Abstract
Aims/hypothesis
The aim of this study was to estimate the incidence of type 2 diabetes (primary objective) and hospitalisation for cardiovascular events (secondary objective) in women with previous gestational diabetes mellitus (GDM) and in those with normal glucose tolerance (NGT) in pregnancy, and to evaluate the role of stillbirth in differentiating the risks.
Methods
This was a population-based cohort study using administrative data and involving 12 local health authorities. Women with GDM (n = 3,851) during the index period from 2002 to 2010 were propensity matched with women with NGT (n = 11,553). Information was collected on type 2 diabetes development and hospitalisation for cardiovascular events.
Results
During a median follow-up of 5.4 years, the incidence rate per 1,000 person-years of type 2 diabetes was 2.1 (95% CI 1.8, 2.5) in women without GDM and 54.0 (95% CI 50.2, 58.0) among women with GDM and pregnancy at term (incidence rate ratio [IRR] 26.9; 95% CI 22.1, 32.7 compared with NGT and pregnancy at term). A history of stillbirth increased the risk of type 2 diabetes development by about twofold, irrespective of GDM status. No significant interaction between stillbirth and GDM on type 2 diabetes risk was found. GDM was associated with a significantly higher risk of cardiovascular events compared with NGT (IRR 2.4; 95% CI 1.5, 3.8).
Conclusions/interpretation
Pregnancy complicated by GDM and ending in stillbirth represents an important contributory factor in determining type 2 diabetes development. Women with GDM are at a high risk of future cardiovascular events. Women with pregnancy complicated by GDM and stillbirth deserve careful follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of type 2 diabetes mellitus is reaching alarming levels all over the world [1], with relevant social and economic impact [2]. Major scientific societies emphasise the need to prioritise the implementation of prevention programmes [3, 4], and the latest guidelines of the American Heart Association for the prevention of cardiovascular disease in women underline the role of gestational diabetes as an important cardiovascular risk factor, in addition to its strong predictive role in the development of diabetes [5].
Gestational diabetes mellitus (GDM) is currently defined as glucose intolerance with onset or first identification during pregnancy [6]. GDM is a dangerous condition for the mother and fetus during pregnancy or at the time of delivery [7–9].
However, the negative consequences of GDM are not restricted to the period of pregnancy, since women suffering from this condition are at increased risk of the onset of type 2 diabetes, metabolic syndrome and cardiovascular disease in the years following pregnancy. Despite specific follow-up recommendations for the identification of any dysglycaemia after pregnancy [3], only a very low percentage of women follow them [10].
Several studies have analysed the association between GDM and long-term maternal cardiovascular morbidity [11–14]; nevertheless, methodological shortcomings make it difficult to generalise the results. In particular, some studies were based on patient self-reported medical history [11, 13], or were conducted in selected populations [15].
Women with GDM also have a significantly higher relative risk of stillbirth compared with women without GDM [16]. Despite this, the role of stillbirth in determining type 2 diabetes development risk has seldom been investigated [17]. GDM and pregnancy loss share many predisposing factors which are also common risk factors for metabolic syndrome. Insulin resistance, dyslipidemia, coagulation dysfunction and hyperglycaemia are some of the possible factors linked to both pregnancy loss and diabetes [18]. In our study, we have hypothesised that among GDM pregnancies, stillbirth could represent an indicator of more severe conditions that lead to an increased risk of type 2 diabetes and cardiovascular disease (CVD).
We conducted a study using administrative data with the primary objective of estimating the incidence of type 2 diabetes in women with previous GDM and those with normal glucose tolerance (NGT) in pregnancy, and evaluating the role of stillbirth in differentiating the risks. The secondary endpoint of the study was to estimate the risk of cardiovascular events, although a low rate of development of cardiovascular disease was reasonably expected.
Methods
We conducted a population-based cohort study using a record linkage analysis of hospital discharge records, prescription databases and the civil registry, including data on 4.1 million citizens in 12 local health authorities in Puglia, Italy.
