Abstract
Background
Anterior shoulder dislocations are the most common type of joint dislocation with the majority treated with closed reduction. Reduction methods can be grouped into their principle mode of action: traction–countertraction, leverage and scapular manipulation. The best method has yet to be identified and our aim was to find the most effective, safe and least painful method of closed reduction for acute anterior shoulder dislocations.
Methods
A search of the online databases of CENTRAL, MEDLINE and Embase was performed to identify randomised control trials (RCTs) comparing closed reduction methods for anterior shoulder dislocations. A systematic review and meta-analysis were performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Results
Twelve eligible RCTs were included with a total of 1055 patients. Our meta-analysis showed traction–countertraction methods are marginally less painful than leverage methods by 0.86 points on the VAS scale but leverage methods are quicker by 20 s. Amongst traction–countertraction methods, the Spaso technique was the least painful and quickest, albeit with no difference in overall success rate. A meta-analysis was not possible for comparisons involving scapular manipulation due to the paucity of studies, but within two studies, scapular manipulation was significantly less painful than both leverage and traction–countertraction methods by 1.5 and 2.3 points (VAS), respectively.
Conclusion
Traction–countertraction methods are less painful but slower than leverage methods with no difference in complication rates. However, there was no difference in overall reduction success rate between any of the groups.
Level of evidence
I.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The glenohumeral joint of the shoulder is the most commonly dislocated joint with a reported incidence between 8.2 and 23.9 per 100,000 persons per year [1,2,3,4]. Anterior dislocations comprise up to 98% of all shoulder dislocations [5,6,7]. Anterior shoulder dislocations occur at the highest rates in young males involved in sporting activities followed by a second incidence peak in older females after low energy falls [8].
Acute anterior shoulder dislocation is most commonly treated with early, closed reduction to restore glenohumeral joint congruity and allow a pain-free functional range of movement. Many thousands of reduction techniques have been described, dating as far back as 3200 years [9]. They can be classified in three categories according to their principle mode of action.
Traction-counter traction techniques, such as the traditional Hippocratic [10] and Stimson [11], apply longitudinal force to the humerus to overcome muscular spasm and allow humeral head relocation. Other, less traditional, traction–countertraction methods include the Spaso [12], FARES (Fast, Reliable and Safe) [13] and Boss–Halzach–Matter [14] methods. The patient is supine in the Spaso method, with longitudinal traction applied the arm forward flexed at 90º followed by external rotation [12]. In the FARES [13] method, the clinician holds the patient’s wrist and slowly abducts the arm whilst applying longitudinal traction and oscillating up and down. The arm is then externally rotated once the abducted past 90º. The Boss–Halzach–Matter [14] is a self-reduction method in which the patient sits up and locks their hands around a flexed knee on the same side as the dislocated shoulder. They are then asked to lean back whilst hyperextending their neck, thereby using their own body weight to reduce the dislocation.
Leverage techniques, typified by the Kocher [15] and Milch [16] use a combination of traction and rotation to manipulate the humeral head back into the glenoid fossa. The Eachempati [17] method, alternatively named the external rotation method, is similar to the Kocher technique and essentially involves externally rotating the arm in a supine patient with elbow flexed to 90º and shoulder forward flexed to 20º to relax the anterior capsule.
Scapular manipulation techniques [18] are a newer group of techniques which aim to manipulate the glenoid fossa into a position that allows the humeral head to fall back into place. There are various different variations but in general they involve putting the patient prone and applying downward traction to the arm which is flexed to 90º followed by pushing the tip of the scapula medially and upward.
The choice of reduction technique is based on clinician experience and training. It is vital that the reduction technique used relocates the humeral head efficiently whilst minimising pain and complications. Our aim in this study is to summarise the evidence from randomised controlled trials that compare different techniques of closed reduction of acute anterior shoulder dislocation to determine the most effective and least painful technique.
Materials and methods
Search strategy
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register, the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and Embase up to 31st March 2019. We also searched the World Health Organization International Clinical Trials Registry platform, ClinicalTrials.gov and Current Controlled Trials and the conference proceedings of the British Elbow and Shoulder Society, The Bone and Joint Journal, American Orthopaedic Trauma Association and American Shoulder and Elbow Society to identify ongoing, recently completed and completed but unpublished trials. We did not apply any restrictions based on language or publication status. Non-English papers were translated by professional translators.
