Abstract
Background
The effects of immediate operation on hip fracture (HF) are unclear. Therefore, we investigated the influence of time to operation within 12 h vs. > 12–24 h on survival and adverse events.
Methods
This retrospective study was based on our database from 2006 to 2019. Patients ≥ 20 years of age with operations for HF were included. A total of 40 characteristics were analyzed for operations within 12 h (group 1) and > 12–24 h (group 2) after admission. The primary endpoint was survival at 1 year after operation. Secondary endpoints were revision surgery for any reason, infection, and serious adverse events.
Results
A total of 1015 patients received operations within 12 h (group 1), and 985 patients received operations > 12–24 h (group 2) after admission. The mean age of the patients was 78.8 ± 12.3 years. Patients in group 1 were younger and had better health status and shorter hospitalizations than those in group 2. However, no differences were found for revision surgery, infection or adverse events. The mortality rates at 30 days, 90 days, 6 months, and 1 year were 6.2, 11.8, 15.9, and 21.0%, respectively. The mortality rate at day 30 was significantly better (p = 0.04) in group 1, but no further differences in survival were observed (hazard ratio 1.071; 95% confidence interval 0.864–1.328; log rank 0.179). A subgroup analysis of geriatric patients ≥ 65 years assessed no differences according the primary and secondary endpoints.
Conclusions
Within the limits of single-center analysis, the patients receiving treatment for HF within 12 h were younger and healthier and had the benefits of shorter hospitalizations and a higher 30-day survival rate than patients treated > 12–24 h after admission. At the endpoint 1 year after operation, no differences were observed in adverse events or survival rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The best time to treat HF has not been defined or evaluated, but the general consensus is that these operations should be performed as soon as possible. Some national guidelines recommend operations within 24 h, and others recommend operations within 48 h after admission [1,2,3]. However, treatment starting later than 48 h after admission should generally be avoided, because of the significantly higher morbidity and mortality rates [4, 5]. Most recommendations are based on registry data with large numbers of patients, but some of the associated outcomes have been limited to the time of hospitalization or 30 days after operation [6, 7].
Few studies have evaluated the outcomes of operations performed within 12 h after admission. In 1967, Alderete et al. compared treatment performed within 12 h vs. 13–48 h after admission [8]. The authors found no differences in mortality. However, these results can be considered outdated.
Recent data from the Norwegian Registry for HF also indicated no differences when patients were treated within 12 h after admission to the hospital [4]. The registry included 83,727 HF; however, only 53% of the fractures were assessed, owing to incomplete data transfer [4].
In contrast, Bretherton and Parker have reported a significantly lower 30-day mortality rate in patients treated within 12 h after admission, but the study has some limitations [9]: only 6.6% of the patients received treatment within 12 h, and the data analyzed go back until 1989. Moreover, procedures, complications, or 1-year survival rates were not reported.
The aim of this retrospective single-center study was to address an important knowledge gap regarding the comparison between operation within 12 h vs. > 12–24 h in terms of 1 year survival and adverse events. The null hypothesis was no difference between groups.
Methods
The study was conducted in our level-1 trauma hospital as an observational study according to the principles of the Declaration of Helsinki. Ethical approval was obtained from institutional review board of our hospital prior to conducting this study; and oral informed consent was obtained from all participants or their next of kin.
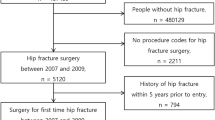
The initial informations according to the patients were obtained from our hospital database with all operations conducted for HF starting in 2006 (Fig. 1). For each patient, information on perioperative characteristics was recorded from the time of registration in the emergency department to the time of operation (skin incision), in minutes. In cases of fall in our hospital, the time started when X-ray report was obtained.
In this study, the inclusion criteria were patients with a HF according to AO/OTA classification 31-A and 31-B, including subtrochanteric fractures, standard treatment with osteosynthesis or a hip replacement within 24 h after index admission, and a treatment period between January 1, 2006 and December 31, 2019. An additional inclusion criterion was patients at least 20 years of age.
