Abstract
Purpose
It was aimed to compare the results of long segment posterior instrumentation with intermediate pedicular screw + fusion at the level of the fractured segment including one vertebra above and one below the fractured vertebra (LSPI) and short segment posterior instrumentation with intermediate pedicular screw + fusion at the level of the fractured segment including one vertebra above and one below the fractured vertebra (SSPI) in the surgical treatment of thoracolumbar vertebral fractures.
Methods
Ninety patients with thoracolumbar vertebral (T11-L2) fractures operated between March 2015 and February 2022 were included in this retrospective study. The patients were divided into two groups as those who underwent LSPI (n, 54; age, 40.3) and those who underwent SSPI (n, 36; age, 39.7). Radiological evaluations like vertebral compression angle (VCA), vertebral corpus heights (VCH), intraoperative parameters, and complications were compared between the groups.
Results
Correction in early postoperative VCA was statistically significantly better in LSPI (p = 0.003). At 1-year follow-up, postoperative VCA correction was significantly more successful in LSPI (p = 0.001). There was no difference between the two groups in terms of correction loss in VCA measured at 1-year follow-up. There was no statistically significant difference between the two groups in terms of postoperative VCH, VCH at 1-year follow-up, and correction loss in VCH.
Conclusion
LSPI provides better postoperative kyphosis correction of the fractured vertebra than SSPI. Regarding the segment level of posterior instrumentation, there was no difference between the two groups in terms of the loss of achieved correction of VCA, ABH, and PBH at 1-year follow-up. Operating a thoracolumbar fracture with LSPI will lengthen the operation and increase the number of intraoperative fluoroscopies compared to SSPI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The most frequent spine injuries are thoracolumbar fractures (T11-L2) [1]. This area is a significant biomechanical stress area because it marks the change from the rigid thoracic spine with the rib cage to the more dynamic lumbar spine. Neurological deficits occur in approximately 20% of patients after thoracolumbar vertebral fractures. As a result, it is a prevalent source of morbidity in the community [2].
Anterior, posterior, or combined approaches are used in the surgical treatment of thoracolumbar fractures. The difference in approach depends on the experience of the surgeon. Posterior fusion stands out with its short learning curve, short operation times, and less blood loss [3, 4]. In the surgery of thoracolumbar fractures with posterior fusion, long segment fusion provides more stable fixation, but leads to more mobile segment loss. Short segment fusion causes less mobile segment loss, but in long-term follow-up, it may cause implant failure and progressive kyphosis. It is still a matter of debate whether to use long segment or short segment in unstable fractures. Different studies report different results [5,6,7]. Short segment fusion is recommended in studies conducted in the last 5 years. However, the benefits of long segment fusion cannot be ignored.
When performing long segment and short segment fusion, it is debatable whether a screw should be placed on a fractured spine. Pedicular screw placement on the fractured vertebra improves stability and lowers load on the non-fractured vertebra, according to biomechanical studies [8]. Biomechanical studies point to intermediate screw fixation in the short section, with few studies on long segment fixation [7].
The aim of this study is to compare the results of long segment posterior instrumentation (consisting of pedicular screws, 2 levels above and below the fractured vertebra, with interconnected rods) with intermediate pedicular screw + fusion at the level of the fractured segment including one vertebra above and one below the fractured vertebra by posterolateral/posterior allograft (LSPI) and short segment posterior instrumentation (consisting of pedicular screws, 1 level above and below the fractured vertebra, with interconnected rods) with intermediate pedicular screw + fusion at the level of the fractured segment including one vertebra above and one below the fractured vertebra by posterolateral/posterior allograft (SSPI) in the surgical treatment of thoracolumbar vertebral fractures.
Materials and methods
Study design and patient characteristics
It was formed on patients who were operated with posterior instrumentation due to thoracolumbar vertebral fracture in the Orthopedics and Traumatology Department since the approval date of the Medical Research Ethics Committee. Our study is a retrospective study. Before beginning study methods, the participant’s informed consent was obtained.
Ninety patients with thoracolumbar vertebral (T11-L2) fractures operated between March 2015 and February 2022 were included in the study. The patients were divided into two groups as those who underwent long segment posterior instrumentation (consisting of pedicular screws, 2 levels above and below the fractured vertebra, with interconnected rods) with intermediate pedicular screw + fusion at the level of the fractured segment including one vertebra above and one below the fractured vertebra by posterolateral/posterior allograft (LSPI) (n, 54; age, 40.3) and those who underwent short segment posterior instrumentation (consisting of pedicular screws, 1 level above and below the fractured vertebra, with interconnected rods) with intermediate pedicular screw + fusion at the level of the fractured segment including one vertebra above and one below the fractured vertebra by posterolateral/posterior allograft (SSPI) (n, 36; age, 39.7) (Figs. 1 and 2). We noted the patients’ age, sex, level of injury, AO classification, mechanism of injury, and American Spinal Cord Injury Association (ASIA) impairment scale (Table 1). The data obtained were compared among the groups.
