Abstract
Deleted in lung and esophageal cancer 1 (DLEC1), located at 3p22-p21.3, is involved in the carcinogenesis of multiple cancers, but its role in prostate cancer (PrCa) remains unclear. Here, we studied the epigenetic alteration of DLEC1 and its functions in prostate cancer. We found that DLEC1 was highly expressed in normal prostate tissues, normal prostatic epithelium cell line (RWPE-1), and benign prostatic hyperplasia cell line (BPH-1), but frequently downregulated by promoter methylation in PrCa cell lines. Pharmacologic demethylation could restore DLEC1 expression. DLEC1 was downregulated in prostate tumor tissues compared with their adjacent non-malignant tissues. DLEC1 was methylated in 76/110 primary tumors, but rarely in benign prostatic hyperplasia tissues. DLEC1 methylation was associated with higher PSA levels (p = 0.016), higher Gleason scores (p = 0.015), and more advanced tumor stages (p = 0.003). Furthermore, DLEC1 methylation was detected in 11/30 urine sediment samples from PrCa patients, but seldom in ones from BPH patients. Ectopic expression of DLEC1 inhibited the colony formation of PrCa cells, through inducing cell apoptosis. DLEC1 also suppressed PrCa cell migration. Moreover, DLEC1 inhibited NF-κB transcription activity in PrCa and HEK293 cells. Taken together, our data demonstrate that DLEC1 functions as a tumor suppressor but is frequently methylated in prostate cancer. DLEC1 methylation is associated with prostate cancer progression, which could be a non-invasive epigenetic biomarker for PrCa diagnosis.
Key messages
• Promoter methylation of DLEC1 is a potential prognostic biomarker for PrCa.
• DLEC1, a functional tumor suppressor, is frequently methylated in PrCa.
• DLEC1 suppresses prostate cancer growth and metastatic behavior.
• DLEC1 mediates tumor-suppressive activities through NF-κB signaling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PrCa), as the most common male malignancy, accounted for the second leading cause of cancer death in men in the USA [1]. With an aging population, changing in lifestyle factors, and better screening methods, the incidence of PrCa detected in China has increased in recent years, which severely affects the life quality and life expectancy of men >50 years old. Epigenetic inactivation of tumor suppressor genes (TSG) by promoter methylation is well recognized to play a crucial role in prostate carcinogenesis [2–4], while the underlying molecular mechanisms involved in PrCa pathogenesis remain elusive.
Multiple TSGs with aberrant promoter methylation have been found in PrCa, such as GSTP1, RASSF1A, RARβ, APC, AR, ESR1, and ESR2 [5–11]. These genes are associated with key cellular pathways, including DNA repair, cell cycle control, hormone response, signal transduction, and tumor invasion [6]. The aberrant promoter methylation of GSTP1, PTGS2 has been shown related to PrCa initiation and progression, suggesting its potential as good biomarkers for early detection and prognosis prediction [10, 12]. Identification of TSGs with aberrant promoter methylation involved in PrCa carcinogenesis will benefit for uncovering molecular heterogeneity of PrCa and providing insights into its biomarker discovery. Due to the poor specificity of current methods (e.g., serum PSA), there is an urgent clinical need to identify more novel biomarkers to improve PrCa diagnosis and treatment.
Deleted in lung and esophageal cancer 1 (DLEC1) is located at 3p22-p21.3 and encodes a 1755-amino acid polypeptide. That chromosomal region has been shown to be a “hot spot” associated with multiple types of cancer development, including prostate cancer [13]. DLEC1 was initially identified as a tumor suppressor gene for esophageal and lung cancers, being frequently inactivated by hemi-zygote deletion and promoter methylation [14]. More recent studies also demonstrated that DLEC1 is silenced by promoter methylation in other common types of tumors, including ovarian, hepatocellular, gastric, renal, and breast carcinomas [15–19]. Furthermore, DLEC1 methylation was identified as an independent marker of poor survival in patients with non-small cell lung carcinoma [20]. All these studies suggested that DLEC1 serves as a tumor suppressor gene and plays an important role in cancer development and progression, while there are no reports about DLEC1 methylation and its biological functions in prostate cancer.
In this study, we investigated whether DLEC1 was a newly identified TSG with aberrant promoter methylation for PrCa. To get this conclusion, we examined DLEC1 expression and methylation in prostate tumor cell lines, primary tumors, and urine sediments and analyzed the relationship between its methylation and clinicopathological features in PrCa patients. We also investigated its tumor-suppressive functions and related mechanisms in PrCa cells.
