Abstract
Purpose
Mental ill health in adults with intellectual disability (ID) is a neglected field in psychiatry and thus still widely understudied. This paper provides data on the prevalence of mental illness and problem behaviour and analyses support needs, mental health service use and psychotropic medication in a representative sample of adults with mild to moderate ID.
Methods
A set of well-established instruments was used to assess the main parameters in n = 371 participants recruited within a cross-sectional epidemiological multicentre study using a stratified randomised cluster sampling.
Results
Point prevalence of mental disorders was 10.8 %, that of problem behaviour 45.3 %. Most study participants needed help in specific lower order need areas (e.g., money budgeting, food, accommodation), and these need areas were mostly rated as met. The highest ratios of unmet to met need were found with respect to sexuality issues and with respect to mental health problems. The focus of psychiatric treatment was psychotropic medication.
Conclusions
Referring to ICD-10 based diagnostic criteria and consequently avoiding confusing problem behaviour with mental disorders, point prevalence of mental disorders was lower than in the general population. A systematic deficit in meeting mental health problems in adults with ID indicates the need for implementing strategies to maximise the quality of identification and management of mental disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ratification of the UN Convention on the rights of persons with disabilities [1] stimulated discussion about mental health issues in adults with intellectual disability (ID). A number of national and international clinical guidelines or recommendations on mental health care in adults with ID have been published in the last years [2, 3]. However, this topic is still widely understudied. Knowledge about the most important epidemiological parameters to be assessed within health services research (i.e., prevalence of mental health problems, prevalence of needs for care, health care utilization [4]) is rather scarce.
The few existing studies on the prevalence of mental disorders in adults with ID reported widely varying prevalence rates. In previous systematic reviews, reported prevalence rates ranged from 3.9 to 46.3 % [5] or from 13.9 to 75.2 % [6], respectively. One of the methodically most elaborate studies reported population-based point prevalence rates between 15.7 and 40.9 or 15.6 and 28.3 %, respectively, depending on the diagnostic criteria used and depending on the inclusion or exclusion of problem behaviours [7]. The relationship between mental disorders, defined as a consensus about clusters of clinical symptoms, and problem behaviour, defined as socially striking behaviour that causes distress, harm or drawback to the person or to others (e.g., screaming or shouting, aggression towards others) [2] and that has complex and multifactorial causes (e.g., physical complaints, societal factors or mental disorders [8]), however, is not fully understood [9–11]. In light of this, it was strongly recommended not to confuse problem behaviour with mental illness, although adults with ID may suffer from both [3].
Even less is known about the extent to which existing support systems meet the needs of adults with ID. The few present studies, most of them conducted with small samples, reported specific lower order needs such as food or accommodation as mostly met, but they also suggest a deficit in meeting higher-order needs such as receiving help due to mental health problems, behaviour problems or problems in sexual expression [12]. This might be explained by the fact that, in many countries, the needs of adults with ID cross traditional lines of responsibility between ID professionals and mental health professionals. However, methodically sound research into service use is lacking.
In contrast, much research has been conducted on the use of psychotropics in adults with ID. Recent findings suggest that adults with ID still comprise an overmedicated population and that especially prescription of antipsychotics often violates existing guidelines [2, 13].
Against this background, the purpose of the present study was to examine mental illness, problem behaviour, needs and mental health service use in a representative sample of adults with mild to moderate ID.
Methods
The MEMENTA-Study [14] (“Mental health care provision for adults with mental retardation and a psychiatric diagnosis”) was a cross-sectional, epidemiological, multicentre study funded by the Federal Ministry of Education and Research (BMBF, Grant ID-No. 01GY1134).
Setting
The study was set in three different regions of Germany, the Regional Area Dresden (1.6 m inhabitants, 205/km2), the Rhine Neckar Metropolitan Region (2.3 m inhabitants, 410/km2), and Bavarian Swabia (1.8 m inhabitants, 179/km2). It thus covered urban and rural areas in West and East Germany.
Ethics
The project was approved by all relevant ethics committees. Informed consent was obtained by the person with ID themselves and, if the adult with ID lacked decision-making capacity, by their legal guardian.
Participants
The target population was a representative sample of adults with mild or moderate ID, aged between 18 and 65 years.
