Abstract
Purpose
Most people with mental health problems do not use mental health services, resulting in poor psychiatric outcomes and greater illness burden. Although perceiving the need for mental health care was identified to be a key factor for service use, factors that explain differences in perceived need for mental health care are incompletely understood. The present paper investigates the role of illness representations in predicting perceived need for mental health care.
Methods
In a community sample of 202 persons currently distressed by symptoms related to mental illness, illness representations were assessed using the Brief Illness Perception Questionnaire and perceived need for mental health care was measured by the Self-Appraisal of Illness Questionnaire. Multiple linear regression models were used to determine the association between a person’s illness representations and the level of perceived need for mental health care.
Results
Two illness representations were positively associated with perceived need for mental health care: the belief that treatment could improve the current mental health problem and the attribution of experienced symptoms to a mental health problem. Increased perceived need for care was related to current mental health service use.
Conclusions
Interventions that aim to increase mental health service use could focus on people’s attitudes toward mental health treatment and enable people to recognize symptoms as a mental illness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mental illness and substance use disorders are among the leading causes of disease burden accounting for 7.3 % of worldwide disability-adjusted life years (DALYs) and 12.3 % of DALYs in high-income countries [1]. This can partly be attributed to widespread under-treatment due to low help-seeking behavior [2–5]. Every year approximately 30 % of the European population suffers from a mental illness, and even though treatment is available, 50 % of serious cases and 75 % of moderate or mild cases go undiagnosed and untreated, resulting in more severe outcomes and greater illness burden [6–11]. To reduce the burden associated with mental illness, it is crucial to detect factors that increase help-seeking behavior and adherence to treatment.
Help-seeking for a health problem can be defined as a “problem-focused, planned behavior” [12]. The multi-stage process starts when symptoms are first recognized by the individual, followed by the definition of the health problem and as a result, the intention to seek help to cope with the health threat. Accordingly, previous research identified low perceived need for mental health care as a key barrier for initiating help-seeking for mental health problems [13–15]. But even if a person perceives the need for treatment, attitudinal, structural, and stigma-related barriers may hinder treatment seeking [13]. Perceiving a need for mental health care is not only linked to psychopathology but also associated with personal characteristics and the social context [2, 15–18]. These previous studies provide important insights into single variables as correlates of perceived need for treatment. To increase explanatory power, research has applied comprehensive behavioral models to help-seeking for mental health problems [19–25]. One of these behavioral models is the self-regulatory model (SRM; [26]), which is particularly useful for our purposes as outlined in more detail below.
The SRM has been used to explain differences in illness-related behaviors and beliefs, including treatment seeking and adherence among people with physical health problems [27, 28]. Moreover, first interventions designed to change illness representations in order to improve illness-related behavior were successful [29, 30]. In general, the model is based on viewing an individual as an active problem solver who will, when faced with a health threat, try to identify and understand the problem, and consequently find solutions for it. It describes a dynamic, iterative process, which starts when first symptoms are recognized and continues until a desired health state is reached. The decision for a coping strategy (e.g., to seek help or wait for the problems to solve themselves) is based on illness representations, which are best described as an individual’s understanding, interpretation and evaluation of the health threat [26, 31]. While the original model included five cognitive illness representations, consecutive research additionally identified two emotional illness representations and two factors covering illness comprehensibility and causal beliefs [26, 32, 33]. The cognitive representations contain the identity of the illness (recognition of symptoms and attribution to a mental illness), perceived consequences, expected timeline, and the perceived level of how and to what extent the illness can be controlled (personal control and control through treatment); emotional components are the level of concern and experienced emotions due to the illness; the level of understanding of the symptoms is covered by the illness comprehensibility, and the belief of what caused the symptoms is described by the causal representation [34].
Reviewing several illness behavior models, Lobban et al. [32] found the SRM to be a promising framework to be applied to mental diseases. Their statement was based on the fact that the SRM considers cognitive and emotional components, its successful application to a variety of physical diseases, the conformity with previous mental illness research, and the possibility of adapting the model to a mental health context (e.g., by identifying additional illness representations). In line with this, some studies applied the SRM to people with different mental health problems, including schizophrenia [35], psychotic disorders [36–38], anorexia [39], and depression [40, 41]. These studies found illness representations to be associated with quality of life, emotional burden, medication adherence, return to work expectations, and overall functioning. In summary, sufficient evidence was found for the SRM being applicable to mental illness. However, to date no study has used the SRM to explain differences in treatment seeking or perceived need for mental health care. Illness representations could be a meaningful target in interventions trying to increase help-seeking rates among people distressed by mental health problems.