Search strategies for MEDLINE, CENTRAL and Embase can be found in online Appendix 1.
Study selection
Two review authors (HD and EJ) independently screened search results by title and abstract to identify randomised and quasi-randomised controlled trials evaluating closed reduction methods for acute anterior shoulder dislocation. The full text of the selected articles was obtained. The two review authors (HD and EJ) assessed the full text articles to ensure that they met the inclusion criteria. In the event of uncertainty, a third review author (KT) was consulted. The criteria for study selection are shown in Table 1. The selection of included studies is shown in Table 2. All included trials not originally published in English were translated.
Data collection
We designed a data collection proforma to extract the following data from the included trials: (1) author; (2) publication date (3) study type (4) study population (5) interventions (6) primary outcomes (reduction success, pain and complications) (7) secondary outcomes (reduction failure, duration of reduction procedure, number of attempts at reduction, recurrence of dislocation, long term shoulder outcomes, patient satisfaction). The data collection proforma was modified after trialling it on three studies and outcomes modified. Reduction success was initially defined as success after up to two attempts and reduction failure was used to capture studies that used other definitions of reduction success. We noticed that many of the studies measured reduction success after one attempt and therefore we changed our reduction success outcome to include both reduction success after one attempt and after up to two attempts without a change in reduction technique. Reduction failure was then defined as failure requiring reduction in theatre under general anaesthetic. This allowed comparison of all studies regardless of which reduction success measure they used. Two review authors (HD and EJ) independently collected all data. Study authors were contacted to obtain missing data or when clarification of methodology was required.
Study quality assessment
Two study authors (HD and EJ) assessed the risk of bias and appropriateness of study design using the Cochrane risk of bias tool [19]. The assessment judges seven domains as high, low or unclear risk of bias. In the event of disagreement, the third study author (KT) was consulted and a consensus decision made.
Comparisons between interventions
We planned the following comparisons based on principle modes of action:
-
1.
Leverage vs traction–countertraction
-
2.
Scapular manipulation vs traction–countertraction
-
3.
Scapular manipulation vs leverage
However, a significant proportion of studies compared two methods of reduction with the same principle mode of action, e.g., leverage vs leverage. These studies could not be incorporated into the above three comparisons for meta-analysis. Therefore, to utilise the data from these studies, two further comparisons were analysed within the traction–countertraction and leverage groups:
-
4.
Spaso vs other traction–countertraction methods
-
5.
Milch vs other leverage methods
The reason that these two comparisons were chosen is that the majority of studies are in the traction–countertraction and leverage groups, with only two papers looking at scapular manipulation. Within these two groups, Spaso was the mostly commonly used traction–countertraction method and Milch was the most commonly used leverage method.
Statistical analysis
We calculated risk ratios (RR) with 95% confidence intervals (CI) for dichotomous outcomes (such as reduction failure) using the Mantel–Haenszel method and mean differences with 95% CIs for continuous outcomes (such as duration of reduction) using the inverse variance method.
Heterogeneity was assessed by visual inspection of forest plots and calculation of I2 statistic. We judged there to be “considerable” heterogeneity if I2 ≥ 75% [19]. When pooling data, the choice of whether to use fixed or random effects models was based on a careful consideration of heterogeneity, number of studies and size of studies. The level of statistical significance was set at p < 0.05. As there were fewer than ten studies in each comparison a funnel plot was not used to evaluate for publication bias [19]. All statistical analyses were performed using Revman Review Manager [20].
Results
Search results
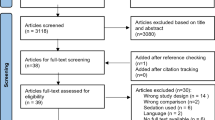
We screened a total of 644 records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (12 records); CENTRAL (242), MEDLINE (221), Embase (318). We also identified 15 potentially eligible studies from other sources: WHO International Clinical Trials Registry Platform (n = 8) and BJJ Proceedings (n = 7). No restrictions were placed on language.