Materials and methods
Tissue specimen collection
All prostate specimens, including 110 cases of primary PrCa samples and 26 cases of benign prostatic hyperplasia (BPH) samples, were obtained from the urology department, Peking University First Hospital, Beijing, People’s Republic of China, from January 2011 to December 2013. Clinicopathological features of patients were listed in Table 1. All prostate cancer specimens were collected from radical prostatectomy (RP) without adjuvant therapy, and BPH specimens were collected from transurethral resection (TUR), after obtaining patients’ written content, and defined by two urological pathology physicians. Tumor tissues were selected in areas rich in neoplastic cells. Normal kidney and prostate tissue RNA samples were purchased commercially (Stratagene, La Jolla, CA).
Cell lines and drug treatment
Prostate cancer cell lines studied include C4-2, PC3, DU145, and LNCap. The immortalized human prostatic epithelial cell line RWPE-1 and benign prostatic hyperplasia cell line BPH-1 were used as controls. All of these cell lines were originally obtained from the American Type Culture Collection (ATCC, Manassas, VA, USA). The PrCa cell lines and benign prostatic hyperplasia cell line were routinely maintained in RPMI1640 supplemented with 10 % fetal bovine serum (FBS) (Invitrogen, Carlsbad, CA), 1 % penicillin G, and 1 % streptomycin. RWPE-1 was cultured in keratinocyte serum-free medium (K-SFM) supplied with bovine pituitary extract (BPE) and human recombinant epidermal growth factor (EGF) (Invitrogen, Carlsbad, CA). All these cell lines were cultured at 37 °C in humidified CO2 (5 %) incubator. For demethylation treatment, PrCa cells were diluted to 1 × 105/ml and incubated overnight. Fresh medium containing 10 μM 5-aza-2-deoxycytidine (Aza) (Sigma, St. Louis. MO) was changed every 24 h. After Aza treatment for 3 days or an additional 24-h treatment with 100-nM Trichostatin A (TSA), the cells were harvested for further analysis.
DNA and RNA extraction
Total RNA was isolated from tissues and cell lines using TRI Reagent (Molecular Research Center, Cincinnati, OH), as previously described [21]. Genomic DNA was extracted according to the protocol supplied by QIAamp DNA Mini Kit (Qiagen GmbH, Hilden, Germany).
Semi-quantitative RT-PCR and real-time PCR analysis
Semi-quantitative real-time PCR (RT-PCR) was used to detect gene expression with GoTaq® Green Master Mix (Promega, Madison, WI, USA). The primers used were DLEC1A: 5’-TCCGGATCCCTTGGAAACAC-3′ and DLEC1B: 5′-CCTCAGGAACAATTCGGTAA-3′, which were performed for 36 cycles (94 °C for 30 s, 53 °C for 30 s, and 72 °C for 30 s). Real-time PCR was performed to detect DLEC1 expression in primary prostate tumors, according to the manufacturer’s protocol (HT7500 system, Applied Biosystems). The primers used were DLEC1LCF: 5′-CACGGAAGAGGCATCG-3′ and DLEC1LCR: 5′-ATAAGCCGGAAGTAGTGT-3′. Real-time PCR was done for 45 cycles (94 °C for 30 s, 55 °C for 30 s, and 72 °C for 30 s). GAPDH was used as an internal control.
Bisulfite treatment and promoter methylation analysis
Sodium bisulfite conversion of genomic DNA was performed as described previously [22, 23]. Methylation-specific PCR (MSP) was used to detect promoter methylation of DLEC1. The MSP primers used for DLEC1 were DLEC1m1: 5′-GTTTCGTAGTTCGGTTTCGTC-3′, DLEC1m2: 5′-CGAAATATCTTAAATACGCAACG-3′, DLEC1u1: 5′-TAGTTTTGTAGTTTGGTTTTGTT-3′, and DLEC1u2: 50-ACAAAATATCTTAAATACACAACA-3′. The detailed methylation information was analyzed by bisulfite genomic sequencing (BGS). The BGS primers were DLEC1BGS56: 5′-GGGTTTAGTAGTTTTAGTTAG-3′ and DLEC1BGS4: 5′-CAACTACAACCCCAAATCCTAA-3′. The bisulfite-treated DNA was used as a template for MSP and BGS. Forty cycles of PCR were performed using GoTaq®Hot Start Green Master Mix (Promega, Madison, WI). The BGS PCR products were cloned into the pEASY-T5 zero vectors (TransGen Biotech Co., Ltd, Beijing), and 5–8 colonies were randomly chosen and sequenced.