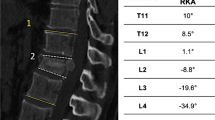
MRI and CT scan of a 51-year-old male patient admitted to the emergency department with vertebral fracture (a, f). Vertebral compression angle (VCA) measurement preoperative (b), early postoperative (c), 1-year follow-up (d), and after removal of the implants (e) in LSPI. Anterior body height (ABH) and posterior body height (PBH) measurements preoperative (g), early postoperative (h), 1-year follow-up (i), and after removal of the implants (j) in LSPI
MRI and CT scan of a 34-year-old male patient admitted to the emergency department with vertebral fracture (a, f). Vertebral compression angle (VCA) measurement preoperative (b), early postoperative (c), and 1-year follow-up (d) in SSPI. Anterior body height (ABH) and posterior body height (PBH) measurements preoperative (g), early postoperative (h), and 1-year follow-up (i) in SSPI. Despite the fact that this patient did not have a significant mechanically unstable spinal fracture, short segment fixation had less favorable results in terms of kyphotic corrective preservation over time (e, j)
Since estimating the screw length in a fractured pedicle with a tiny spherical tip probe used to confirm the length of the entrance hole would be challenging, placing the proper pedicular screw in a fractured vertebra could be difficult. Moreover, it can cause medial or lateral pedicle penetration during the insertion of the pedicular screw. In our study, the pedicles of the fractured vertebrae of all patients included in the study were intact.
Assessment of the parameters among groups
During the surgery, the intraoperative parameters (instrumentation duration and intraoperative fluoroscopy number) were noted. Three orthopedic surgeons who took part in the research used the software Sectra to acquire and evaluate preoperative computed tomography (CT) and postoperative plain radiograph images (Sectra AB, Linkoping, Sweden). All the radiological images were assessed in a blinded fashion. Radiological images of the thoracolumbar spine were compared retrospectively preoperative, 1 day after operation, and 1-year follow-up. The fractures were classified according to the AO classification. Additionally, the following measurements were performed using preoperative CT and standing plain radiographs [9].
-
1—Vertebral compression angle (VCA; defined as the angle between the lower and upper border of the fractured vertebra) (Fig. 1b–e, Fig. 2b–e)
-
2—Anterior body height (ABH; measured from the anterosuperior corner of the vertebra to the anteroinferior corner) (Fig. 1g–j, Fig. 2g–j)
-
3—Posterior body height (PBH; measured from the posterosuperior to posteroinferior corner) (Fig. 1g–j, Fig. 2g–j)
-
4—Anterior vertebral body compression percentage (ABH/PBH ratio)
Surgery
The surgeons decided to operate on patients with thoracolumbar vertebral fractures, if the posterior osteoligamentous complex is impaired, if the vertebral corpus kyphosis is greater than 25°–30°, if the vertebral corpus height loss is more than 50%, or if there is more than 50% canal compression in the radiological evaluations. All surgeries were done when the patients’ general condition permitted, all radiological examinations were completed, and consultations were completed in the emergency department (< 48 h). All patients underwent posterior instrumentation with intermediate pedicular screw + fusion at the level of the fractured segment including one vertebra above and one below the fractured vertebra by posterolateral/posterior allograft under general anesthesia, with the posterior midline approach and the fractured vertebra centered using the Roy-Camille method [10, 11]. All surgeries were performed by two experienced surgeons (O.A., A.M.O.) using similar approach and implants except the level of the instrumentation. LSPI was preferred by surgeon 1; on the other hand, SSPI was preferred by surgeon 2 during surgery. According to surgeon 1, reason for choosing LSPI was: long segment fixation has superiority in construct stability, which is important in fusion surgeries. Besides, using a longer precontoured rod during surgery may help more in achieving correction of the kyphosis during surgery because the pedicular screws in the fractured vertebra biomechanically behave as a push point with an anterior vector, providing a more powerful lordosing force that corrects the kyphosis than short segment fixation [12, 13] (Figs. 1, 3, and 4). In addition, short segment fixation has been shown to produce less favorable results in terms of kyphotic correction, correction maintenance, and implant failure when compared to long segment fixation in cases with poor anterior column support and lower mechanical stiffness, even when intermediate screws are used (Fig. 2) [14, 15]. Surgeon 2’s reason for his decision although long segment posterior fixation provides more stability and support with fewer risks of implant failure is that it comes with the loss of motion segments. Long segment fixations have also been linked to greater movement in adjacent disc spaces, resulting in increased intradiscal pressure. These biomechanical impacts are known to accelerate the process of adjacent disc degeneration [16]. To overcome these limitations of long segment fixation, he decided to operate with a short segment fixation technique incorporating the pedicle of fractured vertebrae. He believed that with intermediate screw in short segment fixation, the construct gains sufficient rigidity in fusion surgery.
Precontoured rods. When we use intermediate screw, using a longer precontoured rod may act more effectively as a push point to increase forward force on fractured vertebrae by providing a more powerful lordosing effect with a longer anterior vector arm at the time of indirect reduction of the fracture during surgery
The implants were removed after 1 year in patients in the LSPI group, while implant removal surgery was not performed in patients in the SSPI group.
Statistical analysis
The frequencies and percentages were given for categorical variables, and the mean and standard deviation (SD) were given for numerical variables as descriptive statistics. Categorical variables were compared between groups with Pearson’s chi-squared test. The Shapiro–Wilk test was used to test normality assumption in numerical variables. Group comparisons for numerical variables were performed with independent sample t-test. The change in radiological outcomes was analyzed by repeated measures analysis of variance (ANOVA) in each group. The ıntraclass correlation coefficient (ICC: two-way mixed effects, absolute agreement, three raters) was used to analyze interrater reliability at each measurement time point.
Statistical significance was assessed at p < 0.05, and all statistical analyses were performed using IBM SPSS Statistics 23.0 (IBM SPSS Statistics for Windows, version 23.0. Armonk, NY: IBM Corp.).
Results
There was no statistical difference with respect to age, sex, mechanism of injury, level of injury, AO classification of the fracture, and ASIA impairment scale between the groups (Table 1).
