Abstract
Background
The LMA SupremeTM (LMA-S) and i-gelTM are two of the most commonly used supraglottic airway devices (SADs) with an inbuilt drain channel. These devices are particularly indicated for performing certain procedures accompanied by high peak airway pressure, such as laparoscopy. This study compared the devices regarding efficacy, safety, ease of use and incidence of adverse events, focusing on the postoperative rate of sore throat, dysphagia or dysphonia and development with time, in patients undergoing laparoscopic cholecystectomy procedures under general anesthesia.
Methods
This was a prospective, randomized, controlled clinical study including 140 patients randomized into 2 groups undergoing elective laparoscopic cholecystectomy to use either i-gel or LMA-S. After the general anesthesia procedure, the speed of insertion, success rates, ease of insertion of the drain tube, leak pressure and tidal volume achieved by the devices were evaluated. The postoperative oropharyngeal discomfort (POPD) during the period of stay of the patients in the recovery room was also recorded.
Results
The mean leak pressure was comparable between the two groups (i-gel 28.18 ± 3.90 cmH2O and LMA-S 27.50 ± 4 cmH2O, p = 0.09), as well as maximum expiratory tidal volume provided (i-gel 559.60 ± 45.25 ml and LMA-S 548.95 ± 56.18 ml, p = 0.12). Insertion times were lower for the i-gel (10 ± 1.62 s) compared with the LMA-S (11.31 ± 2.85 s, p = 0.008). Insertion success rate at the first attempt was higher for the LMA-S (95 % compared with i-gel 79 %, p = 0.007). Drain tubes were easier to insert in the LMA-S group (p < 0.001). No differences were found between groups relating to intraoperative complications. Frequency of coughing and visible blood on removal of the device were low and comparable in both groups (p = 0.860 and p = 0.623, respectively). There were no differences relating to the incidence of sore throat, dysphagia or hoarseness at 10 min postoperatively between groups (p = 0.088). The i-gel group complained about a higher sore throat score at 2 h postoperatively (p = 0.009), specifically patients receiving i-gel suffered more from sore throats with 0.24 more points on the visual analog scale (VAS) than patients from the LMA-S group. The i-gel group also reported a lower POPD drop during the first 2 h (p < 0.001).
Conclusion
No differences were found between i-gel and LMA-S regarding leak pressure in the groups of anesthetized patients undergoing laparoscopic cholecystectomy. The LMA-S was easier to insert than the i-gel (based on its better first time success rate) and this device showed better ease of drain tube insertion, although the i-gel was quicker to insert than the LMA-S. The i-gel resulted in higher sore throat scores at 2 h postoperatively and lower POPD reduction during the 2 h period studied in the recovery room was reported.
Zusammenfassung
Hintergrund
LMA SupremeTM (LMA-S) und i-gelTM sind 2 der am häufigsten verwendeten supraglottischen Beatmungsgeräte mit eingebautem Magensaftablaufkanal. Sie sind besonders indiziert bei Interventionen, bei denen es zu hohen Spitzen im Atemwegsdruck kommt, etwa bei Laparoskopien. In der Studie wurden Wirksamkeit, Sicherheit, Benutzerfreundlichkeit und die Inzidenz von unerwünschten Ereignissen verglichen. Besondere Beachtung erfuhren dabei die Raten an postoperativ auftretenden Halsschmerzen, Dysphagie oder Dysphonie und der Entwicklung im zeitlichen Verlauf bei Patienten nach laparoskopischer Cholezystektomie in Allgemeinnarkose.
Methoden
In die prospektive, kontrollierte klinische Studie wurden 140 Patienten aufgenommen, die sich einer elektiven laparoskopischen Cholezystektomie unterzogen; sie wurden randomisiert auf 2 Gruppen und mit i-gel oder LMA-S intubiert. Nach Allgemeinanästhesie wurden evaluiert: Geschwindigkeit der Einführung, Erfolgsraten, Benutzerfreundlichkeit hinsichtlich der Einführung der Magensonde über den Ablaufkanal, Dichtheitsdruck und Atemvolumen. Darüber hinaus wurden postoperative oropharyngeale Beschwerden („postoperative oropharyngeal discomfort“, POPD) der Patienten während des Aufenthalts im Aufwachraum dokumentiert.