Urine sediments preparation and MSP analysis
The first voided urine samples after digital rectal examination (DRE) were collected from PrCa patients undergoing RP and BPH patients undergoing TUR. Urine sediments were immediately prepared after collection to obtain good sample quality according to Hessels’s report [24]. In brief, the urine was centrifuged at 4 °C at 1000 × g for 10 min. The obtained urine sediments was suspended in 1 ml of PBS buffer and transferred to a 1.5-ml microcentrifuge tube. After centrifuging at 4 °C at 10,000 × g for 10 min, sediment was obtained and then stored at −70 °C. For bisulfite conversion, 1∼13 μl of sediments were used and directly converted to bisulfited DNA according to the handbook of EZ DNA Methylation-Direct Kit (Zymo research, Inc., Irvine, CA). One microliter of bisulfite-treated DNA was used for MSP, conducted at 95 °C for 10 min, then 41 cycles (94 °C, 30 s; 58 °C, 30 s; 72 °C, 30 s), followed by 72 °C for 5 min.
Immunohistochemistry
Nine paraffin-embedding primary prostate tumor and their paired adjacent non-malignant tissues were used to examine DLEC1 expression by immunohistochemistry (IHC). The slides were deparaffinized in xylene, rehydrated in a concentration decreasing ethanol series, subsequently boiled for 2 min in citrate buffer (pH 6.0) for antigen retrieval, and stained by anti-DLEC1 antibody produced in rabbit, a Prestige Antibody (Sigma, St. Louis. MO) in a 1:100 dilution. Antibody binding was visualized using ChemMate Envision kit (Dako, Hamburg, Germany). Immunostaining was assessed by two urological pathologists (He Qun and Shen Qi) in a blinded manner and scored from 0 to 3 depending on the intensity of staining (none = 0; weak = 1; moderate = 2; strong = 3).
Colony formation assay
To assess tumor cell clonogenicity, colony formation assay was used. Briefly, 1.5 × 105 cells were plated in a 12-well plate and incubated overnight. Then the cells were transfected with DLEC1 expression construct or the empty vector using Lipofectamine 2000 (Invitrogen, Carlsbad, CA). After 48 h, the transfectants were replated in triplicate in a 6-well plate and selected with G418 for 10–15 days. The best selective concentration of G418 for PC3, DU145, and LNCap cells were 0.1, 0.2, and 0.3 mg/ml, respectively. Visible colonies (≥50 cells) were stained with gentian violet after methanol fixation and counted.
Annexin V Apoptosis assay
The PrCa cells transfected with DLEC1-expressing vectors or empty vectors were harvested after transfection for 48 h. Then the cells were fixed in 75 % ethanol, stained with Annexin V-FITC and 7-AAD (BD Biosciences, Bedford, MA), and sorted by Becton Dickinson LSRII (BD Biosciences, Bedford, MA) according to the manufacturer’s protocol. The data were analyzed using Flow Jo software (BD Biosciences), and the Annexin V-FITC-positive cells were counted as apoptotic cells.
Wound-healing assay
The cell motility was assessed by scratch wound healing assay. DU145 cells (2–3 × 106 per well) were plated in a 6-well plate for 1 day and then transfected with DLEC1 expression vectors or the control vectors for 24 h. The cell layers were washed with PBS after carefully scratching by sterile tips. After incubation for 0, 24, and 48 h, photos were taken. The assays were performed in triplicate.
Transwell migration assay
The PrCa cells (DU145 and LNCap) were placed on the upper layer of a cell permeable membrane after transfection with DLEC1 expression vector or control vector for 24 h. Following another 24–48 h incubation, the cells migrated through the membrane were stained with 1 % Crystal Violet and counted.
Western blot
PrCa cells were transiently transfected with DLEC1 expression vector or empty vector for 48 h then lysed in ice-cold lysis buffer containing 137 nmol/L of NaCl, 2 mmol/L of EDTA, 1 % Triton X, 10 % glycerol, 50 mmol/L of NaF, 1 mmol/L of DTT, and a protease inhibitor cocktail (Roche Applied Science, Mannheim, Germany). Cell lysates were separated by SDS-PAGE and transferred to nitrocellulose membrane. The membranes were probed with the following antibodies after blocking with 5 % milk: cleaved PARP (Cell Signaling Technology Inc., Beverly, MA), Flag (Sigma, St. Louis. MO), and NF-κB/p65 (Cell Signaling Technology Inc., Beverly, MA). The blots were visualized using the enhanced chemiluminescence (ECL) Western blotting detection system (Thermo Scientific).