The radiological examinations were made by three different experienced orthopedic surgeons at three assessments. The ICC values were 0.989, 0.984, and 0.991 for VCA; 0.994, 0.993, and 0.992 for ABH; and 0.996, 0.989, and 0.995 for PBH according to the time schedule of measurements.
The results of the radiological evaluations are shown in Table 2. Both groups significantly restored VCA and VBH (vertebral body height) after operation (p < 0.001). There was no significant difference in preoperative VCA (p = 0.849). Correction in early postoperative VCA was significantly better in LSPI (p = 0.003). At the 1-year follow-up, postoperative VCA correction was significantly more successful in LSPI (p = 0.001). There was no difference between the two groups in terms of correction loss in VCA measured at the 1-year follow-up. There were no significant differences in preoperative ABH, postoperative ABH, 1-year follow-up ABH, correction loss ABH, preoperative PBH, postoperative PBH, 1-year follow-up PBH, correction loss PBH, preoperative ABH/PBH ratio, postoperative ABH/PBH ratio, and 1-year follow-up ABH/PBH ratio among the groups (p = 0.121, p = 0.129, p = 0.136, p = 0.234, p = 0.129, p = 0.125, p = 0.109, p = 0.444, p = 0.418, p = 0.282, and p = 0.153, respectively).
There was a significant difference in operation time and intraoperative fluoroscopy numbers in LSPI (155.08 ± 13.42 min, 25.18 ± 2.20 times) compared to SSPI (104.86 ± 14.81 min, 15.46 ± 2.13 times) (p < 0.001, p < 0.001 respectively) (Table 2).
Following surgery, all patients had effective solid posterior spinal fusion. Early superficial tissue infection was observed in one patient (1.85%) in LSPI and treated effectively with oral antibiotic. Implant failure occurred in two patients (3.70%) in LSPI and one patient (2.78%) in SSPI.
Discussion
The most striking result of our study is that although LSPI provides better postoperative correction of the fractured vertebra than SSPI, there is no difference between the two groups in terms of loss of gained correction in the 1-year follow-up.
It is controversial whether pedicle screws in the fractured vertebra should be used for short segment fixation or long segment fixation in the treatment of thoracolumbar vertebral fractures performed with a posterior approach [17, 18]. Numerous studies on this topic can be found in the literature. Pedicle screw placement in the fractured vertebra in short segment posterior instrumentation is recommended by many authors and is almost out of discussion. Studies have focused on short segment fusion where screws are placed on the fractured vertebra and long segment fusion where no screws are placed on the fractured vertebra. Our study is important because there are few studies comparing short segment posterior instrumentation combined with intermediate screw and long segment posterior instrumentation combined with intermediate screw.
Short segment instrumentation offers the advantage of involving fewer motion segments in fusion but may not provide adequate long-term stabilization. Negative effects of short segment instrumentation have been reported in the literature [19, 20]. It is important that the use of pedicle screws in the fractured vertebra are functional, so the choice of short segment fusion is not appropriate for every patient. On the other hand, although posterior long segment instrumentation provides more stable fixation and less correction loss on follow-up, it reduces the number of mobile vertebrae because it involves multiple segments and results in increased operative time, blood loss, and fluoroscopy number.
Tezeren et al. [21] showed that posterior instrumentation with long segment produced better radiographic results, although no difference was found between the two groups in terms of clinical outcomes when comparing short and long segment instrumentation without intermediate screw. Aly TA et al. [22] compered short segment versus long segment pedicle screw fixation in his meta-analysis and he showed that no significant difference was identified between the two groups regarding radiological outcome, functional outcome, neurologic improvement, and implant failure rate.
The intermediate screw fixation technique, introduced in 1994 under the direction of Dick et al., offered a new perspective for the treatment of thoracolumbar fracture. In a biomechanical study, it was shown that insertion of screws into the fractured vertebra stabilized the fracture and reduced the loss of correction [23,24,25,26]. Clinical studies have shown that fixation of the fractured vertebra with a pedicle screw during posterior short segment instrumentation stabilizes the fracture and that there is no change in kyphosis at follow-up [27,28,29].
Dobran et al. [27] compared instrumentation of the long segment without screws at the fractured vertebra and instrumentation of the short segment with screws at the fractured vertebra and they demonstrated similar correction of kyphosis and preservation of sagittal alignment at follow-up. Guven et al. [29] compared 4 groups with intermediate screws and without intermediate screws posterior short segment and long segment fusion. It was found that long segment fusion with a intermediate screw provided the best results at follow-up. In our study, correction in early postoperative VCA was statistically significantly better in LSPI (p = 0.0025). There was no difference between the two groups in terms of correction loss in VCA measured at 1-year follow-up. There was no statistically significant difference between the two groups in terms of postoperative VCH, VCH at 1-year follow-up, and correction loss in VCH. There is no difference between the two groups in terms of loss of correction during the 1-year follow-up, despite the fact that long segment fusion offers superior postoperative correction of the fractured vertebra than short segment fusion.
Biomechanically, it has been shown that intermediate screws in the fractured vertebra can act as a repulsion point for an anterior vector, resulting in a lordotic force that also corrects kyphosis in the segment [12]. The three-point fixation afforded decreases the cantilever effects that cause kyphosis. The screw head of the pedicle screw in the fractured vertebra serves as the fulcrum for this forward thrust, which causes compression behind the screw head and distraction anteriorly. With this mechanism, when the appropriately precontoured rod is placed on the pedicular screws during indirect reduction, the pedicular screw in the fractured vertebrae acts as a pressure point, increasing the forward force and providing more effective lordosis of the collapsed segment [13]. We found in our study that the correction in early postoperative VCA was significantly better in LSPI (p = 0.003). Furthermore, at 1-year follow-up, postoperative VCA correction was significantly more successful in LSPI (p = 0.001). Since we use a longer precontoured rod in LSPI, it may act more effectively as a push point to increase forward force on fractured vertebrae by providing a more powerful lordosing effect with a longer anterior vector arm at the time of indirect reduction of the fracture during surgery.