The search identified a total of 19 articles for potential inclusion, for which full reports were obtained where possible. Upon study selection, 12 were included, 7 were excluded. Two of these studies were not published in English [21], so full translations were obtained for them. One trial [22] was never published and therefore unpublished data were sought from the authors and included in the meta-analysis.
A PRISM [23] flow chart summarising the study selection process is shown in Fig. 1.
Study characteristics
We included 12 studies with a total of 1055 patients randomised. No trials specified any source of funding or declared any conflicts of interest. Table 2 shows some of the key characteristics of the studies and the outcomes relevant to our meta-analysis.
Reduction methods included: Spaso [12, 22, 24], traction–countertraction [14, 24, 25], Stimson [26], Milch [26,27,28], Kocher [12, 13, 18, 27], FARES [13, 22, 29], Eachempati [29], Boss-Halzach-Matter (BHM) [14], Hippocratic [13, 21], Scapular manipulation [18], Modified scapular manipulation [25], “external rotation” method [28] and “manipulative reduction” [21]. For the meta-analysis, the reduction methods were divided into three groups based on their principle mode of action (Table 3).
Five studies explicitly excluded children from their study [14, 25, 26, 29]. A maximum age restriction was specified in five studies: 60 years old in three studies [14, 24, 25] and 90 years old in one study [22].
Most (n = 8) of the studies used clinical examination and X-rays to diagnose dislocation [12, 13, 18, 21, 25,26,27, 29] but two studies only used X-rays [18, 24] and two studies did not specify how dislocation was diagnosed [22, 28].
None of the studies focused on fracture dislocations but six studies specifically allowed inclusion of greater tuberosity fractures associated with dislocation [13, 18, 22, 25, 28, 29]. The rest of the studies did not specify whether greater tuberosity fractures were included. Whilst all studies focused on acute anterior dislocations, only eight of the studies specified that dislocations had to be less than 24 h old [13, 18, 22, 24,25,26, 28, 29].
With regards to number of previous dislocations, only two of the studies excluded patients who had previous dislocations [13, 29].
Baseline characteristics measured varied widely between studies, but the only significant baseline imbalance was reported by Marcano-Fernandez et al. [14] where the average age of the Spaso group (37.1 years) was significantly older than the BHM group (29.7).
Risk of bias
The studies varied widely in the quality of their methods and a summary of their risk is bias is presented in Figs. 2 and 3. All studies were randomised controlled trials except two studies [26, 27], which were quasi-randomised. All studies had balanced patient numbers in each group apart from Amar et al. [26] with n = 35 in the Milch group and n = 25 in the Stimson group, which the author attributed to the method of quasi-randomisation used. In the remaining trials, random number tables were used in four studies [12, 13, 24, 29], block randomisation was used in two studies [14, 18], whilst the rest of the studies did not specify how randomisation was performed. Envelopes were used for concealment in three studies [18, 22, 24], although only Almeida et al. [24] specified that the envelopes were opaque and only Chang et al. [22] specified that the envelopes were presealed.
Due to the nature of the shoulder reduction in awake patients, it was impossible to blind participants and personnel to the method of shoulder reduction. Although, as many patients would naturally not be familiar with different shoulder reduction methods, this lack of patient blinding would be unlikely to create a large amount of bias. The lack of blinding of personnel performing the reduction could, however, generate significant performance bias as different doctors often have their own preferred reduction method(s). The blinding of outcome assessment was very poorly reported with no mention of it in half of the studies [18, 21, 24, 25, 28] and in the other half of the studies [12, 13, 22, 26, 29] it could be deduced that no blinding had been performed.
All the studies had low attrition bias as there were very few drop outs. This probably reflects the fact that all data were collected in one single A&E attendance and no patients were subsequently followed up. Most of the studies appeared to report all comparisons mentioned in their methods but two studies [25, 27] were judged to have high reporting bias as they did not clearly present estimates of effect for their primary outcomes amongst other reporting inconsistencies.