Dual-luciferase reporter assay
Luciferase reporters of several key signaling pathways, including p53bs-luc, p21p-luc, NF-κBbs-luc, and MYCp-luc, were used to screen for a signaling pathway modulated by DLEC1. Cells were transiently co-transfected with DLEC1 expression vector, phRL-TK, the luciferase reporters, or empty vector. After 48 h, the cells were lysed and the luciferase activities were measured using Dual-Luciferase® Reporter Assay System (Promega, Madison, WI, USA). To normalize transfection efficiency, phRL-TK luciferase activities were measured as an internal control. At least three independent experiments were carried out, and each experiment was repeated in triplicates.
Statistical analysis
Statistical analyses were done using the two-tailed t test, Fisher exact test, or chi-square test to determine p values, in which <0.05 is considered significant.
Results
DLEC1 is downregulated in primary prostate tumor samples
We firstly evaluated DLEC1 expression in prostate tumor tissues. Quantitative RT-PCR was used to evaluate messenger RNA (mRNA) expression level of DLEC1 in eight cases of primary prostate cancer and their paired adjacent non-malignant tissues. Compared with the adjacent non-malignant tissues, DLEC1 was significantly downregulated in prostate tumor tissues (p < 0.05; Fig. 1a). The protein expression of DLEC1 was further detected by IHC in another nine cases of paired prostate tumor samples. Results showed that DLEC1 was highly expressed in adjacent non-malignant tissues, but reduced in prostate tumor tissues (p < 0.05; Fig. 1b). These results indicate that DLEC1 may be a potential TSG for prostate cancer.
DLEC1 mRNA and protein expression in prostate tissues. a Real-time PCR was performed to detect mRNA expression levels of DLEC1 in eight paired human prostate cancer tissues and their adjacent non-malignant prostate tissues.*p < 0.05. b Expression of DLEC1 in representative adjacent non-malignant tissues and prostate cancer tissues by immunohistochemistry. **p < 0.01
DLEC1 is frequently silenced by promoter methylation in PrCa cell lines
We then examined mRNA expression level of DLEC1 in PrCa cell lines (C4-2, DU145, PC3, and LNCaP) and found that DLEC1 was silenced or reduced in these cell lines. In contrast, DLEC1 was highly expressed in normal human prostate tissue, immortalized prostate epithelial cell line RWPE-1, and benign prostatic hyperplasia cell line BPH-1 (Fig. 2a). As described in our previous report, there is a typical CpG island at promoter and exon 1 region of DLEC1 [18]. We thus hypothesize that the promoter methylation may be responsible for DLEC1 downregulation or silencing in PrCa cells. We next examined DLEC1 methylation in PrCa cell lines. MSP showed that DLEC1 was completely methylated in DU145, C4-2, LNCap, and PC3 cells, whereas unmethylated in RWPE-1 and BPH-1 cells (Fig. 2a), consistent with its silencing. BGS analysis further confirmed the MSP results (Fig. 2c). These data suggest that aberrant promoter methylation contributes to DLEC1 silencing in PrCa cells.
a DLEC1 is frequently silenced and methylated in PrCa cell lines (C4-2, PC3, DU145, and LNCap), but highly expressed and unmethylated in immortalized normal prostate epithelial cell line RWPE-1 and benign prostatic hyperplasia cell line BPH-1. M methylated, U unmethylated. b Pharmacological demethylation with Aza (A) alone or combined with TSA (A + T) restored DLEC1 expression in PrCa cell lines (PC3, DU145, and LNCap). c Detailed BGS analyses of the DLEC1 promoter in PrCa cell lines with or without demethylation treatment. Filled circle represents the methylated while open circle the unmethylated
Pharmacologic demethylation restores DLEC1 expression in PrCa cell lines
To determine whether DLEC1 expression was directly repressed by promoter methylation, PrCa cell lines with methylated and reduced DLEC1 (DU145, PC3, and LNCap) were treated with DNA methylation inhibitor Aza alone or combined with the HDAC inhibitor TSA. As shown in Fig. 2, DLEC1 expression was restored after demethylation treatments, accompanied by an increase of unmethylated alleles and a decrease of methylated alleles. Detailed BGS analysis further confirmed DLEC1 demethylation (Fig. 2c). These results suggest that promoter methylation directly mediates DLEC1 downregulation in PrCa cells.
