Abstract
Objective
Most patients with first episode psychosis (FEP) are neither studying nor employed (have a poor functional status) when first accessing care. Knowledge of the characteristics of patients with poor functioning and the features influencing functional status over time may pave the way to better treatment.
Method
A medical file audit was used to collect data on premorbid, entry, treatment and 18-month outcome characteristics on 661 FEP patients who consecutively attended the Early Psychosis Prevention and Intervention Centre, Melbourne, Australia, between 1998 and 2000. Functional status was ascertained using the modified vocational status index and was rated at baseline (poor or good) and according to its evolution over the treatment period (stable good, stable poor, deteriorating or improved functional status).
Results
52.0% of patients had a poor functional status at service entry. They were more likely to be male with a non-affective psychosis. They also had lower levels of premorbid global functioning and education, and were more likely to have self-reported histories of learning disability, forensic issues, traumatic experiences and substance use. At service entry, they had more severe symptoms and poorer global functioning. 37% of these patients maintained a poor functional status at discharge, and 18% of those with a good functional status at service entry experienced a decline.
Conclusions
Although psychosocial interventions might assist a young person with FEP with working towards functional goals, for some, the impact of factors such as ongoing substance use and forensic issues on functional status needs to be addressed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unemployment and/or disruption to educational goals is prevalent and debilitating issues affecting young people with first episode psychosis (FEP) [1, 2]. Young people with psychosis are more likely to have disrupted and less education than their peers, which can impede future employment opportunities [3]. Rates of unemployment among FEP groups range from 13 to 55% [1], with rates increasing to 75–95% within the first couple of years after diagnosis [4]. This poor functioning and lack of educational and employment attainment may result in a downward spiral towards poverty and social isolation [5].
In order to effectively target and improve psychosocial interventions, it is important to first understand the characteristics of FEP patients who are either unemployed or not studying (have a poor functional status) at service entry. Only a few such studies have been conducted with FEP and most have focused on employment. Those unemployed when they first present for treatment for psychosis lack educational attainment [5–8] have poorer premorbid adjustment [9], more severe symptomatology [9–11], longer duration of untreated psychosis (DUP, [8, 9]), dependence on disability benefits [5], poorer cognitive functioning [10, 12], substance use [12] and lower quality of life (QoL, [9]). FEP patients who are students and/or employed have lower levels of depressive symptoms and higher global and social functioning [13]. Previous studies, however, have been based on small unrepresentative samples with sample sizes confined to under 200 participants (e.g. [9, 11, 13, 14]), with predominant features including non-affective (e.g. [7]) or inpatient samples (e.g. [11]).
Recent reports have confirmed the importance of combining early intervention programs with vocational and psychosocial support [1, 2]. Findings suggest that clinical services alone produce less favourable functional outcomes in their patients [2, 15]. However, improved employment outcomes (albeit not improved educational outcomes) have been observed in studies of early intervention programs additionally providing evidence-based vocational services [2, 16]. Most, however, have not considered predictors of changes in functional status after receiving treatment from a specialised early intervention service. Understanding predictors of not working/studying, particularly those, which are malleable, will enhance targeted vocational and psychosocial interventions.
This is a unique study in terms that data were collected prior to the introduction of a formal vocational intervention, namely individual placement support (IPS), to the Early Psychosis Prevention and Intervention Service (EPPIC, [3, 17]), Melbourne, Australia. It is a naturalistic observational study with three aims: (i) to delineate the premorbid, diagnostic and clinical characteristics of FEP patients with a poor functional status (either unemployed or not studying) at entry to a specialist early intervention service; (ii) to examine changes in functional status over an 18-month treatment period at the service; and (iii) to identify predictors of change in functional status.
Method
Sample and setting
The sample consisted of 786 youth registered at the Early Psychosis Prevention and Intervention Centre (EPPIC) between 1998 and 2000. EPPIC is a specialist early intervention service for youth experiencing FEP. Participants were aged between 15 and 29 years, residing in the north-western suburbs of Melbourne, Australia, and treated for up to 18 months [18]. This cohort was unique in that there were few other treatment facilities or private psychiatrists who serviced this catchment area at the time; thus, this is a treated epidemiological sample from a defined catchment area.