Data sources
All Italian citizens have equal access to healthcare services and are cared for by a general practitioner as part of the National Health System. Hospital and pharmaceutical services are provided free or at a minimum charge. Prescription databases provide data on all community prescriptions reimbursed by the National Health System, with drugs coded according to the Anatomical Therapeutic Chemical (ATC) classification system [19]. Hospital discharge records cover all admissions in both public and private hospitals. They include information on primary diagnoses and up to five coexisting conditions, performed procedures (diagnostic and therapeutic interventions), date of hospital admission and discharge, and in-hospital death. All diagnoses are coded according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) (www.icd9data.com/2007/Volume1). Data sources, such as hospital discharge records and prescription databases, and the reliability of record linkage in producing epidemiological information have been validated and described elsewhere [20–23]. All security and protection measures for patient data were performed according to national law [24].
Study design
We identified women diagnosed with GDM during the index period from 1 January 2002 to 31 December 2010. Until 2010, GDM was diagnosed according to ADA criteria [6, 25, 26]. Risk assessment for GDM was undertaken at the first prenatal visit. Women with clinical characteristics consistent with a high risk of GDM (obesity, personal history of GDM, previous macrosomia, glycosuria or a strong family history of diabetes) underwent glucose testing as soon as feasible. If they were found not to have GDM at the initial screening, they were re-tested between 24 and 28 weeks of gestation. Women at an average risk had a glucose test at 24–28 weeks of gestation. Those with a low risk status (age <25 years, normal prepregnancy weight, member of an ethnic group with a low prevalence of GDM, no known diabetes in first-degree relatives, no history of abnormal glucose tolerance and no history of poor obstetric outcome) required no glucose testing. Individuals were considered to be affected by GDM if they were discharged from the Department of Obstetrics and Gynaecology with a specific diagnosis of GDM (ICD-9-CM code 648.8x: abnormal glucose tolerance) or if they started insulin therapy during the pregnancy (ATC code A10A). Women treated with glucose-lowering drugs before pregnancy were excluded from the analysis. We considered all women with GDM whose pregnancies have ended in a live birth (ICD-9-CM codes 650, 651.x, 652.x, 659.5 and 669.7x) or a stillbirth (ICD-9-CM code 634.x). The date of delivery or stillbirth was considered the patient’s index date. If a woman had more than one pregnancy ending in a live birth or stillbirth during the period of study, then the first one was considered. All pregnant women who did not have a diagnosis of GDM or diabetes mellitus were considered controls.
Outcome variables
The primary outcome of interest was a diagnosis of type 2 diabetes. Secondary outcomes were hospitalisation for cerebrovascular complications, acute myocardial infarction, peripheral vascular disease, heart failure, ischaemic heart disease (ICD-9-CM codes shown in electronic supplementary material [ESM] Table 1) occurring after the index pregnancy. Type 2 diabetes was defined as the presence of a specific diagnosis of type 2 diabetes (ICD-9-CM codes 250.x0 and 250.x2) at hospital discharge or exposure to at least three prescriptions of glucose-lowering agents (ATC code for insulin, A10A; ATC code for blood glucose-lowering drugs, excluding insulin, A10B) in the years following the index date. All patients were followed up from their index date to the development of diabetes, to the earliest hospitalisation for one of the established cardiovascular outcomes or to the end of the study period, providing a maximum follow-up of 8 years.
Possible confounding factors
To control for confounding factors, drugs taken for the prevention of conditions with a high cardiovascular risk or for hypertensive disorders were taken into account.
Individuals were considered to be affected by hypertension if they had received at least three prescriptions of antihypertensive agents (e.g. centrally acting antiadrenergic agents, α-blockers, thiazide-type diuretics, β-blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists) in the year previous to the index date. Current use of antithrombotic agents and statins was also identified. In line with previous studies [27], current use was defined as receiving a prescription for such drugs within the 3 months previous to an event or at the end of follow-up.
Statistical analyses
From the overall sample population of 2.1 million women, a sample of 267,740 women with a normal pregnancy or a pregnancy ending in stillbirth was identified. The entire cohort was divided into two subsamples according to the presence of GDM.