The removal of implants after satisfactory fusion of thoracolumbar fractures may be useful in regaining flexibility and eliminating pain, but it also has the potential to result in complications after surgery. Both operators and their patients must be informed of the indications necessitating implant removal and have realistic expectations on the advantages and hazards. There was insufficient evidence to support routine removal of pedicle screw tools following complete fusion of thoracolumbar fractures, which could expose patients to avoidable risks like infection and costs [30]. Although there are discussions, it is not recommended to remove the implant in the literature, especially in cases with short segment posterior instrumentation + fusion since the fusion occurs throughout the construct segments. Because there will be no movement in the fusion segments following solid fusion, the stress on the fixation during movement will be reduced, hence the risk of implant failure. On the other hand, in patients in the LSPI group, the stress on the screw and rod in the non-fused areas continued with movement. Therefore, implants were removed after 1 year in patients in the LSPI group, while implant removal surgery was not performed in patients in the SSPI group. This can be defined as a disadvantage of preferring LSPI as a treatment for thoracolumbar fractures. The implant removal was suggested to the LSPI after 1 year postoperatively due to the possibility of implant failure, which invalidated the hardware removal comparison between the groups. In our study, implant failure occurred in two patients in LSPI and one patient in SSPI. The implant removal was performed after a 1-year follow-up in patients in LSPI. However, for some patients who participated in the study, this period was longer due to the patient’s social status or excuse. Since the fusion was made only at the fractured vertebral level, bending and twisting forces may have continued in pedicle screws and rods located above and below the fusion site. Therefore, we think that a fracture was detected in one of the lowest screws in two patients in LSPI. Screw breakage was connected with a history of direct trauma in the patient in SSPI.
Due to the fact that more segments are implanted in patients operated on with LSPI, in accordance with the literature, the operation time and the number of fluoroscopy were found to be higher in LSPI compared to SSPI in our study [5,6,7, 21, 22, 27]. This can be shown as another disadvantage of preferring LSPI as a treatment for thoracolumbar fractures.
Osteoporosis in older patients may have a negative effect on the insertion torque of the pedicle screws inserted at the time of posterior instrumentation, and the screws may not hold tightly in the pedicle. Compared to patients with normal bone morphology, the incidence of pedicle screw loosening and loss of vertebral sagittal correction is increased in patients with advanced age-related osteoporosis undergoing spine surgery [31]. For all of these reasons, while short segment fixation with intermediate screws can increase system rigidity, long segment posterior instrumentation may be preferable in older age and osteoporotic patients with vertebral fractures. However, in younger patients, especially in lumbar fractures, short segment posterior instrumentation may be preferred to leave more mobile segments free. In our study, long segment fixation was also applied in young patients. Pedicular screw placement in the fractured vertebra is generally not preferred by surgeons when long segment posterior instrumentation performed. In our study, the surgeon who preferred fracture surgery with long segment posterior instrumentation also placed pedicular screws in the fractured vertebra during the operation. Many studies have found that fracture level screw fixation with pedicular screw is more effective than bridging in terms of correcting the local kyphosis angle and anterior body height [12, 18, 29, 32]. Guven et al. [29] explained this through the lordosing effect. When we extend the level arm of the construct through long segment posterior fixation, then we have the potential to improve stability while also effectively reducing kyphotic deformity through a more powerful lordosing effect [33]. This allows more effective intraoperative fracture reduction and correction of sagittal deformity. Therefore, in our study, some patients with vertebral fractures in LSPI underwent long segment posterior instrumentation with screw placement in the fractured vertebra despite their young age.
Severe vertebral body fractures, such as comminuted and burst fractures, may require corpectomy and reconstruction with a vertebral body cage. Especially in the cases of severe fractures, the bone fragment may penetrate into the spinal canal and can compress the neurological structures and lead to spinal canal stenosis. Corpectomy allows resection of the fractured vertebral corpus, including bone fragments that compress the nerves and enter the spinal canal. There is no clear consensus in the literature about the necessity of anterior column reconstruction after thoracolumbar burst fractures. To determine the ideal surgical approach in patients with thoracolumbar vertebra fractures, factors such as fracture type, stability, degree of canal compression, and neurological status should be examined [34]. The benefits of anterior column reconstruction include the ability to fuse a shorter segment, allowing decompression of the anterior canal by direct removal of fracture fragments entering the spinal canal via corpectomy, and better sagittal realignment [35, 36]. In the literature, only Wang et al. [37] conducted a prospective randomized controlled study on thoracolumbar vertebral fractures and suggested that anterior and combined approaches may be more effective therapeutic approaches than posterior approaches due to better spinal canal assessment and ease of spinal decompression. However, a recent meta-analysis by Gonzales et al. [38] recommends posterior instrumentation over anterior approaches for the surgical treatment of vertebral fractures due to its significant advantages in terms of operative time, blood loss, length of stay, postoperative kyphotic angle, return to work, and complication rates. To insert pedicular screws on fractured vertebra during surgery provide directly raise the end plate to assist in the restoration of the compressed vertebral height. Besides there may be a vertebral body filling effect and anterior support on fractured segment. Because vertebral compression results in trabecular bone destruction, a cavity is produced within the vertebral body after reduction, which may induce vertebral re-collapse postoperatively. A pedicle screw inserted into the fractured vertebra can fill this cavity, which can result in better reduction of the fractured vertebra. Because of all these it can be a viable alternative to anterior augmentation surgical procedures that include transpedicular grafting as well as cementing of the injured vertebra or anterior fusion [39].