A newly developed standardised assessment sheet was used to assess the level of ID. It is based on the definition of ID by the American Association on Intellectual and Developmental Disabilities and on well-defined criteria of impairment in different degrees of ID [15, 16]. It comprises six items assessing the level of functioning in three skill domains (conceptual, practical and social) on four-point scales indicating different levels of disability (A = severe ID, B = moderate ID, C = mild ID, D = learning disability). However, the instrument does not allow a solid distinction between different levels of ID. The inclusion criterion of a mild to moderate ID was met if skills were rated as mild or moderately impaired in at least two of the three domains.
As regional registers of adults with ID do not exist and as, in Germany, the vast majority of the target population is employed in a sheltered workshop, the study population was accessed through sheltered workshops.
Recruitment
A stratified randomised cluster sampling was used.
Random selection of sheltered workshops
A systematic search was conducted in April and May 2012 to identify all sheltered workshops for adults with ID in each study region. At this stage, 56 institutions were identified in the Regional Area Dresden, 15 institutions in the Rhine Neckar Metropolitan Region and 28 institutions in Bavarian Swabia. Altogether, 11,542 potential study participants were employed in these 99 sheltered workshops.
In each study region, the identified sheltered workshops were stratified by (1) type of service-providing non-governmental organisation and (2) size. To keep the burden on potentially participating institutions reasonable, we decided to assess a maximum of 15 % of all employees of a participating sheltered workshop. The number of sheltered workshops to be randomly selected from each specific stratum directly resulted from intended sample sizes and from the aim to recruit study participants representatively from each stratum. Thus, 20 institutions were randomly selected in the Regional Area Dresden, 14 in the Rhine Neckar Metropolitan Region and 11 in Bavarian Swabia. Two institutions refused to participate so that they had to be replaced by two other randomly selected institutions. The 45 participating sheltered workshops employed a total of 6487 potential study participants.
Random sampling of potential study participants
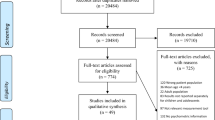
Subsequently, 1165 potential study participants were randomly selected between September 2012 and April 2014 from an anonymous list of all employees with ID working in each randomly selected sheltered workshop, 487 of which could be assessed for eligibility. Finally, 371 datasets on adults with mild or moderate ID were available (Fig. 1). Information was gathered from relevant staff members in the sheltered workshops (n = 132) or key carers (n = 4) or from both informants (n = 235).
Measures
Mental health status
The Psychiatric Assessment Schedule for Adults with Developmental Disability Checklist (PAS-ADD Checklist [17, 18]) was used to screen for symptoms of mental illness. This instrument was designed to be easily completed by untrained users and has shown good reliability [18]. Twenty-five items measuring severity and frequency of psychiatric symptoms during the past 4 weeks were rated on a four-point rating scale. Ratings for each item were combined to three subscales: ‘affective or neurotic disorder’ (20 items), ‘possible organic condition’ (six items) and ‘psychotic disorder’ (three items), which each have a threshold score indicating the presence of a potential psychiatric problem. In addition, items were dichotomised into symptom present/absent to report the prevalence of specific symptoms.
If either the PAS-ADD Checklist scores and/or specific behaviour described and/or current intake of psychotropic drugs and/or any current or lifetime psychiatric disorder suggested an existing psychiatric symptomatology, the semi-structured Mini Psychiatric Assessment Schedule for Adults with Developmental Disability (Mini PAS-ADD Interview [19]) was used to collect detailed information on psychiatric symptoms. The Mini PAS-ADD interview assesses primary psychiatric symptoms based on their frequency and severity during the past 4 weeks. It has shown good psychometric properties and is considered the best instrument for adults with ID [20]. The assessment on 66 items produces six symptom scores relating to ICD-10 based diagnostic categories: ‘depression’ (17 items), ‘anxiety’ (seven items), ‘mania/hypomania’ (11 items), ‘obsessive compulsive disorder’ (four items), ‘psychosis’ (eight items), ‘unspecified disorder’ (i.e., dementia and other organic problems, eight items). Threshold scores exist for each diagnostic area. If scores reached or exceeded a threshold, criteria for a specific psychiatric diagnosis were considered as met.
Items on the PAS-ADD Checklist were rated by relevant staff of the sheltered workshop and or the key carer. Items on the Mini PAS-ADD interview were rated by the interviewers based on information gathered from relevant staff of the sheltered workshop and or the key carer.