Between 1998 and 2000, IPS had not commenced at EPPIC and there was no employment consultant within the service. Young people would have access to medical review, clinical case management and may have been referred by case managers to other services to address issues such as housing, welfare or employment. Young people had the opportunity to access group programs at EPPIC that included some vocationally orientated groups [19]. At the time, young people could access disability support and unemployment benefits from external agencies.
A file audit was conducted on these patients as part of the First Episode Psychosis Outcomes Study (FEPOS, [20]). Of the 786, 82 were discharged or transferred to other services and their medical files were unavailable for review, and a further 43 had a non-psychotic diagnosis at discharge. Data were therefore available for 661 patients (see Fig. 1). The local research and ethics committee approved the study.
Materials
To systematically assess consecutive medical files, we used the Early Psychosis File Questionnaire [20]. The measures included in this questionnaire are detailed below.
Functional status
The modified vocational status index (MVSI, [21]) was used to measure functional status, rating individuals on one of the seven occupational levels: (1) full-time gainful employment (≥30 h/week); (2) homemaker or student; (3) part-time gainful employment; (4) retired; (5) full- or part-time volunteer; (6) on medical or psychiatric leave of absence; and (7) unemployed, whether or not expected to work. Good functioning status was defined as full-time employment, homemaker or student, part-time gainful employment or full- or part-time volunteer. Poor functioning status was defined as either being on medical or psychiatric leave, or unemployment. Individuals could only fall into one of these seven categories of the MVSI.
Diagnosis
Intake diagnoses were primarily performed by well-trained EPPIC clinicians working in a specialised assessment and crisis intervention team [20]. Two research psychiatrists (ML and PC) reviewed all the information in the medical file pertaining to diagnosis. A consensus rating between both research psychiatrists and the case manager was performed. For a subset of 115 randomly selected patients, SCID-I/P diagnoses were available and were used to determine the validity of FEPOS discharge diagnoses [21]. There was good concordance for both psychotic (κ = 0.80) and substance use (κ = 0.74) diagnoses [21].
Pretreatment characteristics
Characteristics of patients prior to service entry included: premorbid functioning in the year preceding illness onset using the global assessment of functioning scale (GAF); previous history and family history of psychiatric disorder (using DSM-IV-TR criteria); age of onset (when first experienced positive symptoms for longer than 1 week); DUP (age of entry into EPPIC minus age when first experienced positive psychotic symptoms for longer than 1 week); past substance use disorders [(SUD), using the drug and alcohol assessment schedule (DASS, [22])]; suicide attempts (ICD-10 categories); exposure to trauma (physical and/or sexual; [23, 24]); years in school; and forensic history (offence against property, motor traffic, drug-related offences, offences against persons; [25]).
Service entry
Characteristics assessed at service entry included: type and severity of substance use (DASS); severity of illness [using the Clinical Global Impressions—severity of illness (CGI-S, [26])] and Clinical Global Impressions—bipolar scales (CGI-BP, [27]); functioning (GAF); insight; and history of a learning disability [20].
Treatment and service discharge characteristics
Treatment factors included: illness severity (CGI-S and CGI-BP); type and severity of substance use disorders (DASS); level of functioning (GAF); involvement with the service or disengagement, defined as the patient’s refusal of treatment or the service being unable to contact the patient [28]; medication non-adherence, defined as not taking medication for 1 week or more [29]; and hospital admissions. At discharge, illness severity (CGI-S), global functioning (GAF) and persistent substance use were assessed.
Reliability and validity
Estimates obtained for inter-rater reliability for the CGI, CGI-BP, GAF, and insight for 40 files were good (range: ICC2,1 = 0.87 for CGI-S to ICC2,1 = 0.89 for insight score) [20].
Data analyses
A series of logistic regression models determined which premorbid and service entry variables were associated with functional status at entry. From these analyses, unadjusted odds ratios (OR) and the 95% confidence intervals (CI) of the ORs were derived. The Wald statistic (z) was used to determine significance of individual predictors. From these models, variables that were predictive of good or poor functional status at service entry at the p < 0.10 level were entered in a forward stepwise fashion (based on the Wald statistic) into a multivariate logistic regression model; this model allowed determination of which variables best differentiate good or poor functional status at service entry.
