affects women during emerging adolescence and old age, and men during middle adulthood. Key strategies to improve mental health services in Macau are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Major depression is the most prevalent disorder worldwide. Findings from the World Health Organization (WHO) World Mental Health Surveys showed that 12-month prevalence of depression in ten high-income countries and eight low- and middle-income countries [1] was 5.5 and 5.9%, respectively. In the United States, 8.7% of the population were estimated to have the current depression in 2006 [2]. Depression is also a major source of disability globally. The Global Burden of Disease Study 2015 showed that depression is the third leading cause of years lived with disability (YLDs), and has been increasing since 1990 [3]. Identifying country and regional population patterning of depression is a key step in formulating a comprehensive mental health action plan and can inform data-driven policy decisions regarding efficient and fair distribution of scarce mental health resources.
China accounts for the largest population in the world and issues related to mental health surveillance, treatment, stigma, and the development of scalable solutions to mental health problems persist [4]. Regional differences in a country as geographically vast as China presents challenges for calculating generalizable and accurate estimates of country-level prevalence and burden of psychiatric disorders. Therefore, regional studies are needed.
Few previous epidemiological studies have estimated the burden of depression in China. The WHO Composite International Diagnostic Interview (CIDI) was administered to more than 5000 community-dwelling adults (aged 18–80) in Beijing and Shanghai, large cities in the north and northeast of China. The 12-month prevalence of DSM-IV depression was reported to be 1.8% [5] and no significant sex differences in prevalence were reported. A second study, more comprehensive in scope, covered four provinces in China and integrated both urban and rural areas into the methodological design [6]. The study included more than 63,000 people and employed face-to-face methods and lay health workers to assess various psychiatric conditions. The 1-month prevalence of depression was 6%. Differences between these prevalence estimates may be due to the absence of rural participants from the Lee and colleagues [5] sample, as people in rural areas were more likely [adjusted rural: urban prevalence ratio = 1.44 (1.12–1.84)] to have depression [6]. A more recent population-representative spatial epidemiological study conducted in Guangzhou, a major city in China, reported a 5.1% 2-week prevalence of depression [7]. This study focused on regions in Guangzhou that were home to a larger proportion of migrants, largely from rural areas. This figure was closer to the Phillips’ and colleagues’ study [6]. A review of epidemiological studies in mainland China showed the pooled prevalence of the current depression was 1.6, 2.1% among women, and 1.3% among men (Gu et al. 2013).
Similarly, Macau is similar to as both are Special Administrative Regions in China and Cantonese is the most widely spoken dialect language in both regions. Several studies have documented the prevalence of psychiatric conditions in Hong Kong. The Hong Kong Mental Morbidity Survey examined common mental disorders (anxiety and depression) among 5719 Chinese adults using face-to-face interviews [8]. The estimated prevalence of any mental disorder was 13.3%. Estimates of the current depression (past week) were 2.9% and women had a higher prevalence than men (3.5 vs. 2.2%). Another population survey including over 5000 adults conducted via telephone estimated the prevalence of depression was 8.4% in the past 12 months [9]. A more recent population-representative study of over 1000 people, conducted one-month following the pro-democracy umbrella protests, found a higher prevalence of depression. The study reported 14.4% current depression prevalence using a cut-score ≥10 on the Patient Health Questionnaire-9 (PHQ-9) [10, 11]. The authors attributed this higher prevalence to recent social and economic turmoil caused by the umbrella movement.
In the _ENREF_9, first two Hong Kong studies mentioned earlier [8, 9], and older adults had the highest prevalence of depression of all age groups. This was also supported in studies specifically designed to evaluate older adults. For example, Chi et al. [12] face-to-face surveyed over 900 older adults (aged 60 and over) with the Geriatric Depression Scale and found that 12.5% were depressed.
In addition to age and sex differences in depression, other significant correlates were identified in the previous population studies in China. The estimated prevalence for depression was higher among those unemployed [2, 9] and those with lower economic resources in several studies [5, 13,14,15]. Migrant populations have higher levels of lifetime depression [15] than non-migrants, but comparative depression point prevalence is not known. In China, marriage is a critical determinant of status, and therefore, studies have shown that being single or divorced was associated with greater depression [2, 5]. Lower educational level was associated with greater depression [13, 15]. Subjective health status is a robust correlate of depression [15, 16].
