Abstract
Background
An emergency department thoracotomy (EDT) is performed in critically injured patients after a recent or in an imminent cardiac arrest following trauma. Emergent thoracotomy (ET) or operation room thoracotomy is reserved for more stable patients. However, the number of these interventions performed in an European settings is limited. Thus, we initiated the current study to investigate outcomes and risk factors for mortality of patients required EDT or ET at the largest trauma center in Estonia.
Methods
All patients admitted after trauma to the North Estonia Medical Centre between 1/1/2017 and 31/12/2021 subjected to EDT or ET were included. Primary outcome was 30-day mortality.
Results
Overall, 39 patients were included. EDT and ET were performed in 16 and 23 patients, respectively. Median age was 45 (33–53) years and 89.7% were males. The crude 30-day mortality was 56.4% being 87.5% and 34.8% in the EDT and ET group, respectively. None of the patients with pre-hospital CPR requirement, severe head injury (AIS head ≥ 3) or severe abdominal injury (AIS abdomen ≥ 3) survived. All the patients in the survival group had signs of life in the emergency department. The rate of stab wounds was significantly higher in the survival group (p = 0.007). Patients with CGS < 9 had significantly lower possibility for survival (p < 0.001).
Conclusions
EDT and ET outcomes in Estonian trauma system are comparable to similar advanced trauma systems in Europe. Patients with GCS > 8, signs of life in the ED and with isolated penetrating chest injury had the most favorable outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An emergency department thoracotomy (EDT) is performed in critically injured patients after a recent or in an imminent cardiac arrest following trauma. Emergent thoracotomy (ET) or operation room thoracotomy is reserved for more stable patients sustaining transport to an operating room. However, less than 5% of patients with blunt trauma and only about 20% of patients with penetrating injuries require thoracotomy; thus, the number of these interventions performed in an European settings is limited [1]. We initiated the current study to investigate outcomes and risk factors for mortality of patients required EDT or ET at the largest trauma center in Estonia and compare outcomes with recent studies from other European trauma centers. We hypothesized that our outcomes are comparable to outcomes in similar European trauma systems.
Materials and methods
After the Research Ethics Committee approval, all patients admitted after trauma to the North Estonia Medical Centre (NEMC) between 1/1/2017 and 31/12/2021 subjected to EDT or ET were included using the NEMC trauma repository. EDT was defined as a left-sided anterolateral or a clamshell thoracotomy performed in the emergency department (ED) for the patients in an imminent or a recent cardiac arrest due to trauma. ET was defined as a thoracotomy performed for trauma patients in an operating room during the first 24 h after admission to the emergency department. Patients subjected to sternotomy were excluded. Signs of life were defined as a pupil reaction, spontaneous breathing, carotid pulse, measurable or palpable pulse, movement of extremities and/ or cardiac electrical activity on admission to the ED [2]. EDT indications at the study site followed the Western Trauma Association guidelines to perform EDT including CPR time less than 15 min for penetrating torso injuries, less than 10 min for blunt trauma and less than 5 min for extrathoracic penetrating injuries [3]. Due to an aggressive management policy at the study site, occasional EDT was performed, while CPR time exceeded the suggested time frame by Western Trauma Association. Likewise, ET classical indications were utilized including hemorrhagic shock, immediately > 1000 ml blood from the chest tube, ongoing blood loss of 150–200 ml per hour from the chest tube or a massive air leak with respiratory failure. Also, rib fixations performed during the first 24 h after admission were included.
Pre-hospital thoracotomies were not performed in our trauma system during the study period.
All the acute care general surgeons on call have passed the Advanced Trauma Life Support (ATLS), Advanced Surgical Skills for Exposure in Trauma (ASSET) and Definitive Surgical Trauma Care (DSTC) courses. Also, most of the general surgeons taking trauma calls have practiced in large trauma centers in South Africa or USA.
Data collection included demographics, management, hospital length of stay (HLOS), abbreviated injury scale (AIS), injury severity score (ISS), revised trauma score (RTS), 30-day mortality, expected mortality per TRISS score and standardized mortality ratio (SMR; ratio of observed deaths to predicted deaths per TRISS).
Primary outcome was 30-day mortality. Secondary outcomes were risk factors for mortality.