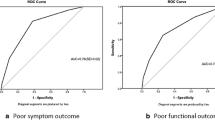
We also examined predictors of change in functional status over the course of treatment. Four categories were developed based on MVSI ratings at entry and discharge: (i) stable good (studying and/or working at entry and discharge); (ii) improved (not studying, working, homemaker, or volunteer at entry but were at discharge); (iii) decline (studying, working, homemaker or volunteer and/or working at entry but not at discharge); and (iv) stable poor (not studying, working, homemaker or volunteer at entry or discharge). A series of logistic regression models were developed to delineate individual variables that discriminated between: (i) stable good versus stable poor functional status; (ii) stable good versus those who had a decline in functional status; and (iii) stable poor versus those who improved in functional status. From these analyses, adjusted odds ratios (OR) and the 95% confidence intervals (CI) of the adjusted ORs were derived. Again, the Wald statistic (z) was used to determine significance of individual predictors. Variables that were related to the outcome variables at the p < 0.01 level were then entered into three separate multivariate stepwise (forward based on Wald statistic) logistic regression models to determine the best predictors associated with change in functional status.
Results
At service entry, data on functional status were available for 659 patients (see Fig. 1). Overall, 47.8% (n = 316) had a good functional status at service entry according to the MVSI, meaning they were engaged in some functional activity including 20.6% (n = 136) who had full-time employment and 21.5% (n = 142) who were homemakers/students; 5.5% (36) with part-time employment; and 0.3% (n = 2) volunteers. 52.0% (n = 343) of the cohort were not studying or unemployed at service entry (poor functional status).
Comparison to population data
Unemployment rates in the cohort were compared to Australian Bureau of Statistics (ABS 2001) Census data (Table 1). In the 15–19-year age range, 49.0% of the cohort was unemployed as compared to 18.7% in this age range in the general community. Notably, as age of the cohort increased, rates of unemployment increased while the converse was true in the general population.
Predictors of functional status at service entry
Univariate comparisons indicated that poor functional status at service entry was associated with male gender, fewer years of education, poor premorbid functioning as determined by the GAF, and histories of learning disabilities, substance use, forensic issues, sexual and/or physical trauma and a longer DUP (Table 2). Patients with poor functional status were also more likely to have an intake diagnosis of schizophrenia, a substance or polysubstance use disorder, more severe levels of psychotic symptomatology, poor insight into illness and poorer global functioning at presentation to the service. In a multivariate logistic regression model, there were seven predictors of poor functional status at service entry: fewer years of education, poorer premorbid functioning, past history of substance use, intake diagnosis of schizophrenia (compared to schizoaffective and bipolar disorders),Footnote 1 polysubstance use at service entry and insight at entry (Table 3). The comparison of these predictors against the constant-only model was statistically significant, χ 2(11) = 149.60, p < 0.001, indicating that the predictors reliably delineated differences between those with poor and good functional status at service entry; however, the explained variance in functional status was modest with Nagelkerke R 2 = 0.30. Using these variables, the model correctly classified 70.1% of those with a good functional status and 70.7% of those with a poor functional status (overall 70.4% correct classification).
Discharge functional status
Data on functional status at discharge were available for 569 patients (see Fig. 1). A series of comparisons were conducted to determine whether those who did and did not have 18-month data differed significantly with respect to premorbid and baseline characteristics. Those who did not have data at 18 months were more likely to have longer DUP (no data available M = 238.4, SD = 522.6; data available, M = 355.5, SD = 653.16, t(648) = −4.67, p < 0.001), a past history of substance use (no data available 84.8%, n = 78, N = 92; data available, 72.4%, n = 41, N = 569, χ 2(1) = 6.32, p = 0.012), substance use at service entry (no data available 72.8%, n = 67, N = 92; data available, 59.6%, n = 339, N = 569, χ 2(1) = 5.87, p = 0.015), more severe psychopathology (CGI-S, no data available M = 5.8, SD = 0.8; data available, M = 5.5, SD = 0.8, t(659) = 2.97, p = 0.003) and lower GAF (no data available M = 27.0, SD = 9.0; data available, M = 33.0, SD = 9.6, t(657) = 5.62, p < 0.001).