The primary exclusion criterion was treatment starting later than 24 h after admission (n = 1315). The further rigorous exclusion criteria are shown in Fig. 1. Any patients not admitted directly to the clinic after the injury or with a delay in admission (e.g., secondary transfer from other hospitals or from abroad) were also excluded. Therefore, the study sample included only patients with an injury and immediate admission to our emergency department. Patients with an operation for a contralateral hip fracture during the study period were recorded only as having contralateral fractures (n = 78); thus, the number of patients was the same as the number of operations.
The demographic variables were age, sex, affected side, and body mass index (BMI; weight in kilograms divided by height in meters, squared). Baseline blood tests at the time of admission were hemoglobin in mg/dl, creatinine in mg/dl and C-reactive protein in mg/dl.
Coexisting conditions were summarized according to the American Society of Anesthesiology (ASA) [10]. Reported illnesses included atrial hypertension, dementia, heart disease or coronary artery disease, diabetes mellitus, atrial fibrillation, chronic renal diseases (creatinine ≥ 3.0 mg/dl), chronic obstructive pulmonary disease (COPD), alcoholism or a history of cancer (Table 1). Recorded drug treatments included anticoagulant medications [phenprocoumon or new direct oral anticoagulants (NOACs)] and insulin.
The following variables were recorded until discharge: type of fracture according to AO/OTA classification [11], type of operation (osteosynthesis vs. replacement with hemi- or total hip arthroplasty), duration of operation from incision to suture in minutes, red blood cell transfusion in units and duration of hospitalization in days (including the day of admission and the day of discharge).
The data cutoff for the primary and secondary analysis was 1 year after operation. The primary endpoint was death. Secondary endpoints were any revision to the index operation, including operation for infection, hematoma, implant failure or reduction for dislocation; and the following serious adverse events at hospitalization: heart failure, stroke, pneumonia, pulmonary thromboembolic events, delirium or deep vein thrombosis.
Infection was defined according to the working group of the Musculoskeletal Infection Society [12].
Patients or their relatives were contacted by telephone to collect missing data, particularly for death or survival outcomes, or possible reoperations conducted outside our system.
Statistical analyses
Kolmogorov–Smirnov tests were used to determine the distribution of the variables. No variables in this study demonstrated normal distribution. Mann–Whitney U tests were used to compare two independent samples, and Fisher’s exact tests were used for unadjusted comparison of proportions, whereas Pearson’s chi-squared tests were used for unadjusted comparison of ordinal distributions. Data are presented as mean values with standard deviations or as percentages. Kaplan–Meier survival analyses were used to determine the association between mortality and the time to operation. Log-rank tests were used to compare survival probabilities. All statistical tests were two-sided, and p values less than 0.05 were considered to indicate statistical significance. SPSS software for Windows, version 24.0 (SPSS, Chicago, Illinois), was used for all analyses. The statistical analysis was performed by a professional statistician.
Results
Patients
From January 1, 2006, to December 31, 2019, a total of 3543 surgeries for hip fractures were performed; among these cases, 2000 patients were enrolled according to our rigorous inclusion and exclusion criteria (Fig. 1). Of the enrolled patients, 1015 were treated within 12 h (group 1), and 985 patients were treated > 12–24 h (group 2) after admission. The mean age of the patients was 78.8 ± 12.3 years, and 71.3% of the patients were women.
Group 1 had younger average age (p < 0.001) and better health status according to, e.g., ASA classification, dementia, hypertension or atrial fibrillation (Table 1). The further baseline and clinical characteristics of the study patients are listed in Table 1. Given their younger age, the patients in group 1 received total hip arthroplasty more often than patients in group 2 (p < 0.001), and the latter received hemiarthroplasty more often (p = 0.002). With the exception of subtrochanteric fractures, fracture patterns according to AO classification were similar between treatment groups.