In posterior instrumentation, the question “is fusion really necessary in all cases with thorocolumbar fractures operated by posterior instrumentation?” is controversial in the literature. In the studies supporting non-fusion, less blood loss, shorter operation time, better preservation of segmental motion, and prevention of donor site complications were shown as positive benefits [40,41,42]. On the other hand, there are studies indicating that the risk of implant failure decreases with the achievement of posterior intact fusion and that the kyphosis correction in the fractured segment is better preserved in the long term [43,44,45]. Hence, although the necessity of additional fusion in posterior internal fixation is still debated, Lan T et al. [46] in their meta-analysis compared fusion and non-fusion of 445 thoracolumbar burst fracture patients and concluded that the safety and efficacy between non-fusion and fusion are similar, and satisfactory clinical and radiological results can be achieved, and non-fusion is superior to fusion with less blood loss, shorter operative time, and lower donor site complications. Although the literature does not clearly recommend fusion in the posterior instrumentation of thoracolumbar fractures, the surgeons in our study, as stated in some studies in the literature, fused the fractured segment during surgery because they believed it was more effective in maintaining the achieved correction.
As is well known in spine surgery, minimally invasive surgery using percutaneous instrumentation provides the advantage of less tissue dissection and minimizes approach-related complications. However, there is limited data on its effectiveness compared to conventional open posterior instrumentation in thoracolumbar and lumbar fractures [47]. The open posterior instrumentation technique may cause damage to the paraspinal muscle and surrounding soft tissues due to traction at the time of surgery and may cause iatrogenic permanent muscle atrophy and postoperative pain [48]. Hong et al. [49] concluded the minimally invasive spinal surgery group had less blood loss during surgery, shorter operation time, and less postoperative pain in their study comparing the clinical and radiological results of minimally invasive spine surgery and open posterior instrumentation surgery in the treatment of unstable burst fractures. In surgeries for thoracolumbar and lumbar fractures, minimally invasive surgery has been reported to achieve comparable fracture reduction and maintenance of reduction compared to open posterior surgery [47, 49]. Although the benefits of minimally invasive surgery in thoracolumbar and lumbar fractures are reported in the literature, all patients included in our study underwent surgery with the open posterior instrumentation method.
Implant removal surgery is generally recommended in cases such as rod fracture or screw fracture, whereas there is no consensus in the literature regarding planned implant removal after vertebral fractures. While some authors state that after implant removal causes loss of obtained kyphosis correction and advocate not removing the implants, other authors recommend implant removal after 12 months in order to regain the mobile segment, to prevent implant fractures that may occur in the long term, and to prevent adjacent segment problems that may occur especially in long segment fixations [50,51,52,53,54,55]. Infection, migration, or compromised neurological structures are objective reasons for implant removal, as are difficulties with the flexibility of the spine caused by long segment posterior fixations [56]. Kweh et al. [57] reported in their meta-analysis that removal of the implant did not lead to loss of kyphosis correction, but this procedure improved functional outcomes in patients. In our study, we applied fusion only to the fractured segment. In long segment fixation, fusion was not applied to the upper and lower segments. In short segment posterior instrumentation, no planned implant removal was performed because the fusion covered the entire implant area, whereas in long segment fixation, planned implant removal was performed 12 months after surgery to restore motion in the upper and lower fusion-free segments.
Some limitations could be noted in this study. It was a retrospective study. A larger patient population is needed for further assessment. Postoperative results of fractures in the thoracolumbar region, rather than a single fracture type, were compared. Instead of comparing the outcomes of operations performed by a single surgeon, we made a comparison between groups by including patients with thoracolumbar fractures who were operated on by two experienced surgeons working in two different university hospitals in the same province. In order to eliminate the bias arising from the operation performed by two different surgeons, it would be more appropriate to form two groups with a simple randomization method according to the order of admission of the patients to the emergency department, to perform the operations by a single surgeon, and to compare the results of the two groups in a prospective study to be planned in the future. The idea of the adjacent segment degeneration was not evaluated in this study. During radiological evaluations, it was difficult to identify the endplate in cases with heavily comminuted and collapsed fractures. The implant removal was suggested to the LSPI after 1 year postoperatively due to the possibility of implant failure, which invalidated the hardware removal comparison between the groups.
Conclusion
LSPI provides better postoperative kyphosis correction of the fractured vertebra than SSPI. Regardless of the segment level of posterior instrumentation, there was no difference between the groups in terms of loss of the achieved correction of VCA, ABH, and PBH in the 1-year follow-up. Operating a thoracolumbar fracture with LSPI will lengthen the operation and increase the number of intraoperative fluoroscopies compared to SSPI. The need for implant removal in the LSPI group can be defined as a disadvantage of preferring LSPI as a treatment for thoracolumbar fractures.
Data availability
No datasets were generated or analysed during the current study.
References
Gertzbein SD, Scoliosis Research Society. Multicenter spine fracture study. Spine (Phila Pa 1976). 1992;17(5):528–40. https://doi.org/10.1097/00007632-199205000-00010.
Thurman DJ, Burnett CL, Jeppson L, Beaudoin DE, Sniezek JE. Surveillance of spinal cord injuries in Utah, USA. Paraplegia. 1994;32(10):665–9. https://doi.org/10.1038/sc.1994.107.
