Abstract
Introduction
Emergency laparotomy is associated with high rates of morbidity and mortality. The need for highly sensitive readily prognostic biomarkers is necessary to improve the outcome. We investigated the usefulness of post-operative arterial lactate and ScvO2/lactate ratio as predictors of outcome after post-operative emergency open laparotomy. To the best of our knowledge, the novel ScvO2/lactate ratio was not investigated before in emergency open laparotomy patients.
Methods
It is a prospective observational cohort study. We investigated the usefulness of post-operative arterial lactate and ScvO2/lactate ratio as predictors of early mortality in 40 patients following emergency open laparotomy admitted to the ICU.
Results
Admission and 24 h lactate levels were predictor of mortality with cut-off point > 3.95 mmol/L, sensitivity 100%, and specificity 93.3%, and cut-off > 3.5 mmol/L, sensitivity 100%, and specificity 96.7%, respectively. In this study, ScvO2/lactate ratio on admission was predictor of at day 7 with cut-off point < 13.95, sensitivity 100%, and specificity 96.7% p < 0.0001. Lactate at 12 and 24 h was also predictor of survival p < 0.0001. Serial arterial lactate was highly correlated to ICU length of stay; admission APACHE II and day 1; and 2 MODS and SOFA scores (p < 0.001).
Conclusion
Serial blood lactate as well as the novel ScvO2/lactate ratio can be useful for early predictors of mortality at 7 days. Serial lactate levels correlate to admission ICU scores APACHE II; MODS and SOFA in post-operative emergency open laparotomy patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Emergency laparotomy is associated with high rates of mortality and post-operative complications, as well as prolonged hospital stay [1]. Global tissue hypoxia (GTH) is often not recognized by use of routinely monitored vital signs or physical findings, such as urine output (UO).
Central venous oxygen saturation (ScvO2) and lactate have been used frequently to better guide clinicians to begin and optimize early hemodynamic treatment and determine the resolution of GTH [2]. Rivers et al. identified a subset of patients with severe sepsis and septic shock by an elevation in lactate and by optimizing early therapy—targeted at the normalization of ScvO2—morbidity and mortality were improved [3].
Global tissue hypoxia after major surgery has been associated with a prolonged ICU course. More recently, abnormal lactate and ScvO2 values obtained immediately after surgery have been found to detect latent shock, and elevated lactate and low ScvO2 have been associated independently with an increased risk of complications after high-risk general surgical patients.
ScvO2 have been shown to reflect circulatory insufficiencies successfully. Elevations in lactate have been associated with increased risk of morbidity and mortality in high-risk surgical patients. ScvO2 has been associated independently with post-operative complications in patients who have undergone emergency laparotomy. Patients after emergency laparotomy who had prolonged ICU LOS have been found to have a significantly lower ScvO2 [4].
Materials and methods
This is a prospective cohort observational study conducted on 40 patients, 22 males (55%) and 18 females (45%), Nasser institute hospital during 30 month duration. Patients were admitted to intensive-care unit following emergency laparotomy as specified by treating health care teams. All patients were subjected to post-operative care management according to ICU protocols. An arterial line is inserted and informed patient consent was obtained for all patients. The study was approved by critical care department and Cairo University ethical committee.
Study criteria
Inclusion criteria
Adult patients admitted to intensive-care unit after open emergency laparotomy for any cause and considered at high risk of post-operative complications.
Exclusion criteria
-
Age less than 18 years.
-
Intraoperative cardiac arrest.
-
Presence of cardiogenic shock immediately before surgery.
-
Patients with terminal malignancy.
-
Metabolic inborn errors affecting lactate metabolism.
-
Patients on metformin or any drug affecting lactate metabolism.
Study procedure
Following ICU admission, all patients were subjected to detailed and full history taking and thorough clinical examination from the patient and/or his relatives.
