Abstract
Restenosis after angioplasty is a serious clinical problem that can result in re-occlusion of the coronary artery. Although current drug-eluting stents have proved to be more effective in reducing restenosis, they have drawbacks of inhibiting reendothelialization to promote thrombosis. New treatment options are in urgent need. We have shown that netrin-1, an axon-guiding protein, promotes angiogenesis and cardioprotection via production of nitric oxide (NO). The present study examined whether and how netrin-1 attenuates neointimal formation in a femoral wire injury model. Infusion of netrin-1 into C57BL/6 mice markedly attenuated neointimal formation following wire injury of femoral arteries, measured by intimal to media ratio (from 1.94 ± 0.55 to 0.45 ± 0.86 at 4 weeks). Proliferation of VSMC in situ was largely reduced. This protective effect was absent in DCC+/− animals. NO production was increased by netrin-1 in both intact and injured femoral arteries, indicating netrin-1 stimulation of endogenous NO production from intact endothelium and remaining endothelial cells post-injury. VSMC migration was abrogated by netrin-1 via a NO/cGMP/p38 MAPK pathway, while timely EPC homing was induced. Injection of netrin-1 preconditioned wild-type EPCs, but not EPCs of DCC+/− animals, substantially attenuated neointimal formation. EPC proliferation, NO production, and resistance to oxidative stress induced apoptosis were augmented by netrin-1 treatment. In conclusion, our data for the first time demonstrate that netrin-1 is highly effective in reducing neointimal formation following vascular endothelial injury, which is dependent on DCC, and attributed to inhibition of VSMC proliferation and migration, as well as improved EPC function. These data may support usage of netrin-1 and netrin-1 preconditioned EPCs as novel therapies for post angioplasty restenosis.
Key message
-
Netrin-1 attenuates neointimal formation following post endothelial injury via DCC and NO.
-
Netrin-1 inhibits VSMC proliferation in situ following endothelial injury.
-
Netrin-1 inhibits VSMC migration via a NO/cGMP/p38 MAPK pathway.
-
Netrin-1 augments proliferation of endothelial progenitor cells (EPCs) and EPC eNOS/NO activation.
-
Netrin-1 enhances resistance of EPCs to oxidative stress, improving re-endothelialization following injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restenosis is a serious clinical problem as an untoward result of angioplasty, which is commonly performed in patients with myocardial infarction or severely occluded coronary artery. It is a major complication after angioplasty treatment of myocardial infarction. In order to prevent occurrence of restenosis/re-occlusion of the coronary artery, different kinds of drug-eluting stents (DES) have been developed. Although DES reduced the occurrence of in-stent restenosis compared with bare-metal stents, it raises the concern that most of drugs used in DESs inhibit reendothelialization to promote thrombosis [1], which can be associated with more mortality. Hence, novel therapeutic strategies are in urgent need to prevent cardiovascular complications derived from restenosis.
The reason that restenosis remains unsolved clinically is likely attributed to its intricate mechanisms. Restenosis is primarily triggered by the damage of the endothelium that induces inflammatory response and thrombosis, followed by vascular smooth muscle cell (VSMC) proliferation and migration, and extensive vascular remodeling [2]. The endothelium has a crucial role in regulating vascular tone and structure by synthesizing nitric oxide (NO) from endothelial NO synthase (eNOS), which is known to be a vasodilator with anti-inflammatory and anti-thrombotic properties. NO produced in the endothelium activates cyclic GMP (cGMP) and cGMP-dependent protein kinase in VSMC, which induce vasodilatation as well as inhibition of VSMC proliferation and migration. Therefore, augmentation of NO action at physiological levels may have good potential for attenuating restenosis. Nonetheless, none of the currently available therapies could ensure modest and continuous release of NO. For example, nitroglycerin releases NO quickly but transiently to relieve chest pain associated with angina. Overdosing, however, leads to side effects such as severe hypotension [3]. In addition, it has been shown that many patients develop nitrate tolerance to become insensitive to the treatment [4].
Previously, our group have shown that netrin-1, originally discovered as an axon-guiding molecule [5, 6], exerts potent angiogenic and cardioprotective effects via the production of NO, mediated by DCC/ERK1/2 dependent activation of eNOS [7–9]. Binding of netrin-1 to DCC activates ERK1/2 to produce NO by phosphorylation of eNOS at serine 1179 residue [8]. Further, production of NO in turn activates DCC or ERK1/2 pathway, resulting in a feed-forward mechanism to contribute to cardioprotective or angiogenic signaling [7–13]. Therefore, it is reasonable to hypothesize that netrin-1 may prevent restenosis following endothelial injury, via the protective effect of NO.
In the present study, we examined the effects of netrin-1 on neointimal formation using a femoral artery wire injury model that simulates angioplasty procedure [14]. Netrin-1 infusion into femoral artery injured mice markedly attenuated neointimal formation in a DCC/NO-dependent manner. VSMC proliferation in situ was reduced. We further demonstrated an inhibitory effect of netrin-1 on VSMC migration, via a NO/cGMP/p38 MAPK pathway. In addition, netrin-1 infusion accelerated timely EPC homing after injury. Injection of netrin-1 preconditioned wild-type EPCs, but not EPCs of DCC+/− animals, largely abrogated neointimal formation. Proliferation, NO production, and resistance against oxidative stress-induced apoptosis of EPCs were significantly augmented by netrin-1. Taken together, our data for the first time establish that netrin-1 can serve as a potent vascular protective agent against restenosis after endothelial damage, and its effects are mediated by NO-dependent inhibition of VSMC migration and augmentation of EPC functions.
Methods
Animals
All animal procedures were approved by the Institutional Animal Care and Usage Committee at the University of California, Los Angeles. Six- to eight-week-old male C57BL/6 mice from Charles River Laboratories (Wilmington, MA) were used. Animals were housed in a pathogen free facility, with food and water ad labium, and under a 12-h light/dark cycle.
