Abstract
Background
Timing of surgery remains a topic of debate for hip fracture treatment in the geriatric patient population. The quality indicator “early surgery” was implemented in 2014 at the Department of Trauma Surgery of the University Hospitals Leuven to enhance timely operative treatment. In this follow-up study, we aim to evaluate the performance of this quality indicator, the clinical outcomes, and room for improvement.
Methods
The charts of 1190 patients surgically treated for an acute hip fracture were reviewed between June 2017 and May 2022 at the University Hospitals Leuven. Primary endpoints were adherence to early surgery, defined as surgery within the next calendar day, and the evaluation of the reasons for deviating from this protocol. Secondary endpoints were length of stay (LOS); intensive care unit (ICU) admission and length of ICU stay; mortality after 30 days, 60 days, 90 days, and 6 months; and 90-day readmission rate. Pearson’s Chi-square test and Mann–Whitney U test were used for data analysis.
Results
One thousand eighty-four (91.1%) patients received early surgery versus 106 (8.9%) patients who received delayed surgery. The main reasons for surgical delay were the use of anticoagulants (33%), a general health condition not allowing safe surgery and/or existing comorbidities requiring workup prior to surgery (26.4%), and logistical reasons (17.9%). Patient delay and transfer from other hospitals were responsible for respectively 8.5% and 6.6% of delayed surgery. Early surgery resulted in a significantly shorter LOS and ICU stay (12 [8–25] vs. 18 [10–36] and 3 [2–6] vs. 7 [3–13] days, early vs. delayed surgery, respectively). No significant reduction was observed in ICU admission, mortality, and readmission rate.
Conclusion
We have been able to maintain the early surgery hip fracture protocol in approximately 90% of the patients. Comorbidities and anticoagulant use were responsible for delayed surgery in the majority of the patients. Correct implementation of the existing protocol on anticoagulant use could lead to a one-third decrease in the number of delayed surgeries. Subsequently, since the LOS and ICU stay in the delayed surgery group were significantly longer, a further increase of early surgery will lower the current economic burden.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hip fractures are common injuries among geriatric patients causing a significant socioeconomic burden due to the associated high morbidity and mortality [1]. Hip fractures do not only result in loss of independence and reduced quality of life, but effectively are the leading fall-related cause of death in the elderly [2]. Osteoporosis, increased incidence of fracture comminution, and high incidence of comorbidities all result in a higher risk for complications and mortality in the geriatric population [3]. The mortality following surgery for hip fracture remains high, with a 3-month mortality of 13–19% and 1-year mortality estimated around 26–36% [4,5,6,7]. Among nursing home residents, we see that the outcomes are even worse with a 120-day mortality rate of 38.1% [8]. Management of hip fractures usually requires surgery and a multidisciplinary team approach to maximize recovery in these patients [9, 10].
Timing of surgery is thought to be associated to survival. Early surgery for hip fractures is incorporated as a quality indicator by several international clinical practice guidelines in the field of the orthopedics and trauma surgery. Notably, the National Institute for Health and Care Excellence (NICE) guidelines advocate for surgical intervention within a 48-h window from the patient’s admission to the hospital [11]. Previous investigations have demonstrated 5% heightened odds of 1-year mortality with each 10-h increment in surgical delay [12]. Extant data gleaned from hip registries have revealed that surgical delays surpassing 24 h significantly escalate intra- and postoperative medical complications, such as pressure ulcers and systemic infections, the latter directly attributable to immobilization [13,14,15]. Early surgery directly facilitates early mobilization and its beneficial effects. The nexus between mortality and morbidity is most conspicuous when surgical intervention is postponed beyond the 48-h threshold, persisting throughout the initial year post-fracture [16]. This effect is notably pronounced in patients with heightened comorbidities, as indicated by an increased ASA score.