Outcomes
Reduction success
First attempt reduction success was measured in six studies [21, 25,26,27,28,29] and reduction success after up to two attempts using the same technique was also measured in six studies [13, 18, 21, 22, 24, 29]. Two studies used a cross-over technique for the second attempt [25, 27]. Other measures of reduction success included a pragmatic decision by treating doctor to cease further attempts [14] (confirmed by correspondence with author) and successful reduction within 3 min [12]. These other measures of success will be included in the “reduction failure” outcome.
Reduction success after one attempt
Comparison 1: Leverage vs traction–countertraction (Fig. 4)
In the leverage vs traction–countertraction comparison, reduction success after one attempt was measured in three studies. Pooling the data from all three studies showed no significant difference between the groups (RR 0.99, 95% CI 0.87 to 1.14, p = 0.91).
Comparison 2: scapular manipulation vs traction–countertraction
Ghane et al. [25] was the only study that compared scapular manipulation with traction–countertraction and it showed no statistical difference between Modified scapular manipulation and traction–countertraction methods in reduction success after one attempt (RR 1.21, 95% CI 1.00 to 1.46, p = 0.054).
Comparison 3. Milch vs other leverage methods
Two studies [27, 28] compared Milch with other leverage methods. No significant difference was found between groups in either study, or after pooling of the data (RR 0.89, 95% CI 0.74 to 1.08, p = 0.29).
Reduction success after up to two attempts
Comparison 1: leverage vs traction–countertraction (Fig. 5 )
Three studies [13, 21, 29] measured reduction success after success up to two attempts when comparing leverage vs traction–countertraction methods. There was no significant difference the groups in any of the studies, or after pooling of the data (RR 0.94, 95% 0.88 to 1.01, p = 0.07).
Comparison 2: scapular manipulation vs traction–countertraction
Ghane et al. [25] was the only paper to compare scapular manipulation with traction–countertraction and they did not find a significant difference between the groups for reduction success after up to two attempts (RR − 0.13, 95% CI − 0.71 to 0.45, p = 0.66).
Comparison 3: scapular manipulation vs leverage
Sahin et al. [18] was the only study that compared scapular manipulation with leverage and it showed no significant difference between scapular manipulation and Kocher methods in reduction success after up to two attempts (RR 1.07, 95% CI 0.91 to 1.26, p = 0.39).
Comparison 4: spaso vs other traction–countertraction
Two studies [22, 24] compared Spaso vs other traction–countertraction methods measuring reduction success after up to two attempts. No significant difference was found between the groups for reduction success for either study, or after pooling of the data (RR 1.09, 95% CI 0.87 to 1.35, p = 0.54).
Pain
Pain was measured in ten studies all using the 10 point VAS score [12,13,14, 18, 21, 22, 24,25,26, 29]. Whilst pain was measured at various different points in the studies, such as before reduction or prior to discharge, the pain score values used in our meta-analysis are those for pain experienced during reduction itself as this was measured by all of the studies.
Comparison 1: leverage vs traction–countertraction (Fig. 6)
Four studies [13, 22, 26, 29] measured pain during reduction whilst comparing leverage vs traction–countertraction methods. When data was pooled, there was a significantly higher pain score for the leverage group than the traction–countertraction group (MD 0.86, 95% CI 0.64 to 1.08, p < 0.00001).
Comparison 2: scapular manipulation vs traction–countertraction
Ghane et al. [25] showed a significantly lower pain score in the Modified scapular manipulation method than in the traction–countertraction method (MD − 2.27, 95% CI − 2.81 to − 1.73, p < 0.00001).
Comparison 3: scapular manipulation vs leverage
Sahin et al. [18] showed no significant difference between scapular manipulation and Kocher (leverage) methods in terms of pain during reduction (RR 1.07, 95% CI 0.91 to 1.26, p = 0.39).
Comparison 4: spaso vs other traction–countertraction (Fig. 7)
Two studies [22, 24] compared Spaso vs other traction–countertraction methods. Pooling the data showed that pain scores for the Spaso group are significantly lower than other traction–countertraction methods (MD − 1.92, 95% CI − 2.85 to − 1.00, p = 0.00046).
Duration of reduction
Duration taken for reduction was measured in ten studies [12, 13, 18, 22, 24,25,26, 28]. All duration unit of measures were standardised to minutes prior to use in the meta-analysis.