Reagents
Netrin-1 (#1109-N1) was purchased from R&D Systems (Minneapolis, MN). Antibodies of proliferating cell nuclear antigen (PCNA/#sc-56) and Flk-1 (#sc-19530) were purchased from Santa Cruz (Dallas, TX). CD34 antibody (#ab8158) and GFP antibody (#ab290) were obtained from Abcam (Cambridge, MA), and Alexa Fluor 594 conjugate-Isolectin GS-IB4 antibody (#I21413) was purchased from Life Technologies (Carlsbad, CA). CD133 antibody (#orb10288) was obtained from Biorbyt (San Francisco, CA). P38 MAPK inhibitor SB202190 (#559388) and JNK inhibitor SP600125 (#420119) were purchased from EMD Millipore (Germany). ERK1/2 inhibitor U0126 (#U120), cGMP antagonist Rp-8-Br-PET-cGMPs (#B6684), NO scavenger 2-phenyl-4,4,5,5-tetramethylimidazoline-1-oxyl-3-oxide (PTIO), anti-von Willebrand Factor (vWF) antibody (#F3520), and anti-actin antibody (#A2066) were all purchased from Sigma. Antibody for p38 MAPK (#506123) was obtained from Calbiochem. Antibodies for phospho-p38 MAPK (#9211), alpha-Tublin (#2125), eNOS (#9586), and phospho-eNOS (Ser1179) (#9571) were all purchased from Cell Signaling Technology (Danvers, MA). Goat anti-rabbit IgG-HRP conjugate (#172–1019) was obtained from Bio-Rad (Irvine, CA). Other chemicals were obtained from Sigma in the highest purity.
Surgical procedures—osmotic pump
Animals were anesthetized in a closed chamber filled with isoflurane, then quickly moved to a breathing mask supplied with 95%:5% O2/CO2 mixed with 1.5% isoflurane. Hair between the shoulder blades was removed using a hair removal lotion (Nair, Princeton, NJ), then disinfected using an iodine solution. A small incision was made in this area and a 4-week release osmotic pump (Durect Corp) was inserted into the left flank. Pumps were filled with either vehicle or netrin-1 (15 ng/day, 1109-N1, R&D Systems, Minneapolis, MN). Femoral wire injury was performed a day after the insertion of the osmotic pump to allow for the pretreatment of netrin-1.
Surgical procedures—femoral wire injury model
Animals were anesthetized as described above. After checking for proper anesthesia, the animal was turned on its back and restrained using surgical tape. Hair on the thigh area was removed using a hair removal lotion (Nair), then disinfected using an iodine solution. An incision was made on the right thigh area above the femoral artery. The femoral artery was then isolated and cleared of connective tissue. Blood flow is temporarily stopped using a small artery clamp, and an incision was made on a branch between the rectus femoris and vastus medialis muscles [14]. A fixed core wire guide coated with heparin was inserted into the artery and moved up. The artery clamp was then removed and the wire moved up toward the iliac artery. The wire was then allowed to stay for 60 s, then pulled back towards the incision point. This insertion and pulling back were repeated for a total of three times. At the end of the third time, the artery was once again clamped and the wire guide pulled out of the artery. The incision site on the artery was then ligated using surgical silk (5–0 Vicryl). The skin was then closed and sutured together, then sealed with surgical glue. A similar procedure was performed on the left leg, with the exception that the wire was not inserted into the artery. The femoral artery from the left leg was used as control.
Tissue processing
After euthanasia via CO2, animals were injected with 0.1 mL of heparin and flushed of blood using ice-cold PBS via the left ventricle. The animals were then perfused with 4% paraformaldehyde. Both femoral arteries were removed from the body and fixed overnight in 4% paraformaldehyde, prior to being embedded in paraffin and sectioned at 5 μm. For histological analysis on acute samples, harvested femoral arteries were directly embedded in OCT and subjected to slicing at 5 μm by cryostat sectioning.
H&E staining and immunostaining
H&E staining was performed by the Translational Pathology Core Laboratory Core Facility at UCLA using standard protocols, following sectioning. Further, PCNA immunostaining was performed using VECTASTATIN ABC Kit (Vectr Laboratories, Burlingame, CA). To observe the acute response after injury, CD34 and Isolectin GS-IB4 antibodies were used to detect homing EPCs and mature endothelial cells, respectively, on 1-h post-injury tissues. In addition, EPCs isolated from GFP transgenic mice were also subjected to netrin-1 preconditioning prior to injection, and the homing to the wound site was determined by co-staining with anti-GFP antibody and anti-Isolectin GS-IB4 antibody.
Quantification of neointimal formation
Using Image J software, the areas of the intimal and medial layers were measured manually. Ratio of intima to media was used for quantitative assessment of neointimal formation.
Nitric oxide radical detection by electron spin resonance
Bioavailable NO radical in femoral arteries and EPCs was detected using electron spin resonance (ESR) as previously described [8, 15] with modifications for the current experimental setup. For in vivo experiments, femoral arteries from four animals were combined for one experimental data point. NO production was measured from non-injured with or without netrin-1 injection (100 ng/ml of recombinant netrin-1 injected via the tail vein immediately after femoral injury surgery) and injured with or without netrin-1 injection. For in vitro experiments using EPCs, two 10-cm culture dishes were combined for each group. The tissues or cells were incubated with freshly prepared NO-specific spin trap Fe2+ (DETC)2 (0.5 mmol/L) colloid in modified Krebs/HEPES buffer with 50 μM (femoral artery) or 10 μM (EPCs) of calcium ionophore A23187 (Sigma, St Louis, MO) at 37 °C for 3 (femoral artery) or 1.5 (EPCs) hours. After incubation, tissues or cells were snap frozen in liquid nitrogen, then loaded into a finger Dewar for ESR measurement. The instrument settings were as follows: bio-field, 3410.00 G; field sweep, 100 G; microwave frequency, 9.79 GHz; microwave power, 13.26 mW (6 dB); modulation amplitude, 9.82 G; resolution, 512 points; and receiver gain 356.
Co-culture of VSMCs and endothelial cells
Rat aortic smooth muscle cells (Lonza, Switzerland) were cultured in DMEM/F12 media (Invitrogen) containing 15 ng/ml of amphotericin and 10% fetal bovine serum to confluence and starved in serum-free media overnight before experiments. Bovine aortic endothelial cells (BAECs) (Cell Systems, Kirkland, WA) were cultured as described previously [16]. Confluent VSMCs and endothelial cells were mixed together with equal cell number for migration assay.
VSMC migration assay
Transwell migration chamber (8-μm pore size, Corning) in 24-well plates was used for migration assay. Confluent cells were starved with serum-free media overnight prior to plating to the upper chamber. Co-culture of VSMCs and endothelial cells were seeded at a density of 2–2.5 × 105 cells/well on the top of the insert in 350 μl of serum-free culture medium, while 1 ml of 5% FBS medium containing pharmacological inhibitors [U0126 (50 μM), SB202190 (10 μM), SP600125 (10 μM), Rp-8-Br-PET-cGMPs (10 μM) and PTIO (60 μM)] was placed in the lower chamber. After 30 min of incubation, netrin-1 (100 ng/ml) was added into the medium in the lower chamber. The plates were then incubated for 24 h, followed by treatment of the cells with a dissociation buffer (Trevigen, Gaithersburg, MD) containing calcein AM (Calbiochem, Germany) to detect and quantify the fluorescence of migrated cells. The fluorescence were measured in a Bio-Tek fluorescence plate reader set at an excitation wavelength of ~485 nm and an emission wavelength of ~520 nm with triplicate readings.