The Department of Traumatology of the University Hospitals Leuven implemented the quality indicator “early surgery” in 2014, enhancing operative treatment within the next calendar day in geriatric patients suffering a hip fracture. Surgery will only be postponed if the medical condition of the patient can be significantly improved within the next 24–48 h [17]. An evaluation of the care provided in the 3 years preceding and in the 3 years following the protocol was published in 2018. The most room for improvement was seen in keeping the engagement of all stakeholders involved: following the established protocols on the use of DOACs (direct oral anticoagulants) and on logistic arrangements [17]. The actual study is an extended 5-year follow-up study evaluating the performance of our early surgery protocol for geriatric hip fracture patients. The aims of the study are to evaluate the performance of the quality indicator “early surgery” and to measure clinical outcomes. The reasons for surgical delay were analyzed to evaluate if there is still room for improvement.
Methods
Patients
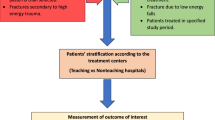
This single-center retrospective study includes a total of 1190 patients aged ≥ 75 who were surgically treated for an acute hip fracture at the University Hospitals Leuven, Belgium, between June 2017 and May 2022. All clinical data were obtained from the medical records and stored at the hospital’s electronic patient file system KWS. Patient inclusion and exclusion criteria are displayed in Fig. 1. Exclusion criteria are periprosthetic fractures, pathological fractures, coxarthrosis electively planned for total hip arthroplasty (THA), and patients requiring revision surgery. The follow-up period was 6 months.
This study was completed in compliance with national legislation and the guidelines of the ethics committee of the University Hospitals Leuven.
Objectives
The aim of the study was to analyze all included geriatric hip fracture cases and to identify the patients not receiving early surgery. Early surgery was defined as surgery within the next calendar day. We assessed demographic characteristics and outcomes of the patients receiving early and delayed surgery. Primary endpoints were adherence to the early surgery protocol and identifying the reasons for delayed surgery. Secondary endpoints were length of stay (LOS); ICU admission and length of ICU stay; mortality after 30 days, 60 days, 90 days, and 6 months; readmission rate; and hospitalization costs. By analyzing the outcomes, we aimed to identify the main reasons for delayed surgery, allowing for optimization of the management of this fragile patient population.
Data collection and analysis
Demographic data and outcomes included age, sex, ASA (American Society of Anesthesiologists) score, date and time of hospital admission, time to surgery, type of surgery, intensive care unit (ICU) admission rate and stay (number of ICU days), length of stay (LOS), hospitalization costs, 90-day readmission rate, 30-day mortality, 60-day mortality, 90-day mortality, and mortality after 6 months. The type of surgery was classified as either hip arthroplasty (hemi and total) or osteosynthesis (proximal femoral nail antirotation, dynamic hip screw, and screw osteosynthesis). LOS was defined as the number of consecutive hospital admission days. The hospitalization costs (cost of daily patient care) were calculated by multiplication of the LOS with the day-based care fee (2017: €763.98; 2018: €746.88; 2019: €722.53; 2020: €756.38; 2021: €830.16; 2022: €801.89). All costs were corrected for inflation with reference to the last year of inclusion (2022). Readmission was defined as rehospitalization within 90 days after discharge. The time of death was obtained from the federal database (Kruispuntbank). Statistical analyses were conducted using SPSS Statistics 28. Continuous variables were noted as median with the interquartile range (IQR) values, and categorical variables were noted as numbers with percentages. Mann–Whitney U test and Pearson Chi-square test were used for data analysis of respectively continuous variables and categorical variables. A P-value less than 0.05 was considered statistically significant.