A 1:3 propensity score matching algorithm was used to enable an unbiased comparison between women with and without a diagnosis of GDM, [28, 29]. A logistic regression model including age, local health authority code, and use of antihypertensive and antithrombotic agents as covariates was used to predict the probability (propensity score) of having GDM. Statin was not considered a covariate in the propensity score matching analysis because the percentage use was very low and the between-group difference was not significant. An 8:1 greedy matching algorithm [29] was used to identify three matched controls for each woman with GDM according to their propensity scores. The adequacy of covariate balance in the matched sample was assessed via standardised mean differences between the two groups, with differences of less than 10% indicating a good balance [30]. Covariate balance in the matched sample was also assessed for those variables of interest which did not take part in the logistic model to predict the propensity score.
Characteristics of the study population are reported as percentages, mean (SD) or median (interquartile range). Incidence rates (IRs) with 95% CIs of type 2 diabetes onset and cardiovascular events per 1000 person-years were estimated for both cohorts. Cerebrovascular complications, acute myocardial infarction, peripheral vascular disease, heart failure, ischaemic heart disease and a composite cardiovascular endpoint were assessed; for the latter, the first occurrence of a cardiovascular event was considered. Risks were reported as incidence rate ratios (IRRs) along with their 95% CIs. For subgroup analyses according to sample characteristics, p values for interactions were also assessed.
The cumulative proportion of patients developing type 2 diabetes and cardiovascular events during follow-up according to the presence of GDM and pregnancy course (at term vs stillbirth) was estimated using an age-adjusted Cox model. Two-sided p values of <0.05 were considered statistically significant. All statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC, USA).
Results
From the initial cohort of 267,740 pregnant women, 15,404 were selected using propensity score matching: 3,851 women with pregnancies complicated by GDM and a sample of 11,553 controls (Fig. 1). Pre-matching characteristics differed widely between those with and those without GDM, but propensity score matching led to a satisfactory balance for all of the characteristics considered (ESM Table 2).
Overall, a total of 1.3 million person-years of observation was accumulated, with a median follow-up of 5.4 years (interquartile range 2.9–7.3 years) and a mean (SD) age of 35.7 (6.0) years. Among women with GDM, 1,732 (45.0%) were treated with insulin during pregnancy.
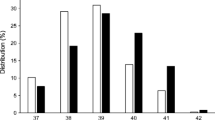
Overall, 674 stillbirths occurred: 48 (1.3%) in the GDM group and 626 (5.4%) in the non-GDM group. The presence of GDM was associated with a 26 times increased risk of developing type 2 diabetes compared with NGT (Table 1). Among women with GDM and a pregnancy ending in stillbirth, the IR of type 2 diabetes development was markedly higher, being almost twice (IR 115.00) that of women with GDM and pregnancy at term. The increased risk of type 2 diabetes development caused by stillbirth is similar (approximately double) in both GDM and non-GDM groups. Notably, even in the absence of GDM, the IR of type 2 diabetes development was also high among women with a history of stillbirth (IR 3.86). Among women with GDM, the diabetes incidence decreased steeply with age. The IR exceeding the upper limit of the 95% CI for the estimate relative to the whole population was observed in women aged <30 years (IR 72.60; 95% CI 57.31, 91.87 per 1000 person-years). Significant interactions were detected between the magnitudes of the risks conferred by GDM and age. The cumulative IRs of type 2 diabetes development resulting from GDM and stillbirth are reported in Fig. 2. Compared with women with a normal pregnancy, the risk of type 2 diabetes was 21.7 times higher for those with GDM and 46.9 times higher for those with GDM complicated by stillbirth. A history of stillbirth without GDM also increased the risk of type 2 diabetes by 1.8 times.