Table 4 comprises details on changes in functional status from baseline to discharge. Overall, 30.4% (n = 173) had a stable good functional status from baseline to discharge, 4.1% (n = 80) had an improved functional status, 18.3% (n = 104) had a decline in functional status, and 37.3% (n = 212) had stable poor functional status.
Stable good versus poor functional status
Multivariate logistic regression indicated that as compared to those with stable good functional status, those who had stable poor functional status were more likely to have lower levels of education, a lower premorbid GAF, longer DUP and a forensic history (Table 5). At service entry, they were older, were more likely to be polysubstance users and had poor insight and poor functioning. Persistent substance use through treatment was also problematic. This model was significantly different from the constant-only model, χ 2(10) = 221.51, p < 0.001. The Nagelkerke R 2 was 0.69. Overall, classification success was at 83.0% (good stable functional status 82.5% and poor stable functional status 83.4%).
Stable good versus decline in functional status
Multivariate logistic regression indicated that those who had a decline in functional status were more likely than those with a stable good functional status to have a significantly longer DUP (see Table 6). At service entry, they were more likely to be using cannabis and to have a lower GAF. They had a shorter duration of time in the service, a greater number of admissions and were more likely to be persistent substance users. The model with these variables was significantly better than the constant-only model, χ 2(7) = 48.64, p < 0.001, and the Nagelkerke R 2 was 0.23. Based on these variables, correct classification of those who had a decline in functional status was 43.6% and successful classification of those with a stable good functional status was 87.6% (overall correct classification 70.6%).
Stable poor versus improved functional status
Multivariate analyses indicated that those who had an improved functional status were more likely than those with a poor stable functional status to have a shorter DUP, be more adherent with treatment, and were less likely to be using substances during treatment (see Table 6). This model was significantly different from the constant-only model, χ 2(4) = 55.38, p < .001. The Nagelkerke R 2 was modest at 0.29. The classification rate for those who had improved functional status was 27.9%, whereas for those who had a poor stable functional status correct classification was at 90.9% (overall success in classification 74.0%).
Discussion
Previous studies have indicated that psychosis causes significant distress for the young person by disrupting attainment of vocational and educational goals, social relationships and identity formation [30]. However, in our study, there was evidence of functional decline prior to illness onset with disruption to both education and global premorbid functioning being more likely in those who had a poor functional status at service entry. Such findings indicate that for some individuals peer concordant functioning is not established [31].
In our study, just over 50% of the patients were unemployed or not studying at service entry. Unemployment rates were markedly higher than those seen in Australian 2001 Census data. Moreover, rates of unemployment in FEP increased with age, whereas the reverse was true in the general community. This study provides more evidence of poor functional status in a representative sample of FEP patients.
Those who were not employed and/or studying at service entry had a complicated history before accessing EPPIC. Based on univariate analyses, their functional decline appeared related to numerous problems: learning disabilities; exposure to traumatic experiences; forensic issues; a longer DUP; and ongoing substance use. However, multivariate analyses indicated that education, premorbid functioning and substance use (previous history and polysubstance use at service entry) were the strongest predictors of poor functional status. It may be the case that variables such as learning disabilities and exposure to traumatic experiences may increase the likelihood of educational difficulties and substance use. For example, cognitive problems often occur prior to the onset of clinical symptoms [32] and are observed during prodrome [33] or as early as first grade at school [34]. Poor premorbid academic functioning is associated with impairments in both verbal learning and working memory in individuals with FEP [35]. Because of learning difficulties, rates of secondary school drop-out are much higher in FEP cohorts [7]. Fewer years of formal education results may result in increased risky behaviours such as substance use [7] and criminal activity including violence towards others [36].
Exposure to traumatic experiences such as sexual abuse and/or physical abuse is common prior to the onset of psychotic disorders [23, 24, 37]. Such exposure has been associated with reduced psychosocial premorbid functioning including decreased educational attainment and poor work attendance [23, 37]. This relationship may be confounded by increased risk of substance use in FEP patients with a history of trauma [38].