In addition, routine laboratory labs plus arterial lactate and central venous oxygen saturation collected from central venous line every 6 h for 24 h. Comparative data between scores and morbidity and mortality, central venous oxygen saturation and lactate, and effect on morbidity and mortality were also collected.
Outcome
Primary outcome is the mortality and secondary outcomes include length of hospital stay and development of major adverse events as shock, cardiac arrest, serious arrhythmias, acute kidney injury, and cerebrovascular stroke.
Statistical methods
Data were analyzed using IBM© SPSS© Statistics version 23 (IBM© Corp., Armonk, NY, USA) and MedCalc© version 18.11.3 (MedCalc© Software bvba, Ostend, Belgium).
Continuous numerical data were presented as mean and standard deviation and intergroup differences were compared using the unpaired t test. Categorical data were presented as number and percentage and intergroup differences were compared using Fisher’s exact test. Receiver-operating characteristic (ROC) curve analysis was used to examine the prognostic value of serum lactate or ScvO2/lactate ratio for prediction of mortality. Survival analysis was done using the Kaplan–Meier method. The log-rank test was used to compare individual Kaplan–Meier curves. p values < 0.05 were considered statistically significant.
Results
This is a prospective observational cohort study conducted on 40 post-operative patients admitted to the surgical intensive-care unit (ICU), Nasser institute hospital during the period from March 2013 to October 2015. The mean age of patients was 59.7 ± 12.9 years (range 30–81 years). There were 22 males (55%) and 18 females (45%).
In our study, causes of emergency laparotomy were intestinal obstruction 11 patients (27.5%), perforated duodenal ulcer (DU) 10 patients (25%), complicated hernia 6 patients (15%), rupture appendix 5 patients (12.5%), trauma 4 patients (10%), and intra-abdominal abscess 1 patient (2.5%) (Table 1).
Out-of-study population different co-morbidities were found: 20 patients were smokers (50%), 31 patients were hypertensive (77.5%), 28 patients were diabetic (70%), 28 patients presented with history of cardiac problems including heart failure, ischemic heart disease, and valvular heart disease (70%), 11 patients had chronic renal disease (27.5%), and 6 patients had decompensated liver failure (15%).
In this study, 26 patients were mechanically ventilated upon ICU admission following emergency laparotomy (65%). Twenty patients developed renal impairment (50%) after ICU admission. Twenty-eight patients (70%) were in need for use of vasopressors with mean duration 79.5 h. In our study, mean length of stay (LOS) in ICU was 3.7 ± 1.2 days with range from 2 to 8 days. Length of hospital stay was 3–12 days with mean 7.6 ± 2.3 days (Table 2).
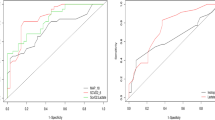
Initial and serial lactate levels at 12 h were highly predictor of mortality with cut-off point > 3.9 mmol/L and > 3.5 mmol/L with sensitivity 100% and specificity 93.3% p < 0.0001, respectively. In addition, lactate at 24 h at cut-off level > 2.9 mmol/L is highly predictor of mortality with sensitivity 90% and specificity 96.7% p < 0.0001 (Table 4 and Fig. 1).
Correlations of serial blood lactate levels with length of stay in ICU
There was highly significant positive correlation between lactate OA, 12 and 24 h, and length of stay in ICU (correlation coefficient 0.522, 0.551, and 0.554), respectively; p < 0.001.
Kaplan–Meier curves showed the significant importance of initial and serial lactate levels and initial and serial ScvO2/lactate ratio as predictor of mortality in open emergency laparotomy patients admitted to the ICU (Figs. 2, 3, 4).