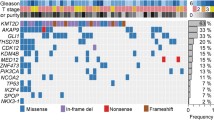
DLEC1 methylation in primary prostate tumors
DLEC1 methylation was further analyzed in 110 primary PrCa samples and 26 BPH samples. MSP analysis showed that DLEC1 methylation was detected in 76 out of 110 PrCa tissues, but seldom in BPH tissues (2 out of 26) (Fig. 3a, b). In addition, the high-solution BGS results showed densely methylated CpG sites in two representative primary tumors, but only scattered methylated alleles in three representative BPH tissues (Fig. 3d). Thus, DLEC1 methylation is a frequent event in PrCa tumorigenesis. We further detected DLEC1 methylation in urine samples from 30 PrCa patients and 30 BPH patients. Results showed that DLEC1 was methylated in 11 out of 30 urine sediments of PrCa samples but rarely in BPH urine sediments samples (Fig. 3c), indicating that DLEC1 methylation is a potential non-invasive marker for PrCa.
DLEC1 methylation is associated with poor prognosis of PrCa patients
We further evaluated the relationship between DLEC1 methylation and clinicopathological features of PrCa patients. As shown in Table 1, there was no significant difference between DLEC1 methylation and age, while DLEC1 methylation was detected in patients with higher PSA levels (p = 0.016), higher Gleason scores (p = 0.015), and more advanced tumor stages (p = 0.003), which showed a statistically significant difference. These results indicate that DLEC1 methylation is correlated with poor prognosis of PrCa.
DLEC1 is a functional tumor suppressor in PrCa cells
To investigate the tumor-suppressive functions of DLEC1 in PrCa, we examined the colonogenecity of PrCa cells by colony formation assay. DLEC1 expression vector and empty vector were transfected to PrCa cell lines (PC3, DU145, and LNCap) with reduced DLEC1. The abilities of colony formation were significantly inhibited in DLEC1-expressing prostate tumor cells compared with control ones (Fig. 4a). Re-expression of DLEC1 mRNA in these cells was confirmed by RT-PCR (Fig. 4b).
Tumor suppressive functions of DLEC1 in PrCa cells. a DLEC1 inhibits tumor cell growth by colony formation assay. Quantitative analyses of colony numbers in three replicates were shown as values of mean ± s.d., **p < 0.01. b DLEC1 expression was detected by RT-PCR in DLEC1- or vector- transfected cells, with GAPDH as a control. c DLEC1 induced apoptosis of prostate tumor cells (PC3, DU145, and LNCap) by Annexin V-PE and 7-AAD double staining. d Representative flow cytometry plots. *p < 0.05, **p < 0.01. e Western blot showed that increased cleaved PARP in DLEC1-expressing DU145, PC3, and LNCap cells. DLEC1 expression was probed by Flag-tag antibody, GAPDH was used as a control
To examine whether DLEC1-mediated growth inhibition was the result of apoptosis, cell apoptosis was determined in PrCa cell lines (DU145, PC3, and LNCap) by Annexin V-PE and 7-AAD double staining. Results showed that the number of total apoptotic cells significantly increased in the cells transiently transfected with DLEC1 expression vector compared with their controls (Fig. 4c, d). We further checked the classic apoptotic marker cleaved PARP by Western blot and found that cleaved PARP was obviously increased in DLEC1-expressing DU145, PC3, and LNCap cells (Fig. 4e).
We further evaluated the migration ability of DLEC1 in PrCa cells by wound healing and transwell migration assays. The scratch wound healing assay showed that DLEC1-expressing DU145 cells closed the wound much slower than controls (Fig. 5a). The transwell migration assay showed that ectopic expression of DLEC1 significantly inhibited the migration abilities of DU145 and LNCap cells. These data suggest that DLEC1 acts as a functional TSG in PrCa cells through inhibiting tumor cell colonogenecity and migration.
DLEC1 inhibits NF-κB signaling in PrCa cells
To elucidate the molecular mechanisms of DLEC1 in tumor suppression in PrCa, we examined several signaling pathways involved in apoptosis (p53bs), cell cycle (p21), and cell proliferation (NF-κBbs, MYCp) in HEK293 by luciferase reporter assay. DLEC1 could activate p53 signaling and downregulate NF-κB signaling pathway in HEK293 cells (Fig. 6a). We then detected NF-kB transcriptional activity in PrCa cell lines and found that NF-kB signaling was also significantly inhibited in DLEC1-expressing DU145, PC3, and LNCap cells (Fig. 6b), together with a decreased NF-κB (p65) protein level (Fig. 6c).