Cumulative incidence of women developing type 2 diabetes during follow-up, by gestational diabetes status and stillbirth. HRs for different experimental categories (women without GDM and with a live birth represent the reference class): HR (95% CI) 46.9 (29.1–75.5) for women with GDM and a stillbirth; HR 21.7 (17.8–26.5) for women with GDM and a live birth; HR 1.8 (1.0–3.3) for women without GDM and with a stillbirth. Dotted line, women with GDM and a stillbirth; dotted/dashed line, women with GDM and a live birth; continuous line, women without GDM and with a stillbirth; dashed line, women without GDM and with a live birth
As a hypertensive pregnancy (pre-eclampsia and pregnancy-induced hypertension) is also a risk factor for type 2 diabetes, we performed additional analyses to investigate a possible role for pre-eclampsia in the association between GDM and type 2 diabetes development. Data on pre-eclampsia were not available from hospital discharge records; however, they were deduced from antihypertensive drug use during the pregnancy, excluding women using those drugs before pregnancy. For women both with and without GDM, the presence of a hypertensive pregnancy did not significantly increase the risk of type 2 diabetes (IRR 1.28, 95% CI 0.90, 1.82; and IRR 1.99, 95% CI 0.63, 6.25, respectively), probably because of the small number of women with a hypertensive pregnancy (n = 257, of whom 121 were in the GDM group).
For the secondary outcome, 76 first episodes of cardiovascular events requiring hospitalisation were registered during the follow-up period. The presence of GDM was associated with a more than doubled risk of developing cardiovascular disease compared with NGT (IRR 2.43; 95% CI 1.53, 3.84). In particular, a diagnosis of GDM was associated with an excess risk of heart failure (IRR 3.34; 95% CI 1.36, 8.23), peripheral vascular disease (IRR 5.84; 95% CI 2.26, 15.06) and ischaemic heart disease (IRR 4.54; 95% CI 1.88, 10.96). Though not statistically significant, an excess risk was also documented for cerebrovascular events (IRR 1.98; 95% CI 0.84, 4.67). However, no excess risk was found for myocardial infarction (IRR 0.99; 95% CI 0.33, 2.98). Table 1 shows the IRs for cardiovascular events by GDM diagnosis and their IRRs according to the presence of a stillbirth.
The concomitant presence of GDM and stillbirth noticeably increased the risk of cardiovascular events (IRR 16.70; 95% CI 3.74, 74.65), while a stillbirth without GDM did not increase the risk of cardiovascular events (IR 0.89; 95% CI 0.29, 2.75 per 1000 person-years). Compared with women with a normal pregnancy, women with GDM and a pregnancy ending in stillbirth had a 17 times higher risk of cardiovascular events (HR, 17.1; 95% CI 6.1, 48.0), while for women with GDM and a full-term pregnancy the risk was two times higher (HR, 1.9; 95% CI 1.2, 3.2).
We performed additional analyses to investigate a possible link between the occurrence of type 2 diabetes and hospitalisation for CVD. We found that 11 women out of 76 developed type 2 diabetes before the occurrence of a cardiovascular event. Among these, 10 women had been diagnosed with GDM in the index pregnancy. We also performed a sensitivity analysis after excluding these women: the association between GDM and hospitalisation for CVD was confirmed (IRR 1.68, 95% CI 0.93, 3.02), although statistical significance was not reached because of the smaller number of events.
Discussion
Women with previous GDM are at an increased risk of type 2 diabetes onset and have a high cardiovascular risk. Surprisingly, the simultaneous presence of GDM and stillbirth strongly affects the risk of developing type 2 diabetes in a ‘real-world’ setting. Our study also provides a better understanding of the relationship between GDM and future cardiovascular events by showing that GDM complicated with stillbirth markedly increases the risk of future cardiovascular events.
The mechanisms underlying the link between stillbirth and the future development of type 2 diabetes are largely unknown. Possible explanations could include the established role of insulin resistance status in both pregnancy and type 2 diabetes. Immune disorders, hyperglycaemia and endothelial dysfunction could represent aetiological elements supporting a common mechanistic pathway for stillbirth and cardiovascular disease.