Western blot analysis on co-cultured cells
Co-cultured cells were starved overnight in 0.5% FBS containing DMEM, incubated with or without Rp-8-Br-PET-cGMPs (10 μM, 30 min), and then exposed to netrin-1 (100 ng/ml) for 24 h. After treatment, cells were harvested and lysed, and subjected to detection of total p38 MAPK and phospho-p38 MAPK protein levels by Western blotting per standard protocols using 12% SDS/PAGE and nitrocellulose membranes. Antibody dilutions used were as follows: p38 MAPK (1:1000) and phospho-p38 MAPK (1:1000); alpha-Tublin (1:1000) was used as internal control. Goat anti-rabbit IgG-HRP conjugate (1:3000) was used as the secondary antibody. The blotting results were quantified using ImageJ, normalized to alpha-Tublin, and statistically analyzed from four independent experiments.
EPC isolation and culture
Mononuclear cells were collected from bone marrow of femur and tibia of 6–8-week-old C57BL6 mice (WT) or DCC+/− mice using density centrifugation and cultured in EGM-2 media (Lonza). The non-adherent cells were removed after 48 h, and then colony forming cells became confluent on the culture plate after 7–10 days. EPCs were characterized by immunocytochemical staining with CD34, CD133, Flk-1, and vWF antibodies.
EPC injection
Primarily, cultured EPCs isolated from WT or GFP transgenic mice were preconditioned with netrin-1 (100 ng/ml, 1 h) and 500 of the unconditioned and conditioned cells were injected through the tail vein of the animal immediately after femoral injury surgery. One hour or 4 weeks later, femoral arteries were harvested and processed for histological analyses of immunofluorescent or H&E staining, and re-endothelialization or the intimal growth was quantified.
EPC proliferation assay
EPCs from DCC+/+ and DCC+/− animals were seeded at an initial density of 1.0 × 105 cells/well in 12-well plates and incubated at 37 °C with a 5% CO2 incubator. After overnight incubation to allow cells to attach to the bottom of the plates, cells were starved with 5% FBS contained endothelial growth basal medium-2 (EBM-2) for 12 h. Then, cells were additionally incubated with or without netrin-1 (100 ng/ml in 5% FBS contained EBM-2 medium) for 24 h, following a pretreatment with or without PTIO (60 μM, 30 min). At the end of the incubation, cells in each well were resuspended following trypsinization and counted using a hemocytometer. Individual experiment was prepared in triplicate and was repeated three times.
EPC apoptosis assay—caspase 3 assay
EPCs from DCC+/+ and DCC+/− animals were seeded at approximately 1.0 × 105 cells/well in 24-well plates and cultured for 3 to 4 days till the cells become more than 90% confluent. Cells were then starved with 5% FBS contained EBM-2 medium. After overnight starvation, medium was discarded and replaced with PBS with or without PTIO (60 μM, 30 min) and/or netrin-1 (100 ng/ml, 30 min), and then exposed to hydrogen peroxide (H2O2, 500 μM) for 30 min. Caspase 3 activity was assessed with a fluorimetric caspase 3 Assay Kit (Sigma), following the manufacturer’s instruction. Briefly, cells were suspended into tubes with lysis buffer. Assay buffer and caspase 3 substrate Ac-DEVD-AMC were added and the sample mixtures were transferred to a black 96-well plate along with substrate blank and caspase 3 positive control. The fluorescent signal from AMC, which is the hydrolysed substrate by caspase 3, was detected at excitation of 360 nm and emission of 460 nm every 10 min for 1 h.
EPC apoptosis assay—TUNEL assay
APO-BrdU TUNEL assay (Invitrogen) was performed using the identically treated EPCs subjected to caspase 3 assay. The kit detects the DNA fragmentation of apoptotic cells by reacting terminal deoxynucleotidyl transferase (TdT) and the deoxythymidine analog (BrdUTP) to label the break sites. The incorporated BrdU at DNA break sites was detected by an Alexa Fluor 488 dye-labeled anti-BrdU antibody. Therefore, the Alexa Fluor 488 dye along with propidium iodide (detects the total cellular DNA content) was imaged with the Nikon Eclipse Ti confocal microscope.
eNOS phosphorylation in EPCs
Alongside, NO radical detection by ESR, eNOS phosphrylation at serine 1179 in mouse EPCs was examined using Western blot analysis. Antibody dilutions used were as follows: eNOS (1:500) and phospho-eNOS (Ser 1179) (1:500). Actin (1:10,000) was used as an internal control. Goat anti-rabbit IgG-HRP conjugate (1:3000) was used as the secondary antibody.
Statistics
All statistics were performed using Prism software. Comparisons between two groups were performed using t tests, with a significance level of 0.05. Comparisons among multiple groups were performed using ANOVA, with Newman-Keuls as the post hoc test and a significance level of 0.05.
Results
Netrin-1 infusion markedly attenuated neointimal formation post endothelial injury
To test whether netrin-1 induces protection against neointimal growth, femoral wire injury was performed on animals that were infused with netrin-1 or vehicle. Intima to media ratio (averaged at 0.15 ± 0.05 for intact vessels) was 1.98 ± 0.47 at 4 weeks after surgery in vehicle-treated animals, while netrin-1 infusion markedly decreased this ratio to 0.64 ± 0.14 (Fig. 1a, b). Netrin-1 was also effective in reducing neointimal growth even at week 1. The representative H&E images of the vessels which are shown in Fig. 1a, c, d demonstrate that VSMC proliferation in situ, labeled by PCNA, was significantly increased in wire injured femoral arteries. This was, however, largely prevented by netrin-1 infusion.
