Abstract
Purpose
The use of three-dimensional printing models in medical practice has been booming recently and its application to orthopedic surgery is gaining popularity. When treating fractures by open reduction and internal fixation, potential benefits have been associated with the use of 3D printing models. This review aims to quantitatively analyze the effectiveness of using 3D printing models in fracture management.
Materials and methods
A structured systematic review was conducted, and multiple databases were searched using a combination of terms related to 3D printing in fracture management. The literature search was limited from inception to Nov 2020. Only comparative randomized studies were accepted for inclusion. Any software or material using 3D printing versus no technological assistance was included. All types of fracture treated by open reduction and internal fixation were included. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) methodology was applied with the Joanna Briggs Institute’s critical appraisal tool used to assess the quality of the included studies. Quantitative analysis was performed.
Results
Based on 13 RCTs including 673 patients (325 and 348 in the 3D and control groups, respectively), the weighted effect size outcomes were as follows: (a) operative duration − 1.47 (95% CI = − 1.759 to − 1.182), (b) intraoperative blood loss − 1.41 (95% CI = − 1.792 to − 1.029), (c) fluoroscopy use − 1.25 (95% CI = − 1.637 to − 0.867), in favor of the 3D group. The weighted Odds ratio outcomes were: (a) overall good or excellent result 2.05 (95% CI = 1.119 to 3.845) and (b) anatomic fracture reduction 2.64 (95% CI = 1.150 to 6.051) in favor of the 3D group. The mean residual displacement and time to union showed no significant difference. The mean JBI appraisal tool score for the randomized studies was of 9, out of a maximum of 13.
Conclusions
When compared to the non-use of 3D technology for open reduction and internal fixation of fractures, the review demonstrated evidence that 3D printing yielded significantly better perioperative results. Further studies are needed to evaluate the effect of 3D printing on union and long-term function.
Level of evidence
I.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Additive manufacturing, commonly known as three-dimensional or 3D printing, has been an ever-evolving field since 1981 when the first technique was developed at the Nagoya Municipal Industrial Research Institute involving ultraviolet-ray hardened polymers [1]. Over the years, this technique has been refined and 3D printing has become a staple in a multitude of fields including the automotive industry, construction, robotics, and medicine [2].
Over the past decade, computer-aided imaging software has allowed for 3D reconstruction of traditionally two-dimensional imaging studies. These virtual reconstructions have been beneficial for preoperative diagnosis and planning and have even been shown to improve postoperative results [2]. The promising outcomes using virtual reconstruction have encouraged further research into the possible benefits of printing 3D models, which allows for physical assessment of the intended anatomic area.
The imaging study of the desired anatomic area is first retrieved then converted from the traditional DICOM file-type into a one that can be rendered as a 3D object. The subsequent 3D file is then edited to exclude artifacts and unwanted structures, and prepared for the printing process [3].
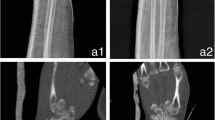
Surgeons, particularly orthopedists, are now capable of preparing anatomically accurate models to be used in pre-operative planning, as well as custom implants made to fit the patient’s particular anatomy [4,5,6]. This has highlighted the possibility of relying on realistic printed models for the visualization of orthopedic deformities and fractures. Three-dimensional printing provides a novel method to analyze orthopedic complaints by adding a textile element that classical imaging methods cannot. Utilizing this technique has helped in reducing operative complications, has increased the likelihood of a successful operative outcome [7, 8], and may have profound educational benefits for both patients and upcoming healthcare providers [9, 10]. Figures 1, 2, 3, 4, and 5 show the use of 3D printing models in a case of lateral plateau tibial fracture treated with plate and screws.
Despite its significant presence in the relevant literature and the promising results, the use of 3D printing in the pre-operative planning of orthopedic surgeries remains controversial enough to not be a part of the usual preoperative workup. The aim of this meta-analysis was to look for significant differences in outcomes such as intraoperative blood loss, fluoroscopy use, anatomic fracture reduction and time to union between 3D printing-assisted methods and non-assisted methods.
Methods
Search strategy
An electronic search strategy was planned using the following databases from inception to Nov 2020: PubMed, Embase, CINAHL, Cochrane Library and Google Scholar. A number of terms were used to locate a maximum number of relevant studies: fracture AND (3D OR 3-dimensional OR three-dimensional) AND (printing OR ‘’Virtual Windowing’’). No language or date limitations were imposed.