Kaplan-–Meier survival curves in patients with serum lactate ≤ 3.9 mmol/l or > 3.9 mmol/l (upper plot, a) and in patients with ScvO2/lactate ratio > 13.95 or ≤ 13.95 (lower plot, b) at ICU admission. Median survival in patients with serum lactate > 3.9 mmol/l is 4 days (95% CI 4–7 days) and could not be estimated in patients with serum lactate ≤ 3.9 mmol/l. The difference between the survival curves of both subgroups is statistically significant (Log-rank test Chi squared, 39.128; df 1; p value < 0.0001; hazard ratio could not be estimated). Likewise, median survival in patients with ScvO2/lactate ratio ≤ 13.95 is 4 days (95% CI 4–7 days) and could not be estimated in patients with ScvO2/lactate ratio > 13.95. The difference between the survival curves of both subgroups is statistically significant (Log-rank test Chi squared, 43.816; df, 1; p value < 0.0001; hazard ratio, 382.6; 95% CI 65.8–2226.1)
Kaplan-Meier survival curves in patients with serum lactate ≤ 3.5 mmol/l or > 3.5 mmol/l (upper plot, a) and in patients with ScvO2/lactate ratio > 19.74 or ≤ 19.74 (lower plot, b) at 12 h from ICU admission. Median survival in patients with serum lactate > 3.5 mmol/l is 4 days (95% CI 4–7 days) and could not be estimated in patients with serum lactate ≤ 3.5 mmol/l. The difference between the survival curves of both subgroups is statistically significant (log-rank test chi-squared, 39.128; df 1; p value < 0.0001; hazard ratio could not be estimated). Likewise, median survival in patients with ScvO2/lactate ratio ≤ 19.74 is 4 days (95% CI 4–7 days) and could not be estimated in patients with ScvO2/lactate ratio > 19.74. The difference between the survival curves of both subgroups is statistically significant (log-rank test chi-squared, 39.128; df 1; p value < 0.0001; hazard ratio could not be estimated)
Kaplan–Meier survival curves in patients with serum lactate ≤ 2.9 mmol/l or > 2.9 mmol/l (upper plot, a) and in patients with ScvO2/lactate ratio > 25.0 or ≤ 25.0 (lower plot, b) at 24 h from ICU admission. Median survival in patients with serum lactate > 2.9 mmol/l is 4 days (95% CI 4–7 days) and could not be estimated in patients with serum lactate ≤ 2.9 mmol/l. The difference between the survival curves of both subgroups is statistically significant (log-rank test chi-squared, 37.668; df 1; p value < 0.0001; hazard ratio, 191.2; 95% CI 35.7–1023.3). Likewise, median survival in patients with ScvO2/lactate ratio ≤ 25.0 is 4 days (95% CI 4–7 days) and could not be estimated in patients with ScvO2/lactate ratio > 25.0. The difference between the survival curves of both subgroups is statistically significant (log-rank test chi-squared, 37.668; df, 1; p value < 0.0001; hazard ratio, 191.2; 95% CI 35.7–1023.3)
In our study, central venous oxygen saturation/lactate ratio on admission was predictor of survival at day 7 with cut-off point ≤ 13.95, sensitivity 100%, and specificity 96.7% p < 0.0001 (Table 4; Fig. 1).
Correlation of arterial lactate to APACHE II, MODS D1, and SOFA D1 critical illness scores
Admission arterial lactate; lactate at 12 and 24 h was highly correlated with APACHE II score day 1 (p < 0.001) and correlation coefficient was (0.67; 0.649; 0.569).
Admission arterial lactate; lactate at 12 and 24 h was highly correlated with MODS score day 1 (p < 0.001) and correlation coefficient was (0.737; 0.747; 0.767).
Admission arterial lactate; lactate at 12 and 24 h was highly correlated with SOFA score day 1 (p < 0.001) and correlation coefficient was (0.632; 0.617; 0.579) (Fig. 5).
Relations of lactate with survival at day 7
There was highly significant positive relation between lactate OA, at 12 h and 24 h, and mortality as p value was < 0.0001 (Table 3; Fig. 1).