Relative social status is a robust predictor of depression across many studies [17, 18]. One study in Hong Kong found higher standing on self-reported socioeconomic ladder associated with lower depression [19], but this has yet to be applied in Macau or in Mainland China. Overall quality of life is associated with depression [20], but this has not been tested in Chinese samples. Lower levels of cognitive social capital, or the belief in the trust and community norms of reciprocity, is associated with greater depression [21], and has thus far only been applied to older adults in Macau [22] and China [7, 23], but not in the general adult population. Social capital is a critical community-level risk factor given the interconnected and collective features of Chinese society [24].
The current study
To date, no study has attempted to estimate the prevalence of depression in Macau, China. Although Macau shares the same language to Hong Kong and Guangdong Province, there are key differences to suggest that a separate psychiatric epidemiologic program is needed in Macau. First, even Macau and Hong Kong share the history of colonialism, and they were governed by Portugal and the United Kingdom, respectively. Second, Macau is the only region in China, where gambling is legal. In the past 10 years, it has undergone rapid economic development with a singular focus on the casino and hospitality industry, which helped its transformation from a small fishing town to the largest gaming center in Asia. Third, it is also the most densely populated region in the world, even more so than Hong Kong. Each of these unique features may have profound influences on shaping population mental health.
The only previous population-representative study of 1881 older adults of age 60 and above, estimated the depression prevalence was 10.4% [25]. In another study of 380 urban dwelling older adults living in public housing, the estimated prevalence of depression was 15.0% [22]. Overall, we know little about the level of depression and the general mental health of the Macau population, which limits public health planning and action towards establishing appropriate care models for mental health. The aim of this study was to estimate the population prevalence of the current depression and correlates of depression among the adult Chinese population.
Methods
Telephone surveys and respondent recruitment were carried out in January 2015 using Computer-Assisted Telephone Interview (CATI) system. Interviewers were local research assistants who possessed at least a bachelor’s degree and were trained in research ethics and how to ask questions related to depression. The database of telephone numbers was generated by the latest local phone number catalog. The target sample was Macau citizens aged 18 or above that can speak Cantonese, the local dialect. This population included the majority Chinese population in Macau that consists of local born Chinese and newer migrants, mostly from the nearby province of Guangdong in Mainland China. All calls were made during 6:00 PM to 10:00 PM during weekdays and from 2:00 PM to 10:00 PM during weekends. After successful contact with a random household, trained interviewers first confirmed if any members met eligibility (over 18 years, Chinese, spoke Cantonese), then performed random sampling by inviting an eligible respondent with the closest birthday to the interview date. If the respondent with the closest birthday to the interview date was not at home, the interviewer would schedule a call at the respondent’s convenience, or would call the household again up to eight times until the person was reached, or counted as a non-response. Oral informed consent was obtained at the beginning of the interview and confidentiality was assured. No financial incentive was offered for study participation. This study was approved by the research ethics review panel of the Macau (SAR) government.
The sampling error was ±3.00% at 95% confidence level. A total of 7738 phone numbers were attempted, 2272 (29.0%) numbers were confirmed ineligible (e.g., not in use), and eligibility of 971 numbers (13%) was unknown. Among the 3427 (44.3%) eligible numbers, 1068 (31.1%) were successful and completed; 740 (21.6%) refused to participate, either at the household-level or by individual eligible respondents. Response rate and cooperation rates were 40.4 and 57.9%, respectively (Rate 3, American Association for Public Opinion Research) [26]. Average time of completion was 13.95 min.
Measures
Depression
The Chinese version of the nine-item Patient Health Questionnaire (PHQ-9) [27] assessed depressive symptom severity during the past two weeks on a four-point scale with 0 ‘not at all’ 1 on ‘several days,’ 2 ‘on more than half of the days,’ and 3 ‘nearly all of the days.’ The scale is summed with higher scores indicating greater depression severity. The previous studies with Chinese samples found excellent scale reliabilities (>0.80) [10, 27, 28]. A score of 10 or greater was used to indicate depression within the sample. This method is consistent with the previous population studies in Chinese populations [11, 28]. The alpha for the scale was 0.84.