DLEC1 inhibited NF-κB signaling in PrCa cells. a The effect of DLEC1 on several signaling pathways in HEK293 cells as measured by luciferase reporter assay. b NF-κB transcriptional activity was inhibited in DLEC1-expressing PrCa cells by dual-luciferase reporter assay in three replicates, *p < 0.05. c NF-κB/p65 downregulation was detected by Western blot in DLEC1-expressing DU145, PC3, and LNCap cells. DLEC1 expression was detected by Flag antibody. GAPDH was used as a control
Discussion
Despite improved screening methods for PrCa and advances in the treatment of progressive disease, PrCa remains the most common cause of cancer death for men. Thereby, early detection and monitoring of this disease may improve its prognosis and treatment. DNA methylation has been recognized as a hallmark of cancer, which helps to uncover the molecular mechanisms underlying tumor development and provide molecular screening strategies to identify cancer-specific diagnostic and prognostic tools [25, 26]. Recently, DNA methylation detection in tissues and body fluids could serve as feasible tumor markers [27–30].
In this study, we identified DLEC1 as a functional TSG silenced by promoter methylation in PrCa, which implies a potential biomarker for PrCa. Silencing of DLEC1 by promoter CpG methylation has been identified to be involved in multiple carcinogenesis including nasopharyngeal, esophagus, lung, gastric, hepatocellular, colon, and renal [14–19], suggesting that it could be an epigenetic biomarker for the molecular diagnosis and prognosis prediction of these tumors. We found that DLEC1 was frequently silenced by promoter methylation in PrCa cell lines but not in BPH cells and normal prostate epithelial cells. After being treated with demethylation drugs in DLEC1-methylated PrCa cells, we found that pharmacologic demethylation could reactivate its expression. DLEC1 methylation was also frequently detected in PrCa patients, but rarely in BPH tissues. Moreover, DLEC1 methylation in PrCa was associated with serum PSA level, Gleason score, and advanced stage, suggesting its potential as a prognostic predictor for PrCa. Remarkably, DLEC1 methylation was examined in PrCa urine sediments samples, indicating that it could be a non-invasive tumor marker for PrCa. Furthermore, a large-scale clinical validation in body fluids from PrCa patients is currently underway in our department to investigate the role of DLEC1 in prostate cancer metastasis and confirm it as a methylation marker for PrCa diagnosis.
Recent studies showed that DLEC1 as a TSG participates in the pathogenesis of multiple cancers and regulates cell proliferation [14, 17]. In this study, the tumor-suppressive functions of DLEC1 were found in PrCa cells, including the inhibition of cell proliferation, migration, and induction of apoptosis. As the programmed cell death can also be measured by loss of colony-forming ability, thus, DLEC1 likely inhibits colony formation of prostate tumor cells partially through inducing apoptosis. Moreover, the molecular mechanism of DLEC1 was further explored. DLEC1 inhibited NF-κB signaling in PrCa cells, suggesting that DLEC1 may exert its tumor-suppressive function through regulating NF-κB signaling pathway. Aberrant NF-κB activation has been reported to be associated with the initiation and progression of many cancers, including prostate cancer. NF-κB signaling activation was implicated in the progression of prostate cancer, which might be employed as a novel therapeutic target [31–34]. As LNCaP/C4-2 is an ideal model of prostate cancer progression, a further in-depth investigation of the mechanisms of DLEC1 in prostate cancer metastasis will be carried out using LNCaP/C4-2 model.
In summary, we found that DLEC1 is a functional TSG in PrCa, and its frequent methylation is associated with tumor poor prognosis of PrCa, which could serve as a potential tumor marker for PrCa.