Criteria for study selection
Only comparative randomized studies were accepted for inclusion. Any software or material using 3D printing versus no technological assistance were included. All types of fracture treated by open reduction and internal fixation were included.
Screening and selection of literature
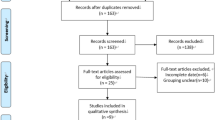
Initial hit records were screened based on titles and abstracts and duplicates were removed. The full manuscripts of potentially relevant papers were read and inclusion/exclusion criteria were applied. Reference lists were checked for additional relevant studies. Disagreement on eligibility was resolved by consensus.
Unit of analysis and types of outcome measures
The unit of analysis was defined as the fracture, not the patient. The primary outcome was set to be the operative duration. Secondary outcomes were defined as intraoperative blood loss, fluoroscopy use, overall excellent/good results, anatomic fracture reduction and time to union. Fracture reduction was evaluated subjectively by the surgeons.
Data collection
In preparing this review, the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) checklist was used for guidance [11].
Data extraction
An Excel sheet for data extraction was prepared to report all relevant details reported in the studies. data Data extraction was conducted by three authors followed by a joint review to produce agreed accurate data. Patient demographic data, fracture site, surgical approach, internal fixation type, follow-up duration and outcomes were recorded.
Quality assessment
The Joanna Briggs Institute (JBI) critical appraisal tool for randomized trials was used to detect potential sources of bias [12].
Data analysis
Statistical analysis was conducted using StatsDirect (Cambridge, UK). Weighted standard mean difference was used for continuous variables and proportion meta-analysis for categorical variables was such as the weighted frequencies. Heterogeneity was assessed by the inconsistency test (I2). The random-effect estimate was selected for reporting when the I2 value was more than 50%. The reported confidence interval (CI) values were the 95% CI.
Results
Search results
The search yielded 593 record hits and eight duplicates were removed. Title and abstract screening of the remaining 585 papers led to locating 24 studies with relevant potential for inclusion. The examination of the full-text manuscripts isolated 12 studies meeting inclusion criteria. The 12 excluded studies were either prospective not randomized or retrospective comparative. An additional study was found through checking of the reference lists. In total, 13 RCTs were included in the review (Fig. 3. PRISMA Flow Diagram).
Study characteristics results
The total pooled sample comprised 673 patients: 325 and 348 in the 3D and control groups, respectively. The mean age was 42.1 ± 8.7 years and 42.6 ± 8.4 years for the 3D and control groups, respectively. Gender distribution was as follows: 269 females and 404 males.
The mean follow-up period was 14 ± 5 months and 14.4 ± 5.1 months for the 3D and control groups, respectively. Table 1 summarizes the characteristics of the included studies.
Outcomes
Intraoperative outcomes
Operative duration
The weighted effect size was of − 1.47 (95% CI = − 1.759 to − 1.182, I2 = 60.4%, P < 0.0001), in favor of the 3D group.
Intraoperative blood loss
All studies but one [7] reported this outcome with a weighted difference of Shuang 1.41 (95% CI = Shuang 1.792 to Shuang 1.029, I2 = 77.7%, P < 0.0001), in favor of the 3D group.
Fluoroscopy use
Based on seven studies, the difference was Shuang 1.25 (95% CI = Shuang 1.637 to Shuang 0.867, I2 = 74.3%, P < 0.0001), in favor of the 3D group. Table 2 shows intra-operative outcomes of individual studies.
Postoperative outcomes
Rate of overall good or excellent result
Five studies reported functional outcomes with a weighted OR of 2.05 (95% CI = 1.119 to 3.845, I2 = 0%, P = 0.03) in favor of the 3D group.
Rate of anatomic fracture reduction
Four studies yielded a weighted OR of 2.64 (95% CI = 1.150 to 6.051, I2 = 0%, P = 0.03) in favor of the 3D group.
Mean residual displacement
Two studies reported this outcome. The mean displacement values of the 3D and control groups were 4.2 ± 0.7 mm and 5.8 ± 2.5 mm, respectively (P = 0.2).
Time to union
Based on three studies, the pooled difference was Shuang 0.008 (95% CI = Shuang 0.266 to 0.250, I2 = 33.6%, P = 0.9). Table 3 show postoperative outcomes of individual studies.
Quality score
The mean JBI appraisal tool score for the randomized studies was 9, out of a maximum of 13 (Table 4).