As a consequence of a complex history, it is unsurprising that those who had a poor functional status at service entry had more severe symptomatology and poorer insight, were more likely to be abusing multiple substances and had poorer ratings of global functioning. 37.3% of those with a poor functional status at service entry still had a poor vocational status at discharge. Poor functional outcomes (compared with stable good outcomes) were associated with lower levels of premorbid functioning, less years of education, a forensic history, longer DUP, more severe symptoms and poorer functioning at service entry and discharge as well as more admissions and no change in substance use during treatment. Additional predictors of a stable poor functional status were a history of physical abuse, substance use or polysubstance use disorder and treatment non-adherence.
Only 30.4% of those FEP patients with a good functional status at service entry retained this status at discharge and only 14.1% achieved an improvement in their functional status at discharge. Predictors of maintenance of good functional level at discharge were virtually polar opposites of those associated with negative outcomes, highlighting potential protective factors and targets for clinical and vocational interventions.
It is worth mentioning that the predictive models pertaining to those who either declined or improved in functioning over the 18 months were less impressive in terms of classification and sensitivity. Statistical power may be one issue; however, it may be the case that factors other than those perused in this study may increase the predictive power of the models. For example, neurocognition and social cognition have been considered important predictors of functioning [39]. It may be the case that those with better neurocognition and social cognition may be more likely to improve over 18 months in terms of functioning. Further work on identifying other variables that may predict those who decline and improve in functioning over the course of treatment is needed.
While specialist early intervention programs result in better functional outcomes compared to standard care [5, 40], it is clear that those studying or working at service entry can still experience a decline in functional status during treatment [2, 15, 16]. In our cohort 18.3% experienced decline in functional status. This may be a reflection that those who have a worsening of symptoms are more likely to decline in function [41].
In line with the recent literature [2, 15, 16], we anticipate that those with a persistent poor functional status or who experience a decline in functional status may benefit from targeted vocational intervention in addition to SEI. Three to four years after this cohort of FEP EPPIC patients were discharged, individual placement support (IPS) was introduced at EPPIC [3, 17, 42]. IPS is considered suitable for anyone interested in looking for work, regardless of whether the individual is work-ready or symptom-free [17]. IPS involves an individualised approach to vocational support; employment consultants work closely with individuals to assess their interests and preferences with respect to employment. Support workers are integrated within mental health services and offer time-unlimited support, this continuing once a person has achieved the goal of competitive employment. Preliminary support for the effectiveness of IPS for FEP has been noted with respect to employment outcomes [3]. However, there are variables which may impact on the success of IPS interventions including motivation, substance use and cognitive abilities [43].
The primary limitation of this study was the use of retrospective medical file audit methodology. Numerous problems can exist with this approach including: poor quality of documented information, rater inexperience, lack of inter-rater reliability and poor data validity. Strategies were employed to minimise the impact of these limitations, including double-rating of medical files by two consultant psychiatrists with expert knowledge of EPPIC and the treatment of FEP, determination of inter-rater reliability for clinical and functioning measures, and establishing concurrent validity of psychoses and baseline SUD for a sub-sample of patients [20]. Another limitation of medical file auditing is the lack of more specific assessments (e.g. of neurocognitive deficits). More detailed data were not available on the sociodemographic characteristics of clients and the work and educational statuses of their parents.
An additional key limitation relates to a lack of more specific data regarding concurrent functional activities. A shortcoming of the MVSI is that it only allows for one status to be recorded for each individual. In some cases, this may not have accurately reflected circumstances (e.g. a person may have been engaged in both voluntary work and education). Information was also not available on utilisation of vocational group programs or access to external agencies, and with data collected at cross-sectional time-points, information was not available regarding stability of functional status from month to month over the 18 months. There also needs to be consideration that not everyone had 18 month data and those who did not have this data were more likely to have a history of substance use issues, longer DUP, more severe symptomatology and poorer functioning at presentation to the service. By not having data on this subgroup may mean that the estimates of poor functional outcomes at 18 months are an underestimate. Further, despite being a longitudinal study, our results do not allow for cause–effect analyses. Contrasting these limitations, the study comprised a large representative sample of patients with FEP.