Netrin-1 infusion significantly inhibits neointimal growth after femoral artery wire injury. Femoral artery was injured by the passing of a guide wire, and netrin-1 was infused via an osmotic minipump. Femoral arteries were harvested after 1 or 4 weeks, fixed in paraformaldehyde, and sectioned and stained for H&E and PCNA antibody. a Representative H&E images. b Grouped data of intima to media ratio. Data show that at 1 and 4 weeks, netrin-1-infused animals had significantly smaller intima to media ratio in the wire-damaged artery, indicating inhibition of neointimal growth. n = 4–8 *p < 0.05,**p < 0.01. c Representative images of immunohistochemical staining. PCNA-positive cells are stained with dark brown in color. d Grouped quantitative data of PCNA-positive cells to whole tissue ratio. Netrin-1-infused animals had significantly less PCNA both at 1- and 4-week postinjury. n = 4–7, **p < 0.01, ***p < 0.001 v.s. CTRL in 1 week, # p < 0.05, $$ p < 0.01
Netrin-1’s protective effect against neointimal formation is dependent on DCC
To test whether netrin-1 receptor DCC is involved in the protective effect to attenuate neointimal formation, similar experiments described above were performed in DCC+/+ and DCC+/− animals. The results, shown in Fig. 2a for representative H&E images and Fig. 2b for quantitative data, indicate that netrin-1’s inhibition on neointimal growth was abolished in DCC+/− animals. This confirms that DCC is the receptor through which netrin-1 exerts its vascular protective effects against wire-induced endothelial injury.
Netrin-1’s protective effect against neointimal growth is mediated by the receptor DCC. Netrin-1 was infused via an osmotic minipump into DCC+/+ and DCC+/− mice that received a femoral wire injury. The femoral arteries were harvested 4 weeks later, fixed in paraformaldehyde, sectioned, and stained for H&E. a Representative H&E images. b Grouped data for intima to media ratio from DCC+/+ and DCC+/− animals, indicating that netrin-1-induced attenuation of neointimal growth was absent in DCC+/− mice. n = 4–9 each, *p < 0.05, **p < 0.01
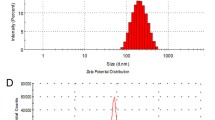
Netrin-1 significantly induces NO production in femoral arteries
In previous studies in our laboratory, we found that netrin-1 can increase NO production both in cells [8] and tissue [7, 9–13]. Since NO is known to attenuate neointimal formation [16, 17], we hypothesized that NO mediates netrin-1’s inhibitory effect on neointimal formation in the wire injury model. Here, we measured NO production using ESR from femoral arteries 1 h after injury, in the presence or absence of netrin-1 intravenous injection (immediately after surgery, 100 ng/mL blood). As shown in Fig. 3, we observed a 38.5% reduction in NO bioavailability in the injured femoral arteries, indicating loss of endothelium and eNOS. Netrin-1 treatment elevated NO production in both injured and non-injured vessels, implicating potent activation of eNOS in both intact and partially remained endothelium.
Netrin-1 infusion increases NO production. Netrin-1 was injected via tail vein immediately after injury. The harvested 1-h post-injured femoral arteries were incubated in the spin trap solution for 3 h before electron spin resonance (ESR) determination of NO production. a Representative ESR spectra. b Grouped data for NO production. n = 4–10 each, *p < 0.05, ***p < 0.001 vs. CTRL, intact, ### p < 0.001, vs. CTRL, injured
Netrin-1 inhibits VSMC migration via an NO-dependent mechanism
Migration of VSMC is one of the major events that leads to abnormal intimal growth after endothelial damage. In a previous study, we demonstrated increased NO production in netrin-1 endothelial cell [8], which has been shown to be a potent inhibitor of VSMC migration. Hence, we examined whether netrin-1’s protective effect on neointimal growth is related to inhibition of VSMC migration by NO. We co-cultured VSMCs with endothelial cells, treated the cells with vehicle, netrin-1, or netrin-1 in combination with PTIO, an NO scavenger, and then the migrated cells were dissociated and quantified by detecting fluorescence from calcein AM. The results, shown in Fig. 4a, demonstrate that netrin-1 significantly and reproducibly inhibited cell migration from these co-cultures. Further, co-treatment with PTIO largely abolished this inhibition, suggesting that netrin-1’s effect on VSMC migration is mediated via NO.
Netrin-1 inhibits migration of vascular smooth muscle cells. Vascular smooth muscle cells (VSMCs) and endothelial cells (ECs) were co-cultured in equal cell numbers. Cell migration was measured using transwell assay. a VSMC migration from VSMC/EC co-cultures treated with netrin-1 in the absence or presence of pharmacological inhibitors (PTIO (60 μM) as NO scavengers, and inhibitors for p38 MAPK (10 μM), cGMP (10 μM), ERK (50 μM), JNK (10 μM)) **p < 0.05, n = 3–4. Data indicate NO, cGMP, and p38 MAPK-dependent attenuation of VSMC migration by netrin-1. b Western blot analysis for p-p38 MAPK/p38 MAPK in netrin-1-treated co-cultures in the presence or absence of cGMP antagonist Rp-8-Br-PET-cGMPs, indicating cGMP lies upstream of p38 MAPK. n = 3, *p < 0.01, **p < 0.05 vs. netrin-1
We further examined the downstream signaling pathways that lead to the inhibition of migration in VSMCs by pretreating VSMCs with inhibitors against cGMP, and those of major mitogenic pathways. The results in Fig. 4a show that while inhibitors against ERK1/2 and JNK had no effect on netrin-1’s inhibition of VSMC migration, blockade of cGMP and p38 MAPK signaling abolished netrin-1’s effect. We next examined the relationship between cGMP and p38 MAPK. Using Western blotting, we examined the phosphorylation levels of p38 MAPK in the EC-VSMC co-cultures treated with netrin-1 in the absence or presence of the cGMP antagonist. The results in Fig. 4b demonstrate that cGMP antagonist attenuated p38 MAPK activation, implicating a NO/cGMP/p38 MAPK pathway in mediating netrin-1-induced inhibition of VSMC migration.
Netrin-1 infusion accelerates timely homing of EPCs to the wound site
Timely re-endothelialization after endothelium damage is critical in the prevention of vascular remodeling. Hence, there must be a more acute modification by netrin-1 that helps re-endothelialization, so that the inhibition of VSMC migration can be triggered. Figure 5 shows increased expression and colocalization of CD34 (a EPC marker) with Isolectin (an EC marker) in netrin-1 infused injured femoral arteries 1-h post-injury and EPC injection (Fig. 5D’), whereas neither of those were present at the endothelial layer of the injured femoral arteries without netrin-1 infusion (Fig. 5C’). Therefore, the results indicate that netrin-1 accelerated timely homing and re-endothelialization of EPCs to the wound site. To further examine homing of EPCs from the injected population, EPCs isolated from GFP transgenic mice (GFP-EPCs) were traced after injecting into WT animals by imaging GFP. As shown in Fig. 5e–g, homing of GFP-EPCs to the injured femoral arteries was accelerated by netrin-1 preconditioning.