Hypotheses
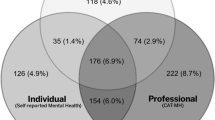
Using a community sample of people with elevated psychiatric symptom levels and current distress due to a mental illness, we expected the illness representations identity, consequences, timeline, treatment control, concern, emotions, and comprehensibility to be positively associated with perceived need for mental health care, while an inverse association was expected for personal control (hypothesis 1). Higher perceived need was expected to be associated with current mental health service use (hypothesis 2), and perceived treatment barriers (stigma and non-stigma related) to reduce the positive association between perceived need and service use (hypothesis 3; Fig. 1).
Methods
Design and participants
All data were derived from the Epidemiology survey of the ZInEP-study (Zurich Program for Sustainable Development of Mental Health Services) which assessed the prevalence of common mental diseases and mental health service use in the Canton of Zurich, Switzerland (for details on the study design see [42]). In a first step, a random sample of people aged 20–41 years was drawn from the Zurich population register, and telephone screening interviews (N = 9.829) were conducted. During the telephone interviews, the Global Severity Index (GSI) score of participants was obtained using the Symptom Checklist-27 (SCL-27; [43]). A 75th percentile cutoff of SCL-27 scores was used to stratify the sample into low and high scorers, resulting in two random samples (low scorers N = 600, high scorers N = 900). This sample was interviewed with regard to psychopathological syndromes/disorders in a comprehensive face-to-face interview. Subsequently, a sub-sample (N = 227) was selected based on paranoia and/or psychoticism scores assessed during the telephone screening interviews. This sub-sample comprised one group with increased (top quintile) paranoia and/or psychoticism symptoms (N = 190), and one group with values below the top quintile for both paranoia and psychoticism symptoms (N = 37). Both groups participated in additional examinations and assessments and form the basis for our analysis. For the purpose of this paper, participants reporting no current distress due to a mental disorder (cutoff: <50 on a scale ranging from 0 to 100, N = 12) were not included in the analysis. Additionally, subjects with missing data (N = 13) were excluded, yielding a final sample of 202 participants.
Measures
Illness representations
The Brief Illness Perception Questionnaire (B-IPQ) was used to assess illness representations of a mental disease or symptoms related to mental health problems [34]. The scale comprises eight questions ranging from 0 to 10 capturing cognitive representations of the experienced disease (item 1: consequences, item 2: timeline, item 3: personal control, item 4: treatment control, item 5: identity), emotional representations (item 6: illness concern, item 8: emotional response), and comprehensibility of the illness (item 7). All 8 illness representations were used as predictor variables (hypothesis 1).
Perceived need for mental health care
To assess perceived need for mental health care, the Need for Treatment sub-scale of the Self-Appraisal of Illness Questionnaire (SAIQ) was used [44]. Participants were asked to rate six items on four-point Likert scales, with higher mean scores indicating more perceived need for mental health care (Cronbach’s alpha in our sample: 0.89). Their mean score was firstly used as an outcome variable (hypothesis 1), and secondly as a predictor variable (hypotheses 2 and 3).
Barriers to help-seeking
The Barriers to Access to Care Evaluation Scale (BACE), a 30-item questionnaire, was used to assess stigma- and non-stigma-related barriers to help-seeking for mental illness [45]. Participants were asked to rate the extent of agreement toward 30 potential barriers to help-seeking regarding a mental health problem from 1 (not at all) to 4 (a lot). All answers within each of the two sub-scales (stigma/non-stigma) were used to create two continuous variables expressing the mean level of perceived stigma- (12 items, Cronbach’s alpha in our sample: 0.89) and non-stigma (18 items, Cronbach’s alpha in our sample: 0.86)-related barriers of help-seeking for mental illness. Both variables were used as potential moderator variables (hypothesis 3).