In summary, a subgroup of FEP patients who are not studying and/or working at service entry appear to have a long history of functional impairment that might be related to exposure to traumatic experiences, learning disabilities and substance use. These problems were found to be more common in males and individuals with schizophrenia. Such factors may contribute to a delay in receiving treatment for psychosis. Consequently, at service entry, such patients have more severe symptoms and poor insight. Persistent substance use, forensic issues and lack of educational attainment all might impede future functioning and vocational opportunities. Thus, there is a need to get young people into treatment quickly, build upon engagement and relationships with young people and offer adjunctive treatments that may address comorbid substance use. Indeed, there is some evidence from longitudinal studies that by reducing substance use in individuals with early psychosis, better functional outcomes are assured [44, 45]. Apart from managing symptoms and substance use, vocational and psychosocial support during early intervention is essential [2], highlighting the importance an integrated model of early intervention.
Importantly, further research is needed to ascertain whether these risk factors for poor outcome are also found for those young people now receiving IPS in early intervention services. Finally, the FEPOS cohort is currently being followed up; through this new study, we will be able to map the trajectory of functional outcomes and to determine whether the same risk factors that apply in the short term, predict poor outcomes over the long term.
Notes
Schizophrenia was the reference category in the logistic regression. Those with schizoaffective disorders had significantly better outcomes than those with schizophrenia. The same result was found when comparing schizophrenia to bipolar disorder.
References
Rinaldi M, Killackey E, Smith J, Shepherd G, Singh SP, Craig T (2010) First episode psychosis and employment: a review. Int Rev Psychiatry 22:148–162
Bond GR, Drake RE, Luciano A (2016) Employment and educational outcomes in early intervention programmes for early psy-chosis: a systematic review. Epidemiol Psychiatr Sci 24:446–457
Killackey E, Jackson HJ, McGorry PD (2008) Vocational intervention in first episode psychosis: individual placement and support versus treatment as usual. Br J Psychiatry 193:114–120
Marwaha S, Johnson S (2004) Schizophrenia and employment. A review. Soc Psychiatry Psychiatr Epidemiol 39:337–349
Dewa CS, Trojanowski L, Cheng C, Loong D (2012) Examining the factors associated with paid employment of clients enrolled in first episode of psychosis programs. Schizophr Res Treatment 2012:739616. doi:10.1155/2012/739616
Norman RMG, Malla AK, Manchanda R, Windell D, Harricharan R, Takhar J, Northcott S (2007) Does treatment delay predict occupational functioning in first episode psychosis. Schizophr Res 91:259–262
Goulding SM, Chien VH, Compton MT (2010) Prevalence and correlates of school drop-out prior to initial treatment of non-affective psychosis: further evidence suggesting a need for supported education. Schizophr Res 116:228–233
Tapfumaneyi A, Johnson S, Joyce J, Major B, Lawrence J, Mann F, Chisholm B, Ra-haman N, Wooley J HF (2015) Predictors of vocational activity over the first year in inner-city early intervention in psychosis services. Early Interv Psychiatry 9:447–458
Turner N, Browne S, Clarke M, Gervin M, Larkin C, Waddington JL, O’Callaghan E (2009) Employment status amongst those with psychosis at first presentation. Soc Psychiatry Psychiatr Epidemiol 44:863–869
Chang WC, Man Tang JY, Ming Hui CL, Wa Chan SK, Ming Lee EH, Hai Chen EY (2014) Clinical and cognitive predictors of vocational outcome in first-episode schizophrenia: a prospective 3 year follow-up study. Psychiatry Res 220:834–839
Ramsay C, Stewart T, Compton MT (2012) Unemployment among patients with newly diagnosed first-episode psychosis: prevalence and clinical correlates in a US sample. Soc Psychiatry Psychiatr Epidemiol 47:797–803