Hughes H, Carthy AM, Sheridan GA, Donnell JM, Doyle F, Butler J. Thoracolumbar burst fractures: a systematic review and meta-analysis comparing posterior-only instrumentation versus combined anterior-posterior instrumentation. Spine (Phila Pa 1976). 2021;46(15):E840–9. https://doi.org/10.1097/BRS.0000000000003934.
Alvine GF, Swain JM, Asher MA, Burton DC. Treatment of thoracolumbar burst fractures with variable screw placement or Isola instrumentation and arthrodesis: case series and literature review. J Spinal Disord Tech. 2004;17(4):251–64. https://doi.org/10.1097/01.bsd.0000095827.98982.88.
Mittal S, Ifthekar S, Ahuja K, Sarkar B, Singh G, Rana A, et al. Outcomes of thoracolumbar fracture-dislocation managed by short-segment and long-segment posterior fixation: a single-center retrospective study. Int J Spine Surg. 2021;15(1):55–61. https://doi.org/10.14444/8006.
Basaran R, Efendioglu M, Kaksi M, Celik T, Mutlu İ, Ucar M. Finite element analysis of short- versus long-segment posterior fixation for thoracolumbar burst fracture. World Neurosurg. 2019;128:e1109–17. https://doi.org/10.1016/j.wneu.2019.05.077.
Kapoen C, Liu Y, Bloemers FW, Deunk J. Pedicle screw fixation of thoracolumbar fractures: conventional short segment versus short segment with intermediate screws at the fracture level-a systematic review and meta-analysis. Eur Spine J. 2020;29(10):2491–504. https://doi.org/10.1007/s00586-020-06479-4.
Norton RP, Milne EL, Kaimrajh DN, Eismont FJ, Latta LL, Williams SK. Biomechanical analysis of four- versus six-screw constructs for short-segment pedicle screw and rod instrumentation of unstable thoracolumbar fractures. Spine J. 2014;14(8):1734–9. https://doi.org/10.1016/j.spinee.2014.01.035.
Keynan O, Fisher CG, Vaccaro A, Fehlings MG, Oner FC, Dietz J, et al. Radiographic measurement parameters in thoracolumbar fractures: a systematic review and consensus statement of the spine trauma study group. Spine (Phila Pa 1976). 2006;31(5):E156-165. https://doi.org/10.1097/01.brs.0000201261.94907.0d.
Roy-Camille R, Saillant G, Berteaux D, Salgado V. Osteosynthesis of thoraco-lumbar spine fractures with metal plates screwed through the vertebral pedicles. Reconstr Surg Traumatol. 1976;15:2–16.
Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986;203:7–17.
Kanna RM, Shetty AP, Rajashekhran S. Posterior fixation including the fractured vertebra for severe unstable thoracolumbar fractures. Spine J 15:256–264. https://doi.org/10.1016/j.spinee.2014.09.004.
Jindal R, Jasani V, Sandal D, Garg SK. Current status of short segment fixation in thoracolumbar spine injuries. J Clin Orthop Trauma. 2020;11(5):770–7. https://doi.org/10.1016/j.jcot.2020.06.008.
Lin H, Chang M, Wang S, Liu C, Chou P. The fates of pedicle screws and functional outcomes in a geriatric population following polymethylmethacrylate augmentation fixation for the osteoporotic thoracolumbar and lumbar burst fractures with mean ninety five month follow-up. Int Orthop. 2018;42(6):1313–20. https://doi.org/10.1007/s00264-018-3812-3.
Kim H, Park S, Joy H, Ryu J, Kim S, Ju C. Bone cement augmentation of short segment fixation for unstable burst fracture in severe osteoporosis. J Korean Neurosurg Soc. 2008;44(1):8–14. https://doi.org/10.3340/jkns.2008.44.1.8.
Kasliwal MK, Shaffrey CI, Lenke LG, et al. Frequency, risk factors, and treatment of distal adjacent segment pathology after long thoracolumbar fusion: a systematic review. Spine (Phila Pa 1976). 2012;37(22 Suppl):165–79. https://doi.org/10.1097/BRS.0b013e31826d62c9.
Modi HN, Chung KJ, Seo IW, Yoon HS, Hwang JH, Kim HK, et al. Two levels above and one level below pedicle screw fixation for the treatment of unstable thoracolumbar fracture with partial or intact neurology. J Orthop Surg Res. 2009;4:28. https://doi.org/10.1186/1749-799X-4-28.10.1186/1749-799X-4-28.
Ökten Aİ, Gezercan Y, Özsoy KM, Ateş T, Menekşe G, Aslan A, et al. Results of treatment of unstable thoracolumbar burst fractures using pedicle instrumentation with and without fracture-level screws. Acta Neurochir (Wien). 2015;157(5):831–6. https://doi.org/10.1007/s00701-015-2383-y.
Gurwitz GS, Dawson JM, McNamara MJ, Federspiel CF, Spengler DM. Biomechanical analysis of three surgical approaches for lumbar burst fractures using short-segment instrumentation. Spine (Phila Pa 1976). 1993;18(8):977–82. https://doi.org/10.1097/00007632-199306150-00005.
Kramer DL, Rodgers WB, Mansfield FL. Transpedicular instrumentation and short-segment fusion of thoracolumbar fractures: a prospective study using a single instrumentation system. J Orthop Trauma. 1995;9(6):499–506. https://doi.org/10.1097/00005131-199509060-00007.
Tezeren G, Kuru I. Posterior fixation of thoracolumbar burst fracture: short-segment pedicle fixation versus long-segment instrumentation. J Spinal Disord Tech. 2005;18(6):485–8. https://doi.org/10.1097/01.bsd.0000149874.61397.38.