Comparison 1: leverage vs traction–countertraction (Fig. 8)
3 studies [13, 26, 29] compared leverage vs traction–countertraction methods looking at duration taken for reduction. When data were pooled, leverage methods showed a significantly shorter duration of reduction than traction–countertraction methods (MD -0.34 min, 95% CI -0.59 to -0.08, p = 0.0088).
Comparison 3: scapular manipulation vs leverage
Sahin et al. [18] found no significant difference in reduction duration between Scapular manipulation and Kocher (leverage) groups (MD − 0.30 min, 95% CI − 1.31 to 0.71, p = 0.56).
Comparison 4: spaso vs other traction–countertraction (Fig. 9)
Two studies [22, 24] compared duration of reduction for Spaso against other traction–countertraction methods. Pooling the data showed a significantly shorter duration of reduction for the Spaso group compared to other traction–countertraction groups (MD − 4.79, 95% CI − 6.56 to − 3.02, p < 0.00001).
Number of attempts at reduction
Only one study [29] measured average number of attempts at reduction.
Comparison 1: leverage vs traction–countertraction
Maity et al. [29] showed a significantly higher number of reduction attempts needed for the Eachempati (leverage) group than the FARES (traction–countertraction) group (MD 0.32 attempts, 95% CI 0.19 to 0.45, p < 0.00001).
Reduction failure
All papers measured reduction failure, which we defined as failures of reduction requiring reduction in theatre under GA. This outcome allows us to compare all studies in each comparison despite them measuring different success outcomes such as 1st attempt success or success after a certain time period. Reduction failure was not analysed in the scapular manipulation vs traction–countertraction and scapular manipulation vs leverage groups as there was only one study in each comparison and therefore the reduction failure would simply reflect the inverse of their reduction success outcomes. Reduction failure was also not analysed in the Milch vs other leverage methods comparison as both the studies in that comparison had the same reduction success measure (success rate after one attempt) and so reduction failure would simply be the reverse of the pooled data for reduction success after one attempt.
Comparison 1: leverage vs traction–countertraction (Fig. 10)
Five studies [12, 13, 21, 26, 29] compared leverage vs traction–countertraction methods for which reduction failure was measured. Pooling all data showed no significant difference in reduction failure between the two groups (RR 1.07, 95% CI 0.75 to 1.53, p = 0.69).
Comparison 4: spaso vs other traction–countertraction
Three studies [14, 22, 24] compared Spaso against other traction–countertraction methods. There was no significant difference in reduction failure rate between the groups in any of the studies, or after pooling of data (RR 1.52, 95% CI 0.76 to 3.03, p = 0.24).
Complications
Complications were not looked at in detail in any of the studies but eight studies did mention that no short-term complications occurred following the reductions [12,13,14, 22, 24,25,26, 29]. Only Beattie et al. [27] reported a complication which was a fracture of neck of humerus of an 85-year-old woman. None of the studies described any follow-up of the patients after discharge from A&E.
Other outcomes
None of the studies looked at patient satisfaction with the intervention, subsequent recurrence of dislocation or long-term shoulder function.
Discussion
To the best of our knowledge, this the first meta-analysis looking at how effective different methods of closed reduction are for anterior shoulder dislocations. There has only been one previous systematic review (but not meta-analysis) by Alkadulhimi et al. [30] in 2017 which also looks at closed shoulder reduction techniques which included non-RCTs and restricted publications to four languages. They concluded that scapular manipulation was the best method as it was the most successful, fastest, least painful and had the shortest hospital stay. Our meta-analysis included four additional RCTs including the most recent trial looking at self-reduction by Marcano-Fernandez et al. [14] in 2018.
Synthesis of results
After pooling of data, we found six statistically significantly different results between groups.