The association between GDM and future development of type 2 diabetes was reviewed by Bellamy et al [31] in a recent comprehensive systematic review and meta-analysis of 20 studies comprising a total of 675,455 women. They showed that women with a previous diagnosis of GDM have a sevenfold increased risk of developing type 2 diabetes in the future, compared with women with normoglycaemic pregnancies. Although the duration of follow-up was relatively short and the women studied were young, we found a much higher risk of type 2 diabetes onset (IRR 26.00) than that described in other reports, particularly for younger women (IRR 85.60). The most striking observation of our study is the very high type 2 diabetes incidence IR (115.00 per 1000 person-years) in women with a stillbirth whose pregnancy was complicated by GDM. The association of stillbirth and future onset of type 2 diabetes has not previously been specifically investigated in a population of women with and without GDM. Surprisingly, we found that one in two women with GDM and with pregnancies ending in stillbirth developed type 2 diabetes within 5 years. Stillbirth was associated with doubling of the risk of type 2 diabetes development in both GDM and non-GDM groups. In previous studies, evidence for an association between childbearing and the future development of diabetes has been contradictory, and in most the role of pregnancy loss in this association had not been considered. Kharazmi and colleagues [17] showed a modest association between childbearing and the development of type 2 diabetes. This modest increase in risk could be explained by factors such as BMI or pregnancy complications such as GDM. In their study, the association between stillbirth and diabetes was not statistically significant, possibly, as they have explained, because of the relatively small number of women who had a history of stillbirth. Our study design gave no information on parity, and increasing parity is associated with the future development of metabolic syndrome, which can include type 2 diabetes in its definition. Despite this, recent evidence demonstrates that adjusting for parity does not change the increased risk of diabetes in women with a history of stillbirth [17].
In agreement with previous studies, we showed that the incidence of cardiovascular disease is more than doubled after an index pregnancy complicated by GDM compared with a normal pregnancy. Analysis of single cardiovascular outcomes confirmed an excess risk for almost all endpoints, although statistical significance was not reached for cerebrovascular events because of the small number of events. Several studies have described different magnitudes of alterations to the cardiovascular system in women with GDM that can explain their predisposition to cardiovascular diseases [32–35]. Our study has confirmed previous evidence, while attempting to overcome the methodological shortcomings of the studies published to date. Other studies based on patient self-reported medical history [11, 13] attributed the increased cardiovascular risk not to GDM itself, but rather to the subsequent development of type 2 diabetes [12]. Alternatively, they were conducted in a single centre, thus making the results poorly generalisable [15]. Our study, for the first time, provides additional important information on the risk of cardiovascular events occurring after pregnancies complicated or not by GDM, and ending in stillbirth. With all the caveats related to the small number of events, we document that women with GDM whose pregnancies end in stillbirth have the highest risk of cardiovascular events. We could not distinguish between different risks for single cardiovascular outcomes, in relation to the presence of a stillbirth, because of the limited number of cases. Nonetheless, overall, the simultaneous presence of GDM and stillbirth resulted in a marked increase in the risk of cardiovascular disease. The cumulative IR of cardiovascular events according to the presence of GDM and stillbirth shows that in women with GDM the risk of cardiovascular events starts to increase very soon after a stillbirth. In this sense, it is unlikely that the association between stillbirth and CVD events are mediated by the onset of diabetes. Although there is a suggestion that the excess risk of CVD associated with GDM results from the excess risk of type 2 diabetes [12], the sensitivity analysis we performed after excluding women who developed type 2 diabetes before the occurrence of a cardiovascular event confirmed an association between GDM and hospitalisation for CVD, even if statistical significance was not reached because of the smaller number of events. However, data on cardiovascular endpoints are inconclusive and must be confirmed by larger studies.
Our study has both strengths and limitations. The main strength is the number of studied women with GDM, which is one of the largest reported in the literature.