Social status
Relative social standing was assessed with one item that inquired ‘Which of the following social classes do you think you belong to.’ Responses ranged from 1 ‘lower class’ to 5 ‘upper class.’ We dichotomized this variable as middle/upper middle/upper class = 0 and lower class/low class = 1. This item was dichotomised as middle/upper middle/upper class = 0 and lower class/low class = 1 to reflect high and low self-reported social status.
Quality of life
One item asked participants to rate their quality of life on a scale between 1 ‘bad to 5 ‘excellent.’ This item was dichotomised as good/very good/excellent = 0 and bad/poor = 1 to reflect high and low self-reported quality of life.
Cognitive social capital
Cognitive social capital was measured with four items that address its common domains [29]. Perceived trust was measured by asking ‘overall, most people in my community can be trusted,’ and perceived fairness ‘do you think the majority of people in your community would take advantage of you if given the chance.’ Social cohesion was measured by asking ‘most people in my community get along well,’ and social integration was measured by asking ‘You feel a part of your community.’ Response options were yes, no, and not sure for each item. Not sure responses were coded as no.
Self-rated health
Health status was assessed using a common single item measurement ranging from 1 ‘very good’ to 4 ‘very poor.’ This item was dichotomised as good/very good/excellent = 0 and bad/poor = 1 to reflect good and poor self-reported health. Brief health status measures are found to be valid predictors of mortality [30].
Participant characteristics
These were obtained for sex, age, marital status, employment, education, marital status, family income, and migration status.
Analysis
Data were weighted to account for non-response bias utilizing the latest census data on gender, age, and population size (total population 379, 932, and 55.14% female) [31]. A total of 51 participants were missing one or more items on the PHQ-9. Multiple imputations with chained equations were used to create ten data sets and estimates were pooled to account for missing data. Total and age and sex stratified depression prevalence was estimated with 95% confidence intervals. Prevalence estimates were then used to estimate the total and age and sex stratified number of potential cases requiring treatment, along with 95% confidence intervals.
Logistic regression models were used to estimate the association between depression and correlates found to be associated with depression in the previous studies. Our analysis included individual characteristics (i.e., sex, age, income, education, marital status, and migration status), individually reported health status, relative social status, and individual perceptions of community social capital. All analyses were conducted utilizing the Taylor linearised approach with STATA MP 12.1 [32].
Results
The weighted sample demographic characteristics are shown in Table 1. The final study population age ranged between 18 and 98 (M = 43.22; SE 0.49). The majority were between age 45 and 54 (23.2%). Slightly over half were females (52.8%). Over one-third (36.37) had junior school education or below. 38.43% reported family income lower than 30,000 MOP per month and over half (52.38%) were not born locally. Fair or poor health was reported by 46.1%. 52.0% reported low relative social class, and 55.8% reported low quality of life. A total of 35.8% reported low trust, 20.4% reported low perceived fairness, 21.8% reported low integration, and 16.8% reported low social cohesion. The mean depressive symptom severity in the population was 3.54 (SD = 4.70).
The overall population estimate of depression was 8.0% (95% CI 6.3–9.7), 9.3% (95% CI 6.9–11.7) for women, and 6.6% (95% CI 4.1–9.0) for men. Applying these estimates to the total population size, an estimated 23,556 to 36,625 Macau Chinese adults are likely to meet criteria for the current major depression. The distribution of depression shows that a larger proportion of women are depressed across the lifespan compared to men, except between the ages of 35–44. The highest estimated prevalence for depression in this sample was for older women aged 65 and above (13.4%, 95% CI 6.2–20.6). Complete sex- and age-stratified prevalence estimates are displayed in Table 2.