Aly TA. Short segment versus long segment pedicle screws fixation in management of thoracolumbar burst fractures: meta-analysis. Asian Spine J. 2017;11(1):150–60. https://doi.org/10.4184/asj.2017.11.1.150.
Baaj AA, Reyes PM, Yaqoobi AS, Uribe JS, Vale FL, Theodore N, et al. Biomechanical advantage of the index-level pedicle screw in unstable thoracolumbar junction fractures. J Neurosurg Spine. 2011;14(2):192–7. https://doi.org/10.3171/2010.10.SPINE10222.
Wang H, Li C, Liu T, Zhao WD, Zhou Y. Biomechanical efficacy of monoaxial or polyaxial pedicle screw and additional screw insertion at the level of fracture, in lumbar burst fracture: an experimental study. Indian J Orthop. 2012;46(4):395–401. https://doi.org/10.4103/0019-5413.98827.
Bolesta MJ, Caron T, Chinthakunta SR, Vazifeh PN, Khalil S. Pedicle screw instrumentation of thoracolumbar burst fractures: biomechanical evaluation of screw configuration with pedicle screws at the level of the fracture. Int J Spine Surg. 2012;6:200–5. https://doi.org/10.1016/j.ijsp.2012.09.002.
Mahar A, Kim C, Wedemeyer M, Mitsunaga L, Odell T, Johnson B, et al. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine (Phila Pa 1976). 2007;32(14):1503–7. https://doi.org/10.1097/BRS.0b013e318067dd24.
Dobran M, Nasi D, Brunozzi D, di Somma L, Gladi M, Iacoangeli M, et al. Treatment of unstable thoracolumbar junction fractures: short-segment pedicle fixation with inclusion of the fracture level versus long-segment instrumentation. Acta Neurochir (Wien). 2016;158(10):1883–9. https://doi.org/10.1007/s00701-016-2907-0.
El Behairy HF, Abdelaziz AM, Saleh AK, Elsherief FAH, Abuomira IEA, Elkawary AI, et al. Short-segment fixation of thoracolumbar fractures with ıncorporated screws at the level of fracture. Orthop Surg. 2020;12(1):170–6. https://doi.org/10.1111/os.12590.
Guven O, Kocaoglu B, Bezer M, Aydin N, Nalbantoglu U. The use of screw at the fracture level in the treatment of thoracolumbar burst fractures. J Spinal Disord Tech. 2009;22(6):417–21. https://doi.org/10.1097/BSD.0b013e3181870385.
Wang X, Wu X-D, Zhang Y, Zhu Z, Jiang J, Li G, Liu J, Shao J, Sun Y. The necessity of ımplant removal after fixation of thoracolumbar burst fractures—a systematic review. J Clin Med. 2023;12(6):2213. https://doi.org/10.3390/jcm12062213.
Lee JH, Lee JH, Park JW, Shin YH. The insertional torque of a pedicle screw has a positive correlation with bone mineral density in posterior lumbar pedicle screw fixation. J Bone Joint Surg Br. 2012;94(1):93–7. https://doi.org/10.1302/0301-620X.94B1.27032.
Farrokhi MR, Razmkon A, Maghami Z, Nikoo Z. Inclusion of the fracture level in short segment fixation of thoracolumbar fractures. Eur Spine J. 2010;19(10):1651–6. https://doi.org/10.1007/s00586-010-1449-z.
Altay M, Ozkurt B, Aktekin CN, Ozturk AM, Dogan O, Tabak AY. Treatment of unstable thoracolumbar junction burst fractures with short- or long-segment posterior fixation in magerl type a fractures. Eur Spine J. 2007;16(8):1145–55. https://doi.org/10.1007/s00586-007-0310-5.
Shin SR, Lee SS, Kim JH, et al. Thoracolumbar burst fractures in patients with neurological deficit: anterior approach versus posterior percutaneous fixation with laminotomy. J Clin Neurosci. 2020;75:11–8. https://doi.org/10.1016/j.jocn.2020.03.046.
Sasso RC, Renkens K, Hanson D, Reilly T, McGuire RA Jr, Best NM. Unstable thoracolumbar burst fractures: anterior-only versus short-segment posterior fixation. J Spinal Disord Tech. 2006;19(4):242–8. https://doi.org/10.1097/01.bsd.0000211298.59884.24.
Xu GJ, Li ZJ, Ma JX, Zhang T, Fu X, Ma XL. Anterior versus posterior approach for treatment of thoracolumbar burst fractures: a meta-analysis. Eur Spine J. 2013;22(10):2176–83. https://doi.org/10.1007/s00586-013-2987-y.
Wang J, Liu P. Analysis of surgical approaches for unstable thoracolumbar burst fracture: minimum of five-year follow-up. J Pak Med Assoc. 2015;65(2):201–5.
Hinojosa-Gonzalez DE, Estrada-Mendizabal RJ, Bueno-Gutierrez LC, et al. A network meta-analysis on the surgical management of thoracolumbar burst fractures: anterior, posterior, and combined. Spine Surg Relat Res. 2023;7(3):211–8. https://doi.org/10.22603/ssrr.2022-0196. (Published 2023 Mar 13).
Öztürk AM, Süer O, Aydemir S, Kılıçlı B, Akçalı Ö. The effect of the size of pedicle screw on the long-term radiological and clinical results of short-segment posterior instrumentation in the management of thoracolumbar vertebral fractures. Acta Orthop Traumatol Turc. 2024;58(1):20–6.
Dai LY, Jiang LS, Jiang SD. Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures a five to seven-year prospective randomized study. J Bone Joint Surg Am. 2009;91(5):1033–41.