A well-recognised limitation of using administrative data [36] is the lack of important prognostic indicators, such as vital signs, laboratory and diagnostic test results, and social and functional status. In particular, we could not consider BMI as an adjusting covariate in the performed analyses. Nevertheless, it is unlikely that BMI can account for the impressive increased risk of cardiovascular events and type 2 diabetes associated with GDM and stillbirth [37]. We performed a propensity score matching analysis including the local health authority code with the aim to remove a possible confounding centre effect resulting from different policies used to diagnose GDM. Other covariates included in the model were women’s age and the use of antihypertensive and antiplatelet agents. The last were chosen to avoid differences between groups in terms of taking medication typically taken to prevent cardiovascular disease or in pregnancies complicated by hypertensive disorders. Second, we used both specific ICD-9-CM codes and starting insulin therapy during pregnancy to identify women with GDM. It is thus possible that we selected the more severe cases of GDM, leading to higher estimates of type 2 diabetes incidence. However, the prevalence of insulin-treated GDM in our study was not dissimilar to that reported in other studies [38, 39]. Third, the lack of a validation study capable of confirming the optimal algorithm to identify stillbirths or spontaneous abortion in administrative databases may be responsible for misclassification [39]. Considering that a diagnosis of GDM is usually made at 24–28 weeks of gestation, the most severe GDM cases, leading to spontaneous abortion in the first weeks of pregnancy, could have been attributed to the non-GDM group, thus underestimating the real impact of GDM on type 2 diabetes and cardiovascular risk. Fourthly, we had no information on the rate of women tested or not tested for GDM, and we can assume incomplete coverage for GDM testing due to the limits of detection of the risk factor based screening criteria for GDM. Finally, because of the limited duration of the follow-up period we could not detect a substantial number of cardiovascular events; this was also affected by the mean age of the studied population.
Future research is needed to explore possible molecular mechanisms and genetic linkage explaining the future development of type 2 diabetes, and to discover the mechanisms responsible for the initial phase of subclinical cardiovascular alterations so that they can be detected at an early stage. Finally, an economic model predicting the cost savings resulting from the prevention of new cases of type 2 diabetes and cardiovascular events by identifying high risk women would be valuable.
In conclusion, GDM represents a condition that confers a high risk of future development of type 2 diabetes and cardiovascular disease. A history of stillbirth doubles the risk of type 2 diabetes development, irrespective of GDM status. Pregnancies complicated by GDM and ending in stillbirth are associated with an increased risk of cardiovascular events occurring soon after pregnancy. To address the multiple associated risks, women with a pregnancy complicated by GDM, particularly if ending in stillbirth, should have careful follow-up to prevent type 2 diabetes and cardiovascular diseases. Since most women who have had GDM do not comply with the recommendation to have a postpartum OGTT [10], healthcare professionals should increase their efforts to motivate mothers to attend screening programmes. The main clinical implications of our work are first, to take into account the higher metabolic and cardiovascular risks of subgroups of women with previous GDM, particularly when associated with stillbirth; second, to plan a more intensive and personalised cardiovascular and metabolic follow-up for these patients so as to alter the natural disease trajectory of GDM; and third, to confirm data on modifiable risk factors such as diet and physical exercise highlighted in a recent systematical review [40] with the aim of promoting an intensive lifestyle change to tackle unhealthy habits. Finally, as we have shown an important contributory factor for the future development of type 2 diabetes, current guidelines for detecting diabetes or impaired glucose tolerance after a pregnancy complicated by GDM should be changed to recommend a shorter interval between OGTTs in the follow-up period and for stillbirth to be considered when determining the risk.