Correlates of depression are reported in Table 3. Significant bivariate associations were noted between depression and employment. Individuals who were unemployed [OR = 4.9 (2.3–10.5), p < 0.001], retired [OR = 2.3 (1.3–4.0), p = 0.005], or were housewives [OR = 2.1 (1.0–4.3), p = 0.043], all had higher odds of being depressed compared to people who were employed. Compared to people who were married, those who were separated or divorced [OR = 3.1 (1.1–8.9), p = 0.036] had higher odds of being depressed. Those whose family income was lower than 30,000 MOP per month had higher odds of being depressed [OR = 1.9 (1.2–3.0), p = 0.009] than those with higher than 30,000 MOP per month. Individuals who reported to have poor self-rated health status [OR = 5.0 (2.8–9.0), p < 0.001], low social status [OR = 2.4 (1.4–4.0), p = 0.001], low quality of life [OR = 6.3 (3.1–12.7), p < 0.001], and low cognitive social capital: general trust [OR = 1.9 (1.2–3.1), p = 0.009], social cohesion [OR = 3.8 (2.3–6.2), p < 0.001], and social integration [OR = 3.0 (1.9–5.0), p < 0.001], all had higher odds of being depressed compared to those who reported good self-rated health, high social status, high quality of life, and high cognitive social capital, respectively.
Discussion
In our current study of a representative sample of 1068 Macau Chinese adults, the estimated population prevalence of the current major depression was 8.0%. This finding is striking as it suggests that the depression prevalence in Macau is higher than in Mainland China and in Hong Kong regardless of whether the study utilized face-to-face methods [6, 7], or telephone methods [9]. For example, S. Lee and colleagues [9] reported that the 12-month prevalence of depression was 8.4% in Hong Kong, while we estimated the current major depression in our current study. It is notable that telephone assessments in the current study and the Lee et al.’s study [9] were higher than estimates obtained using face-to-face methods in the previous studies. Telephone surveys may provide participants an anonymous and potentially less stigma evoking mechanism to disclose sensitive information [33].
The overall prevalence of depression was higher among women compared to men (9.3 vs. 6.6%). This finding compares well with past research in China, which showed in each study that women had a higher prevalence of depression than men [8, 9]. In the present study, depression remained relatively stable from early to middle adulthood for women but began to increase at age 45–54. Age specific comparisons showed that during middle adulthood, the prevalence of depression for men was higher than for women (10.0 vs. 7.35%), and during this period, depression prevalence nearly doubled for men. Future research is needed to explore possible reasons for these ages and sex trends.
Older adults had a higher prevalence of depression compared to younger and middle aged adults. This finding is consistent with the previous studies conducted in Mainland China and in Hong Kong [2, 6, 8, 13, 14, 34]. In general, the depression prevalence increased for men and women in Macau by age, peaking in older adults over age 65. Macau people have one of the longest life expectancies in the world, and an emphasis on positive aging and maintaining a good quality of life among older adults should be a public health priority. Functional decline and impaired health status is associated with decreased life satisfaction [35], and depressed older adults are at twice the risk to die from suicide than non-depressed older adults [36]. The current study extends the findings of the previous population study of older adults in Macau [22] utilizing a population-representative sampling method that enabled comparisons of depression prevalence across the lifespan.
Key socioeconomic risk factors were associated with depression in our sample. Being unemployed, a housewife or retired all were consistent with Lee and Tsang’s study [9] in Hong Kong, where those factors were also identified. Lower self-rated social class was a significant correlate, and is consistent with a Hong Kong older adult sample [19]. Poor quality of life was a significant correlate of depression.
A growing literature points to social capital as a key correlate of depression among Chinese populations [7, 22, 23]. In the current study, lower perceived trust, lower perceived fairness, lower cohesion, and lower integration all were associated with increased odds of being depressed. It is uncertain if social capital eroded in the past 10 years, a period of rapid economic development, or if this is a stable feature of local society. However, other scholars have noted that older adults have especially become vulnerable to depression due to rapid social change in China [37].
Epidemiologic investigations of common mental disorders among Chinese populations in the greater China region are crucial. The absence of this data, mental health stigma, poor mental health infrastructure, and poor treatment seeking present significant barriers to mental health provision [4]. The current study presents the first epidemiological investigation of the prevalence and correlates of depression in Macau (SAR), China, part of a larger initiative to contextualise the mental health needs across the Pearl River Delta in Southern China [7, 10, 22, 38]. The representative sample and focus on individual and perceived community-level correlates that may influence depression were strengths. However, the present study also has several limitations.