Current service use
Participants were asked about their mental health treatment status (yes, currently; yes, more than 12 months ago; no, never). For the purpose of this paper, a binary variable of current service use (yes/no) was created and used as an outcome variable (hypotheses 2 and 3).
Covariates
Symptom severity, age, and gender were considered as potential confounding variables. Symptom severity was assessed during the screening interviews using the SCL-27 [43]. Participants were asked to rate symptoms associated with mental illness during the last 7 days on a five-point Likert scale. A global severity index (GSI) was created by calculating the mean score across all items.
Statistical analysis
Data were checked for normality by visual inspection and additional Kolmogorov–Smirnov tests, and non-parametric alternatives were used if violations of normality were found. First, descriptive statistics were conducted and Pearson’s correlations between perceived need for mental health care and the independent variables were calculated. To assess internal consistency, Cronbach’s alpha values were obtained for all included instruments. SPSS version 22 was used for all analyses.
To test hypothesis 1, three multiple linear regression models were run to predict perceived need for mental health care. The first block included the illness representations, and the second and third block additionally included symptom level, age, and gender as covariates. To examine hypothesis 2, differences in perceived need for mental health care between the two treatment groups (current service use: no, yes) were compared using Mann–Whitney U tests. To test hypothesis 3, differences in perceived barriers (stigma and non-stigma related) between the two treatment groups (no, yes) and a lower and a higher perceived need for care group (75th percentile cutoff: 2.75) were compared using Mann–Whitney U tests. A moderator analysis was performed testing for an interaction between perceived need and perceived barriers (stigma/non-stigma related) with treatment status as the outcome variable.
Results
Descriptive and bivariate analysis
Table 1 presents the characteristics of participants and the results of the bivariate analysis. Our study population was two-thirds female, was aged 31.1 years on average, and was roughly equally split in terms of current mental health treatment. With regard to symptom severity, low to moderate GSI-scores were observed. Perceived need for mental health care was moderate, and perceived barriers (stigma and non-stigma related) were low. Illness representations indicated moderate to high perceived personal control, treatment control, and illness comprehensibility. All illness representations, apart from the comprehensibility dimension, were significantly correlated with perceived need for mental health care, with the highest coefficients found for consequences, identity, concern, and emotions. GSI-scores, age, and current service use were also related to perceived need for mental health care. Increased stigma-related barriers were associated with higher perceived need for mental healthcare.
Hypothesis 1—illness representations as predictors of perceived need for treatment
More perceived treatment control and higher recognition and attribution of symptoms to a mental illness (identity) were significantly associated with increased perceived need for mental health care (Table 2). Both illness representations remained significant predictors after controlling for symptom level (GSI-score), age, and gender in the following steps of the regression analysis. Higher symptom levels were related to more perceived need for treatment. The model explained about half of perceived need’s variance. No indication of multicollinearity was detected in any of models (variance inflation factor <5 and tolerance >0.10).
Hypotheses 2 and 3—differences in perceived need levels by treatment status and moderator analysis
Significantly higher levels of perceived need for mental health care were found among participants currently treated for a mental health problem, compared with those without treatment (Table 3). Participants who were currently in treatment, compared to those who were not, reported lower levels of non-stigma-related barriers at a trend level (Table 3). Subjects perceiving high need for mental health care, compared to those perceiving low need, reported higher levels of stigma-related barriers at a trend level (Table 4). Similar findings were obtained from the bivariate analysis (Table 1) which found a significant positive correlation between stigma-related barriers and perceived need for mental health care.
In two logistic regression models, interactions of perceived need for mental health care with stigma-related barriers and of perceived need with non-stigma related did not predict current service use (Table 5).
Discussion
In this study, we applied the SRM to a community sample of participants with elevated symptom levels and current distress due to mental illness to explain differences in levels of perceived need for mental health care. Two illness representations, namely the belief that treatment could help to improve the current mental health problems and a higher attribution of experienced symptoms to mental health problems, were positively associated with perceived need for mental health care. The hypothesized positive association between perceived need for mental health care and current service use was confirmed. No evidence was found for the expected interaction effect of perceived need for mental health care and perceived treatment barriers (stigma and non-stigma-related) on service use.