Netrin-1 accelerated EPC homing after endothelial injury. Femoral arteries were harvested at 1-h post-injury, with or without netrin-1 pre-infusion. EPC homing was evaluated by co-staining with anti-CD34 and Isolectin antibodies. Shown here are the representative immunohistochemical images from each group. a Intact tissue without netrin-1 infusion. b Intact tissue with netrin-1 infusion. c Injured tissue without netrin-1 infusion. d Injured tissue with netrin-1 infusion. Data indicate accelerated EPC homing, implicated by co-localization of CD34 and Isolectin at the endothelial layer of netrin-1 infused injured femorals, but not on the injured femorals without netrin-1 infusion. Moreover, femoral arteries were harvested at 1-h post-injury, with or without netrin-1 preconditioning on EPCs isolated from GFP transgenic mice. EPC homing was evaluated by co-staining with anti-GFP and Isolectin antibodies. e Showing an intact femoral artery from GFP transgenic animal as a comparison. f Injured tissue received GFP-EPC without netrin-1 pre-condition. g Injured tissue received GFP-EPC with netrin-1 precondition. Data indicate accelerated EPC homing by netrin-1 pre-condition, implicated by co-localization of GFP and Isolectin at the endothelium of injured femorals, but not on injured femorals without netrin-1 pre-conditioning. A’–D’, F’, and G’ zoomed-in pictures of selected areas. The pictures were inverted due to the use of inverted confocal microscope with 40× objective lens
Netrin-1 preconditioned EPCs attenuate wire injury-induced neointimal formation
EPCs play an important role in the re-endothelialization process [19]. EPCs derived from bone marrow mobilize to peripheral circulation and differentiate into mature ECs once they attach to the wound site. Therefore, timely recruitment of EPCs to the damaged vessel is essential to the prevention of neointimal growth [18]. Hence, another mechanism by which netrin-1 may exert its protective effect is via functional augmentations of EPCs. Here, we examined whether netrin-1 preconditioned EPCs can confer vascular protection. EPCs isolated from either DCC+/+ or DCC+/− animals were injected into WT mice vai tail vein immediately after wire injury. The femoral arteries were harvested after 4 weeks to assess intima to media ratio. Figure 6a shows the characterization of bone marrow-derived EPCs, which express CD34, CD133, Flk-1, and vWF. Figure 6b shows representative H&E images of the femoral arteries, while Fig. 6c shows summarized data. The results indicate that netrin-1 preconditioned EPCs largely attenuated neointimal formation, which was absent when EPCs isolated from the DCC+/− animals were used, suggesting that netrin-1 can directly impinge on EPCs to exert the beneficial effect, and that the EPCs also require DCC receptor to respond to netrin-1 preconditioning. These results implicate a role of EPCs in the repair mechanism and suggest that netrin-1 preconditioned EPCs may serve as a potential therapeutic application.
Netrin-1 preconditioned EPCs significantly reduces neointimal growth in a DCC-dependent fashion. a Characterization of EPCs isolated and differentiated from mouse bone marrow (scale 20 μm). These EPCs express CD34, CD133, vWF, and Flk-1, which colocalize well with each other. Particularly, vWF is localized to Weibel-Palade bodies. EPCs isolated from DCC+/+ or DCC+/− mice were preconditioned with netrin-1 (100 ng/ml, 1 h) prior to being tail vein injected into wild-type animals immediately after femoral wire injury. The femoral arteries were harvested after 4 weeks, fixed, sectioned, and stained for H&E. b Representative H&E images. c Grouped data of intima to media ratio, indicating that netrin-1-treated EPC markedly attenuated neointimal growth, while this protective effect was abolished with EPCs harvested from DCC+/−animals
Netrin-1 significantly improves EPC proliferation
As endothelial cells are potent inhibitors of VSMC migration, timely regeneration of the endothelial layer is critical in preventing neointimal growth after vascular injury. Hence, the proliferation of EPCs is one of the critical factors that are involved in re-endothelialization and vascular repair. Here, we examined whether netrin-1 can improve proliferation of EPCs. The results, shown in Figure7a, b, indicate that netrin-1 (100 ng/ml, 24 h) significantly increased DCC+/+-EPC proliferation by 42%, which was also mediated by NO as NO scavenger PTIO attenuated this response.
We have previously shown that netrin-1 can promote endothelial cell proliferation and migration through its receptor DCC via an ERK1/2-NO pathway [8]. In this study, we examined proliferation of WT EPCs and those isolated from DCC+/− animals. The EPCs isolated from DCC+/− mice did not show improvement in proliferation in response to netrin-1 treatment (Fig. 7b). Therefore, the beneficial response to netrin-1 in EPC proliferation requires the presence of DCC.
Netrin-1 augments EPC function: increased proliferative activity and resistance to oxidative stress-induced apoptosis. a Proliferation of wild-type EPCs was measured by cell number using hemocytometer. Netrin-1 increased the proliferative activity of EPCs, while having no effect on EPCs pretreated with NO scavenger PTIO. n = 3, *p < 0.001 vs. netrin-1 in the control group. b Netrin-1 increases the proliferative activity of EPCs, while having no effect on EPCs isolated from DCC+/− animals. n = 5–6, *p < 0.01, **p < 0.001 vs. control of DCC+/+ EPCs. c EPC apoptosis measured by caspase 3 activity after the treatment of hydrogen peroxide (500 μmol/L, 30 min), showing that netrin-1 preconditioning (100 ng/ml) for 30 min significantly reduced apoptosis while this response was absent in PTIO pretreated cells. n = 3, p < 0.05. d EPC apoptosis was measured by TUNEL assay after the treatment of hydrogen peroxide (500 μmol/L, 30 min), showing that preconditioning of netrin-1 (100 ng/ml) for 30 min significantly reduced apoptosis. n = 4–6, ## p < 0.01, ### p < 0.001 vs. control, ***p < 0.001 vs. netrin-1, $ p < 0.05, $$$ p < 0.001 v.s. netrin-1 + H2O2. e Representative pictures of TUNEL assay. Apoptotic cells detected by TUNEL staining is shown in green, whereas total cellular DNA detected by PI staining is shown in red. Grouped quantitative data are shown in panel d
Netrin-1 significantly improves EPC resistance to oxidative stress-induced apoptosis
It has been shown that EPCs are sensitive to oxidative stress-induced apoptosis [19], and its number is often reduced in patients with coronary artery disease [20, 21]. Therefore, it is important to augment the resistance to oxidative stress of EPCs to ensure their viability to promote vascular repair. Hydrogen peroxide (H2O2)-induced apoptosis in EPCs was measured using a caspase 3 assay. It turned out H2O2 increased caspase 3 activity by 43%, which was abolished by netrin-1 treatment (Fig. 7c). TUNEL assay also showed a significant decrease of H2O2-induced apoptosis in netrin-1-treated EPCs (Fig. 7d, representative images in Fig. 7e). For both assays, the protective effect of netrin-1 was absent with PTIO scavenging of NO. These data clearly demonstrate that netrin-1 protects EPCs against apoptosis via NO.