Abbreviations
- Aza:
-
5-Aza-2-deoxycytidine
- ATCC:
-
The American Type Culture Collection
- BGS:
-
Bisulfite genomic sequence
- BPH:
-
Benign prostatic hyperplasia
- DLEC1:
-
Deleted in lung and esophageal cancer
- DRE:
-
Digital rectal examination
- FBS:
-
Fetal bovine serum
- IHC:
-
Immunohistochemistry
- MSP:
-
Methylation specific polymerase chain reaction
- PrCa:
-
Prostate cancer
- RT-PCR:
-
Reverse-transcription polymerase chain reaction
- RP:
-
Radical prostatectomy
- TSA:
-
Trichostatin A
- TSG:
-
Tumor suppressor gene
- TUR:
-
Transurethral resection
References
Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63:11–30
Barbieri CE, Baca SC, Lawrence MS, Demichelis F, Blattner M, Theurillat JP, White TA, Stojanov P, Van Allen E, Stransky N et al (2012) Exome sequencing identifies recurrent SPOP, FOXA1 and MED12 mutations in prostate cancer. Nat Genet 44:685–689
Mahapatra S, Klee EW, Young CY, Sun Z, Jimenez RE, Klee GG, Tindall DJ, Donkena KV (2012) Global methylation profiling for risk prediction of prostate cancer. Clin Cancer Res 18:2882–2895
Hoque MO (2009) DNA methylation changes in prostate cancer: current developments and future clinical implementation. Expert Rev Mol Diagn 9:243–257
Henrique R, Jeronimo C (2004) Molecular detection of prostate cancer: a role for GSTP1 hypermethylation. Eur Urol 46:660–669
Jeronimo C, Bastian PJ, Bjartell A, Carbone GM, Catto JW, Clark SJ, Henrique R, Nelson WG, Shariat SF (2011) Epigenetics in prostate cancer: biologic and clinical relevance. Eur Urol 60:753–766
Kuzmin I, Gillespie JW, Protopopov A, Geil L, Dreijerink K, Yang Y, Vocke CD, Duh FM, Zabarovsky E, Minna JD et al (2002) The RASSF1A tumor suppressor gene is inactivated in prostate tumors and suppresses growth of prostate carcinoma cells. Cancer Res 62:3498–3502
Millar DS, Ow KK, Paul CL, Russell PJ, Molloy PL, Clark SJ (1999) Detailed methylation analysis of the glutathione S-transferase pi (GSTP1) gene in prostate cancer. Oncogene 18:1313–1324
Tian J, Lee SO, Liang L, Luo J, Huang CK, Li L, Niu Y, Chang C (2012) Targeting the unique methylation pattern of androgen receptor (AR) promoter in prostate stem/progenitor cells with 5-aza-2′-deoxycytidine (5-AZA) leads to suppressed prostate tumorigenesis. J Biol Chem 287:39954–39966
Yegnasubramanian S, Kowalski J, Gonzalgo ML, Zahurak M, Piantadosi S, Walsh PC, Bova GS, De Marzo AM, Isaacs WB, Nelson WG (2004) Hypermethylation of CpG islands in primary and metastatic human prostate cancer. Cancer Res 64:1975–1986
Zhang J, Liu L, Pfeifer GP (2004) Methylation of the retinoid response gene TIG1 in prostate cancer correlates with methylation of the retinoic acid receptor beta gene. Oncogene 23:2241–2249
Enokida H, Shiina H, Urakami S, Igawa M, Ogishima T, Pookot D, Li LC, Tabatabai ZL, Kawahara M, Nakagawa M et al (2005) Ethnic group-related differences in CpG hypermethylation of the GSTP1 gene promoter among African-American, Caucasian and Asian patients with prostate cancer. Int J Cancer 116:174–181
Hesson LB, Cooper WN, Latif F (2007) Evaluation of the 3p21.3 tumour-suppressor gene cluster. Oncogene 26:7283–7301
Daigo Y, Nishiwaki T, Kawasoe T, Tamari M, Tsuchiya E, Nakamura Y (1999) Molecular cloning of a candidate tumor suppressor gene, DLC1, from chromosome 3p21.3. Cancer Res 59:1966–1972
Kwong J, Lee JY, Wong KK, Zhou X, Wong DT, Lo KW, Welch WR, Berkowitz RS, Mok SC (2006) Candidate tumor-suppressor gene DLEC1 is frequently downregulated by promoter hypermethylation and histone hypoacetylation in human epithelial ovarian cancer. Neoplasia 8:268–278
Qiu GH, Salto-Tellez M, Ross JA, Yeo W, Cui Y, Wheelhouse N, Chen GG, Harrison D, Lai P et al (2008) The tumor suppressor gene DLEC1 is frequently silenced by DNA methylation in hepatocellular carcinoma and induces G1 arrest in cell cycle. J Hepatol 48:433–44117
Ying J, Poon FF, Yu J, Geng H, Wong AH, Qiu GH, Goh HK, Rha SY, Tian L, Chan AT et al (2009) DLEC1 is a functional 3p22.3 tumour suppressor silenced by promoter CpG methylation in colon and gastric cancers. Brit J Cancer 100:663–669