Previous studies focusing on differences in perceived need and treatment seeking are consistent with our findings. In a recent review, Gulliver and colleagues [46] found that deficits in symptom recognition reduced help-seeking among adolescents and young adults. Another study found negative previous treatment experience and a lack of confidence in depression treatment to be associated with lower levels of perceived need for mental health care in a sample of young adults with moderate to severe symptoms of depression [18]. Other studies further highlight the importance of positive treatment beliefs in order to increase perceived need for mental health care [47, 48]. Interestingly, while previous research found female gender to be associated with increased perceived need for mental health problems, we could not replicate this association in our study [16, 49].
Contrary to our third hypothesis, perceived treatment barriers did not weaken the association between perceived need for mental health care and mental health service use. This finding differs from previous studies that found perceived stigma and non-stigma-related barriers to be important factors hindering help-seeking once the need for mental health care is perceived [13, 14]. The relatively low symptom levels among our study population could explain our negative finding. Possibly, perceived stigma- and non-stigma-related barriers become more relevant with increased symptom severity. Our findings partially support this by showing higher perceived stigma-related barriers among people reporting high perceived need for mental health care. Another consideration is the relative lack of financial barriers to mental health services in Switzerland.
A major strength of the present study is the use of a community sample of people currently distressed by symptoms related to mental illness, rather than a clinical sample. This design allowed us to study individuals with elevated symptom levels and current distress, whether or not they received current mental health care. In addition, we applied a comprehensive behavioral model and controlled for symptoms and socio-demographic variables in our analyses. However, limitations of our study need to be considered. First, the data are cross-sectional and causality cannot be inferred. Second, we did not control for the onset and duration of experienced mental illness. Illness representations are likely to differ based on the length of time the current problems are already present [33]. For example, a person who suffers from mental illness symptoms for a longer time period might have tried and failed with several coping strategies, and thus might be more prone to perceive a need for mental health care, compared to persons who have just started to recognize their symptoms. Third, the measure used to assess illness representations was initially designed for people with a physical illness and thus the included illness representations might not be comprehensive [33].
Our findings can be interpreted in the context of mental health literacy (MHL). First introduced by Jorm and colleagues, MHL is defined as “knowledge and beliefs about mental disorders which aid their recognition, management or prevention” [50], p. 182]. The correct recognition of symptoms as a mental illness and a positive picture and knowledge of treatment options are crucial parts of MHL. Interestingly, similar to the two illness representation identified in the present study, higher MHL was found to positively influence help-seeking behavior among people who experience mental illness [51, 52].
In conclusion, we found that both the positive belief in effective treatment for the experienced symptoms and the correct attribution of these symptoms to a mental illness were associated with higher levels of perceived need, after controlling for symptom severity, age, and gender. Interventions focusing on improving attitudes toward mental health care and enabling people to correctly identify symptoms as a mental health problem are therefore likely to enhance mental health help-seeking.
References
World Health Organization (2012) DALY estimates for 2000–2012. http://www.who.int/healthinfo/global_burden_disease/estimates/en/index2.html. Accessed 15 Dec 2014
Corrigan PW (2004) How stigma interferes with mental health care. Am Psychol 59(7):614–625
Swift JK, Greenberg RP (2012) Premature discontinuation in adult psychotherapy: a meta-analysis. J Consult Clin Psychol 80(4):547–559
Wang PS, Aguilar-Gaxiola S, Alonso J et al (2007) Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet 370(9590):841–850