Ergebnisse
Dichtheitsdruck (i-gel 28,18 ± 3,90; LMA-S 27,50 ± 4 cm H2O, p = 0,09) und maximales exspiratorisches Atemvolumen (i-gel 559,60 ± 45,25; LMA-S 548,95 ± 56,18 ml, p = 0,12) waren in beiden Gruppen vergleichbar. Die Einführungszeiten waren beim i-gel niedriger als beim LMA-S (10 ± 1,62 vs. 2,85 ± 11,31 s, p = 0,008). Die Einführungerfolgsquote beim ersten Versuch war höher beim LMA-S (95 % vs. i-gel: 79 %, p = 0,007). Die Platzierung einer Magensonde über den Ablaufkanal wurde als einfacher in der LMA-S-Gruppe (p < 0,001) beurteilt. Hinsichtlich intraoperativer Komplikationen wurden keine Gruppenunterschiede beobachtet. Husten und Blutspuren bei Entfernung der Geräte waren selten und in beiden Gruppen vergleichbar (p = 0,860 bzw. p = 0,623). Zehn Minuten postoperativ gab es keine Gruppenunterschiede (p = 0,088) in der Inzidenz von Halsschmerzen, Dysphagie und Heiserkeit. In der i-gel-Gruppe zeigten sich höhere Werte in den Angaben zu Halsschmerzen 2 h postoperativ (p = 0,009), vor allem litten die i-gel-Patienten mehr an Halsschmerzen (0,24 mehr auf der visuellen Analogskala, VAS) als die Patienten der LMA-S-Gruppe. In der i-gel-Gruppe verringerten sich die POPD in den ersten 2 postoperativen Stunden weniger (p < 0,001).
Schlussfolgerungen
Zwischen i-gel und LMA-S wurden im Hinblick auf den Dichtheitsdruck keine Unterschiede gefunden. LMA-S war leichter einzuführen als i-gel (auf der Basis der besseren initialen Erfolgsrate), und bei diesem Geräte war das Einführen der Magensonde leichter, auch wenn i-gel schneller einzusetzen waren als LMA-S. Nach i-gel wurden 2 h postoperative höhere Halsschmerzenscores angegeben und eine geringere POPD-Verringerung während der 2 h im Aufwachraum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
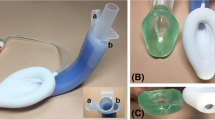
The Laryngeal Mask Airway Classic™ (LMA-C) is the most widely studied supraglottic airway device (SAD) and since it was introduced, several devices have been incorporated in order to improve the SAD indications, some of them with incorporation of a gastric access. There are six SADs with a drain tube available on the market at present: the Laryngeal Tube Suction™ (LTS or LTS-D if disposable), LMA Proseal™ (LMA-P), LMA Supreme™ (LMA-S), i-gel™ and recently Guardian CPV™, Baska Mask™ and Ambu AuraGain™. The LMA-P, LMA-S and i-gel are the most commonly used devices with gastric access in clinical anesthesia. These devices are a suitable choice when performing anesthesia for procedures accompanied by high peak airway pressure, such as laparoscopy. In addition, the drain channel helps to identify the correct tip position just after insertion [1]. Over the last 10 years some studies have been performed in order to establish the safety of SADs with gastric access for this purpose. In this sense, a number of studies have been performed with LMA-P [2, 3] and LMA-S [4–7] but only a few articles were identified evaluating i-gel for laparoscopic procedures [5, 8, 9]. The LMA-S and i-gel were compared in patients undergoing gynecological laparoscopy [5] but to the best of our knowledge this is the first report comparing these two devices for laparoscopic cholecystectomy.