First, the survey was based on self-reported data via telephone survey. The global tread that landline phone use is declining is also occurring in Macau. According to the Macau Census Data [31], there are 170,769 households in Macau. Of the 152,618 landline phones in Macau, 94,630 were classified as household landlines when the survey was conducted [39]. It is possible that some Macau people who would otherwise be eligible for the study would not participate if they did not have a landline phone. However, according to a study released by the PEW research center, the growing cell-only population is not undermining National Survey results [40].
We believe that telephone methods were appropriate in this study context given significant mental health stigma among Chinese that interferes with reporting emotional and psychiatric issues. The previous studies showed that minimal bias is expected with telephone survey [41, 42] and general acceptability of this method [43, 44].
Another limitation is the diagnosis which is based on screening but not clinical diagnostic interviews. Therefore, the current depression prevalence estimates may include depressive episodes related to bipolar disorder, and we could not evaluate comorbid mood disorders or other psychiatric conditions. Future epidemiological investigations are needed to fully assess psychiatric conditions in Macau using screening and diagnostic interview methods.
There may be important correlates of depression that were unmeasured in the present study. Future qualitative work is needed to identify additional context-specific risk factors. Although we estimated population prevalence based on census information, nonparticipation bias may have influenced our results. The relatively low prevalence of depression in certain age strata produced wide confidence intervals and future investigations will require larger sample sizes to produce more stable sub-population estimates. The present study does not consider local signs and symptoms of distress not codified in the Western nomenclature. In addition to exploring western psychiatric conditions, future research is needed to contextualise specific signs and symptoms of mental illness that are locally important among Chinese populations [45]. These studies should additionally focus on lay concepts and explanatory beliefs about mental illness to develop a more complete understanding of mental disorders and inform the development of culturally informed interventions. Finally, the cross-sectional nature of this work limits our ability to infer causal associations between depression and correlates we measured.
Towards a plan for mental health action
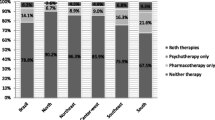
Depression is a common mental disorder that is among the leading causes of disability worldwide. In Macau, depression is a prevalent condition, primarily affecting people aged 35 and older. Women and older adults of either sex appear to be most affected by depression. Prevention and intervention programming tailored for women, men in emerging adulthood, and older adults is warranted. Barriers to address these treatment goals involve few service providers, a focus on inpatient versus outpatient community-based care, and lack of research into mental disorders and their treatment in Macau.
A mental health workforce should be recruited or trained that can adequately treat common mental disorders utilizing evidence-based methods. According to the Macau Government’s registration figures, there are 21 registered Psychotherapists in Macau [46], but the current professional accreditation law does not specify the qualification requirement for psychotherapists. Although some had a MA course in clinical psychology, most registered psychotherapists received only a bachelor degree. So far as we are aware, in Macau, there are only four doctoral-level clinical psychologists, but only one among them can conduct treatment in the Chinese language. There are currently no specialist programs for postgraduate training in clinical psychology, so it is unlikely that Macau can train an adequate workforce and other models should be considered.
Working with NGOs and the existing social work workforce to enhance skills and build capacity to provide mental health care is promising. New scalable packages of care are being developed and tested that can be implemented by community members and lay health workers without specialist mental health training in resource constrained settings [47]. Social workers who already provide mental health services could be trained to implement and eventually supervise time-limited evidence-based treatments such as these.
Mental healthcare should shift to community-based outpatient centers. This could increase access to care and lesson stigma associated with seeking psychiatric care. At present, there are two local hospitals in Macau that provide inpatient hospitalization for patients with severe mental illness, but no outpatient care facilities. This leads to medication and hospitalization as frontline treatments rather than preventative or psychosocial interventions. Developing services that can complement and extend the existing system is needed, and enhanced coordination between various stakeholders in the government, NGOs, public hospitals, academics, and mental health consumers, would provide leadership in setting a mental health agenda and ensuring the provision of meaningful services.
Research into culturally specific illness beliefs and potentially appropriate culturally informed treatments are needed. Macau is a traditional Chinese society and it is unclear to what extent Western concepts of illness or individual models of psychotherapy are acceptable. The level of mental health literacy as it relates to Western psychiatric conditions like depression is low among the general public and among elders in particular. Systematic surveillance of common mental disorders, culturally relevant illness concepts, and service utilization will identify treatment gaps and inform priorities for health system strengthening.