Results
Early surgery could be achieved in 1084 out of 1190 patients (91.1%). One hundred six patients (8.9%) received delayed surgery. There was no significant difference in surgical delay between the COVID-19 pandemic years (2020–2022) and the previous study years (2017–2019); 8.3% vs. 9.5%, P = 0.437, 2020–2022 vs. 2017–2019, respectively. All patient characteristics in the early and delayed surgery groups are displayed in Table 1. In the total study population, there was a female predominance of 69.4%. However, the gender distribution differed significantly between the two study groups. A female predominance of 70.6% was observed in the early surgery group versus 55.7% in the delayed surgery group (P < 0.001). The ASA scores significantly differed between both study groups, especially the percentage of ASA 3 and ASA 4 indicating more comorbidities in the delayed surgery group (70.1% ASA 3 and 8.2% ASA 4 in early surgery group versus 59.4% ASA 3 and 21.7% ASA 4 in the delayed surgery group; P < 0.001). The most frequently applied surgical treatment for the total population was proximal femoral nail antirotation (PFNA), received by 616 patients (51.8%). Other surgery types were hemi-hip arthroplasty (HHA) performed in 473 patients (39.7%), screw osteosynthesis applied in 45 patients (3.8%), dynamic hip screw performed in 41 patients (3.4%), and total hip arthroplasty (THA) applied in 15 patients (1.3%). Treatment type prevalence was found to be significantly different between the two study groups (P < 0.001). PFNA was the primary surgery type in the early surgery group (584 patients, 53.9%) with HHA as second (416 patients, 38.4%). HHA was the most common treatment in the delayed surgery group (57 patients, 53.8%) and secondly PFNA (32 patients, 30.2%). Treatment with a dynamic hip screw and screw osteosynthesis was equally distributed between the two groups, performed in 3.4% and 3.8% of the early and delayed surgery group, respectively. There were only a few patients with a THA in both groups (0.9% vs. 4.7%, early vs. delayed surgery group, respectively). Hip arthroplasty (HHA and THA) was twice as likely to be delayed as hip osteosynthesis (12.7% vs. 6.3%, respectively).
The median LOS of the total study population was 12 days (IQR 8–26 days). The median LOS was found to be significantly shorter in the early surgery group compared to the delayed group: 12 days (IQR 8–25 days) in the early surgery group and 18 days (IQR 10–36 days) in the delayed surgery group (P < 0.001). The median hospitalization costs per patient were €9125.85 (IQR €5963.74–€19,426.10). The median hospitalization costs were significantly lower in the early surgery group (€9014.90 [IQR €5761.89–€18,920.85] vs. €13,811.36 [IQR €7883.52–€27,911.89]) compared to the delayed surgery group (P < 0.001).
Sixty-nine patients from the total population of 1190 were transferred to the ICU with a median stay of 4.7 days. The number of ICU admitted patients was equally distributed between the early and delayed surgery groups, amounting to 61 (5.6%) and 6 (7.5%) patients, respectively (P = 0.420). However, the duration of stay at the ICU was significantly different, with a median stay of 4.2 days in the early surgery group and 8.5 days in the delayed surgery group (P = 0.041).
For the whole study group, the 30-day mortality rate was 8.1%, the 90-day mortality rate was 14.5%, and the 6-month mortality rate after treatment for acute hip fracture was 21.6%. There was no significant difference in 30-day, 60-day, 90-day, and 6-month mortality rates between the two study groups. The 90-day readmission rates as well were equally distributed between the early surgery and delayed surgery group; in total, 176 patients (14.7%) were readmitted within 90 days from discharge (161 [14.9%] vs. 15 [14.2%], P = 0.846, early vs. delayed surgery group, respectively).
To determine possible room for improvement, the reasons for surgical delay were defined for all 106 patients not operated within the next calendar day. The results are shown in Fig. 2 and Table 2. The main reasons for delayed surgery were the use of anticoagulants (35 patients, 33.0%), the general condition of the patients, and medical reasons not allowing for safe surgery within the next calendar day (e.g., infectious, cardiovascular, or pulmonary comorbidities) or the presence of comorbidities requiring workup prior to surgery (28 patients, 26.4%) and logistical problems (19 patients, 17.9%). In case of logistical problems and the use of anticoagulants, the patients who could not be operated within the next calendar day were most likely to be operated the day after. Some of the latter still met the NICE guidelines criteria of operation within 48 h. Late presentation and transfer from other hospitals were responsible for, respectively, 8.5% (9 patients) and 6.6% (7 patients) of delayed surgeries. When for some patients a combination of factors was responsible for the delay in surgery, we only considered the main reason registered as cause in the patient chart for this study.