Wells JE, Browne MO, Aguilar-Gaxiola S et al (2013) Drop out from out-patient mental healthcare in the World Health Organization’s World Mental Health Survey initiative. Br J Psychiatry 202(1):42–49
Boonstra N, Klaassen R, Sytema S et al (2012) Duration of untreated psychosis and negative symptoms—a systematic review and meta-analysis of individual patient data. Schizophr Res 142(1):12–19
Ghio L, Gotelli S, Marcenaro M et al (2014) Duration of untreated illness and outcomes in unipolar depression: a systematic review and meta-analysis. J Affect Disord 152–154:45–51
Kessler RC, Demler O, Frank RG, Olfson M (2005) Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med 352(24):2515–2523
Penttilä M, Jääskeläinen E, Hirvonen N et al (2014) Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. Br J Psychiatry 205(2):88–94
The WHO World Mental Health Survey Consortium (2004) Prevalence, severity, and unmet need for treatment of mental disorders in the world health organization world mental health surveys. JAMA 291(1):2581–2590
Wittchen HU, Jacobi F (2005) Size and burden of mental disorders in Europe—a critical review and appraisal of 27 studies. Eur Neuropsychopharmacol 15(4):357–376
Cornally N, McCarthy G (2011) Help-seeking behaviour: a concept analysis. Int J Nurs Pract 17(3):280–288
Andrade LH, Alonso J, Mneimneh Z et al (2014) Barriers to mental health treatment: results from the WHO World Mental Health surveys. Psychol Med 44(6):1303–1317
Mojtabai R, Olfson M, Sampson NA et al (2011) Barriers to mental health treatment: results from the National Comorbidity Survey Replication. Psychol Med 41(8):1751–1761
Mojtabai R, Olfson M, Mechanic D (2002) Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Arch Gen Psychiatry 59(1):77–84
Meadows G, Burgess P, Bobevski I et al (2002) Perceived need for mental health care: influences of diagnosis, demography and disability. Psychol Med 32(2):299–309
Rüsch N, Müller M, Ajdacic-Gross V et al (2014) Shame, perceived knowledge and satisfaction associated with mental health as predictors of attitude patterns towards help-seeking. Epidemiol Psychiatr Sci 23(2):177–187
Van Voorhees BW, Fogel J, Houston TK et al (2006) Attitudes and illness factors associated with low perceived need for depression treatment among young adults. Soc Psychiatry Psychiatr Epidemiol 41(9):746–754
Burns T, Eichenberger A, Eich D et al (2003) Which individuals with affective symptoms seek help? Results from the Zurich epidemiological study. Acta Psychiatr Scand 108(6):419–426
Landolt K, Rössler W, Burns T et al (2012) The interrelation of needs and quality of life in first-episode schizophrenia. Eur Arch Psychiatry Clin Neurosci 262(3):207–216
Landolt K, Rössler W, Burns T et al (2012) Unmet needs in patients with first-episode schizophrenia: a longitudinal perspective. Psychol Med 42(7):1461–1473
Elwy AR, Yeh J, Worcester J, Eisen SV (2011) An illness perception model of primary care patients’ help seeking for depression. Qual Health Res 21(11):1495–1507
Mak HW, Davis JM (2013) The application of the theory of planned behavior to help-seeking intention in a Chinese society. Soc Psychiatry Psychiatr Epidemiol 49(9):1501–1515
Schomerus G, Matschinger H, Angermeyer MC (2009) Attitudes that determine willingness to seek psychiatric help for depression: a representative population survey applying the theory of planned behaviour. Psychol Med 39(11):1855–1865
Schomerus G, Appel K, Meffert PJ et al (2013) Personality-related factors as predictors of help-seeking for depression: a population-based study applying the behavioral model of health services use. Soc Psychiatry Psychiatr Epidemiol 48(11):1809–1817
Leventhal H (1984) Illness representations and coping with health threats. In: Singer J, Singer A (eds) A handbook of psychological health. Lawrence Erlbaum Associates, Hillsdale, pp 219–252
Hagger MS, Orbell S (2003) A meta-analytic review of the common-sense model of illness representations. Psychol Health 18(2):141–184
Petrie KJ, Jago LA, Devcich DA (2007) The role of illness perceptions in patients with medical conditions. Curr Opin Psychiatry 20(2):163–167
Broadbent E, Ellis CJ, Thomas J et al (2009) Further development of an illness perception intervention for myocardial infarction patients: a randomized controlled trial. J Psychosom Res 67(1):17–23
Petrie KJ, Cameron LD, Ellis CJ et al (2002) Changing illness perceptions after myocardial infarction: an early intervention randomized controlled trial. Psychosom Med 64(4):580–586
Leventhal H, Benyamini Y, Brownlee S et al (1997) Illness representations: theoretical foundations. Percept Health Illn 2:19–46
Lobban F, Barrowclough C, Jones S (2003) A review of the role of illness models in severe mental illness. Clin Psychol Rev 23(2):171–196