Zhang Q, Ying J, Li J, Fan Y, Poon FF, Ng KM, Tao Q, Jin J (2010) Aberrant promoter methylation of DLEC1, a critical 3p22 tumor suppressor for renal cell carcinoma, is associated with more advanced tumor stage. J Urol 184:731–737
Al Sarakbi W, Reefy S, Jiang WG, Roberts T, Newbold RF, Mokbel K (2010) Evidence of a tumour suppressor function for DLEC1 in human breast cancer. Anticancer Res 30:1079–1082
Seng TJ, Currey N, Cooper WA, Lee CS, Chan C, Horvath L, Sutherland RL, Kennedy C, McCaughan B, Kohonen-Corish MR (2008) DLEC1 and MLH1 promoter methylation are associated with poor prognosis in non-small cell lung carcinoma. Brit J Cancer 99:375–382
Jin H, Wang X, Ying J, Wong AH, Cui Y, Srivastava G, Shen ZY, Li EM, Zhang Q, Jin J et al (2007) Epigenetic silencing of a Ca(2+)-regulated Ras GTPase-activating protein RASAL defines a new mechanism of Ras activation in human cancers. Proc Natl Acad Sci U S A 104:12353–12358
Tao Q, Robertson KD, Manns A, Hildesheim A, Ambinder RF (1998) The Epstein-Barr virus major latent promoter Qp is constitutively active, hypomethylated, and methylation sensitive. J Virol 72:7075–7083
Tao Q, Swinnen LJ, Yang J, Srivastava G, Robertson KD, Ambinder RF (1999) Methylation status of the Epstein-Barr virus major latent promoter C in iatrogenic B cell lymphoproliferative disease. Application of PCR-based analysis. Am J Pathol 155:619–625
Hessels D, Klein Gunnewiek JM, van Oort I, Karthaus HF, van Leenders GJ, van Balken B, Kiemeney LA, Witjes JA, Schalken JA (2003) DD3(PCA3)-based molecular urine analysis for the diagnosis of prostate cancer. Eur Urol 44:8–15
Baylin SB (2012) The cancer epigenome: its origins, contributions to tumorigenesis, and translational implications. Proc Am Thorac Soc 9:64–65
Jones PA, Baylin SB (2007) The epigenomics of cancer. Cell 128:683–692
Ahmed H (2010) Promoter Methylation in prostate cancer and its application for the early detection of prostate cancer using serum and urine samples. Biomarker Cancer 2010:17–33
Cairns P, Esteller M, Herman JG, Schoenberg M, Jeronimo C, Sanchez-Cespedes M, Chow NH, Grasso M, Wu L, Westra WB et al (2001) Molecular detection of prostate cancer in urine by GSTP1 hypermethylation. Clin Cancer Res 7:2727–2730
Truong M, Yang B, Jarrard DF (2013) Toward the detection of prostate cancer in urine: a critical analysis. J Urol 189:422–429
Gyparaki MT, Basdra EK, Papavassiliou AG (2013) DNA methylation biomarkers as diagnostic and prognostic tools in colorectal cancer. J Mol Med 91:1249–1256
Garg R, Blando J, Perez CJ, Wang H, Benavides FJ, Kazanietz MG (2012) Activation of nuclear factor kappaB (NF-kappaB) in prostate cancer is mediated by protein kinase C epsilon (PKCepsilon). J Biol Chem 287:37570–37582
McCall P, Bennett L, Ahmad I, Mackenzie LM, Forbes IW, Leung HY, Sansom OJ, Orange C, Seywright M, Underwood MA et al (2012) NFkappaB signalling is upregulated in a subset of castrate-resistant prostate cancer patients and correlates with disease progression. Br J Cancer 107:1554–1563
Nguyen DP, Li J, Yadav SS, Tewari AK (2014) Recent insights into NF-kappaB signalling pathways and the link between inflammation and prostate cancer. BJU Int 114:168–176
Zhang L, Altuwaijri S, Deng F, Chen L, Lal P, Bhanot UK, Korets R, Wenske S, Lilja HG, Chang C et al (2009) NF-kappaB regulates androgen receptor expression and prostate cancer growth. Am J Pathol 175:489–499
Acknowledgments
This study was supported by grants from the National Natural Science Foundation (No. 81272290, 81171971, 81372898 and 81101492), Beijing Municipal Science and Technology Commission (No.Z131107002213130 and Z121107002512012), Central Health Care Research Foundation (No. W2013BJ28), Shenzhen city (GJHS20120702105523309), and China 973 Program (2012CB518305).
Conflicts of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Lian Zhang and Qian Zhang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, L., Zhang, Q., Li, L. et al. DLEC1, a 3p tumor suppressor, represses NF-κB signaling and is methylated in prostate cancer. J Mol Med 93, 691–701 (2015). https://doi.org/10.1007/s00109-015-1255-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-015-1255-5