Problem behaviour
The Aberrant Behavior Checklist-Community (ABC-C [18, 21]) was used to assess problem behaviour. It has shown good psychometric properties [18]. Each of 58 items was rated by relevant staff of the sheltered workshop and or the key carer on a four-point scale as (0) no, (1) slight, (2) moderate or (3) severe problem, based on the frequency and severity of problem behaviour shown during the past 4 weeks. A participant was classified as presenting clinical significant behaviour problems if at least one of the ABC-C items was rated as a moderate or severe problem by either relevant staff from the sheltered workshop or the key carer [9].
Needs
The Camberwell Assessment of Need for Adults with Developmental and Intellectual Disabilities (CANDID [22]) was used to assess needs. It is a semi-structured interview measuring needs in 25 areas, indicating no, met or unmet need. The CANDID has shown good psychometric properties [12]. A specific need was rated as existing if either the relevant staff of the sheltered workshop or the key carer rated the specific need as existing; it was rated as unmet if either the relevant staff of the sheltered workshop or the key carer rated the specific need as unmet.
Health services utilization and psychotropic medication
The Client Socio-Demographic and Service Receipt Inventory (CSSRI [23]) was used to assess health service use in the preceding 3 months as well as detailed information about medication taken in the preceding month. We used a version that has been adapted to the specific conditions of the MEMENTA-Study, e.g., by itemizing specialized services for adults with ID. Information was obtained by all available sources (e.g., clients’ records of the person with ID from the sheltered workshops or sheltered housing institutions and information provided by all interviewees). In the present study, we will report on mental health services use and psychotropic medication only.
Interviewers
Data were collected by three interviewers per study site which had been trained by experts prior to data collection. The 4-day interviewer training covered transfer of knowledge on ID in general, on mental-ill health in adults with ID, and on all instruments used for data collection.
To ensure the same interview procedures across all interviewers, detailed instructions were provided in an interview manual, and case vignette ratings were conducted and discussed monthly on the Mini PAS-ADD interview and the CANDID throughout the course of the study.
Statistical analyses
Frequency data were derived for point prevalence rates. Odds ratios were calculated to assess the association of mental disorders and problem behaviour with basic socio-demographic variables: age group, gender, and living situation. Association between age group, gender and living situation with total number of needs and total number of unmet needs was assessed by comparing means using t test or rather analysis of variance. The association between mental disorders and problem behaviour with mental health service use and psychotropic medication was assessed in 4 × 2 tables, from which due to otherwise small cell frequencies odds ratios were calculated for psychotropic medication only.
Results
Sample
The cohort of 371 adults with ID comprised 217 men (58.5 %) and 154 women (41.5 %). Mean age was 37.7 years (range 18–64). About half of the cohort lived in a residential accommodation (n = 136, 37.0 %) or another supported housing arrangement (n = 40, 10.9 %), 157 (42.7 %) lived with a family carer, and 35 (9.5 %) lived alone. Mean duration of employment in a sheltered workshop was 14.7 years (range 0–46). Information about physical illnesses was available for 334 of our adults with ID. Epilepsy was prevalent in 6.9 % (n = 23).
The cohort of 262 informants in the sheltered workshops comprised 139 men (53.1 %) and 123 women (46.9 %) with a mean age of 45.3 years (range 20–76). They knew the adult with ID for 6.6 years on average.
The cohort of 227 key carers comprised 118 relatives and 109 staff members in sheltered housing institutions. Relatives comprised 28 men (23.7 %) and 90 women (76.3 %) with a mean age of 58.4 years (range 40–82). Most relatives, predominantly parents (n = 105, 89.0 %), were in daily contact with the adult with ID (n = 101, 86.7 %). Staff members in sheltered housing institutions comprised 28 men (25.7 %) and 81 women (74.3 %) with a mean age of 41.2 years (range 22–60). Most of them (n = 94, 86.6 %) had at least four times a week contact with the adult with ID whom they knew for 16.9 years on average.
Prevalence of mental illness
The highest point prevalence of a specific symptom was found for ‘irritability or bad temper’ (40.7 %, n = 144) and for ‘depressed mood’ (28.1 %, n = 100). All other symptoms showed a prevalence of less than 20 % (Table 1).
In total, 9.2 % (n = 34) reached the PAS-ADD Checklist threshold score on the ‘affective or neurotic disorder’ subscale (3.2 %, n = 12), the ‘possible organic condition’ subscale (1.4 %, n = 5) or the ‘psychotic disorder’ subscale (6.7 %, n = 25). In due consideration of all defined criteria, the Mini PAS-ADD was completed for 122 (32.9 %) adults with mild to moderate ID.