ROC curve of ScvO2/lactate ratio with mortality
In our study, central venous oxygen saturation/lactate ratio on admission was predictor of survival with AUC 0.970, cut-off point ≤ 13.95, sensitivity 100%, and specificity 96.7% p < 0.0001 (Fig. 1).
In our study, central venous oxygen saturation/lactate ratio At 12 h was predictor of survival with AUC 0.962, cut-off point ≤ 19.74, sensitivity 100%, and specificity 93.3% p < 0.0001 (Table 4; Fig. 1).
In our study, central venous oxygen saturation/lactate ratio At 24 h was predictor of survival with AUC 0.977, cut-off point ≤ 25, sensitivity 90%, and specificity 96.7% p < 0.0001 (Table 4; Fig. 1).
Discussion
Emergency open laparotomy poses unique challenges to both the surgeon and anesthetics. Emergency open laparotomy is usually done in patients who are not prepared preoperatively such patients may be dehydrated, hypotensive; with varying degrees of biochemical derangement and very sick with ongoing sepsis.
Emergency surgery may be done by junior staff of surgeons and anesthesiologists, so post-operative complications may be increased.
Emergency laparotomy can lead to serious complications and attentive monitoring is a must. The ongoing imbalance between oxygen demand and oxygen supply is an initiator for the cascade of events leading to multiple organ dysfunction syndrome. Prompt detection and management of hypoperfusion state is, therefore, the key for better survival [5].
Standard indicators of perfusion, such as blood pressure or urine output, have been proved repeatedly to be inaccurate. Therefore, the need for accurate assessment tool of hypoperfusion is essential to suppress the incidence of organ dysfunction in these patients [6].
Central venous oxygen saturation (ScvO2) and blood lactate have been found to be valuable indicators for evaluating the degree of hypoperfusion in patients with different disease processes [3, 4, 7].
In our study, 26 patients were mechanically ventilated after admission to ICU following emergency laparotomy (65%). This agrees with Litton et al. [8] who reported that 51% of patients need mechanical ventilation after major surgery.
In our study, there was highly significant positive relation between serial lactate in the 1st 24 h after ICU admission and mortality as p value was < 0.001; this is similar to the results obtained by Hu [9].
Beebee concluded that patients who developed severe Global Tissue Hypoxia which was defined as ScvO2 < 70% and lactate ≥ 4 mmol/L have longer lengths of ICU stay; time on mechanical ventilation and more complications following post-CABG or valve surgery. He also concluded that the use of ScvO2 and lactate allows rapid identification of occult hypoperfusion post cardiac surgery and can positively affect the outcome. The use of our results agrees also with André Meregalli [10], who reported that increased lactate level was associated with increased incidence of major adverse events and mortality in 44 hemodynamically stable high-risk surgical patients and Husain et al. [11] who showed that elevated the initial and 24-h lactate levels correlated significantly with 30-day mortality in 137 surgical ICU patients.
In our study, the cut-off point for the mortality prediction at day 7 of admission lactate was > 3.9 mmol/L with sensitivity 100% and specificity 93.3%. Ole Kruse et al. [12] also found that a cut-off point for admission lactate 2.5 mmol/L is predictor of 30-day mortality with sensitivity 86% and specificity 77%.
Our results confirm one of the largest studies depicting lactate clearance in major trauma patients; Heinonen et al. [13] who reported that the survival rate of patients with lactate values < 2.5 mmol/L was 88% and of the patients with high lactate levels that cleared within 24 and 48 h, the survival rates were 81% and 71%, respectively. They concluded that arterial lactate clearance trends are reliable simple predictor of outcome following major trauma [13].
In our study, we found that ScvO2/lactate ratio on admission to ICU was predictor for mortality at cut-off point ≤ 13.95 with sensitivity 100%, and specificity 96.7%; this agrees with Zante et al. [14], who reported that the ratio of ScvO2%/lactate at ICU admission is a better predictive power of 28-day mortality in patients after cardiac surgery than the individual values with the optimal cut-off-value was 29.61. This value led to a sensitivity of 81.25% and a specificity of 73.66%.