Netrin-1 induces NO production and eNOS activation in EPCs
Enhanced endothelial repair is attributed to the enhanced EPC proliferation, viability, and NO production. This EPC-derived NO production has been shown to exert antioxidant action and prevent further endothelial injury [22]. Thus, we examined whether NO production changes in netrin-1-treated EPCs. Figure 8a shows significant upregulation of NO production from netrin-1-treated EPCs compared to non-treated EPCs. Further, we demonstrated that there is an increase in eNOSs1179 phosphorylation in EPCs treated with netrin-1 (Fig. 8b). Therefore, netrin-1 promotes EPC function, not only by increasing its number and viability but also by improving eNOS activation and NO production.
Netrin-1 induces NO production and eNOS activation in EPCs. a NO production from EPCs was measured using ESR. Netrin-1 treatment increased NO production by 70%. n = 6, p < 0.05. b p-eNOS to eNOS ratio (normalized with beta-actin individually) in netrin-1-treated EPCs. Netrin-1 treatment significantly increased the phosphorylation of eNOS at serine 1179. n = 3, p < 0.05
Discussion
In this work, we examined the vascular protective effects of netrin-1 against neointimal growth induced by wire injury in the femoral artery. Netrin-1 infusion abolished neointimal formation as assessed by ratio of intimal to medial thickness, when compared to untreated controls. This effect was absent in animals lacking the netrin-1 receptor DCC. VSMC proliferation in situ was largely attenuated by netrin-1. VSMC migration, one of the major events in neointimal growth, was inhibited with netrin-1 and mediated by the NO/cGMP/p38 MAPK pathway. Rapid acceleration of EPC homing and re-endothelialization were induced by netrin-1. In separate experiments, we injected netrin-1-treated EPCs to femoral injured animals, which also reduced the ratio of intimal to medial thickness when compared to animals injected with untreated EPCs. We further observed that EPCs treated with netrin-1 had improved proliferative activity, increased resistance to oxidative stress-induced apoptosis, increased eNOS serine 1179 phosphorylation, and elevated NO production. Overall, these data clearly define a novel and robust effect of netrin-1 serving as a vascular protective agent against neointimal formation/restenosis following endothelial damage. A schematic summary of the mechanisms that are elucidated in this study is shown in Fig. 9.
Schematic summary of mechanistic insights of netrin-1 inhibition of restenosis. Endothelial injury causes restenosis by reducing NO production from the loss of the endothelial cells and subsequently removing its inhibition on VSMC migration. Netrin-1 treatment inhibits VSMC migration via NO/cGMP/p38MAPK. In situ VSMC proliferation was also inhibited by netrin-1 perfusion. In addition, netrin-1 augments functions of EPCs, including increased proliferation and enhanced resistance to oxidative stress, facilitating timely homing of EPCs to the wound site. These downstream pathways contribute to marked inhibitory effects of netrin-1 on neointimal formation post endothelial injury
Netrin-1 has been shown in the past to have angiogenic properties [8, 23, 24]. In our laboratory, we have previously shown that netrin-1 enhances endothelial proliferation and migration through a NO-dependent pathway [8]. In this study, we examined whether netrin-1’s enhancement of endothelial activity and EPC function can offer protection against neointimal formation in a model that simulates angioplasty. Intriguingly, infusion of netrin-1 resulted in near complete attenuation of neointimal formation, which was absent in animals deficient in DCC. This is even more potent than the overexpression of eNOS, which attenuated neointimal formation by 70% [25]. Protein S-nitrosothiols that release NO chronically and locally also attenuates neointimal formation after arterial balloon injury in a rabbit model [26]. Combined with our previous notion that relatively modest concentration of netrin-1 is optimally cardioprotective, persistent and modest release of NO from netrin-1 is particularly vascular protective.
Restenosis is a consequence of a series of events triggered by endothelial damage [2]. Damage to the endothelium result in a loss of NO production from eNOS, which plays a central role in endothelium-dependent vascular protection [27]. Although VSMCs are quiescent under normal conditions, they re-express mitogenic factors under pathological conditions such as restenosis and atherosclerosis [28]. Restricted levels of NO promote VSMC proliferation and migration [29], while inducing vasoconstriction [30]. Migrating VSMCs infiltrate to the intimal area and form the intimal cushion. VSMC migration is provoked by various factors, such as chemotactic cytokines, growth factors, and extracellular matrix components [31]. Our co-culture results demonstrated that cGMP and p38 MAPK are sequentially involved in netrin-1 inhibition of VSMC migration. Previous findings indicate that p38 MAPK mediates VSMC migration in response to platelet-derived growth factor (PDGF) [32] and vascular endothelial growth factor (VEGF) [33]. P38 MAPK has also been shown to decrease mitogenic responses in cardiomyocytes [34]. These disparate responses reflect varied roles of p38 MAPK in different cell types and in response to different stimuli. We further showed that p38 MAPK is downstream of cGMP. The mechanistic details of cGMP signaling to p38 MAPK remain to be elucidated, though it has been suggested to occur in cardiomyocytes [35, 36]. The other two major MAPK pathways, ERK1/2 and JNK, are often studied as pro-proliferative pathways, whereas the p38 MAPK pathway is often associated with anti-proliferative pathways [37]. This might explain the distinct response of p38 MAPK to netrin-1 among those three MAPKs, suggesting that netrin-1 may play a role in inhibiting chemotaxis, rather than DNA synthesis of VSMCs. In addition, loss of NO inhibition of inflammatory responses in general would contribute to neointimal formation, which can be corrected by infusion of netrin-1 to stimulate NO production from the post-injury remaining endothelial cells.