This article presents a prospective and randomized study of 140 patients undergoing elective laparoscopic cholecystectomy, comparing the use of LMA-S and i-gel and evaluating in detail the safety, efficacy and ease of use. The incidence of adverse events was also compared focusing on the postoperative rate of sore throat, dysphagia or dysphonia and development over time. The primary endpoints were to measure leak pressure, speed of insertion and success rates. The secondary endpoints were to evaluate the margin on leak pressure (MLP), a concept related to feasibility of SADs during laparoscopy. This parameter was defined as the margin of pressure (measured in cmH2O) between the highest peak airway pressure (PAW-pk) achieved during pneumoperitoneum and the leak pressure value. The development of postoperative oropharyngeal discomfort (POPD) during the patient stay in the postanesthesia care unit (PACU).
Material and methods
This study was approved by the local research ethics committee of the Hospital Universitario del Sureste, Arganda del Rey, Madrid, Spain (Chairperson Dr. F.J. Yuste, registration number: HUSE 02-0005) on 15 September 2009. Written informed consent was obtained from all participants and recruitment ended on 30 June 2012. A total of 140 adult patients scheduled for elective laparoscopic cholecystectomy were prospectively randomized. Patients were excluded if they presented with an American Society of Anesthesiologists (ASA) classification of physical status score of 4 or higher, a BMI ≥ 40 kg/m2, severe gastroesophageal reflux disease or known risk of aspiration. Patients were randomly assigned using computer generated random numbers to one of the two groups, to be managed with either i-gel or LMA-S as SAD. Patients were premedicated with midazolam 0.03 mg kg−1 body weight and remifentanil 0.1 μg kg−1.min−1 intravenously and connected to standard anesthesia monitoring equipment. Airway management was performed by five senior anesthesiologists who had performed more than 200 LMA-S and 100 i-gel insertions. Prior to the induction all patients underwent preoxygenation and were placed in the supine position. Anesthesia was induced with intravenous remifentanil 0.3 μg kg−1 min−1 and propofol 2–3 mg kg−1 but no neuromuscular blocking drugs were used at this time. After optimum conditions for SAD insertion were achieved (i.e. relaxation of the jaws, loss of eyelash reflex and onset of apnea) either i-gel or LMA-S was introduced. The selection of the size was based on the manufacturer’s recommendations according to the patient’s body weight. All the devices were lubricated and the cuff of the LMA-S was completely deflated. The SADs were inserted with the patient’s head in the semi-sniffing position using a single-handed technique. The cuff of the LMA-S was inflated to a pressure of 60 cm H2O using a manometer (Ambu, Ballerup, Denmark). After insertion, the device was connected to a closed-circuit breathing system under volume-controlled ventilation with a tidal volume (TV) of 8 ml kg−1, a respiration rate (RR) of 12 breaths min−1, an inspiration to expiration (I:E) ratio of 1:2 and fresh gas flow of 3 l min−1. Successful placement was defined as a square wave tracing on the capnography with normal end tidal CO2 (EtCO2) values. After three failed attempts, insertion was considered a failure and endotracheal intubation (ETI) was performed. The time required for successful insertion was defined as the time from removing the face mask to the first square capnogram. In cases of ineffective ventilation, e.g. hypoventilation (TV < 6 ml kg−1) or hypercarbia (> 45 mmHg), despite a successful placement, the device was removed and reinserted performing corrective manoeuvres. If ventilation continued to be ineffective after repositioning the SAD, it was considered a ventilation failure and ETI was performed.