Pie chart for surgical delay: poor general condition and/or comorbidities, 28 (26.4%); late presentation, 9 (8.5%); delayed diagnosis (in hospital), 4 (3.8%); anticoagulation protocol violation, 35 (33.0%); logistics, 19 (17.9%); initial non-operative conservative treatment, 4 (3.8%); transfer from other hospital, 7 (6.6%)
Discussion
This study aimed to analyze the current adherence to the “early surgery” protocol in geriatric patients surgically treated for an acute hip fracture between June 2017 and May 2022 in the University Hospitals Leuven. Outcomes were evaluated and the reasons for surgical delay were identified. We reviewed a large cohort of 1190 patients with a follow-up time of 6 months. Our study demonstrates a 91.1% adherence to the early surgery protocol over the period 2017–2022. There is a slight improvement compared to the 85% adherence achieved over a 5-year time period. This illustrates the beneficial effect of our efforts to keep all stakeholders involved by providing feedback on their performance on a regular base and implementing strategies for improvement [12].
Our findings show a significantly shorter LOS for patients receiving early surgery compared to those receiving delayed surgery (median LOS of 12 days compared to 18 days in the early and delayed surgery group, respectively). This is in line with our previous findings and with recent literature [17,18,19]. In our study, the number of patients admitted to the ICU was comparable between the early and delayed surgery group. However, the duration of ICU admission showed a significant difference, with an average duration of 4.2 days in the early surgery group versus 8.5 days in the delayed surgery group (P = 0.041 < 0.05). This effect has not been evaluated by other authors but undoubtably has a positive effect on total LOS.
Our study could not show a positive impact of early surgery on the 30-day, 60-day, 90-day, and 6-month mortality rates. Literature on this topic still is controversial [20,21,22,23,24,25]. As there is currently no consensus regarding optimal surgical timing, one can also question if even earlier surgery should be beneficial as was investigated in the HIP ATTACK study. The authors concluded that surgery within 6 h of admission was not superior to standard care in terms of primary outcomes of mortality and a composite of major complications [26]. These findings encourage us to keep to the definition of early surgery as surgery within the next calendar day.
We found no effect of the COVID-19 pandemic on the number of delayed surgeries. The explanation for this is that hip fractures are given the highest priority in our hospital, even during the COVID-19 pandemic. In 106 patients (8.9%) of our study group, early surgery could not be performed. In 26.4% of the cases (28 patients), the surgical delay was caused by medical comorbidities. These patients first require optimization of their general condition or workup of their comorbidities in order to allow for safe surgery. In this patient group, timely surgery will most likely never be possible due to the need for prior stabilization of their condition. Lizaur-Utrilla et al. found in their study that delay of surgery in medically fit patients caused by logistical reasons resulted in significant higher postoperative complication rates. However, if the patients were medically not fit for surgery and required workup, the delay did not result in higher complication or mortality rates [27]. Previous studies already proved that the presence of ischemic heart disease, congestive heart failure, paroxysmal atrial fibrillation, and chronic renal failure, as well as male gender and older age, was significantly associated with higher early and late mortality [28]. Optimization before surgery is beneficial, especially in patients with multi-comorbidities. To allow for safe surgery as soon as possible, it is important to define goals when optimizing patients. This will help to keep the time to surgery as short as possible in this frail patient population [29]. 33.0% of the delayed surgery group (35 patients) was related to the use of VKAs (vitamin K antagonists) and DOACS. There still is controversy about timing of surgery in patients taking these medications. A good knowledge of the pharmacology of these drugs and of the availability of antidotes is of utmost importance. For our department, a protocol based on the guidelines of the European Hearth Rhythm Association was developed in collaboration with the anesthesiology and cardiology department [30]. The effects of vitamin K antagonists can be offset by the administration of vitamin K and monitoring the INR (international normalized ratio). Literature shows that an INR value of < 1.6 is a safe value for hip fracture surgery. With higher INR values, an increased risk of both transfusion and 30-day mortality is seen [31]. An INR value of > 1.5 independently increased the risk of mortality in surgical patients [32]. Effective INR reversal can take several hours, and in case of failed reversal with vitamin K treatment, prothrombin complexes can be used. Concerning DOACs however, an antidote is not yet available for all types. For dabigatran with a half-life of 14–18 h depending on the degree of renal impairment, the antidote idarucizumab is available for use in uncontrolled bleeding or in case of emergency surgery. For other DOACs (e.g., rivaroxaban and apixaban), antidotes are not available, but as they have a much shorter half-life of 7–9 h, a discontinuation of 24 h before surgery is sufficient [30]. In a recent study however, Rommens et al. could even show there are no detrimental effects of surgery within 24 h of admission for directly anticoagulated patients [33]. These findings should encourage us to keep to our definition of early surgery as surgery within the next calendar day, even for patients under anticoagulants. Despite the availability of this protocol in our department, it was not followed, and 35 patients on anticoagulants received delayed surgery. So the correct implementation of this criterion could lead to a one-third reduction in the total number of patients receiving delayed surgery.