The treatment with progenitor or stem-like cells has been shown in the past to reduce neointimal growth after vascular injury [18, 38–40]. In one study that also used the femoral artery injury model, intravenous injection with iPS-cell-derived Flk-1+ cells [39] resulted in reduction of neointimal formation when more than 1 × 106 of the cells were injected. In our study, we injected only 500 EPCs, which had no significant effect on neointimal formation. However, preconditioning of these EPCs with netrin-1 markedly attenuated neointimal formation, which could be attributed to augmentations in proliferative activity, resistance to apoptosis, and NO production. After the lost of the endothelium due to vascular injury, the timely recovery of the endothelial layer is essential for the restoration of endothelial homeostasis, attributed to the potent inhibitory effects on neointimal formation of endothelium derived NO [25]. Indeed, we observed the rapid acceleration of EPC homing and re-endothelialization in femoral arteries 1 h after endothelial injury and netrin-1 tail vein injection. Furthermore, the number of functional EPCs is important for the proper healing of the endothelium after vascular repair, while reduced EPC number has been observed in patients with hypertension and coronary artery disease [41]. Oxidative stress develops after vascular injury [42]. Therefore, the effect of netrin-1 in improving the resistance to oxidative stress-induced apoptosis of EPCs would facilitate survival of the EPCs to enhance repair. Taken together, our data also support the use of limited numbers of circulating EPCs for anti-restenosis therapy.
In conclusion, these data establish netrin-1 as a potent vascular protective agent against neointimal growth following femoral wire injury of the endothelium. This effect of netrin-1 is dependent on the receptor DCC for either netrin-1 infusion or treatment with netrin-1 preconditioned EPCs. The protection is mediated by NO/cGMP/p38 MAPK-dependent inhibition of VSMC migration, and augmented functions of EPCs in terms of enhanced proliferative activity, increased resistance to oxidative stress-induced apoptosis, and increased eNOS phosphorylation and NO production. These findings may promote usage of netrin-1 and netrin-1 preconditioned EPCs as novel therapeutics treating post-angioplasty restenosis, which would be highly significant in the management of myocardial infarction at bedside.
References
Garg S, Serruys PW (2010) Coronary stents: current status. J Am Coll Cardiol 56:S1–42
Chaabane C, Otsuka F, Virmani R, Bochaton-Piallat ML (2013) Biological responses in stented arteries. Cardiovasc Res 99:353–363
Thadani U, Rodgers T (2006) Side effects of using nitrates to treat angina. Expert Opin Drug Saf 5:667–674
Munzel T, Daiber A, Mulsch A (2005) Explaining the phenomenon of nitrate tolerance. Circ Res 97:618–628
Kennedy TE, Serafini T, de la Torre JR, Tessier-Lavigne M (1994) Netrins are diffusible chemotropic factors for commissural axons in the embryonic spinal cord. Cell 78:425–435
Serafini T, Kennedy TE, Galko MJ, Mirzayan C, Jessell TM, Tessier-Lavigne M (1994) The netrins define a family of axon outgrowth-promoting proteins homologous to C. elegans UNC-6. Cell 78:409–424
Bouhidel JO, Wang P, Li Q, Cai H (2014) Pharmacological postconditioning treatment of myocardial infarction with netrin-1. Front Biosci (Landmark Ed) 19:566–570
Nguyen A, Cai H (2006) Netrin-1 induces angiogenesis via a DCC-dependent ERK1/2-eNOS feed-forward mechanism. Proc Natl Acad Sci U S A 103:6530–6535
Zhang J, Cai H (2010) Netrin-1 prevents ischemia/reperfusion-induced myocardial infarction via a DCC/ERK1/2/eNOS s1177/NO/DCC feed-forward mechanism. J Mol Cell Cardiol 48:1060–1070
Bouhidel JO, Wang P, Siu KL, Li H, Youn JY, Cai H (2014) Netrin-1 improves post-injury cardiac function in vivo via DCC/NO-dependent preservation of mitochondrial integrity, while attenuating autophagy. Biochim Biophys Acta 1852:277–289
Siu KL, Lotz C, Ping P, Cai H (2014) Netrin-1 abrogates ischemia/reperfusion-induced cardiac mitochondrial dysfunction via nitric oxide-dependent attenuation of NOX4 activation and recoupling of NOS. J Mol Cell Cardiol 78:174–185
Li Q, Cai H (2015) Induction of cardioprotection by small netrin-1 derived peptides. Am J Physiol Cell Physiol DOI: ajpcell 00332:02014
Li Q, Wang P, Ye K, Cai H (2015) Central role of SIAH inhibition in DCC-dependent cardioprotection provoked by netrin-1/NO. Proc Natl Acad Sci U S A 112:899–904
Sata M, Maejima Y, Adachi F, Fukino K, Saiura A, Sugiura S, Aoyagi T, Imai Y, Kurihara H, Kimura K et al (2000) A mouse model of vascular injury that induces rapid onset of medial cell apoptosis followed by reproducible neointimal hyperplasia. J Mol Cell Cardiol 32:2097–2104
Oak JH, Cai H (2007) Attenuation of angiotensin II signaling recouples eNOS and inhibits nonendothelial NOX activity in diabetic mice. Diabetes 56:118–126
Ahanchi SS, Tsihlis ND, Kibbe MR (2007) The role of nitric oxide in the pathophysiology of intimal hyperplasia. J Vasc Surg 45(Suppl A):A64–A73
Bahnson ES, Koo N, Cantu-Medellin N, Tsui AY, Havelka GE, Vercammen JM, Jiang Q, Kelley EE, Kibbe MR (2014) Nitric oxide inhibits neointimal hyperplasia following vascular injury via differential, cell-specific modulation of SOD-1 in the arterial wall. Nitric Oxide 44C:8–17
Kong D, Melo LG, Mangi AA, Zhang L, Lopez-Ilasaca M, Perrella MA, Liew CC, Pratt RE, Dzau VJ (2004) Enhanced inhibition of neointimal hyperplasia by genetically engineered endothelial progenitor cells. Circulation 109:1769–1775
Ingram DA, Krier TR, Mead LE, McGuire C, Prater DN, Bhavsar J, Saadatzadeh MR, Bijangi-Vishehsaraei K, Li F, Yoder MC et al (2007) Clonogenic endothelial progenitor cells are sensitive to oxidative stress. Stem Cells 25:297–304
Vasa M, Fichtlscherer S, Adler K, Aicher A, Martin H, Zeiher AM, Dimmeler S (2001) Increase in circulating endothelial progenitor cells by statin therapy in patients with stable coronary artery disease. Circulation 103:2885–2890