Forty participants (10.8 %) met the Mini PAS-ADD criteria for at least one mental disorder. The percentages of participants who scored above the cut-offs for a specific mental disorder ranged from 0.8 % (n = 3) for ‘mania/hypomania’ and ‘unspecified disorder’ to 4.3 % (n = 16) for ‘psychosis’ (cf. Table 2).
Odds for at least one mental disorder did not differ in males (OR = 1.21, 95 % CI 0.61–2.37) compared to odds in females, and, similarly, odds in those aged between 35 and 49 (OR = 0.71, 95 % CI 0.33–1.55) as well as odds in those aged older than 50 (OR = 1.00, 95 % CI 0.42–2.41) did not differ significantly from the odds in the reference group of those aged between 18 and 34. In adults with ID living in a residential accommodation or any other supported arrangement (OR = 3.12, 95 % CI 0.71–13.76) and in adults with ID living with their family members (OR = 1.12, 95 % CI 0.24–5.37), odds did not differ significantly from the odds in the reference group of those living alone.
Prevalence of problem behaviour
The most frequent problem behaviours found were: ‘easily distractible’ (15.1 %, n = 56); ‘listless, sluggish, inactive’ (9.7 %, n = 36); ‘talks excessively’ (9.2 %, n = 34); ‘aggressive to others’ (8.6 %, n = 32); ‘throws temper tantrum when s/he does not get own way’ (8.6 %, n = 32); ‘irritable and whiny’ (8.4 %, n = 31); ‘disobedient; difficult to control’ (7.8 %, n = 29); ‘temper tantrums’ (7.5 %, n = 28). All other items showed a prevalence of less than 7.5 %.
Of the total sample of 371 adults with ID, 168 (45.3 %) were rated as showing at least one moderate or severe problem behaviour, 42 (11.3 %) of which showed exactly one, 44 (11.8 %) between two and five, and 82 (22.2 %) more than five and up to 26 moderate or severe problem behaviours. Percentage of adults with ID without a comorbid mental disorder and without any problem behaviour was 52.3 % (n = 194; cf. Table 2).
Adults with ID living in a residential accommodation or another supported housing arrangement had significantly higher odds (OR = 3.47, 95 % CI 1.54–7.82) for any problem behaviour compared to the reference group of those living alone. In adults with ID living with their family members (OR = 1.89, 95 % CI 0.83–4.29) odds did not differ compared to this reference group.
Odds in males (OR = 1.08, 95 % CI 0.71–1.64) did not differ compared to the odds in females, and, similarly, odds in those aged between 35 and 49 (OR = 0.88, 95 % CI 0.55–1.40) as well as odds in those aged older than 50 (OR = 1.18, 95 % CI 0.67–2.08) did not differ significantly from the odds in the reference group of those aged between 18 and 34.
Met and unmet needs
According to the proxy-ratings, most of our participants needed help in specific lower order areas (e.g., ‘money budgeting’,’welfare benefits’,’daytime activities’, and ‘accommodation’), and, overall, this specific lower order need was highly met (cf. Table 3).
Unmet needs were most frequent in higher-order areas of needs (e.g., ‘sexual expression’, ‘social relationships’, ‘basic education’, and ‘minor mental health problems’).
The ratio of an unmet need to an existing need, either met or unmet, indicating deficits in meetings an existing need, was especially high in higher-order need areas (e.g., ‘sexual expression’, ‘minor mental health problems’, ‘substance misuse’, ‘major mental health problems’, and ‘communication’).
Altogether, the mean total number of needs per adult with ID was 11.2 (SD = 3.6), the mean total number of unmet needs was 1.0 (SD = 1.3). The total number of needs and the total number of unmet needs was neither associated with gender nor with age. Adults with ID living in a residential accommodation or another supported housing arrangement had a significantly higher total number of needs (M = 12.3, SD = 3.2) compared to those living with their families (M = 10.9, SD = 3.5) or those living alone (M = 7.1, SD = 2.7; F = 37.3, p = 0.000). However, the total number of unmet needs was not associated with the living situation (F = 1.83, p = 0.163).
Mental health services use and psychotropic medication
Within the last 3 months prior to assessment, only a small number of adults with ID had had contact with hospital based psychiatric services (n = 8, 2.3 %), community based psychiatric services (n = 4, 1.3 %) or an office-based psychotherapist (n = 10, 3.4 %; cf. Table 4). An office-based psychiatrist had been contacted by 29 (9.9 %) of the adults with ID.