The cost of the antidote (idarucizumab) is often argued to inequitably increase hospital costs. Connors et al. estimated the acquisition cost of two 2.5 g vials of idarucizumab at €3246.80 [34]. When looking at the difference in hospitalization costs (median €9014.90 versus €13,811.36 in the early and late surgery group, respectively) in our study however, this extra cost seems reasonable.
Besides a reduction in bleeding complications, Pollack also showed a reduction in the use of blood products and pro-hemostatic agents with the use of Praxbind, resulting in indirect cost savings as well [35]. Another 26.4% of the cases (28 patients) of delayed surgery in our study could be appointed to logistical problems. Furthermore, hip arthroplasty was twice as likely to be delayed compared to hip osteosynthesis. When looking in the patients’ charts, this was attributed to logistical problems as well: availability of a surgeon being able to perform prosthetic surgery and of the necessary equipment.
A similar distribution with more surgeries on the day of admission for intertrochanteric fractures (treated by osteosynthesis) and relatively more surgeries on the first and second day after admission for femoral neck fractures (treated by prosthetic joint replacement) was observed in the study of Leicht et al. In their study, the authors could show a higher risk of mortality for patients with intertrochanteric fractures who were operated on the second day after admission. This risk was not present in the patients who were treated with prosthetic joint replacement [36]. In our study, we did not see an increased risk of mortality in the delayed surgery group in general. As our study population was relatively small, we did not do a subgroup analysis based on fracture or treatment type. Both numbers of delayed surgery caused by anticoagulants and logistical problems are in the same range as in our previous study [17]. This should be a strong signal we have to provide better strategies to overcome this delay. In Table 3, we provide some strategies to solve these problems including strategies to decrease patient delay and transfer time from other hospitals. It is clear that all healthcare providers involved should continue (re)assessing their established protocols.
The strength of our study lies in the evaluation of a large cohort of patients (1190) in a single-center study, so we may assume similar surgical procedures and anesthetic techniques reducing bias. As we learned from our previous experience, no more personal preferences of surgeons to delay surgery have been noticed, and the numbers of logistical reasons for delay decreased from 23.9 to 17.9%.
There are also some limitations to this study. First, the single-center design makes it difficult to generalize results. Second, due to the retrospective data collection, there is some missing information especially about the administration of antidotes. As the information on the administration of idarucizumab and prothrombin complexes sometimes is missing, there might be an underestimation of patients having received antidotes. Furthermore, when patients were transferred from another hospital, information on the reason for transfer was often missing, making it difficult to determine the exact reason for surgical delay. Finally, only mortality, ICU admission, and 30-day readmission rates were evaluated as outcome parameter, so the possible beneficial effects of early surgery on other complications were not evaluated.