Vasa M, Fichtlscherer S, Aicher A, Adler K, Urbich C, Martin H, Zeiher AM, Dimmeler S (2001) Number and migratory activity of circulating endothelial progenitor cells inversely correlate with risk factors for coronary artery disease. Circ Res 89:E1–E7
Gao L, Li P, Zhang J, Hagiwara M, Shen B, Bledsoe G, Chang E, Chao L, Chao J (2014) Novel role of kallistatin in vascular repair by promoting mobility, viability, and function of endothelial progenitor cells. J Am Heart Assoc 3:e001194
Wilson BD, Ii M, Park KW, Suli A, Sorensen LK, Larrieu-Lahargue F, Urness LD, Suh W, Asai J, Kock GA et al (2006) Netrins promote developmental and therapeutic angiogenesis. Science 313:640–644
Yang Y, Zou L, Wang Y, Xu KS, Zhang JX, Zhang JH (2007) Axon guidance cue netrin-1 has dual function in angiogenesis. Cancer Biol Ther 6:743–748
von der Leyen HE, Gibbons GH, Morishita R, Lewis NP, Zhang L, Nakajima M, Kaneda Y, Cooke JP, Dzau VJ (1995) Gene therapy inhibiting neointimal vascular lesion: in vivo transfer of endothelial cell nitric oxide synthase gene. Proc Natl Acad Sci U S A 92:1137–1141
Marks DS, Vita JA, Folts JD, Keaney JF Jr, Welch GN, Loscalzo J (1995) Inhibition of neointimal proliferation in rabbits after vascular injury by a single treatment with a protein adduct of nitric oxide. J Clin Invest 96:2630–2638
Oemar BS, Tschudi MR, Godoy N, Brovkovich V, Malinski T, Luscher TF (1998) Reduced endothelial nitric oxide synthase expression and production in human atherosclerosis. Circulation 97:2494–2498
Ross R (1993) The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature 362:801–809
Alef MJ, Vallabhaneni R, Carchman E, Morris SM Jr, Shiva S, Wang Y, Kelley EE, Tarpey MM, Gladwin MT, Tzeng E et al (2011) Nitrite-generated NO circumvents dysregulated arginine/NOS signaling to protect against intimal hyperplasia in Sprague-Dawley rats. J Clin Invest 121:1646–1656
Surks HK (2007) cGMP-dependent protein kinase I and smooth muscle relaxation: a tale of two isoforms. Circ Res 101:1078–1080
Wang XQ, Lindberg FP, Frazier WA (1999) Integrin-associated protein stimulates alpha2beta1-dependent chemotaxis via Gi-mediated inhibition of adenylate cyclase and extracellular-regulated kinases. J Cell Biol 147:389–400
Iijima K, Yoshizumi M, Hashimoto M, Akishita M, Kozaki K, Ako J, Watanabe T, Ohike Y, Son B, Yu J et al (2002) Red wine polyphenols inhibit vascular smooth muscle cell migration through two distinct signaling pathways. Circulation 105:2404–2410
Wang Z, Castresana MR, Newman WH (2004) Reactive oxygen species-sensitive p38 MAPK controls thrombin-induced migration of vascular smooth muscle cells. J Mol Cell Cardiol 36:49–56
Engel FB, Schebesta M, Duong MT, Lu G, Ren S, Madwed JB, Jiang H, Wang Y, Keating MT (2005) p38 MAP kinase inhibition enables proliferation of adult mammalian cardiomyocytes. Genes Dev 19:1175–1187
Kim SO, Xu Y, Katz S, Pelech S (2000) Cyclic GMP-dependent and -independent regulation of MAP kinases by sodium nitroprusside in isolated cardiomyocytes. Biochim Biophys Acta 1496:277–284
Li Z, Zhang G, Feil R, Han J, Du X (2006) Sequential activation of p38 and ERK pathways by cGMP-dependent protein kinase leading to activation of the platelet integrin alphaIIb beta3. Blood 107:965–972
Lopez-Bergami P (2011) The role of mitogen- and stress-activated protein kinase pathways in melanoma. Pigment Cell Melanoma Res 24:902–921
Fujiyama S, Amano K, Uehira K, Yoshida M, Nishiwaki Y, Nozawa Y, Jin D, Takai S, Miyazaki M, Egashira K et al (2003) Bone marrow monocyte lineage cells adhere on injured endothelium in a monocyte chemoattractant protein-1-dependent manner and accelerate reendothelialization as endothelial progenitor cells. Circ Res 93:980–989
Yamamoto T, Shibata R, Ishii M, Kanemura N, Kito T, Suzuki H, Miyake H, Maeda K, Tanigawa T, Ouchi N et al (2013) Therapeutic reendothelialization by induced pluripotent stem cells after vascular injury—brief report. Arterioscler Thromb Vasc Biol 33:2218–2221
Griese DP, Ehsan A, Melo LG, Kong D, Zhang L, Mann MJ, Pratt RE, Mulligan RC, Dzau VJ (2003) Isolation and transplantation of autologous circulating endothelial cells into denuded vessels and prosthetic grafts: implications for cell-based vascular therapy. Circulation 108:2710–2715
Imanishi T, Moriwaki C, Hano T, Nishio I (2005) Endothelial progenitor cell senescence is accelerated in both experimental hypertensive rats and patients with essential hypertension. J Hypertens 23:1831–1837
Juni RP, Duckers HJ, Vanhoutte PM, Virmani R, Moens AL (2013) Oxidative stress and pathological changes after coronary artery interventions. J Am Coll Cardiol 61:1471–1481
Acknowledgements
This work was supported by the National Institute of Health National Heart, Lung and Blood Institute (NHLBI) Grants HL077440 (HC), HL088975 (HC), HL108701 (HC, DGH), HL119968 (HC), an American Heart Association Established Investigator Award (EIA) 12EIA8990025 (HC) and an American Heart Association Predoctoal Fellowship Award 14PRE20380184 (NML).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Additional information
Norika Mengchia Liu and Kin Lung Siu contribute equally to this study.
Rights and permissions
About this article
Cite this article
Liu, N.M., Siu, K.L., Youn, J.Y. et al. Attenuation of neointimal formation with netrin-1 and netrin-1 preconditioned endothelial progenitor cells. J Mol Med 95, 335–348 (2017). https://doi.org/10.1007/s00109-016-1490-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-016-1490-4
Keywords
- Netrin-1
- Neointimal formation
- Vascular smooth muscle cell (VSMC) proliferation
- VSMC migration
- Femoral wire injury
- Deleted in colorectal cancer (DCC)
- Endothelial progenitor cells (EPCs)
- EPC proliferation
- Endothelial nitric oxide synthase (eNOS) phosphorylation
- NO production
- EPC resistance to oxidative stress
- EPC homing
- Re-endothelialization