Pain scores were 0.86 points higher for leverage than traction–countertraction methods. This is counterintuitive as higher forces are usually required for traction–countertraction methods than leverage techniques. One possible explanation is that if leverage techniques are not performed correctly then long lever arms are used with rotational forces causing higher forces through the arm, activating more nociceptors and mechanoreceptors and perhaps predisposing to iatrogenic fractures traditionally associated with leverage techniques (although not evident in this meta-analysis). The minimum clinical important difference (MCID) on the VAS scale has been reported as anywhere between 0.8 and 4.0 points [31]. A score of 0.86 is just at the lower end of the MCID range which suggests that this is probably of some clinical significance. Leverage methods were, however, found to be quicker at reduction by 0.34 min (20.4 s). A possible explanation for this is that, in a similar vein to the closed reduction of distal radius fractures in awake patients, traction–countertraction relies on applying a constant force for long enough to overcome the dynamic shoulder stabilisers through muscle fatigue. It is likely that a quicker reduction technique would avoid a prolonged and potentially painful procedure and therefore shorter duration would be beneficial when considering the reduction technique employed.
When comparing Spaso with other traction–countertraction methods, we found that the Spaso method was less painful by 1.92 points on the VAS scale and was quicker by 4.79 min. These are much more clinically significant effects and therefore it could be concluded that out of all the traction–countertraction methods, Spaso is the best method in terms of being the least painful and quickest, albeit with no difference in overall success rate. In the Spaso technique, traction is applied to a forward flexed arm in a supine patient lifting the scapular off the couch until the patient is relaxed enough to allow their scapular drop down to touch the couch [12]. The fact that it allows gravity/body weight (passive counter-traction) to overcome the dynamic shoulder stabiliser muscles may be why it is the least painful of the traction–countertraction methods. Milch [16] described the shoulder as having three major vector groups acting in a horizontal (rotator cuff), oblique (teres major, pectoralis major and latissimus dorsi) and vertical (deltoid, biceps and triceps) which compete against each other in the normal anatomical position. In the Spaso technique, because the arm is elevated, the three major vector muscle groups align in the same direction and hence this may the reason why it is the fastest traction–countertraction technique [12]. A further reason may be because the Spaso technique also incorporates a leverage element at the end (external rotation after longitudinal traction). As we have shown, leverage methods tend to be faster than traction–countertraction methods.
In the two studies [18, 25] that looked at scapular manipulation, it was significantly less painful than both leverage and traction–countertraction methods by 1.5 and 2.27 points on the VAS scale respectively. However, there was only one study in each comparison and therefore a meta-analysis could not be performed. The reason that scapular manipulation techniques may be the least painful is because they involve rotating the scapula and therefore glenoid to meet the humeral head rather than applying large tractional or leverage forces on the humeral head [10].
It is interesting to note that whilst leverage methods are often not recommended due to the potential for rotational forces to cause fracture, as exemplified by the BESS/BOA Patient Care Pathway for Traumatic anterior shoulder instability [32], only one proximal humerus fracture was reported amongst all the studies [27]. Whilst this may be due to systematic under-reporting of complications, but there is certainly no evidence from this review to demonstrate any increased risk of complications for leverage methods.
After pooling of all results there was no significant difference between the reduction success rates in any of the comparisons.
The use of different types of analgesia, muscle relaxation or anaesthesia is one of the biggest confounding factors to ease of reduction and subjective pain scores. This varied from simple oral analgesia, to intravenous analgesia, to sedation and finally to full anaesthesia, which can make a huge difference to reduction success and pain scores. Unfortunately, details regarding use of analgesia or anaesthesia were under reported in most studies and the exact amount of drugs used in each group were not measured, so meta-analysis could not be performed for this. Fortunately, however, it appears that at least the type of analgesia/anaesthesia used in within each RCT included in the meta-analysis is the same so that each of the reduction groups within each RCT experience the same type of analgesia/anaesthesia.
Greater tuberosity fractures are often treated differently and can influence how difficult it is to achieve closed reduction. However, these were not easy to identify in the studies as it was only clear in six studies [13, 18, 22, 25, 28, 29] that greater tuberosity fractures were included whereas the remaining studies only gave a vague statement that associated fractures were excluded. Amongst these six studies, only three compared the number of greater tuberosity fractures between each group, although no difference was found. The degree of displacement of the fracture following reduction may have been an important outcome measure to use.