Within the last month, psychotropic medication had been used by 64 (19.5 %) adults with ID, with anti-psychotics being the most prevalent (n = 42, 12.2 %). Moreover, 49 (14.9 %) adults with ID had used anticonvulsants, 16 (4.9 %) of which had not used any other psychotropic drug. Of those adults with ID without a comorbid mental disorder, 42 (14.4 %) had used psychotropic medication, and 40 (13.7 %) had used anticonvulsants.
Prescription of psychotropic medication in adults with ID was significantly associated both with comorbid mental health problems and with problem behaviour. Those without a comorbid mental health disorder and at least one problem behaviour (OR = 2.20, 95 % CI 1.28–3.77), those with a comorbid mental health disorder without any problem behaviour (OR = 4.33, 95 % CI 1.03–18.23) and those with a comorbid mental disorder plus at least one problem behaviour (OR = 11.38, 95 % CI 4.63–27.92) had significantly higher odds compared to the reference group of those without a comorbid mental disorder and without any problem behaviour.
Discussion
Summary and comparison with previous research
Using the Mini PAS-ADD and consequently avoiding confusing problem behaviour with mental disorders, we found that 10.8 % of our study population of adults with mild or moderate ID met criteria for any mental disorder. This overall rate is lower than that observed in the German general population which is, referring to the mental disorders assessed within our study, 17.2 % [24]. A merely slightly higher prevalence rate of 14.5 % was found in a study from the UK which used ICD-10-DCR and included, in contrast to our study, adults with mild to profound ID [7]. Another study from the UK, which also used the mini PAS-ADD, found a considerably higher prevalence rate of 22.2 % in adults with mild to moderate ID, but this study selected participants (n = 90) with communication skills from local social services case registers so that the reported prevalence rate is likely to overestimate the true prevalence rate [25].
The rate of psychosis (4.3 %) and the rate of obsessive compulsive disorder (4.0 %) found in our study were higher compared with the German general population which showed rates of 1.5 and 0.4 %, respectively [24]. The finding that psychotic disorders [26] and obsessive compulsive symptoms [27] are more prevalent in adults with ID than in adults without ID is in line with previous research.
The comparison of findings from different studies on the prevalence of problem behaviour in adults with ID underlies well-known difficulties. Using different definitions and different methods, previous studies found totally different rates of problem behaviour: Emerson and colleagues [28] found relatively low rates of problem behaviour in adults with ID (12.1–16.5 %) compared to Deb and colleagues (60.4 % [29]). Cooper and colleagues [7] found extremely low rates of problem behaviour when referring to ICD-10-DCR or DSM-IV-TR (0.1 % each) compared to 22.5 % when referring to clinical diagnosis. In comparison, we found a relatively high prevalence rate (45.3 %), probably due to our broader definition of problem behaviour.
The present study especially presents new findings on met and unmet needs of adults with ID, as the few previous studies had been conducted with very small samples (n ≤ 40 [12, 30]), reported limited information only [31], or assessed needs in older persons with ID [32]. This limitation in mind, our finding that help needed in specific lower order need areas was common and highly rated as met, is in accord with previous findings. As concerns higher-order need areas such as help needed for minor or major mental health problems, the ratio of unmet to met need was significantly higher in our study compared to another study using the CANDID [12]. This study, however, recruited adults already using community-based mental health services and thus probably overestimated the frequency of met mental health needs in adults with ID. Altogether, findings support the assumption that, irrespective of the living environment, the existing support system for adults with ID is largely successful in meeting the specific lower order needs of this population, but has significant deficits in meeting less common and less specific mental health needs [12, 30].
The most common strategy for meeting mental health needs in adults with ID is psychotropic medication [13]. We found that 19.5 % of our study participants used psychotropic drugs, and that another 10.0 % used anticonvulsants. This overall rate of psychotropic medication is slightly higher than that reported in an older study from Germany that found that 21.5 % used psychotropics and 0.2 % used anticonvulsants [33]; in contrast, it is considerably lower than that reported in studies from the UK (50.5 % [25] or the US (58.0 % [13]). Although comparability across studies with different recruitment strategies is limited, this supports the suggestion [33] that psychotropic medication in adults with ID is less frequent in Germany compared to other high-income countries. As in previous studies [13, 34], however, psychotropic medication was associated with problem behaviour, indicating that it is, inconsistent with existing guidelines [2], still accepted as an important treatment option for behaviour problems in adults with ID.