Discussion
Main findings
The results of this review demonstrated the superiority of using 3D printing models in treating orthopedic fractures and that for major outcomes. All three per-operative outcomes, operative duration, intraoperative blood loss and fluoroscopy use, were in favor of the 3D group. Additionally, the rates of excellent/good overall results and anatomic fracture reduction were significantly higher when compared to the control group.
Interpretation of the results
The use of 3D printing seems to be beneficial to the patients at many levels. Prolonged operative duration is associated with complications for any type of surgery irrespective of how an increase in operative time was defined [13]. In orthopedic surgery the same analysis demonstrated a statistically significant 67% increase in the likelihood of experiencing a complication with prolonged surgery duration. It is known that candidates for orthopedic surgery and in particular fracture surgery are often of senior age with associated co-morbidities and, therefore, more prone to complications [14, 15]. Additionally, when fixation needs plating, plate contouring could be carried out before tourniquet inflation, thus reducing operative time, and tourniquet time when it applies.
Some major orthopedic surgery procedures could result in a considerable intra-operative blood loss [16, 17]. An increase in the observed and hidden blood loss was significantly associated with medical complications following hip fracture surgery [18]. Orthopedic surgeons seem to underestimate the amount of blood loss occurring during surgery, and 80% of this loss may be unaccounted for by medical teams [19]. Blood loss during surgery could expose patients to postoperative anemia that might lead to a reduced functional recovery and a detrimental effect on long-term mortality [20]. Reducing intraoperative blood loss by using 3D printing technology could decrease postoperative anemia-related complications.
A lack of radiation safety guidelines in orthopedic surgery residency curricula has been recorded while in some institutions, surgeons and residents may not have access to radiation-dose-tracking equipment [21]. Only 65% of orthopedic surgeons reported attending or participating in a radiation safety course at some point during their training [22]. Radiation exposure has quantifiable and deleterious manifestations which occur with dose-dependent severity [23, 24]. To this, the significant difference in fluoroscopy use found in the 3D printing group would be of great benefit to all the medical staff present in the operating room and in particular to those close to the radiation beam.
The significant differences in favor of the 3D group with respect to the overall excellent/good results and anatomic fracture reduction rates are to be considered as added values to the 3D printing technique. For fractures in general and for articular fractures in particular, a better reduction of fracture site is linked with better outcomes. The printed models were shown to have the potential to optimize fracture site reduction with a potential of reducing long-term complications.
Based on two and three studies, respectively, residual displacement and time to union were not found to be different between groups. Further and big-sampled studies are warranted to better analyze these outcomes.
Limitations
Though the review included 13 randomized trials, many outcomes were not reported in all studies and for some of the results, the weighted estimates were based on fewer studies. Four studies have 15 participants or less in each arm group; however, the pooled sample of 673 patients could be considered as fair enough to look for significant differences in major outcomes. The inclusion of different fracture sites and consequently different approaches and fixation materials could be one of the major limitations of the study. On the other hand, the 3D software was almost the same but with different versions. We do not believe that the different printer types used to create the models could have impacted our results; nonetheless, materials that could be sterilized could offer more practicality during procedure. Another important limitation could be that functional results and rates of anatomic fracture reduction and residual displacement were reported in only some of the included studies; thus, the interpretation of those outcomes should be pondered. Blinding of assessment was reported in only one study and such could have introduced some bias to the results.
Conclusions
This technological marvel permits an in-depth analysis of the fracture and consequently planning surgical approach and adjusting fixation methods ahead of the surgery. When compared to the non-use of 3D technology for open reduction and internal fixation of fractures, the review demonstrated that 3D printing models yielded significantly better outcomes with respect to operative duration, blood loss, radiation exposure, anatomic fracture reduction rate and overall results rate. More studies are needed to explore other outcomes such as residual fracture displacement, time to union and long-term complications. In sum, our results should incite surgeons to use 3D models when treating fractures by open reduction and internal fixation, particularly those with high comminution or when the bone/joint anatomy is complex.
References
Kodama H. Automatic method for fabricating a three-dimensional plastic model with photo-hardening polymer. Rev Sci Instrum. 1981;52(11):1770–3.
Wake N, Rosenkrantz AB, Huang R, Park KU, Wysock JS, Taneja SS, et al. Patient-specific 3D printed and augmented reality kidney and prostate cancer models: impact on patient education. 3D Print Med. 2019;5(1):4–3.
Mitsouras D, Liacouras P, Imanzadeh A, Giannopoulos AA, Cai T, Kumamaru KK, George E, Wake N, Caterson EJ, Pomahac B, Ho VB, Grant GT, Rybicki FJ. Medical 3D printing for the radiologist. Radiographics. 2015;35(7):1965–88.