The experience of the person performing the reduction and in particular their experience with the reduction method of choice is also a large confounding factor. There was a wide variety of different people performing the reductions, from A&E doctors to orthopaedic residents to orthopaedic consultants. Only five studies [13, 18, 22, 26, 29] specifically stated that the people performing reduction have been trained in the reduction methods used.
Limitations
One of the main limitations of this review is the low number of high quality randomised controlled trials found in the literature. Twelve studies were found with a total of 1158 patients. After splitting them into the separate comparisons, there were a limited studies in each comparison. Despite this we were able to find some significant differences between reduction techniques.
There is also a relatively large risk of bias in the 12 studies as shown in Figs. 2 and 3. This mainly reflects a lack of blinding and also paucity of information regarding randomisation, as discussed in further detail in the “Risk of Bias” section above.
Considerable heterogeneity was observed, as defined by I2 > 75% [19], in most of the pooled analyses. We have used fixed-effects models for our meta-analyses for two main reasons. Firstly, random effects models are primarily used for heterogeneity that cannot be explained [19] but we believe the heterogeneity observed in our meta-analyses can be explained by the fact that we are grouping heterogenous reduction methods into three groups. Secondly, when there are few studies (as is the case in our meta-analysis) then a random effects analysis “will provide poor estimates of the width of distribution of intervention effect” [19].
Conclusions
For clinicians who regularly reduce shoulder dislocations, it is reassuring to conclude that, from the information available, regardless of whether they choose traction–countertraction, leverage or scapular manipulation methods, they all appear to be equally as effective as each other with minimal complications. We conclude that leverage techniques tend to be quicker but marginally more painful than traction–countertraction methods which may affect the choice of reduction method based on patient factors.
Reference
Kazar B, Relovszky E. Prognosis of primary dislocation of the shoulder. Acta Orthop Scand. 1969;40:216–24.
Nordqvist A, Petersson CJ. Incidence and causes of shoulder girdle injuries in an urban population. J. Shoulder Elbow Surg. 1995;4:107–12.
Owens BD, Duffey ML, Nelson BJ, et al. The incidence and characteristics of shoulder instability at the United States Military Academy. Am. J. Sports Med. 2007;35:1168–73.
Simonet WT, Melton LJ 3rd, Cofield RH, Ilstrup DM. Incidence of anterior shoulder dislocation in Olmsted County, Minnesota. Clin Orthop Relat Res. 1984;186:186–91.
DePalma AF, Flannery GF. Acute anterior dislocation of the shoulder. J Sports Med. 1973;1:6–15.
Robinson CM, Howes J, Murdoch H, et al. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Jt Surg Am. 2006;88:2326–36.
Rowe CR. Anterior dislocations of the shoulder: prognosis and treatment. Surg Clin North Am. 1963;43:1609–14.
Kroner K, Lind T, Jensen J. The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg. 1989;108:288–90.
Randelli P, Cucchi D, Butt U. History of shoulder instability surgery. Knee Surg Sports Traumatol Arthrosc. 2016;24:305–29.
Mattick A, Wyatt JP. From Hippocrates to the Eskimo–a history of techniques used to reduce anterior dislocation of the shoulder. J. R. Coll. Surg. Edinb. 2000;45:312–6.
Stimson LA. An easy method of reducing dislocations of the shoulder and hip. Med Rec. 1900;57:356–7.
Rezende Bda R, de Almeida JIS, de Sousa UJ, et al. Glenoumeral dislocation: a prospective randomized study comparing spazo and kocher maneuvers. Acta Ortop Bras. 2015;23:192–6.
Sayegh FE, Kenanidis EI, Papavasiliou KA, et al. Reduction of acute anterior dislocations: a prospective randomized study comparing a new technique with the Hippocratic and Kocher methods. J Bone Jt Surg Am. 2009;91:2775–822.
Marcano-Fernandez FA, Balaguer-Castro M, Fillat-Goma F, et al. Teaching patients how to reduce a shoulder dislocation: a randomized clinical trial comparing the Boss-Holzach-Matter Self-Assisted Technique and the Spaso Method. J Bone Jt Surg Am. 2018;100:375–80.