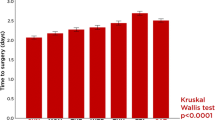
Primary endpoint
In the sample, the mortality rates at 30 days, 90 days, 6 months, and 1 year were 6.2%, 11.8%, 15.9%, and 21.0%, respectively. The 30-day mortality rate was significantly better (log rank 0.033) in group 1, but no differences were observed at later time points or at 1 year (hazard ratio = 1.071; 95% confidence interval = 0.864–1.328; log rank = 0.179). Therefore, with the exception of day 30, the primary endpoint results did not differ between groups (Table 2, Fig. 2).
We conducted a subgroup analysis (Table 3): the analysis of geriatric patients` ≥ 65 years of age (n = 1733) treated within 12 h (n = 830) vs. > 12–24 h (n = 903) showed no significant differences according to the primary endpoints of this study (Table 4, Fig. 3).
Secondary endpoint
The total revision rate was 10.4% at 1 year after operation. Revision for any reason and according to the index operation showed no differences between groups (9.9 vs. 11.0%; p = 0.421). An analysis for infection yielded insignificant results, and the occurrence of serious adverse events was also similar between groups. Therefore, the secondary endpoints of the study showed no differences between groups of the total sample size (Table 2) and the groups of the geriatric patients (Table 4).
Discussion
In this study, operation of HF within 12 h after admission was not found to be superior to operation > 12–24 h after admission in terms of survival and adverse events, with an endpoint 1 year after operation. Therefore, the null-hypothesis was confirmed. The only effect was shorter hospitalization and a lower mortality rate at day 30 in the group receiving operation within 12 h; however, this result should be considered in the context of the better health status, younger patient age and fewer comorbidities in that group. A subgroup analysis with geriatric patients revealed also insignificant effects.
Our study has several strengths. First, the patients were separated into two groups according to the accurate evaluation of time to operation in minutes, from the time of admission to the time of skin incision. The large sample size enabled robust statistical analysis, and most demographic and clinical characteristics were well documented and valid. The sample showed typical clinical characteristics and included patients with cognitive impairment. We also defined strong inclusion criteria, and 150 patients were consequently excluded secondarily (Fig. 1). The endpoint of 1 year for every living patient showed comparable outcomes. According to the primary and secondary endpoints, the follow-up rate was nearly 100%, only two patients were lost to follow-up. In addition, beyond the use of registry data, this study examined the second highest number of patients (n = 2000) treated for HF within 12 h vs. > 12–24 h reported in the literature, and it is, the largest study with detailed clinical information and with an endpoint 1 year after operation.
The time to operation is a major consideration in the treatment of HF. In 1967, Aldrete et al. reported that the optimal time of operation is of particular concern [8]. In that study, the mortality rates of patients treated for HF showed insignificant differences when the operation started within 12 h or 13–48 h after admission, but these data are now outdated.
Given the constantly rising number of geriatric patients with HF [13], health insurance companies aim to decrease health care costs. Therefore, some studies have been conducted or supported by health insurance companies, and those results should be discussed in that context. For example, Müller-Mai et al. [14] reported a higher revision rate and a higher mortality rate (plus 6%), when the patients were treated later than 24 h after admission. However, the health insurance data were based only on International Classification of Diseases (ICD) codes, and the time to operation was assessed in full days rather than the exact time intervals, e.g., the numbers of hours or minutes from admission to skin incision.
In 1992, Bredahl et al. retrospectively assessed the mortality rate among 778 patients with HF [15]. The mortality rate was 10.1% at 1 month and 30.3% at 1 year after operation. Despite similar baseline data (e.g., patient age), the mortality rates observed at day 30 and 1 year in our study were considerably lower. Moreover, the authors found a significantly lower mortality rate only in patients with femoral neck fractures who were treated within 12 h; and in patients with trochanteric fractures, the mortality rate was unaffected by the time to operation. Interestingly, 88% of the patients received internal fixation, and only 8% of the patients received hip arthroplasty [15]. Therefore, the type of treatment was substantially different from that in the current study.