Conclusion
In this extended 5-year follow-up period after implementation of the early surgery protocol in our hospital, the results are still good; more than 90% of the patients do receive early surgery. Due to comorbidities, it will not be possible to provide early surgery to approximately one-third of the patients. However, there is still room for improvement, especially for patients receiving anticoagulants and for patients not receiving early surgery due to logistical problems. Consequently, we should continue our efforts as early surgery will lead to economic advantages (shorter LOS) even when including the extra costs for DOACs antidotes. In our improvement strategies, providing feedback on their performance to all healthcare specialists involved in the care for geriatric hip fracture patients is of utmost importance.
Data availability
No datasets were generated or analyzed during the current study.
References
Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7:407–13.
Deprey SM, Biedrzycki L, Klenz K. Identifying characteristics and outcomes that are associated with fall-related fatalities: multi-year retrospective summary of fall deaths in older adults from 2005–2012. Inj Epidemiol. 2017;4(1):21.
Ekman E, Nurmi H, Reito A, et al. Complications following 250 cemented modular hip hemiarthroplasties. Scand J Surg. 2019;104:321–8.
Librero J, Peiró S, Leutscher E, et al. Timing of surgery for hip fracture and in-hospital mortality: a retrospective population-based cohort study in the Spanish national health system. BMC Health Serv Res. 2012;12:15.
Chiarello E, Tedesco G, Cadossi M, et al. Surgical prevention of femoral neck fractures in elderly osteoporotic patients: a literature review. Clin Cases Miner Bone Metab. 2016;13:42–5.
Librero J, Peiro S, Leutscher E, et al. Timing of surgery for hip fracture and in-hospital mortality: a retrospective population-based cohort study in the Spanish national health system. BMC Health Serv Res. 2012;12:15.
Abrahamsen B, Van Staa T, Ariely R, et al. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009;20:1633–50.
Neuman M, Silber J, Magaziner J, et al. Survival and functional outcomes after hip fracture among nursing home residents. JAMA Intern Med. 2014;174:1273–80.
Handoll HH, Cameron ID, Mak JC, Panagoda CE, Finnegan TP. Multidisciplinary rehabilitation for older people with hip fractures. Cochrane Database Syst Rev. 2021;11(11):CD007125. https://doi.org/10.1002/14651858.CD007125.pub3.
Figved W, Myrstad M, Saltvedt I, Finjarn M, Flaten Odland L, Frihagen F. Team approach: multidisciplinary treatment of hip fractures in elderly patients. JBJS Reviews. 2019;7(6):e6–e6. https://doi.org/10.2106/JBJS.RVW.18.00136.
NICE. Hip fracture: management, Clinical guideline [CG124]. 2014.
Maheshwari K, Planchard J, You J, et al. Early surgery confers 1-year mortality benefit in hip-fracture patients. J Orthop Trauma. 2018;32(3):105–10. https://doi.org/10.1097/BOT.0000000000001043.
Cordero J, Maldonado A, Iborra S. Surgical delay as a risk factor for wound infection after a hip fracture. Injury. 2016;47:S56–60. https://doi.org/10.1016/S0020-1383(16)30607-6.
Haleem S, Heinert G, Parker MJ. Pressure sores and hip fractures. Injury. 2008;39(2):219–23. https://doi.org/10.1016/j.injury.2007.08.030.
Verbeek DOF, Ponsen KJ, Goslings JC, Heetveld MJ. Effect of surgical delay on outcome in hip fracture patients: a retrospective multivariate analysis of 192 patients. Int Orthop. 2008;32(1):13–8. https://doi.org/10.1007/s00264-006-0290-9.
Leer-Salvesen S, Engesæter LB, Dybvik E, Furnes O, Kristensen TB, Gjertsen JE. Does time from fracture to surgery affect mortality and intraoperative medical complications for hip fracture patients? An observational study of 73 557 patients reported to the Norwegian hip fracture register. Bone Jt J. 2019;101-B(9):1129–37. https://doi.org/10.1302/0301-620X.101B9.BJJ-2019-0295.R1.
Sermon A, et al. The implementation of a clinical pathway enhancing early surgery for geriatric hip fractures: how to maintain a success story? Eur J Trauma Emerg Surg. 2019;45:199–205.