Dickerson FB, Stallings C, Origoni A, Boronow JJ, Sullens A, Yolken RH (2007) The association between cognitive functioning and occupational status in persons with a recent onset of psychosis. J Nerv Ment Dis 195:566–571
Tandberg M, Ueland T, Andreassen A, Sundet K, Melle I (2012) Factors associated with occupation and academic status in patients with first-episode psychosis with a particular focus on neurocognition. Soc Psychiatry Psychiatr Epidemiol 47:1763–1773
Malla AK, Norman RMG, Manchanda R, Ahmed MR, Scholten D, Harricharan R, Cortese L, Takhar J (2002) One year outcome in first episode psychosis: influence of DUP and other predictors. Schizophr Res 54:231–242
Dudley R, Nicholson M, Stott P, G S (2014) Improving vocational outcomes of service users in an early intervention in psychosis service. Early Interv Psychiatry 8:98–102
Drake RE, Bond GR, Goldman HH, Hogan MF, Karakus M (2016) Individual Placement and Support services boost employment for people with serious mental illness, but funding is lacking. Health Aff 35:1098–1105
Killackey E, Allott K, Cotton S, Jackson HJ, Scutella R, Tseng Y-P, Borland J, Proffitt TM, Hunt S, Kay-Lambkin F, Chinnery G, Baksheev G, Alvarez-Jimenez M, McGorry PD (2013) A randomized controlled trial of vocational intervention for young people with first-episode psychois: method. Early Interv Psychiatry 7:329–337
Schimmelmann BG, Conus P, Cotton SM, Kupferschmid S, McGorry PD, Lambert M (2012) Prevalence and impact of cannabis use disorders in adolescents with early onset first episode psychosis. Eur Psychiatry 27:463–469
Cotton SM, Luxmoore M, Woodhead G, Albiston DD, Gleeson JFM, McGor ry PD (2011) Group programmes in early intervention services. Early Interv Psychiatry 5:259–266
Conus P, Cotton SM, Schimmelmann BG, McGorry PD, Lambert M (2007) The First-Episode Psychosis Outcome Study: premorbid and baseline characteristics of an epidemiological cohort of 661 first-episode psychosis patients. Early Interv Psychiatry 1(1):191–200
Tohen M, Hennen J, Zarate CM, Baldessarini RJ, Strakowski SM, Stoll AL, Faedda GL, Suppes T, Gebre-Medhin P, Cohen BM (2000) Two-year syndromal and functional recovery in 219 cases of first episode major affective disorder with psychotic features. Am J Psychiatry 157(2):220–228
McGorry PD, Copolov DL, Singh BS (1990) Royal park multidiagnostic instrument for psychosis: part II. Development, reliabillity and validity. Schizophr Bull 16(3):517–536
Conus P, Cotton SM, Schimmelmann BG, McGorry PD, Lambert M (2010) Pre-treatment and outcome correlates of sexual and physical trauma in an epidemiological cohort of first episode psychosis patients. Schizophr Bull 36:1105–1114
Conus P, Cotton SM, Schimmelmann BG, Berk M, Daglas R, McGorry PD, Lambert M (2010) Pretreatment and outcome correlates of past sexual and physical trauma in 118 bipolar I disorder patients with a first episode of psychotic mania. Bipolar Disord 12:244–252
Marion-Veyron R, Lambert M, Cotton SM, Schimmelmann BG, Gravier B, McGorry PD, Conus P (2015) History of offending behavior in first episode psychosis patients: a marker of specific clinical needs and a call for early detection strategies among young offenders. Schizophr Res 161:163–168
Guy W (1976) ECDEC Assesment manual for psychopharmacology, revised. National Institute of Mental Health, Rockville
Spearing MK, Post RM, Leverich GS, Brandt D, Nolen W (1997) Modification of the clinical global impressions (CGI) scale for use in bipolar illness (BP): the CGI-BP. Psychiatry Res 73(3):159–171
Conus P, Lambert M, Cotton S, Bonsack C, McGorry PD, Schimmelmann BG (2010) Rate and predictors of service disengagement in an epidemiological first-episode psychosis cohort. Schizophr Res 118:256–263
Robinson DG, Woerner MG, Alvir JM, Bilder RM, Hinrichsen GA, Lieberman JA (2002) Predictors of medication discontinuation by patients with first-episode schizophrenia and schizoaffective disorder. Schizophr Res 57:209–219