A suction gastric tube was introduced via the drain tube (12 FG for the i-gel and 16 FG for LMA-S) and ease of insertion was scored (e.g. easy to insert, minor difficulty with insertion and difficult to insert). A non-blinded observer who was not involved in the study recorded the number of attempts and time needed for SAD insertion as well as ease of drain tube insertion. Anesthesia was maintained with 2 % sevoflurane in 50 % oxygen and air, remifentanil 0.15–0.5 μg kg−1 min−1 and rocuronium 0.6 mg kg−1. After obtaining an effective and stable airway, leak pressure (LP) was assessed by closing the circuit and allowing a fresh gas flow of 3 l min−1 to build airway pressure until an audible leak was heard over the mouth (not permitted to exceed 40 cm H2O) [10]. Ventilatory variables were recorded before and after the pneumoperitoneum, intra-abdominal pressure was held constant at 13 mmHg and head-up tilt was limited to 30º. Peritoneal insufflation time and anesthesia time were also recorded. Ventilatory parameters were continuously monitored (Picis Care Suit Anesthesia Manager, Picis, Wakefield MA) and adapted to give a pulse oximetry (SpO2) > 95 % and end tidal carbon dioxide (EtCO2) of 35–45 mmHg. Maximum expiratory tidal volume (TVme) was recorded over 1 min after pneumoperitoneum was established based on the expiratory tidal volume shown by the ventilator. This measurement corresponds to the maximum expiratory TV value observed over that time under pneumoperitoneum conditions. During emergence and removal, airway complications (e.g. laryngeal stridor, laryngospasm, bronchospasm, regurgitation, aspiration, cough and hypoxia) and the presence of blood were recorded. Additionally, all patients were interviewed at 10 min and 2 h postoperatively by an assessor blinded to the allocation group about the presence of sore throat, dysphagia and hoarseness, which were assessed using a visual analog scale (VAS, 0 = no sore throat, dysphagia or dysphonia, 10 = severe sore throat, total dysphagia or dysphonia). Patients received a standard postoperative analgesia regimen of dexketoprofen (50 mg) and paracetamol (1 g) i.v. and analgesic requirements were comparable between both groups.
Statistical analysis
Published data on leak pressure were used to calculate the necessary sample size. Assuming a mean oropharyngeal leak pressure (OLP) of 26 cm H2O for the i-gel [11] and 28 cm H2O for the LMA-S [12] and assuming a standard deviation of 5 cm H2O for all devices, 66 patients per group were needed to detect a clinically significant difference of 10 % between the groups with 90 % power (1–β = 0.90) and a significance level of 0.05 (two-tailed). A total of 145 patients were needed to consent to account for a 9 % dropout rate. The data were analyzed with SPSS version 17 (SPSS, Chicago, Ill). The distribution of data was determined using Kolmogorov-Smirnov analysis. Statistical analysis was performed with paired t-test, one-way ANOVA for repeated measurements and the χ2-test for nominal data. For postoperative sore throat, test of within-subjects effects were performed using the Greenhouse-Geisser adjustment. Data are given as means ± standard deviation (SD) unless otherwise stated. A p-value less than 0.05 was considered significant.
Results
The study recruited 145 patients and data were excluded from 4 randomized patients, 2 of them after the surgical approach changed from laparoscopy to open surgery, another patient for a protocol violation (wrong sized device) and in another patient (LMA-S) the gastric tube could not be inserted and the patient had to be intubated for safety reasons. The results of 140 patients (71 LMA-S and 69 i-gel) were finally analyzed (Fig. 1). The groups were comparable for demographic and surgical data (Table 1).
There were no significant differences in mean LP (i-gel 28.18 ± 3.90 cmH2O and LMA-S 27.50 ± 4 cmH2O, p = 0.09), or mean TVme (i-gel 559.60 ± 45.25 ml and LMA-S 548.95 ± 56.18 ml, p = 0.12). Both SADs showed a similar mean MLP (i-gel 2.90 ± 2 cmH2O and LMA-S 2.60 ± 2.30 cmH2O, p = 0.08) (Table 2).