Azuma M, Yanagawa T, Ishibashi-Kanno N, Uchida F, Ito T, Yamagata K, et al. Mandibular reconstruction using plates prebent to fit rapid prototyping 3-dimensional printing models ameliorates contour deformity. Head Face Med. 2014;10:45.
Jeong HS, Park KJ, Kil KM, Chong S, Eun HJ, Lee TS, et al. Minimally invasive plate osteosynthesis using 3D printing for shaft fractures of clavicles: technical note. Arch Orthop Trauma Surg. 2014;134(11):1551–5.
Li C, Yang M, Xie Y, Chen Z, Wang C, Bai Y, et al. Application of the polystyrene model made by 3-D printing rapid prototyping technology for operation planning in revision lumbar discectomy. J Orthop Sci. 2015;20(3):475–80.
Shuang F, Hu W, Shao Y, Li H, Zou H. Treatment of intercondylar humeral fractures with 3D-printed osteosynthesis plates. Medicine (Baltimore). 2016;95(3): e2461.
Wan L, Zhang X, Zhang S, Li K, Cao P, Li J, et al. Clinical feasibility and application value of computer virtual reduction combined with 3D printing technique in complex acetabular fractures. Exp Ther Med. 2019;17(5):3630–6.
Bizzotto N, Sandri A, Regis D, Romani D, Tami I, Magnan B. Three-dimensional printing of bone fractures: a new tangible realistic way for preoperative planning and education. Surg Innov. 2015;22(5):548–51.
Esses SJ, Berman P, Bloom AI, Sosna J. Clinical applications of physical 3D models derived from MDCT data and created by rapid prototyping. AJR Am J Roentgenol. 2011;196(6):683.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7): e1000097.
Munn Z, Barker TH, Moola S, Tufanaru C, Stern C, McArthur A, et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synth. 2020;18(10):2127–33.
Cheng H, Clymer JW, Po-Han Chen B, Sadeghirad B, Ferko NC, Cameron CG, et al. Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res. 2018;229:134–44.
Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331(7529):1374.
Choi JY, Cho KJ, Kim SW, Yoon SJ, Kang MG, Kim KI, et al. Prediction of mortality and postoperative complications using the hip-multidimensional frailty score in elderly patients with hip fracture. Sci Rep. 2017;7:42966.
Millett PJ, Porramatikul M, Chen N, Zurakowski D, Warner JJ. Analysis of transfusion predictors in shoulder arthroplasty. J Bone Jt Surg Am. 2006;88(6):1223–30.
Salido JA, Marin LA, Gomez LA, Zorrilla P, Martinez C. Preoperative hemoglobin levels and the need for transfusion after prosthetic hip and knee surgery: analysis of predictive factors. J Bone Jt Surg Am. 2002;84(2):216–20.
Foss NB, Kehlet H. Hidden blood loss after surgery for hip fracture. J Bone Jt Surg Br. 2006;88(8):1053–9.
Zhu XZ, Tao YL, Ma Z. Routine blood tests as predictors of mortality in hip fracture patients. Injury. 2013;44(11):1659.
Lawrence VA, Silverstein JH, Cornell JE, Pederson T, Noveck H, Carson JL. Higher Hb level is associated with better early functional recovery after hip fracture repair. Transfusion. 2003;43(12):1717–22.
Kaplan DJ, Patel JN, Liporace FA, Yoon RS. Intraoperative radiation safety in orthopaedics: a review of the ALARA (As low as reasonably achievable) principle. Patient Saf Surg. 2016;10:27,8. eCollection 2016.
Nugent M, Carmody O, Dudeney S. Radiation safety knowledge and practices among Irish orthopaedic trainees. Ir J Med Sci. 2015;184(2):369–73.
Hamada N, Fujimichi Y. Classification of radiation effects for dose limitation purposes: history, current situation and future prospects. J Radiat Res. 2014;55(4):629–40.
Lopez M, Martin M. Medical management of the acute radiation syndrome. Rep Pract Oncol Radiother. 2011;16(4):138–46.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Ethics approval
This research does not require an institutional review board approval.
Rights and permissions
About this article
Cite this article
Yammine, K., Karbala, J., Maalouf, A. et al. Clinical outcomes of the use of 3D printing models in fracture management: a meta-analysis of randomized studies. Eur J Trauma Emerg Surg 48, 3479–3491 (2022). https://doi.org/10.1007/s00068-021-01758-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-021-01758-1