Malla AK, Norman R, Joober R (2005) First-episode psychosis, early intervention, and outcome: What have we learned. Can J Psychiatry 50(14):881–891
Rabinowitz J, De Smedt G, Harvey PD, Davidson M (2002) Relationship between premorbid functioning and symptom severity as assessed at first episode of psychosis. Am J Psychiatry 159:2021–2026
Cannon TD, Bearden CE, Hollister JM, Rosso IM, Sanchez LE, Hadley T (2000) Childhood cognitive functioning in schizophrenia patients and their unaffected siblings: a prospective cohort study. Schizophr Bull 26:379–393
Brewer WJ, Francey SM, Wood SJ, Jackson HJ, Pantelis C, Phillips LJ, Yung AR, Anderson VA, McGorry PD (2005) Memory impairments identified in people at ultra-high risk for psychosis who later develop first-episode psychosis. Am J Psychiatry 162:71–78
Bilder RM, Reiter G, Bates J, Lencz T, Szesko P, Goldman RS, Robinson D, Lieberman JA, Kane JM (2006) Cognitive development in schizophrenia: follow-back from the first episode. J Clin Exp Neuropsychol 28:270–282
Rund BR, Melle I, Friis S, Johannesen JO, Larsen TK, Midboe LJ, Opjordsmoen S, Simonsen E, Vaglum P, McGlashan T (2007) The course of neurocognitive functioning in first-episode psychosis and its relation to premorbid adjustment, duration of untreated psychosis, and relapse. Schizophr Res 91:132–140
Large MM, Nielssen O (2011) Violence in first-episode psychosis: a systematic review and meta-analysis. Schizophr Res 125:209–220
Ramsay C, Flanagan P, Gantt S, Broussard B, Compton MT (2011) Clinical correlates of maltreatment and traumatic experiences in childhood and adolescence among predominantly African American, socially disadvantaged, hospitalized, first-episode psychosis patients. Psychiatry Res 188:343–349
Compton MT, Furman AC, Kaslow NJ (2004) Preliminary evidence of an association between childhood abuse and cannabis dependence among African American first episode schizophrenia-spectrum disorder patients. Drug Alcohol Depend 76:311–316
Allott K, Cotton S, Chinnery G, Baksheev G, Massey J, Sun P, Collins Z, Barlow E, Broussard C, Wahid T, Proffit T, Jackson H, Killackey E (2013) The relative contribution of neurocognition and social cognition to 6-month vocational outcomes following individual placement and support in first episode psychosis. Schizophr Res 150:136–143
Garety PA, Craig TKJ, Dunn G, Fornells-Ambrojo M, Colbert S, Rahaman N, Read J, Power P (2006) Specialised care for early psychosis: symptoms, social functioning and patient statisfaction: randomised controlled trial. Br J Psychiatry 188:37–45
Menezes NM, Arenovich T, Zipursky RB (2006) A systematic review of longitudinal outcome studies of first-episode psychosis. Psychol Med 36:1349–1362
Killackey E, Jackson HJ, Gleeson J, Hickie I, McGorry PD (2006) Exciting career opportunity beckons! Early Intervention and vocational rehabilitation in first episode psychosis: employing cautious optimism. Aust NZ J Psychiatry 40:951–960
Lehman AF, Goldberg R, Dixon L, McNary S, Postrado L, Hackman A, McDonnell K (2002) Improving employment outcomes for persons with severe mental illnesses. Arch Gen Psychiatry 59:165–172
Abdel-Baki A, Ouellet-Plamondon C, Salvat E, Grar K, Potvin S (2017) Symptomatic and functional outcomes of substance use disorder persistence 2 years after admission to a first-episode psychosis program. Psychiatry Res 247:113–119
Kerfoot KE, Rosenheck RA, Petrakis IL, Swartz S, Keefe RSE, McEvoy JP, Stroup TS (2011) Substance use and schizophrenia: adverse correlates in the CATIE study sample. Schizophr Res 132:177–182
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cotton, S.M., Lambert, M., Schimmelmann, B.G. et al. Predictors of functional status at service entry and discharge among young people with first episode psychosis. Soc Psychiatry Psychiatr Epidemiol 52, 575–585 (2017). https://doi.org/10.1007/s00127-017-1358-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-017-1358-0