The i-gel showed a shorter mean time to insertion compared with the LMA-S (10 ± 1.62 s versus 11.31 ± 2.85 s) and it could be inserted on average 1.3 s quicker than LMA-S (p = 0.008) (Table 2). The success rate on first attempt insertion was higher for the LMA-S group (95 % compared with i-gel (79 %, p = 0.007). Using the standardized residuals (SR), the insertion success rate of LMA-S was found to be above the expected results on the first attempt (80 %, SR = 3.3) and on the second attempt, reporting a success rate of 5 %, while the expected result was 20 % (SR = − 3.7). The i-gel group showed a success rate on the first and on the second attempts close to expected results (SR between − 2 and 2). No failed insertions were recorded in either group (Table 2). Statistically significant differences were found in ease of insertion of the drain tube. It proved to be easier to insert the LMA-S compared with the i-gel (p < 0.001). In the LMA-S group, the drain tube was easy to insert in 75 % of cases with an expected result of 51 % (SR = 4.5). Insertion of gastric tube was successful in all analyzed cases (Table 2). No differences were found between the groups relating to intraoperative complications. No episodes of laryngeal stridor, laryngospasm, bronchospasm, hypoxia, regurgitation or aspiration were seen. Frequency of coughing and visible blood on removal of the device were comparable in both groups (p = 0.860 and p = 0.623, respectively).
There were no differences relating to the incidence of sore throat, dysphagia or hoarseness at 10 min postoperatively between groups (p = 0.088). Mean VAS values were graded according to three categories: VAS = 0/VAS = 1–3/VAS ≥ 4. Based on this ranking, the percentages obtained by the SADs were: i-gel 57 %/41 %/2 % and LMA-S 45 %/55 %/0 %, respectively (Table 2).
There was a higher incidence of sore throat at 2 h in i-gel group compared with LMA-S group (p = 0.009). Patients from the i-gel group suffered more sore throats (0.24 more points on the VAS scale) than the LMA-S group. In addition, the VAS values by categories (VAS = 0/VAS = 1–3/VAS ≥ 4) were i-gel = 53 %/47 %/0 % and LMA-S = 82 %/18 %/0 %, 3 patients complained of dysphagia (2 LMA-S and 1 i-gel) and 1 patient complained of dysphonia (i-gel) at that time.
Based on these postoperative pharyngolaryngeal discomfort incidences an attempt was made to identify the development of sore throat during the period of time (2 h) studied. A within-subjects effects test (Greenhouse-Geisser adjustment) was applied and significant differences were found with respect to the trend towards sore throat during this time (p < 0.001). Consequently, the i-gel group showed a slight downward trend regarding POPD, compared with the notable downward tendency experienced by the LMA-S group (Fig. 2).
Discussion
A significant proportion of the current literature studying the use of SADs with gastric access focused on comparisons between LMA-S with LMA-P [4, 7] and i-gel with LMA-S [5] or LMA-P [8, 9]. This is the first known study comparing the use of i-gel and LMA-S in patients undergoing laparoscopic cholecystectomy. Leak pressure did not differ among the devices and the LP values measured by both devices are similar to those reported previously [5, 13, 14]. The study conducted by Teoh et al. [5] confirmed the similarity between i-gel and LMA-S (in reference to LP) as observed in non-laparoscopic surgery [11, 15]. Ventilatory ability during the laparoscopic procedure was similar between i-gel and LMA-S, regarding TVme achieved by the devices. This fact was shown by other authors, finding these two SADs comparable regarding inspired and expired tidal volumes, reinforcing their similarity in terms of ventilation [5].
The secondary outcome was to measure MLP, a concept related to the feasibility of SADs during procedures involving high peak airway pressure (PAW-pk). Based on these findings, during a laparoscopic cholecystectomy using these two devices, the highest PWA-pk is usually a mean of 2.75 cm H2O below seal pressure. This statement is valid for this cohort and with the conditions of the study. More studies are necessary in order to extrapolate them to the general practice and generate a general conclusion.