Mental health service use was found to be basically limited to visiting a psychiatrist: nearly 10 % of all study participants and about 37 % of those diagnosed as suffering from any mental disorder had been in contact with a psychiatrist within the last 3 months prior to assessment. In contrast, only 3.4 % (n = 10) and 7.9 % (n = 3), respectively, had been seeing a psychotherapist. Thus, mentally-ill adults with ID seem to show higher rates of contacts with a psychiatrist compared with mentally-ill adults without ID, and, in contrast to them, lower rates of contacts with a psychotherapist than with a psychiatrist [35]. This finding hypothesises that psychotherapy might be not as established in the treatment of mental ill-health in adults with mild to moderate ID as in adults without ID. However, as psychosis was the most prevalent illness in our population and as adults without ID suffering from psychotic disorders also show lower rates of contacts with a psychotherapist, this conclusion must be drawn carefully.
Strengths and limitations
A special strength of the MEMENTA-study is that it is the first large-scale study assessing met and unmet needs and mental health service use of adults with mild to moderate ID. In addition, it used well-established instruments and consequently avoided confusing problem behaviour with mental disorders. All interviewers, most of them psychologists with psychiatric experience, had been extensively trained prior to data collection. To consider the low sensitivity of the PAS-ADD Checklist [7] and to avoid underestimation of the prevalence rate of mental disorders, we established broader inclusion criteria for using the Mini PAS-ADD [14]. The Mini PAS-ADD in fact uses ICD-10 based diagnostic categories and thus mainly uses criteria that define a symptom cluster as a disorder in the general population which might be difficult to be used in adults with ID [36].
The study was set in three different regions, and a complex clustered randomized sampling approach was chosen [14]. However, we encountered well-known barriers into the recruitment of adults with ID [37]: Owing to the lack of regional registers that could be used for identification of potential participants, we decided to access our target population through sheltered workshops. Thus, sampling may be biased by excluding adults with ID not working in sheltered workshops. However, this should primarily pertain to adults with severe or profound ID, as the vast majority of our target population works in sheltered workshops and as sampling was not meaningfully biased by absenteeism caused by any illness or holiday.
A major limitation of our study is that we had to accept a high number of refusals for participation. However, there is no indication that this caused a systematic error.
Conclusions
A positive finding of our study is that adults with mild to moderate ID can be presumed to be a group that is, with respect to basic needs, well-served by their relatives and the existing support system, respectively. The relatively high ratio of unmet to met needs found with respect to minor and major mental health problems, however, reveals a systematic deficit in meeting mental health needs. This is probably owing to the fact that mental health care for adults with ID is, in Germany as in many other countries, provided by a system that is separated from ID services, so that the needs of adults with ID cross traditional lines of professional responsibility. Consequently, it has been postulated that partnership working should be supported and access to mental health services should be improved [38].
The highest ratio of unmet to met needs was found with respect to sexuality issues. The lack of attention towards sexuality of adults with ID is owing to several reasons [39]. To lower related shame and fear and to reframe dysfunctional attitudes of professionals and family carers, opportunities for discussion and information should be provided. This would facilitate the provision of badly needed individually tailored sex education to adults with ID [39, 40].
Prescription of psychotropic drugs for the management of problem behaviour in adults with ID remains controversial [41]. A better adherence to existing guidelines for the management of problem behaviours in adults with intellectual disabilities [2] is needed.
Finally, present findings add important information to the literature regarding mental health problems and met and unmet needs in adults with mild to moderate ID. However, much more research into the development of an appropriate mental health care system for adults with ID is needed. A particular research gap exists regarding mental health problems and mental health services provision for adults with severe to profound ID. Prescription of psychotropic medication needs to be re-assessed to evaluate the effectiveness of recently published guidelines [2]. Cross-national studies, involving countries with different support systems, would allow a comparison and thus a better understanding of the factors underlying successful service provision in this neglected field of mental health care.