Our findings are consistent with those from similar studies comparing patients treated within 12 h vs. later, including a recently published registry from Norway [4]. That national observational study included 73.557 patients treated for HF. Analyses were conducted to evaluate the total delay from fracture to surgery and the delay from admission to surgery to analyze complications and mortality. The study found that only a delay later than 48 h was associated with a higher mortality rate. The authors stressed that the mean prehospital delay was 6 h. According to the records and our local city factors, our patients were admitted within 1 or 2 h after injury, and any further delays, e.g., transfers from other hospitals or from abroad were rigorously excluded. Of note, the Norway registry showed more patients with ASA classifications 1 and 2 in the earlier treatment group—a similar finding to our results.
A recent study has reported on “fast track” treatment [7], in which patients receive a faster “first line treatment” to reduce the time to operation. The authors concluded that “fast track” treatment is safe, but the 30-day, 90-day, and 1 year mortality, or revision for any reason are comparable to those with standard treatment. Interestingly, the mean time to surgery in the “fast track” group was 23.6 h and was 25.7 h in the standard treatment group. Notably, these data were from the aforementioned Norwegian Hip Fracture Registry. Our mean “fast track” time from admission to operation was approximately 7 h and, therefore, was substantially faster.
A retrospective cohort study from Ontario, Canada, with 72 participating hospitals and more than 40,000 patients has reported that a time of operation later than 24 h is associated with a greater risk of 30-day mortality and other complications [6]. However, in this study, only 34% of the patients received operation within 24 h [6]; therefore, a very selection bias must be suspected toward much more healthy patients in this group. Apart from the high number of patients and the 30 assessed variables, a major strength of this study is that the time to operation was collected exactly in hours. Interestingly, approximately half the patients (48%) were treated with sliding hip screws or cannulated screws, and only approximately 16% were treated with intramedullary nails. Of note, our treatment was not consistent with the treatment in this cohort study. Again, the main focus of this study was not the time to operation within 12 h [6].
In 2015, Bretherton and Parker published a single-center study with 6.638 patients treated for HF [9]. The time to operation was recorded and divided into seven subgroups, from 0 to 6, 7–12, 13–18, 19–24 h, and later. The primary endpoint was 30-day mortality. Significantly improved survival was assessed for only the patients treated within 12 h vs. later times (p value 0.013), but not for treatment within or after 24 h. A limitation of that study was its long observation period starting in 1989; therefore, the treatments and devices used can be considered outdated.
Of note, Dorotka et al. have compared 182 patients treated for HF either within or later than 6 h, up to 7 days after admission [16]. This may be the first study examining outcomes of operation within 6 h. After 6 months, the mortality rate was significantly lower in the group receiving earlier treatment (10.1% vs. 21.4%). However, this result became insignificant when patients (n = 14) treated after 36 h were excluded. The authors note that the later the operation was performed, the higher the mortality was; however, the power of the results was low, as a result of the small sample size. From our point of view, performing operations for HF routinely within 6 h after admission is far from the reality.
Some additional studies have assessed time to operation within 12 h in small sample sizes [17,18,19]; and others did not separate the interval below 24 h [20, 21]. Of note, most studies have calculated the time to operation only in days after admission [22, 23], and these data are also particularly outdated.
In summary, on the basis of our results, the benefits of operation within 12 h were a lower mortality rate at day 30 and a shorter hospitalization. A subgroup analysis with geriatric patients ≥ 65 years of age showed that the 30-day mortality rates were similar. The median hospitalization in our study was 12.0 days, and we observed a significant reduction of exactly 1 day in group 1 compared with group 2. In a study conducted by Siegmeth et al., the difference in hospitalization was less than 1 day (mean 22.2 vs. 21.6 days), and the result was not significant within the same time frames [18]. Again, our data suggest that both effects were based on the bias toward younger and healthier patients in the group receiving earlier treatment. Therefore, the effects were not attributable to a faster time to operation.