Data were collected using the REDCap system (Vanderbilt, USA). The p values for continuous variables were derived from the Student’s t test or the Mann–Whitney U test, and for categorical variables, the Fisher’s exact test was utilized (two-tailed probability was obtained by doubling the exact one-tailed probability). Values are reported as median and interquartile range (IQR) for continuous variables or as a number and percentage for categorical variables. All statistical analyses were performed with the R-program version 3.3.2 (R Foundation, Vienna, Austria).
Results
In total, 39 patients met the inclusion criteria. EDT and ET were performed in 16 and 23 patients, respectively. 93.8% (n = 15) of the EDTs were performed by acute care general surgeons on call and 6.2% (n = 1) by thoracic surgeons on call. Seven (30.4%) and sixteen (69.6%) of the ETs were performed by acute care general surgeons and thoracic surgeons, respectively. Table 1 depicts demographics and outcomes of all patients. The vast majority of the patients were males. Penetrating injuries constituted 56% of the cases. All the patients admitted to the operating room for ET had signs of life in the ED. Median RTS was significantly lower and median ISS significantly higher in the EDT group. The crude 30-day mortality was 56.4% (survival rate 43.6%) being 87.5% and 34.8% in the EDT and ET group, respectively. Overall, in the EDT and ET group the predicted mortality rate per TRISS and crude 30-day mortality were almost identical.
Overall 30-day crude mortality after penetrating injuries was 45.5% being 83.3% and 31.3% after EDT and ET, respectively. After blunt injuries overall mortality was 70.6% being 90.0% and 42.9% after EDT and ET, respectively.
In total, the main cause of death was hemorrhagic shock, multiple organ failure and brain injury at 59.1%, 31.8% and 9.1% of the deceased patients, respectively.
Overall, most frequent mechanisms of injury were stab wounds (SW) followed by gunshot wounds (GSW) and motor vehicle accidents (Table 2). GSW was the most common mechanism of injury in the EDT group.
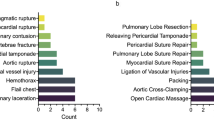
Overall, 92.3% of the patients had thoracic injuries being most often injured region. Most frequent injuries in the chest region were cardiac injuries (48.7%), lung injuries (43.6%) and rib fractures (38.5%). Most frequent vascular injuries in the thoracic region were intercostal artery lesion (10.3%), internal thoracic artery injury (10.3%) and thoracic aortic injury (5.1%).
Indications for ET were hemorrhagic shock in 52.2%, cardiac tamponade in 30.4%, a massive air leak in 13.0% (subjected to rib fixation during the first 24 h after admission) and ongoing bleeding from a chest tube in 4.3% of the cases.
Table 3 compares demographic and injury profiles of the patients who survived vs. deceased. None of the patients who required pre-hospital CPR survived, and all the surviving patients had signs of life in the ED (Fig. 1). Median CPR time for patients requiring CPR and received EDT was 14 min. The rate of stab wounds was significantly higher in the survival group, and penetrating injuries overall were associated with a significant trend (p = 0.055) toward higher rate of survival. Only one patient who required laparotomy survived. All the patients with severe head and/or abdominal injuries deceased.
Two patients in the EDT group survived with survival rate at 12.5%. Both of the patients were neurologically intact at discharge from hospital. Mechanism of injury was GSW in one survivor and auto vs. pedestrian in the second survivor; thus, survival rate after blunt injuries and penetrating injuries was 10.0% and 16.7%, respectively. Both of the survivors had signs of life in the ED, and they did not require pre-hospital CPR. The patient with GSW had a left innominate vein and lung injury. The second survivor had bilateral multiple rib fractures with flail chest on both sides, bilateral lung lacerations, blunt cardiac injury, splenic injury and unstable pelvic injury (Tile C). Left anterolateral thoracotomy and clamshell thoracotomy were performed for 81.2% and 18.8% patients in the EDT group, respectively. Half of the patients (n = 8) deceased in the ED due to cardiac arrest secondary to hemorrhagic shock, and other were taken to the operating theatre after the EDT. Six of the patients deceased in the ICU secondary to MOF. Table 4 compares survivors and deceased patients after EDT. Pre-hospital CPR requirement showed a trend toward higher possibility for death (p = 0.166).