Abbreviations
- ATC:
-
Anatomical Therapeutic Chemical
- CVD:
-
Cardiovascular disease
- GDM:
-
Gestational diabetes mellitus
- IR:
-
Incidence rates
- IRR:
-
Incidence rate ratio
- NGT:
-
Normal glucose tolerance
References
Whiting DR, Guariguata L, Weil C, Shaw J (2011) IDF Diabetes Atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract 94:311–321
ADA (2013) Economic costs of diabetes in the U.S. in 2012. Diabetes Care 36:1033–1046
ADA (2014) Standards of medical care in diabetes 2014. Diabetes Care 37:S14–S80
Canadian Diabetes Association (2013) Clinical Practice Guidelines Expert Committee. Reducing the risk of developing diabetes. Can J Diabetes 37:S16–S19
Mosca L, Benjamin EJ, Berra K et al (2011) Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. Circulation 123:1243–1262
Metzger BE, Coustan DR (1998) Summary and recommendations of the Fourth International Workshop-Conference on Gestational Diabetes Mellitus. The Organizing Committee. Diabetes Care 21(Suppl 2):B161–B167
Casey BM, Lucas MJ, Mcintire DD, Leveno KJ (1997) Pregnancy outcomes in women with gestational diabetes compared with the general obstetric population. Obstet Gynecol 90:869–873
Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS (2005) Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med 352:2477–2486
Landon MB, Spong CY, Thom E et al (2009) A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med 361:1339–1348
Kim C, Tabaei BP, Burke R et al (2006) Missed opportunities for type 2 diabetes mellitus screening among women with a history of gestational diabetes mellitus. Am J Public Health 96:1643–1648
Carr DB, Utzschneider KM, Hull RL et al (2006) Gestational diabetes mellitus increases the risk of cardiovascular disease in women with a family history of type 2 diabetes. Diabetes Care 29:2078–2083
Shah BR, Retnakaran R, Booth GL (2008) Increased risk of cardiovascular disease in young women following gestational diabetes mellitus. Diabetes Care 31:1668–1669
Dawson SI (2009) Glucose tolerance in pregnancy and the long-term risk of cardiovascular disease. Diabetes Res Clin Pract 85:14–19
Fraser A, Nelson SM, Macdonald-Wallis C, Cherry L, Butler E (2012) Associations of pregnancy complications with calculated cardiovascular disease risk and cardiovascular risk factors in middle age: the Avon longitudinal study of parents and children. Circulation 125:1367–1380
Kessous R, Shoham-Vardi I, Pariente G, Sherf M, Sheiner E (2013) An association between gestational diabetes mellitus and long-term maternal cardiovascular morbidity. Heart 99:1118–1121
Rosenstein MG, Cheng YW, Snowden JM, Nicholson JM, Doss AE, Caughey AB (2012) The risk of stillbirth and infant death stratified by gestational age in women with gestational diabetes. Am J Obstet Gynecol 4:309.e1–7
Kharazmi E, Lukanova A, Teucher B, Groß ML, Kaaks R (2012) Does pregnancy or pregnancy loss increase later maternal risk of diabetes? Eur J Epidemiol 27:357–366
Oliver-Williams CT, Heydon EE, Smith GC, Wood AM (2013) Miscarriage and future maternal cardiovascular disease: a systematic review and meta-analysis. Heart 99(22):1636–1644
World Health Organisation ATC Index with DDDs. Norway, Oslo: WHO Collaborating Centre for Drug Statistics Methodology. Available: http://www.whocc.no/atcddd. Accessed 29 Oct 2013
Macchia A, Romero M, D’Ettorre A, Mariani J, Tognoni G (2012) Temporal trends of the gaps in post-myocardial infarction secondary prevention strategies of co-morbid and elderly populations vs younger counterparts: an analysis of three successive cohorts between 2003 and 2008. Eur Heart J 33:515–522
De Berardis G, D’Ettorre A, Graziano G et al (2012) The burden of hospitalization related to diabetes mellitus: a population-based study. Nutr Metab Cardiovasc Dis 22:605–612
Winkler WE Comparative analysis of record linkage decision rules. Proceedings of Survey Research Methods Section. Am Stat Assoc 1992;829–834. Available: http://www.amstat.org/sections/srms/proceedings. Accessed 29 Oct 2013
De Berardis G, Lucisano G, D’Ettorre A et al (2012) Association of aspirin use with major bleeding in patients with and without diabetes. JAMA 307:2286–2294