In the present study the i-gel was found to be 1.3 s quicker to insert than the LMA-S. All the studies that measured this variable did not find any differences between i-gel and LMA-S except the study from Theiler et al. [16], in which LMA-S needed shorter insertion times than i-gel in a crossover comparison in a simulated difficult airway scenario. However, this small difference is clinically irrelevant and due to this fact no differences were found by other authors. The results of this study may be explained by the smaller bowl of the i-gel and the relative firmness of its slightly curved airway tube when compared to the cuffed mask; however, LMA-S may be a more suitable and quicker device for using in difficult airway management, probably due to its anatomically shaped and semi-rigid PVC airway tube. The success rate on the first attempt was significantly higher in the LMA-S group. Most published data did not report differences regarding first-time success rates [5, 11, 16]. Nevertheless, as in this study, Ragazzi et al. [17] found higher insertion success rates in a study performed by novices. The special shape and rigidity of LMA-S makes it an ideal device for easy insertion, principally for inexperienced operators. The gastric tube was easier to insert in the LMA-S group compared with the i-gel. This result is similar to those of Teoh et al. [5] and Fernandez et al. [15] and possibly explained by the more rigid, centered and smoother gastric drain channel of the LMA-S. In addition, the i-gel has a narrower drain access which only allows the introduction of a smaller sized gastric tube. With respect to adverse events at 10 min postoperatively, patients reported similar POPD scores between the two groups and the findings are similar to the results obtained by other authors [5, 11, 16]. The incidence of POPD at 2 h after anesthesia showed significant differences between devices, so that the i-gel group experienced higher numbers of sore throats at that moment. Previous studies did not find differences concerning postoperative sore throat or other complaints among devices during the postoperative period [5, 11, 15]. The study results show a very significant statistical difference (p < 0.001) related to sore throat development during the first 2 h in the PACU. The i-gel resulted in a lower sore throat incidence immediately after the anesthesia procedure but it caused more POPD than LMA-S after 2 h in the recovery room. Therefore, the i-gel group showed a slightly downward trend regarding sore throat compared with the notable downward tendency experienced by the LMA-S group (Fig. 2). These facts are difficult to explain and despite the findings suggesting that i-gels may be a more injurious device than LMA-S regarding airway morbidity, there are not enough data to draw a conclusion. It has to be taken into consideration that a mean difference of 0.24 points in VAS is clinically insignificant with respect to the incidence of postoperative sore throat, as well as the difference related to sore throat development which has no clinical relevance. Consequently, more studies are needed in order to explain the small differences found.
The study has a number of limitations. Firstly, the observer who measured the insertion times and events was not blinded to the type of device. Postoperative outcome assessors were blinded to the group assignment in order to mitigate that limitation. Secondly, the anesthesiologist who inserted the devices had less experience with the i-gel than using the LMA-S. Thirdly, the findings related to MLP value may only be valid for this study and a general conclusion cannot be drawn.
It can be concluded that in this randomized study, i-gel and LMA-S are comparable regarding leak pressure in anesthetised patients undergoing laparoscopic cholecystectomy. The i-gel was more rapidly placed than LMA-S but there was a better first time success rate and ease of drain tube insertion for the LMA-S. The study showed that i-gels reached higher sore throat scores 2 h postoperatively and a lower POPD drop was reported during this 2 h period.
References
O’Connor CJ Jr, Stix MS, Valade DR (2005) Glottic insertion of the ProSeal LMA occurs in 6 % of cases: a review of 627 patients. Can J Anaesth 52(2):199–204
Maltby JR, Beriault MT, Watson NC et al (2003) LMA-Classic™ and LMA-ProSeal™ are effective alternatives to endotracheal intubation for gynecologic laparoscopy. Can J Anaesth 50:71–77