References
Bromet E et al (2011) Cross-national epidemiology of DSM-IV major depressive episode. BMC Med 9:90
Strine TW et al (2008) Depression and anxiety in the United States: findings from the 2006 behavioral risk factor surveillance system. Psychiatr Serv 59(12):1383–1390
GBD 2015 Disease and Injury Incidence and Prevalence Collaborators (2016) Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet 388(10053):1545–1602
Patel V. et al. (2016) The magnitude of and health system responses to the mental health treatment gap in adults in India and China. The Lancet
Lee S et al (2009) The epidemiology of depression in metropolitan China. Psychol Med 39(5):735–747
Phillips MR et al (2009) Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001–05: an epidemiological survey. Lancet 373(9680):2041–2053
Hoi CK et al (2015) The association between social resources and depressive symptoms among Chinese migrants and non-migrants living in Guangzhou, China. J Pacific Rim Psychol 9:120–129
Lam LC-W et al (2015) Prevalence, psychosocial correlates and service utilization of depressive and anxiety disorders in Hong Kong: the Hong Kong Mental Morbidity Survey (HKMMS). Soc Psychiatry Psychiatr Epidemiol 50(9):1379–1388
Lee S, Tsang A, Kwok K (2007) Twelve-month prevalence, correlates, and treatment preference of adults with DSM-IV major depressive episode in Hong Kong. J Affect Disord 98(1–2):129–136
Hou WK et al (2015) Threat to democracy: physical and mental health impact of democracy movement in Hong Kong. J Affect Disord 186:74–82
Lau KM et al (2016) Social media and mental health in democracy movement in Hong Kong: a population-based study. Comput Hum Behav 64:656–662
Chi I et al (2005) Prevalence of depression and its correlates in Hong Kong’s Chinese older adults. Am J Geriatric Psychiatry Off J Am Assoc Geriatric Psychiatry 13(5):409–416
Zhou X et al (2014) The prevalence and risk factors for depression symptoms in a rural Chinese sample population. PLoS ONE 9(6):e99692
Liu J et al (2015) Prevalence of major depressive disorder and socio-demographic correlates: results of a representative household epidemiological survey in Beijing, China. J Affect Disord 179:74–81
Zhong B-L et al (2015) Prevalence and correlates of major depressive disorder among rural-to-urban migrant workers in Shenzhen, China. J Affect Disord 183:1–9
Pan A et al (2008) Prevalence and geographic disparity of depressive symptoms among middle-aged and elderly in China. J Affect Disord 105(1):167–175
Operario D, Adler NE, Williams DR (2004) Subjective social status: reliability and predictive utility for global health. Psychol Health 19(2):237–246
Hu P et al (2005) Relationship between subjective social status and measures of health in older Taiwanese persons. J Am Geriatr Soc 53(3):483–488
Wong SY et al (2008) The influence of multi-morbidity and self-reported socio-economic standing on the prevalence of depression in an elderly Hong Kong population. BMC Publ Health 8:119
Papakostas GI et al (2004) Quality of life assessments in major depressive disorder: a review of the literature. Gen Hosp Psychiatry 26(1):13–17
De Silva MJ et al (2005) Social capital and mental illness: a systematic review. J Epidemiol Community Health 59(8):619–627
Wu TL et al (2016) The association between social capital and depression among Chinese older adults living in public housing. J Nerv Ment Dis 204(10):764–769
Cao W et al (2015) Social capital and depression: evidence from urban elderly in China. Aging Mental Health 19(5):418–429
Yang LH, Kleinman A (2008) ‘Face’ and the embodiment of stigma in China: the cases of schizophrenia and AIDS. Soc Sci Med 67(3):398–408
Zeng W, Chan MF (2010) Investigating factors related to depression among older persons in Macau. Macau Journal of Nursing 9(1)
The American Association for Public Opinion Research, Standard definitions: final dispositions of case codes and outcome rates for surveys. 2016, AAPOR
Yeung A et al (2008) Validation of the Patient Health Questionnaire-9 for depression screening among Chinese Americans. Compr Psychiatry 49(2):211–217