References
UN General Assembly. Convention on the rights of persons with disabilities: A/RES/61/106.2006
Deb S, Kwok H, Bertelli M, Salavdor-Carulla L, Bradley E, Torr J, Barnhill J, for the Guideline Development Group of the WPA Section on Psychiatry of Intellectual Disability (2009) International guide to prescribing psychotropic medication for the management of problem behaviours in adults with intellectual disabilities. World Psychiatry 8:181–186
Joint Commissioning Panel for Mental Health (2013) Guidance for commissioners of mental health services for people with learning disabilities. JCP-MH, London
Schrappe M, Pfaff H (2011) Versorgungsforschung: Konzept und Methodik (Health services research: concept and methods). Dtsch Med Wochenschr 136:381–386
Whitacker S, Read S (2006) The prevalence of psychiatric disorders among people with intellectual disabilities: an analysis of the literature. J Appl Res Intellect 19:330–345
Buckles J, Luckasson R, Keefe E (2013) A systematic review of the prevalence of psychiatric disorders in adults with intellectual disability, 2003–2010. J Mental Health Res Intellect Disabil 6:181–207
Cooper S, Smiley E, Morrison J, Williamson A, Allan L (2007) Mental ill-health in adults with intellectual disabilities: prevalence and associated factors. Br J Psychiatry 190:27–35
Ali A, Blickwedel J, Hassiotis A (2014) Interventions for challenging behaviour in intellectual disabilities. Adv Psychiatr Treat 20:184–192
Myrbakk E, von Tetzchner S (2008) Psychiatric disorders and behaviour problems in people with intellectual disability. Res Dev Disabil 29:316–332
Bertelli MO, Rossi M, Scuticchio D, Bianco A (2015) Diagnosing psychiatric disorders in people with intellectual disabilities: issues and achievements. AMHID 9:230–242
Thakker Y, Bamidele K, Ali A, Hassiotis A (2012) Mental health and challenging behaviour: an overview of research and practice. AMHID 6:249–258
Xenitidis K, Thornicroft G, Leese M, Slade M, Fotiadou M, Philip H, Sayer J, Harris E, McGee D, Murphy DGM (2000) Reliability and validity of the CANDID—a needs assessment instrument for adults with learning disabilities and mental health problems. Br J Psychiatry 176:473–478
Tsiouris JA, Kim SY, Brown WT, Pettinger J, Cohen IL (2013) Prevalence of psychotropic drug use in adults with intellectual disability: positive and negative findings from a large scale study. J Autism Dev Disord 43:719–731
Koch A, Vogel A, Holzmann M, Pfennig A, Salize HJ, Puschner B, Schützwohl M (2014) MEMENTA—‘mental healthcare provision for adults with intellectual disability and a mental disorder’. A cross-sectional epidemiological multisite study assessing prevalence of psychiatric symptomatology, needs for care and quality of healthcare provision for adults with intellectual disability in Germany: a study protocol. BMJ Open. doi:10.1136/bmjopen-2014-004878
Luckasson R, Schalock RL, Spitalnick DM, Spreat S (2002) Mental retardation: definition, classification, and systems of support, 10th edn. American Association on Mental Retardation, Washington
Gaese F (2007) Intelligenzminderung (F7). In: Schanze C (ed) Psychiatrische Diagnostik und Therapie bei Menschen mit Intelligenzminderung. Schattauer, Stuttgart, pp 131–144
Moss S (2002) PAS-ADD checklist. Pavilion Pub Publishing and Media, Brighton
Zeilinger EL, Weber G, Haveman MJ (2011) Psychometric properties and norms of the German ABC-community and PAS-ADD checklist. Res Dev Disabil 32:2431–2440
Moss S (2002) The mini PAS-ADD interview pack. Pavilion Publishing and Media, Brighton
Prosser H, Moss S, Costello H, Simpson N, Patel P, Rowe S (1998) Reliability and validity of the mini PAS-ADD for assessing psychiatric disorders in adults with intellectual disability. J Intellect Disabil Res 42:264–272
Aman MG, Singh NN (1994) Aberrant behavior checklist-community. Slosson Educational Publications Inc, East Aurora
Xenitidis K, Slade M, Thornicroft G, Bouras N (2003) CANDID: Camberwell assessment of need for adults with developmental and intellectual disabilities. Gaskell, London
Chisholm D, Knapp MR, Knudsen HC, Amaddeo F, Gaite L, van Wijngaarden B (2000) Client socio-demographic and Service receipt inventory—European version: development of an instrument for international research. Br J Psychiatry Suppl 177:s28–s33
Jacobi F, Wittchen HU, Hölting C, Höfler M, Pfister H, Müller N, Lieb R (2004) Prevalence, co-morbidity and correlates of mental disorders in the general population: results from the German Health Interview and Examination Survey (GHS). Psychol Med 34:597–611