Wang ST, Ma HL, Liu CL, Yu WK, Chang MC, Chen TH. Is fusion necessary for surgically treated burst fractures of the thoracolumbar and lumbar spine?: a prospective, randomized study. Spine. 2006;31(23):1724–31.
Yang H, Shi JH, Ebraheim M, Liu X, Konrad J, Husain I, Tang TS, Liu J. Outcome of thoracolumbar burst fractures treated with indirect reduction and fixation without fusion. Eur Spine J. 2011;20(3):380–6.
Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 41/2-year series. Spine. 2000;25(9):1157–70.
Yung AW, Thng PL. Radiological outcome of short segment posterior stabilisation and fusion in thoracolumbar spine acute fracture. Ann Acad Med Singap. 2011;40(3):140–4.
Hwang JH, Modi HN, Yang JH, Kim SJ, Lee SH. Short segment pedicle screw fixation for unstable T11–L2 fractures: with or without fusion? A three-year follow-up study. Acta Orthop Belg. 2009;75(6):822–7.
Lan T, Chen Y, Hu SY, Li AL, Yang XJ. Is fusion superior to non-fusion for the treatment of thoracolumbar burst fracture? A systematic review and meta-analysis. J Orthop Sci. 2017;22(5):828–33. https://doi.org/10.1016/j.jos.2017.05.014.
Zhang W, Li H, Zhou Y, et al. Minimally invasive posterior decompression combined with percutaneous pedicle screw fixation for the treatment of thoracolumbar fractures with neurological deficits: a prospective randomized study versus traditional open posterior surgery. Spine (Phila Pa 1976). 2016;41 Suppl 19:23–9.
Khoo LT, Palmer S, Laich DT, Fessler RG. Minimally invasive percutaneous posterior lumbar interbody fusion. Neurosurgery. 2002;51(5):166–81.
Hong SH, Suh SP, Yeom J, Kim JY, Lee SG, Han JW. Minimally invasive spine surgery versus open posterior instrumentation surgery for unstable thoracolumbar burst fracture. Asian Spine J. 2021;15(6):761–8. https://doi.org/10.31616/asj.2020.0572.
Deckey JE, Bradford DS. Loss of sagittal plane correction after removal of spinal implants. Spine (Phila Pa 1976). 2000;25(19):2453–60.
Alpert HW, Farley FA, Caird MS, Hensinger RN, Li Y, Vanderhave KL. Outcomes following removal of instrumentation after posterior spinal fusion. J Pediatr Orthop Part B. 2014;34(6):613–7.
Kim H-J, Kang K-T, Moon S-H, Chun H-J, et al. The quantitative assessment of risk factors to overstress at adjacent segments after lumbar fusion: removal of posterior ligaments and pedicle screws. Spine (Phila Pa 1976). 2011;36(17):1367–73.
Singh V, Shorez JP, Mali SA, Hallab NJ, Gilbert JL. Material dependent fretting corrosion in spinal fusion devices: evaluation of onset and long-term response. J Biomed Mater Res B Appl Biomater. 2018;106(8):2858–68. https://doi.org/10.1002/jbm.b.34067.
Oh HS, Seo HY. Percutaneous pedicle screw fixation in thoracolumbar fractures: comparison of results according to implant removal time. Clin Orthop Surg. 2019;11(3):291–6.
Charles YP, Walter A, Schuller S, Steib JP. Temporary percutaneous instrumentation and selective anterior fusion for thoracolumbar fractures. Spine (Phila Pa 1976). 2017;42(9):E523–31.
Jug M, Al Mawed S, Brilej D, Dobravec M, Herman S, Kalacun D, KidričSivec U, Kokalj J, Košar J, Movrin I, Tominc U, Vesel M, Komadina R. Recommendations for treatment of thoracolumbar fractures by the Slovenian Spine Society. Zdrav Vestn. 2021;90:336–59. https://doi.org/10.6016/ZdravVestn.3140.
Kweh BTS, Tan T, Lee HQ, Hunn M, Liew S, Tee JW. Implant removal versus implant retention following posterior surgical stabilization of thoracolumbar burst fractures: a systematic review and meta-analysis. Glob Spine J. 2022;12(4):700–18. https://doi.org/10.1177/21925682211005411.
Author information
Authors and Affiliations
Contributions
Concept: O.S., O.A., A.M.O.
Design: O.S., S.A., B.K., A.M.O.
Supervision: O.S., O.A., A.M.O.
Materials: O.S., S.A., B.K., A.M.O.
Data Collection and/or Processing: O.S., S.A., B.K., A.M.O.
Analysis and/or Interpretation: O.S, O.A., A.M.O.
Literature Search: All authors.
Writing: All Authors.
Critical Review: O.S., O.A., A.M.O.
Corresponding author
Ethics declarations
Our study was accepted as an oral presentation at the 31st National Turkish Orthopedics and Traumatology Congress (25–30 October 2022, Antalya, Turkey) and was published in the congress book. This internet address belongs to the congress oral presentation book (https://www.totbid.org.tr/uploads/31.totbid_kongre_program.pdf). This study has not been published in any journal.
IRB approval
This study was approved by Medical Research Ethics Committee of Ege University (23-1T12).
Competing interests
The authors declare no competing interests.
Additional information
Level of clinical evidence: 3
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Suer, O., Aydemir, S., Kilicli, B. et al. Should the level of the posterior instrumentation combined with the intermediate screw be a short segment or a long segment in thoracolumbar fractures with fusion to the fractured segment?. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-024-02518-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-024-02518-7