Nan H et al (2013) Effects of depressive symptoms and family satisfaction on health related quality of life: the Hong Kong family study. PLoS ONE 8(3):e58436
Kawachi I et al (1997) Social capital, income inequality, and mortality. Am J Publ Health 87(9):1491–1498
DeSalvo KB et al (2005) Predicting mortality and healthcare utilization with a single question. Health Serv Res 40(4):1234–1246
Direcção dos Serviços de Estatística e Censos, Results of 2011 population census. 2011
StataCorp, Stata Statistical Software: release 12. 2011, StataCorp LP: College Station, TX
Lee S et al (2006) Stigmatizing experience and structural discrimination associated with the treatment of schizophrenia in Hong Kong. Soc Sci Med 62(7):1685–1696
Gu L et al (2013) Epidemiology of major depressive disorder in mainland china: a systematic review. PLoS ONE 8(6):e65356
Hu SX et al (2016) Common chronic health problems and life satisfaction among Macau elderly people. Int J Nurs Sci 3(4):367–370
Sun WJ et al (2012) Depressive symptoms and suicide in 56,000 older Chinese: a Hong Kong cohort study. Soc Psychiatry Psychiatr Epidemiol 47(4):505–514
Shao J et al (2013) Birth cohort changes in the depressive symptoms of Chinese older adults: a cross-temporal meta-analysis. Int J Geriatr Psychiatry 28(11):1101–1108
Hall BJ, Sou K, Chen W, Zhou F, Chang K, Latkin C (2016) An evaluation of the buffering effects of types and sources of support on depressive symptoms among natural disaster–exposed chinese adults. Psychiatry Interpers Biol Process 79:389–402
Direcção dos Serviços de Correios e Telecomunicações. Major Telecommunication Service Statistics. 2015; Available from: http://telecommunications.ctt.gov.mo/web/en/generalinfo/statistics/mainstat/mainstat2015a
Pew Research Center for the People and the Press (2006) The Cell Phone Challenge to Survey Research: National Polls Not Undermined by Growing Cell-Only Population
Hobfoll SE et al (2011) Are community studies of psychological trauma’s impact accurate? A study among Jews and Palestinians. Psychol Assess 23(3):599
Muskens EM et al (2014) Psychiatric diagnosis by telephone: is it an opportunity? Soc Psychiatry Psychiatr Epidemiol 49(10):1677–1689
Allen K, Cull A, Sharpe M (2003) Diagnosing major depression in medical outpatients: acceptability of telephone interviews. J Psychosom Res 55(4):385–387
Pridemore WA, Damphousse KR, Moore RK (2005) Obtaining sensitive information from a wary population: a comparison of telephone and face-to-face surveys of welfare recipients in the United States. Soc Sci Med 61(5):976–984
Hall BJ, Chang K, Chen W, Sou K, Latkin C, Yeung A (2017) Exploring the association between depression and shenjing shuairuo in a population representative epidemiological study of Chinese adults in Guangzhou, China
Serviços de Saúde. Current registration status of medical professionals. 2014; Available from: http://www.gaes.gov.mo/counseling/images/activityinfo/2014/act2014-6/20140920.pdf. Accessed 10 Jan 2016
Dawson KS et al (2015) Problem Management Plus (PM+): a WHO transdiagnostic psychological intervention for common mental health problems. World Psychiatry 14(3):354–357
Acknowledgements
We thank Juliana Yuncg, Elenna Mo, Ray Wong, Emily Iong, Ung Hou Pang, Angela Ma and Jazz Cheong for their assistance with data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial support
This work was supported by the Research and Development Affairs Office (R&DAO), University of Macau, under Grant MYRG2015-00124-FSS and MYRG2015-00109-FSS (PI: Hall). The funding source played no role in the conduct of this research.
Conflict of interest
The authors declare that there is no competing interest.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Rights and permissions
About this article
Cite this article
Hall, B.J., Lam, A.I.F., Wu, T.L. et al. The epidemiology of current depression in Macau, China: towards a plan for mental health action. Soc Psychiatry Psychiatr Epidemiol 52, 1227–1235 (2017). https://doi.org/10.1007/s00127-017-1415-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-017-1415-8