Lieten S, et al. Analysis of the effects of a delay of surgery in patients with hip fractures: outcome and causes. Osteoporos Int. 2021;32:2235–45.
Kristan A, Omahen S, Tosounidis, et al. When does hip fracture surgery delay affects the length of hospital stay? Eur J Trauma Emerg Surg. 2019;45:701–8.
Muller F, Galler M, Zellner M, et al. Total hip arthroplasty for hip fractures: time to surgery with respect to surgical revision, failure and mortality. Geriatr Orthop Surg Rehabil. 2019;10:2151459318818162.
Kristan A, et al. Causes for delay of surgery in hip fractures and how it impacts on mortality – a single level 1 trauma center experience. ACHOT; 1/2021.
Ryan DJ, Yoshihara H, Yoneoka D, et al. Delay in hip fracture surgery: an analysis of patient-specific and hospital-specific risk factors. J Orthop Trauma. 2015;29:343–8.
Siga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis and meta-regression. Can J Anaesth. 2008;55:146–54.
Welford P, et al. The association between surgical fixation of hip fractures within 24 hours and mortality: a systematic review and meta-analysis. Bone JT J. 2021;103B:1176–86.
Lefaivre KA, et al. Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Joint Surg Br. 2009;91(7):922–7.
HIP Attack Investigators. Accelerated surgery versus standard care in hip fracture: an international, randomized, controlled trial. Lancet. 2020;395:698–708.
Lizaur-Utrilla A, Gonzalez-Navarro B, Vizcaya-Moreno MF, Miralles Muñoz FA, Gonzalez-Parreño S, Lopez-Prats FA. Reasons for delaying surgery following hip fractures and its impact on one year mortality. Int Orthop. 2019;43(2):441–8.
Yaacobi, et al. Mortality following surgery for geriatric hip fractures: is it the timing or the co-morbidities? Hip Int. 2022;32(2):271–5.
Wilson H. Orthogeriatrics in hip fracture. Open Orthop J. 2017;11(Suppl-7 M2):1181–9.
Steffel J, Verhamme P, Potpara TS, et al. The 2018 European Hearth Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation.
Mekkawy K, Chaudhry Y, Mawn J, et al. Determining a preoperative international normalized ratio threshold safe for hip fracture surgery. Hip Int. https://doi.org/10.1177/11207000221148096.
Tamim H, Habbal M, Saliba A, et al. Preoperative INR and postoperative major bleeding and mortality: a retrospective cohort study. J Thromb Thrombolysis. 2016;41:301–11.
Devlieger BK, Rommens PM, Baranowski A, Wagner D. Early hip fracture surgery in patients taking direct anticoagulants improves outcome (2023) Research Square. 2023. https://doi.org/10.21203/rs.3.rs-3120714/v1.
Connors J, et al. Idarucizumab (Praxbind) formulary review. Crit Pathw Cardiol. 2016;15(3):77–81.
Pollack C, Bernstein R, Dubiel R, et al. Healthcare resource utilization in patients receiving idarucizumab for reversal of dabigatran anticoagulation due to major bleeding, urgent surgery, or procedural interventions: interim results from the RE-VERSE AD study. J Med Econ. 2017;5:435–42.
Leicht H, Gaertner T, Günster C, et al. Time to surgery and outcome in the treatment of proximal femoral fractures. Dtsch Arztebl Int. 2021;118:454–61. https://doi.org/10.3238/arztebl.m2021.0165.
Author information
Authors and Affiliations
Contributions
AS and EV wrote the main manuscript text, EV and LA collected the data, and HH did the statistics and outlined the manuscript body. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was completed in compliance with national legislation and the guidelines of the ethics committee of the University Hospitals Leuven (S-66890).
Competing interests
The authors declare no competing interests.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sermon, A., Verhulst, E., Aerden, L. et al. A retrospective chart analysis with 5-year follow-up of early care for geriatric hip fracture patients: why we should continue talking about hip fractures. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-024-02514-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-024-02514-x