Kocher T. Eine neue reductionsmethode fur schultetrverrenkung. Berliner Klin Wehnschr. 1870;7:101–5.
Milch H. Treatment of dislocation of the shoulder. Surgery. 1938;3:732–40.
Eachempati KK, Dua A, Malhotra R, et al. The external rotation method for reduction of acute anterior dislocations and fracture-dislocations of the shoulder. J Bone Jt Surg Am. 2004;86:2431–4.
Sahin N, Ozturk A, Ozkan Y, et al. A comparison of the scapular manipulation and Kocher's technique for acute anterior dislocation of the shoulder. Eklem Hastalik Cerrahisi. 2011;22:28–322.
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. 1st ed. USA: Wiley-Blackwell; 2008.
The Nordic Cochrane Centre (2014). The Cochrane Collaboration. Review Manager (RevMan). 5.3
Fang J, Zhang FQ, Wu SF, et al. Manipulation of superduct, adduction, rotation for the treatment of shoulder dislocation. China J Orthop Trauma. 2013;26:16–8.
Chang SH, Lin JH, Hung LW, Chang CH (2014) Comparing FARES method with SPASO method for reduction of anterior shoulder dislocation: a prospective randomized trial. Unpublished material
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med. 2009;3:e123–e130130.
Almeida FIA, de Leitao ICDS, Castro L, de Pires NPJ. Acute anterior glenohumeral dislocation: comparative study between methods of bloodless reduction. Rev Bras Orthop. 2006;41:455–60.
Ghane MR, Hoseini SH, Javadzadeh HR, et al. Comparison between traction–countertraction and modified scapular manipulation for reduction of shoulder dislocation. Chin J Traumatol. 2014;17:93–8.
Amar E, Maman E, Khashan M, et al. Milch versus Stimson technique for nonsedated reduction of anterior shoulder dislocation: a prospective randomized trial and analysis of factors affecting success. J. Shoulder Elbow Surg. 2012;21:1443–9.
Beattie TF, Steedman DJ, McGowan A, Robertson CE. A comparison of the Milch and Kocher techniques for acute anterior dislocation of the shoulder. Injury. 1986;17:349–52.
Sapkota K, Shrestha B, Onta PR, Thapa P. Comparison between external rotation method and milch method for reduction of acute anterior dislocation of shoulder. J. Clin. Diagn. Res. 2015;9:RC01–3.
Maity A, Roy DS, Mondal BC. A prospective randomised clinical trial comparing FARES method with the Eachempati external rotation method for reduction of acute anterior dislocation of shoulder. Injury. 2012;43:1066–70.
Alkaduhimi H, van der Linde JA, Willigenburg NW, et al. A systematic comparison of the closed shoulder reduction techniques. Arch. Orthop. Trauma. Surg. 2017;137:589–99.
Olsen MF, Bjerre E, Hansen MD, et al. Pain relief that matters to patients: systematic review of empirical studies assessing the minimum clinically important difference in acute pain. BMC Med. 2017;15:35.
Noorani A, Goldring M, Jaggi A, et al. BESS/BOA patient care pathways: atraumatic shoulder instability. Shoulder Elbow. 2019;11:60–70.
Puha B, Gheorghevici TS, Veliceasa B, et al. Clasic versus novel in reduction of acute anterior dislocation of the shoulder: a comparison of four reduction techniques. Rev. Med. Chir. Soc. Med. Nat. Iasi. 2016;120:311–5.
Acknowledgements
We would like to thank Mr Subodh Deshmukh and Mr Raj Thakrar for help with the review protocol and screening of studies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest. The authors can confirm that, to the best of our knowledge, there has been no prior or duplicate submission or publication elsewhere of any part of the work. The manuscript has been read and approved by all authors, and each author believes that the manuscript represents honest work.
Ethical approval
No institutional review board (IRB) or Ethical Committee approval was undertaken as this was not applicable.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dong, H., Jenner, E.A. & Theivendran, K. Closed reduction techniques for acute anterior shoulder dislocation: a systematic review and meta-analysis. Eur J Trauma Emerg Surg 47, 407–421 (2021). https://doi.org/10.1007/s00068-020-01427-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-020-01427-9