The current study has several limitations, as follows. Our findings cannot be generalized because this was only a retrospective single-center study. Another limitation is that the two groups were balanced according to the number of patients but not according to some characteristics. The true reasons for treating patients within < 12 or ≥ 12–24 h, e.g., admission late at the night, waiting for informed consent, or waiting for an operating room could not be evaluated retrospectively; however, the reason for delayed admission was never associated with unavailability of surgeons. Despite the higher number of study patients, a total of 1315 patients (37%) were treated later than 24 h after admission within the study period. Furthermore, the time from injury to admission could not be assessed exactly; however, and according to protocols, most patients are admitted to the hospital within 1 or 2 h. The study included only 1 year follow-up data and thus underrepresents long-term complications, e.g., late infection or periprosthetic fractures; ongoing follow-up provide information on longer-term outcomes. Patient-reported outcome measures were not assessed at the time of follow-up. Against the background of many patients with comorbidities, e.g., dementia, any outcome measures would reflect particularly healthy patients, and this was not the intention of the study.
Finally, we note that Bretherton et al. [9] and Siegmeth et al. [18] collected data from the same hospital; Pincus et al. [6] and Weller et al. [19] presented results from the same database from Ontario, Canada; and Leer-Salvensen et al. [4] and Pollmann et al. [7] assessed data from the Norwegian Hip Fracture Registry.
Conclusion
Within the limits of single-center analysis, we found that patients receiving treatment for hip fractures within 12 h were younger and healthier and had the benefit of shorter hospitalizations and a higher 30-day survival rate than those for patients treated > 12–24 h after admission. At the endpoint 1 year after operation, no differences were observed in adverse events or survival rates for the total sample size and for the geriatric patients.
References
No authors listed. Hip fractures in adults. Timing of surgery. National Institute for Health and Care Excellence (NICE). Last updated May 2017. www.nice.org.uk.
No authors listed. Canadian Institute for Health Information. Wait times for priority procedures in Canada. Last updated March 2020. www.waittimes.chih.ca.
Bonnaire F, Weber A. Hip fractures in adults. S2 Guideline. German Society for Trauma Surgery e.V. (DGU). Last updated October 2015. www.awmf.org.
Leer-Salvesen S, Engesæter LB, Dybvik E, Furnes O, Kristensen TB, Gjertsen JE. Does time from fracture to surgery affect mortality and intraoperative medical complications for hip fracture patients? An observational study of 73557 patients reported to the Norwegian Hip Fracture register. Bone Joint J. 2019;101:1129–37. https://doi.org/10.1302/0301-620X.101B9.BJJ-2019-0295.R1.
Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55:146–54. https://doi.org/10.1007/BF03016088.
Pincus D, Ravi B, Wasserstein D, Huang A, Paterson JN, Nathens AB, Kreder HJ, Jenkinson RJ, Wodchis WP. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA. 2017;318:1994–2003. https://doi.org/10.1001/jama.2017.17606.
Pollmann CT, Røtterud JH, Gjertsen JE, Dahl FA, Lenvik O, Årøen A. Fast track hip fracture care and mortality—an observational study of 2230 patients. BMC. 2019;20:248. https://doi.org/10.1186/s12891-019-2637-6.
Aldrete JA, Hamilton SD, Hingson RA. Anesthesia factors in the surgical management of hip fractures. J Trauma. 1976;7:818–26. https://doi.org/10.1097/00005373-196711000-00003.
Bretherton CP, Parker MJ. Early surgery for patients with a fracture of the hip decrease 30-day mortality. Bone Joint J. 2015;97:104–8. https://doi.org/10.1302/0301/620X.97B1.35041.