Discussion
EDT and ET are potentially life-saving surgical efforts in critically injured trauma victims with a limited experience in the European settings. Thus, we initiated the current study to add valuable and recent data from an evolving Estonian trauma center.
Table 5 includes recent studies (published between 2012 and 2022) reporting outcomes of both EDT and ET following blunt and penetrating injuries from European trauma centers [4,5,6,7,8,9]. The prevalence of these interventions is rather low in all of the studies with largest cohort being investigation by Lustenberger and colleagues from Switzerland including 121 cases [4]. Overall survival rates reported range between 17 and 59%; however, there is significant heterogeneity between the available studies. Survival rate in our study was 44% being in the middle of the outcomes range compared to other reports [4,5,6,7,8,9]. Most frequent factors related to survival benefit per the reports from the European trauma centers including our study are penetrating injury, GCS > 8 on arrival, signs of life in the ED and lower ISS [4, 5, 9]. Likewise, we observed that none of the patients with severe abdominal injury, severe head injury or pre-hospital CPR survived. Penetrating injuries constituted 19–64% of the cases being predominately stab wounds [4,5,6,7,8,9]. Our penetrating injury rate is rather high at 56% (Table 2). Thus, we conclude that the typical patient with best possibility for survival would be patient having penetrating trauma with isolated chest injury and signs of life on arrival to the ED.
Survival rate after EDT was 12.5% in our study being 10.0% after blunt injuries and 16.7% after penetrating trauma. Despite the rather low number of EDT cases (n = 16) the pre-hospital CPR requirement still showed a significant trend toward negative outcome (Table 4). In our study none of the patients requiring prehospital CPR survived. A large study utilizing the TraumaRegister DGU® reported survival rate of 4.8% and 20.7% after blunt and penetrating injuries, respectively [10]. This study also found that CPR requirement resulted in worse outcome. Large studies from USA found that independent risk factors for survival are age < 60 years, penetrating mechanism of injury, no pre-hospital CPR and signs of life in the ED [11, 12]. Most of the survivors were between 20 and 49 years old. Outcomes after EDT for blunt trauma patients without signs of life are dismal with survival rate of 0.7% and neurologically intact survival rate of 0.1% [13]. These results raise a question that should we abandon the EDT in older patients with major blunt injury patterns and no signs of life in the ED? Per our reported data observing minimal chance of survival in these selected patients our trauma system is prepared to continue with an aggressive resuscitation policy due to occasional survivors and the low prevalence of EDT and ET that does not burden the trauma system. Nevertheless, selection of appropriate patients is a very controversial subject and every hospital designs their respective management strategy.
Furthermore, it is of paramount importance to improve the EDT and ET outcomes. In our trauma setting, all the acute care surgeons taking calls have passed the ATLS, ASSET and DSTC courses. Also, a large proportion of the acute care surgeons staffing trauma calls in our trauma center are instructors on abovementioned educational instruments. Thus, the training component is an integral component of our trauma facility. Also, we are currently improving our transfusion policy by initiating a full blood transfusion protocol for massively bleeding trauma victims to further improve outcomes of these severely injured patients.
The resuscitative endovascular balloon occlusion of aorta (REBOA) is a promising avenue for patients with non-compressible torso hemorrhage; however, variability in indications and patient characteristics prevents any definitive conclusions [14].
Pre-hospital thoracotomy is not utilized in our trauma system in Estonia due to rather low number of cases, thus, without possibility for adequate experience for pre-hospital personnel.
Conclusion
Emergency department thoracotomy and emergent thoracotomy outcomes in Estonian trauma system are comparable to similar advanced trauma systems in Europe, resulting in improved outcomes in low case burden. Patients with GCS > 8, signs of life in the ED and with isolated penetrating chest injury have the most favorable outcomes.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Demetriades D. The initial assessment and management of the trauma patient. 6th Edition. 2014.
Working Group. Ad Hoc Subcommittee on Outcomes, American College of Surgeons. Committee on Trauma. Practice management guidelines for emergency department thoracotomy. Working Group, Ad Hoc Subcommittee on Outcomes, American College of Surgeons-Committee on Trauma. J Am Coll Surg. 2001;193(3):303–9.