Petrie KJ, Broadbent E, Kydd R (2008) Illness perceptions in mental health: issues and potential applications. J Ment Health 17(6):559–564
Broadbent E, Petrie KJ, Main J, Weinman J (2006) The brief illness perception questionnaire. J Psychosom Res 60(6):631–637
Lobban F, Barrowclough C, Jones S (2004) The impact of beliefs about mental health problems and coping on outcome in schizophrenia. Psychol Med 34(7):1165–1176
Broadbent E, Kydd R, Sanders D, Vanderpyl J (2008) Unmet needs and treatment seeking in high users of mental health services: role of illness perceptions. Aust N Z J Psychiatry 42(2):147–153
Gómez-de-Regil L, Kwapil TR, Barrantes-Vidal N (2014) Illness perception mediates the effect of illness course on the quality of life of Mexican patients with psychosis. Appl Res Qual Life 9(1):99–112
Watson PWB, Garety PA, Weinman J et al (2006) Emotional dysfunction in schizophrenia spectrum psychosis: the role of illness perceptions. Psychol Med 36(6):761–770
Holliday J, Wall E, Treasure J, Weinman J (2005) Perceptions of illness in individuals with anorexia nervosa: a comparison with lay men and women. Int J Eat Disord 37(1):50–56
Fortune G, Barrowclough C, Lobban F (2004) Illness representations in depression. Br J Clin Psychol 43(4):347–364
Løvvik C, Øverland S, Hysing M et al (2014) Association between illness perceptions and return-to-work expectations in workers with common mental health symptoms. J Occup Rehabil 24(1):160–170
Ajdacic-Gross V, Müller M, Rodgers S et al (2014) The ZInEP epidemiology survey: background, design and methods. Int J Methods Psychiatr Res 23(4):451–468
Hardt J, Egle UT, Kappis B et al (2004) Symptom checklist SCL-27-results of a representative German survey. Psychother Psychosom Med Psychol 54(5):214–223
Marks KA, Fastenau PS, Lysaker PH, Bond GR (2000) Self-Appraisal of Illness Questionnaire (SAIQ): relationship to researcher-rated insight and neuropsychological function in schizophrenia. Schizophr Res 45(3):203–211
Clement S, Brohan E, Jeffery D et al (2012) Development and psychometric properties the Barriers to Access to Care Evaluation scale (BACE) related to people with mental ill health. BMC Psychiatry 12(1):36
Gulliver A, Griffiths KM, Christensen H (2010) Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry 10(1):113
Jorm AF (2012) Mental health literacy: empowering the community to take action for better mental health. Am Psychol 67(3):231–243
Ten Have M, de Graaf R, Ormel J, Vilagut G (2010) Are attitudes towards mental health help-seeking associated with service use? Results from the European study of epidemiology of mental disorders. Soc Psychiatry Psychiatr Epidemiol 45(2):153–163
Rabinowitz J, Gross R, Feldman D (1999) Correlates of a perceived need for mental health assistance and differences between those who do and do not seek help. Soc Psychiatry Psychiatr Epidemiol 34(3):141–146
Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P (1997) “Mental health literacy”: a survey of the public’s ability to recognise mental disorders and their believes about the effectiveness of treatment. Med J Aust 166:182–186
Goldney RD, Fisher LJ, Wilson DH, Cheok F (2002) Mental health literacy of those with major depression and suicidal ideation: an impediment to help seeking. Suicide Life Threat Behav 32(4):394–403
Jorm AF (2000) Mental health literacy public knowledge and beliefs about mental disorders. Br J Psychiatry 177(5):396–401
Acknowledgments
We are grateful to all participants. ZInEP was supported by a private donation. The donor had no further role in the experimental design, the collection, analysis, and interpretation of data, the writing of this report or the decision to submit this paper for publication. The ZInEP Epidemiology Survey, in particular research in the Center for Neurophysiology and Sociophysiology, was supported by the Swiss National Science Foundation (grant # 3247B0-122071). The population and education data were provided by the Swiss Federal Statistical Office.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethics
All subjects gave their informed consent prior to their participation. The study was approved by the Cantonal ethics commission Zurich (Reference number: 2009-0061/3).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oexle, N., Ajdacic-Gross, V., Müller, M. et al. Predicting perceived need for mental health care in a community sample: an application of the self-regulatory model. Soc Psychiatry Psychiatr Epidemiol 50, 1593–1600 (2015). https://doi.org/10.1007/s00127-015-1085-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-015-1085-3