Deb S, Thomas M, Bright C (2001) Mental disorder in adults with intellectual disability. 1: prevalence of functional psychiatric illness among a community-based population aged between 16 and 64 years. J Intellect Disabil Res 45:495–505
Cooper SA, Smiley E, Morrison J, Allan L, Williamson A, Finlayson J, Jackson A, Mantry D (2007) Psychosis and adults with intellectual disabilities. Prevalence, incidence, and related factors. Soc Psychiatry Psychiatr Epidemiol 42:530–536
Mavrogiorgou P, Schabos O, Juckel G, Hoffmann K (2015) Zwangsstörung bei Menschen mit intellektueller Entwicklungsstörung. (Obsessive compulsive symptoms in persons with intellectual disabilities). Fortschr Neurol Psychiatr 83:314–320
Emerson E, Kiernan C, Alborz A, Reeves D, Mason H, Swarbrick R, Mason L, Hatton C (2001) The prevalence of challenging behaviors: a total population study. Res Dev Disabil 22:77–93
Deb S, Thomas M, Bright C (2001) Mental disorder in adults with intellectual disability. 2: the rate of behaviour disorders among a community-based population aged between 16 and 64 years. J Intellect Disabil Res 45:506–514
Raghavan R, Marshall M, Lockwood A, Duggan L (2004) Assessing the needs of people with learning disabilities and mental illness: development of the learning disability version of the cardinal needs schedule. J Intellect Disabil Res 48:25–36
McCausland Guerin A, Tyrrell J, Donohore C, O’Donoghue I, Dodd P (2010) Self-reported needs among older persons with intellectual disabilities in an Irish community-based service. Res Dev Disabil 31:381–387
Strydom A, Hassiotis A, Livingston G (2005) Mental health and social care needs of older people with intellectual disabilities. J Appl Res Intellect 18:229–235
Meins W (1988) Psychopharmakagebrauch bei geistig behinderten Erwachsenen. (Use of psychotropic drugs in mentally handicapped adults). Psychiat Prax 6:218–222
Matson JL, Neal D (2009) Psychotropic medication use for challenging behaviors in persons with intellectual disabilities: an overview. Res Dev Disabil 30:572–586
Mack S, Jacobi F, Gerschler A, Strehle J, Höfler M, Busch MA, Maske UE, Hapke U, Seoiffert I, Gäbel W, Zielasek J, Maier W, Wittchen HU (2014) Self-reported utilization of mental health services in the adult German population—evidence for unmet needs? Results of the DEGS1-mental health module (DEGS1-MH). Int J Method Psych 23:289–303
Bertelli MO, Rossi M, Scuticchio D, Bianco A (2015) Diagnosing psychiatric disorders in people with intellectual disabilities: issues and achievements. AMHID 9:230–242
Lennox N, Taylor M, Rey-Conde T, Bain C, Purdle DM, Boyle F (2005) Beating the barriers: recruitment of people with intellectual disability to participate in research. J Intellect Disabil Res 49:296–305
Bjelogrlic-Laakso N, Aaltonen S, Dorn T, Arvio M (2014) Need for special units for the management of neuropsychiatric disorders in people with intellectual disabilities. Acta Psychiatr Scan 130:77–79
Healy E, McGuire BE, Evans DS, Carley SN (2009) Sexuality and personal relationships for people with an intellectual disability. Part I: service user perspectives. J Intellect Disabil Res 53:905–912
Evans DS, McGuire BE, Evans DS, Healy E, Carley SN (2009) Sexuality and personal relationships for people with an intellectual disability. Part II: staff and family carer perspectives. J Intellect Disabil Res 53:913–921
Raghavan R, Patel P (2010) Ethical issues of psychotropic medication for people with intellectual disabilities. AMHID 4:34–38
Acknowledgments
This work is part of the study “Mental health care provision for adults with mental retardation and a psychiatric diagnosis (MEMENTA)” which has been funded by the German Federal Ministry for Education and Research (Grant number 01GY1134). We are grateful for the work of all interviewers and for the German Federal Ministry for Education and Research (BMBF) for their financial support. We appreciate the great support of participating ID services and all persons with ID and their family members for their participation in the MEMENTA-Study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare to have no conflict of interests.
Rights and permissions
About this article
Cite this article
Schützwohl, M., Koch, A., Koslowski, N. et al. Mental illness, problem behaviour, needs and service use in adults with intellectual disability. Soc Psychiatry Psychiatr Epidemiol 51, 767–776 (2016). https://doi.org/10.1007/s00127-016-1197-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-016-1197-4