Moore EE, Knudson MM, Burlew CC, Inaba K, Dicker RA, Biffl WL, Malhotra AK, Schreiber MA, Browder TD, Coimbra R, Gonzalez EA, Meredith JW, Livingston DH, Kaups KL, WTA Study Group. Defining the limits of resuscitative emergency department thoracotomy: a contemporary western trauma association perspective. J Trauma. 2011;70(2):334–9.
Lustenberger T, Labler L, Stover JF, Keel MJ. Resuscitative emergency thoracotomy in a Swiss trauma centre. Br J Surg. 2012;99(4):541–8.
Kandler K, Konge L, Rafiq S, Larsen CF, Ravn J. Emergency thoracotomies in the largest trauma center in Denmark: 10 years’ experience. Eur J Trauma Emerg Surg. 2012;38(2):151–6.
Johannesdottir BK, Mogensen B, Gudbjartsson T. Emergency thoracotomy as a rescue treatment for trauma patients in Iceland. Injury. 2013;44(9):1186–90.
Segalini E, Donato LD, Birindelli A, Piccinini A, Casati A, Coniglio C, Saverio SD, Tugnoli G. Outcomes and indications for emergency thoracotomy after adoption of a more liberal policy in a western European level 1 trauma centre: 8-year experience. Updates Surg. 2019;71(1):121–7.
Thorsen K, Vetrhus M, Narvestad JK, Reite A, Larsen JW, Vennesland J, Tjosevik KE, Søreide K. Performance and outcome evaluation of emergency resuscitative thoracotomy in a Norwegian trauma centre: a population-based consecutive series with survival benefits. Injury. 2020;51(9):1956–60.
Sam ASY, Nawijn F, Benders KEM, Houwert RM, Leenen LPH, Hietbrink F. Outcomes of the resuscitative and emergency thoracotomy at a Dutch level-one trauma center: are there predictive factors for survival? Eur J Trauma Emerg Surg. 2022;48(6):4877–87.
Schulz-Drost S, Merschin D, Gümbel D, Matthes G, Hennig FF, Ekkernkamp A, Lefering R, Krinner S, TraumaRegister DGU. Emergency department thoracotomy of severely injured patients: an analysis of the TraumaRegister DGU®. Eur J Trauma Emerg Surg. 2020;46(3):473–85.
Joseph B, Khan M, Jehan F, Latifi R, Rhee P. Improving survival after an emergency resuscitative thoracotomy: a 5-year review of the trauma quality improvement program. Trauma Surg Acute Care Open. 2018;3(1): e000201.
Panossian VS, Nederpelt CJ, El Hechi MW, Chang DC, Mendoza AE, Saillant NN, Velmahos GC, Kaafarani HMA. Emergency resuscitative thoracotomy: a nationwide analysis of outcomes and predictors of futility. J Surg Res. 2020;255:486–94.
Seamon MJ, Haut ER, Van Arendonk K, Barbosa RR, Chiu WC, Dente CJ, Fox N, Jawa RS, Khwaja K, Lee JK, Magnotti LJ, Mayglothling JA, McDonald AA, Rowell S, To KB, Falck-Ytter Y, Rhee P. An evidence-based approach to patient selection for emergency department thoracotomy: a practice management guideline from the Eastern Association for the surgery of trauma. J Trauma Acute Care Surg. 2015;79(1):159–73.
Castellini G, Gianola S, Biffi A, Porcu G, Fabbri A, Ruggieri MP, Coniglio C, Napoletano A, Coclite D, D’Angelo D, Fauci AJ, Iacorossi L, Latina R, Salomone K, Gupta S, Iannone P, Chiara O. Resuscitative endovascular balloon occlusion of the aorta (REBOA) in patients with major trauma and uncontrolled haemorrhagic shock: a systematic review with meta-analysis. World J Emerg Surg. 2021;16(1):41.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Sten Saar, Edgar Lipping, Artjom Bahhir, Maarja Talviste, Marika Väli, Jaak Lepp and Peep Talving declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Saar, S., Lipping, E., Bahhir, A. et al. Outcomes of resuscitative and emergent thoracotomies following injury at the largest trauma center in Estonia. Eur J Trauma Emerg Surg 50, 243–248 (2024). https://doi.org/10.1007/s00068-023-02284-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02284-y