American Society of Anesthesiologists. New classification of physical status. Anesthesiology. 1963;24:111–4.
Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audigé L. Fracture and dislocation classification compendium—2007: orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(Suppl 10):S1–133. https://doi.org/10.1097/00005131-200711101-00001.
Workgroup Convened by the Musculoskeletal Infection Society. New definition for periprosthetic joint infection. J Arthroplasty. 2011;2011(26):1136–8. https://doi.org/10.1016/j.arth.2011.09.026.
No authors listed. Center for Disease Control and Prevention. Hip fractures among older adults. Last updated September 2016. www.cdc.gov.
Müller-Mai CM, Schulze Raestrup US, Kostuj T, Dahlhoff G, Günster C, Smektala R. One-year outcomes for proximal femoral fractures: posthospital analysis of mortality and care levels based on health insurance data. Unfallchirurg. 2015;118:780–94. https://doi.org/10.1007/s00113-013-2534-7.
Bredahl C, Nyholm B, Hindsholm KB, Mortensen JS, Olesen AS. Mortality after hip fracture: results of operation within 12 h of admission. Injury. 1992;23:83–6. https://doi.org/10.1016/0020-1383(92)90037-s.
Dorotka R, Schoechtner H, Buchinger W. The influence of immediate surgical treatment of proximal femoral fractures on mortality and quality of life. Operation within six hours of the fracture versus later than six hours. J Bone Joint Surg Br. 2003;85:1107–13. https://doi.org/10.1302/0302/0301-620x.85b8.14282.
Uzoigwe CE, Burnand HG, Cheesman CL, Aghedo DO, Faizi M, Middleton RG. Early and ultra-early surgery in hip fracture patients improves survival. Injury. 2013;44:726–9. https://doi.org/10.1016/j.injury.2012.08.025.
Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87:1123–6. https://doi.org/10.1302/0301-620X.87B8.16357.
Hongisto MT, Nuotio MS, Luukkaala T, Väistö O, Pihlajamäki HK. Delay to surgery of less than 12 hours is associated with improved short- and long-term survival in moderate- to high-risk hip fracture patients. Geriatr Orthop Surg Rehabil. 2019. https://doi.org/10.1177/2151459319853142.
Weller I, Wai EK, Jaglal S, Kreder HJ. The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br. 2005;87:361–6. https://doi.org/10.1302/0301-620x.87b3.15300.
Orosz GM, Magaziner J, Hannan EL, Morrison RS, Koval K, Gilbert M, McLaughlin M, Halm EA, Wang JJ, Litke A, Silberzweig SB, Siu AL. Association of timing of surgery for hip fracture and patient outcome. JAMA. 2004;291:1738–43. https://doi.org/10.1001/jama.291.14.1738.
Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important. J Bone Joint Surg Am. 2005;87:483–9. https://doi.org/10.2106/JBJS.D.01796.
Verbeek DOF, Ponsen KJ, Goslings JC, Heetveld MJ. Effect of surgical delay on outcome in hip fracture patients: a retrospective multivariate analysis of 192 patients. Int Orthop. 2008;32:13–8. https://doi.org/10.1007/s00264-006-0290-9.
Funding
The research did not receive any specific Grant from funding agencies in the public, commercial or no-profit sectors.
Author information
Authors and Affiliations
Contributions
We would like to thank Dr. med. Tanja Kottmann, Medical Statistics, Beverstr. 64, 59,077 Hamm, Germany, for doing the statistical analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approval was obtained by the institutional review board.
Consent to participate
All patients or their next relatives gave consent to participate in this study.
Rights and permissions
About this article
Cite this article
Müller, F., Proske, A., Eckstein, C. et al. Two-thousand hip fractures treated within 12 h and > 12–24 h after admission: Are survival and adverse events affected?. Eur J Trauma Emerg Surg 48, 1817–1825 (2022). https://doi.org/10.1007/s00068-021-01697-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-021-01697-x