Italian Republic. Determination of the Italian Medicines Agency of March 20, 2008 [in Italian]. Official Gazette of the Italian Republic. General Series No. 76; 31 March 31 2008
Carpenter MW, Coustan DR (1982) Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol 144:768–773
ADA (2004) Position statement gestational diabetes mellitus. Diabetes Care 27(Suppl 1):S88–S90
McAlister FA, Campbell NR, Duong-Hua M, Chen Z, Tu K (2006) Antihypertensive medication prescribing in 27,822 elderly Canadians with diabetes over the past decade. Diabetes Care 29:836–841
Yanovitzky I, Zanutto E, Hornik R (2005) Estimating causal effects of public health education campaigns using propensity score methodology. Eval Program Plann 28:209–220
Parsons LS. Reducing bias in a propensity score matched-pair sample using greedy matching techniques. In: Proceedings of the Twenty-Sixth Annual SAS Users Group International Conference. Cary, NC: SAS Institute. Available: http://www2.sas.com/proceedings/sugi26/p214-26.pdf. Accessed 29 Oct 2013
Austin PC, Grootendorst P, Anderson GM (2007) A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: a Monte Carlo study. Stat Med 26:734–753
Bellamy L, Casas JP, Hingorani AD, Williams D (2009) Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet 373:1773–1779
Volpe L, Cuccuru I, Lencioni C et al (2008) Early subclinical atherosclerosis in women with previous gestational diabetes mellitus. Diabetes Care 31:e32
Anastasiou E, Lekakis JP, Alevizaki M et al (1998) Impaired endothelium-dependent vasodilatation in women with previous gestational diabetes. Diabetes Care 21:2111–2115
Heitritter SM, Solomon CG, Mitchell GF, Skali-Ounis N, Seely EW (2005) Subclinical inflammation and vascular dysfunction in women with previous gestational diabetes mellitus. J Clin Endocrinol Metab 90:3983–3988
Vrachnis N, Augoulea A, Iliodromiti Z, Lambrinoudaki I, Sifakis S, Creatsas G (2012) Previous gestational diabetes mellitus and markers of cardiovascular risk. Int J Endocrinol 458610
Farmer SA, Black B, Bonow RO (2013) Tension between quality measurement, public quality reporting, and pay for performance. JAMA 309:349–350
Albareda M, Caballero A, Badell G et al (2003) Diabetes and abnormal glucose tolerance in women with previous gestational diabetes. Diabetes Care 26:1199–1205
Moreno-Castilla C, Hernandez M, Bergua M et al (2013) Low-carbohydrate diet for the treatment of gestational diabetes mellitus: a randomized controlled trial. Diabetes Care 36:2233–2238
Likis FE, Sathe NA, Carnahan R, McPheeters ML (2013) A systematic review of validated methods to capture stillbirth and spontaneous abortion using administrative or claims data. Vaccine 31:K74–K82
Kim C (2014) Maternal outcomes and follow-up after gestational diabetes mellitus. Diabet Med 3:292–301
Acknowledgements
We thank the Regional Health Agency and the Department of Health of the Puglia Region for their cooperation, general interest and provision of data.
Funding
The study had no external funding source.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
AN had full access to all study data and takes responsibility for the integrity of the data and the accuracy of data analysis. BP, AN and GDV made substantial contributions to the conception and design of the study. ADE and VL acquired data, and GL, FP, AN, BP, GT, MSc, MSa, GDB and MCR analysed and interpreted the data. BP, GDV and AN drafted the article. FP, GL, GDB, GT, MSa, MCR, VL, ADE and MSc revised the article critically for intellectual content. All authors approved the final version.
AN is the manuscript’s guarantor and affirms that the manuscript is an honest, accurate and transparent account of the study being reported; that no important aspects of the study have been omitted; and that everyone who contributed significantly to the work is listed in this author contribution section.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
(PDF 64 kb)
ESM Table 2
(PDF 67 kb)
Rights and permissions
About this article
Cite this article
Pintaudi, B., Lucisano, G., Pellegrini, F. et al. The long-term effects of stillbirth on women with and without gestational diabetes: a population-based cohort study. Diabetologia 58, 67–74 (2015). https://doi.org/10.1007/s00125-014-3403-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-014-3403-9