Natalini G, Lanza G, Rosano A et al (2003) Standard Laryngeal Mask Airway™ and LMA-ProSeal™ during laparoscopic surgery. J Clin Anesth 15:428–432
Lee AK, Tey JB, Lim Y, Sia AT (2009) Comparison of the single-use LMA Supreme with the reusable Proseal LMA for anaesthesia in gynaecological laparoscopic surgery. Anaesth Intensive Care 37:815–819
Teoh WH, Lee KM, Suhitharan T et al (2010) Comparison of the LMA Supreme vs i-gel in paralysed patients undergoing gynaecological laparoscopic surgery with controlled ventilation. Anaesthesia 65:1173–1179
Yao T, Yang XL, Zhang F et al (2010) The feasibility of Supreme laryngeal mask airway in gynaecological laparoscopy surgery. Zhonghua Yi Xue Za Zhi 90:2048–2051
Beleña JM, Nuñez M, Anta D et al (2013) Comparison of LMA Supreme™ and LMA Proseal™ with respect to oropharyngeal leak pressure in patients undergoing anaesthesia during laparoscopic cholecystectomy: a randomized controlled trial. Eur J Anaesthesiol 30:119–123
Sharma B, Sehgal R, Sahai C, Sood J (2010) PLMA vs. I-gel: a comparative evaluation of respiratory mechanics in laparoscopic cholecystectomy. J Anaesthesiol Clin Pharmacol 26:451–457
Woo JJ, Sang YC, Seong JB, Kyoung HK (2012) Comparison of the Proseal LMA and Intersurgical I-gel during gynaecological laparoscopy. Korean J Anesthesiol 63:510–514
Keller C, Brimacombe JR, Keller K, Morris R (1999) Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients. Br J Anaesth 82:286–287
Russo SG, Cremer S, Galli T et al (2012) Randomized comparison of the i-gel™, the LMA Supreme™ and the Laryngeal Tube Suction-D using clinical and fibreoptic assessment in elective patients. BMC Anesthesiol 12:18
Beleña JM, Gracia JL, Ayala JL et al (2011) The Laryngeal Mask Airway Supreme for positive pressure ventilation during laparoscopic cholecystectomy. J Clin Anesth 23:456–460
Gatward JJ, Cook TM, Seller C et al (2008) Evaluation of the size 4 i-gel airway in one hundred non-paralysed patients. Anaesthesia 63(10):1124–1130
Timmermann A, Cremer S, Eich C et al (2009) Prospective clinical and fiberoptic evaluation of the Supreme Laryngeal Mask Airway™. Anesthesiology 110:262–265
Fernández A, Pérez A, Bermejo JC, Marcos JM (2009) Supreme Laryngeal Mask Airway vs the I-gel Supraglottic Airway in patients under general anesthesia and mechanical ventilation with no neuromuscular block: a randomized clinical trial. Rev Esp Anestesiol Reanim 56:474–478
Theiler LG, Kleine-Brueggeney M, KaiserD et al (2009) Crossover comparison of the laryngeal mask supreme and the i-gel in simulated difficult airway scenario in anesthetized patients. Anesthesiology 111:55–62
Ragazzi R, Finessi L, Farinelli I et al (2012) LMA Supreme™ vs i-gel™: a comparison of insertion success in novices. Anaesthesia 67:384–388
Acknowledgements
The authors would like to thank Sebastian Fairhurst for help and support in translating the English abstract text into German.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J.M. Beleña, M. Núñez, A. Vidal, C. Gasco, A. Alcojor, P. Lee and J.L. Pérez state that there are no conflicts of interest. All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Disclosure of funding
No funds were received for the study from any of the following organizations: National Institutes of Health (NIH), Spanish Society of Anaesthesiology (SSAR), Regional Government of Madrid (RGM), neither from other organization, including departmental or institutional funding.
Clinical trial registry
This trial was not registered in any public registry due to the starting date for patient enrolment (September 2009).
Additional information
Author contributions:
J.M. Beleña: study conception and design, acquisition of data, analysis and interpretation of data, drafting of manuscript and critical revision.
M. Nuñez: study conception and design, acquisition of data, drafting of manuscript and critical revision.
A. Vidal: study conception and design, analysis and interpretation of data, drafting of manuscript and critical revision.
C. Gasco: study conception and design, drafting of manuscript and critical revision.
A. Alcojor: acquisition of data, drafting of manuscript and critical revision.
P. Lee: analysis and interpretation of data, drafting of manuscript and critical revision.
Rights and permissions
About this article
Cite this article
Beleña, J., Núñez, M., Vidal, A. et al. Randomized comparison of the i-gelTM with the LMA SupremeTM in anesthetized adult patients. Anaesthesist 64, 271–276 (2015). https://doi.org/10.1007/s00101-015-0020-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-015-0020-z