In our study, mortality at day 7 was 25%; this agrees with D. I. Saunders [15] who reported that 30-day mortality was 24.4% after emergency laparotomy. Also Clarke [16] showed that 30-day mortality was 19.6% after emergency laparotomy and Vester-Andersen et al. [17] reported that 90-day mortality in 2803 patients after emergency abdominal surgery was 18.4%. Peden et al. also reported that mortality after emergency open laparotomy in United Kingdom was 16% in 1587 patients [18]. In patients older than 65 years; 1 year mortality reached 34% [19] Also emergency laparotomy during hospital stay and remote from admission is associated with high morbidity and > 40% mortality [20] This can be explained by the associated admission co-morbidities and the resistant hospital organisms infections in addition to complications of the prolonged hospital stay.
Emergency open laparotomy in the already admitted critically ill patients showed mortality 55.6%; the authors concluded that the high mortality is anticipatable based on concurrent abnormal physiology [21].
Conclusion
A highly significant correlation < 0.001 was detected between admission and serial arterial lactate levels and ICU length of stay; admission APACHE II; SOFA and MODS.
Serial blood lactate and ScvO2/lactate ratio are reliable predictors of post-operative open laparotomy outcome in critically ill patients with the latter providing 100% sensitivity and 90% specificity at admission cut-off ≤ 13.95, and at 12 h, sensitivity 100%, and specificity 93.3%. cut-off ≤ 19.74 and At 24 h, cutoff ≤ 25.00 can provide sensitivity 90% and specificity 96.7% for mortality prediction.
Serial ScvO2/lactate ratio can improve risk stratification and guide early rapid management to provide better outcome in post-operative emergency open laparotomy patients admitted to the ICU.
Change history
01 June 2022
Addition of the university email: narnar_is@cu.edu.eg.
References
Howes TE, Cook TM, Corrigan LJ, Dalton SJ, Richards SK, Peden CJ. Postoperative morbidity survey, mortality and length of stay following emergency laparotomy. Anaesthesia. 2015;70:1020–7.
ZhongBing ZW. Improvement effect of early goal-directed therapy on the prognosis in patients with septic shock. Ji Jiu Yi Xue. 2015;27(11):899–905.
Rivers E, Nguyen B, Havstad S, Ressler J, Alexandria M, Bernhard K, for the Early Goal-Directed Therapy Collaborative Group, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77.
Rusconi AM, Bossi I, Lampard JG, Szava-Kovats M, Bellone A, Lang E. Early goal-directed therapy vs usual care in the treatment of severe sepsis and septic shock: a systematic review and meta-analysis. Intern Emerg Med. 2015;10(6):731–43. https://doi.org/10.1007/s11739-015-1248-y.
Namas Rami A, Almahmoud Khalid, Mi Qi, Ghuma Ali, Namas Rajaie, Zaaqoq Akram, et al. Individual -specific principal component analysis of circulating inflammatory mediators predicts early organ dysfunction in trauma patients. J Crit Care. 2016;36:146–53.
Rivers EP, Yataco AC, Jaehne AK, Gill J, Margaret D. Oxygen extraction and perfusion markers in severe sepsis and septic shock: diagnostic, therapeutic and outcome implications Curr Opin Crit Care. 2015;21(5):381–7.
Pearse RM, Rhodes A. Mixed and central venous oxygen saturation. In: Vincent JL, editor. Yearbook of intensive care and emergency medicine. Berlin: Springer; 2005. p. 592–602.
Litton E, Silbert B, HoK M. Clinical predictors of a low central venous oxygen saturation after major surgery: a prospective prevalence study. Anaesth Intensive Care. 2015;43(1):59.
Hu BY, Laine GA, Wang PHS, Solis RT. Combined central venous oxygen saturation and lactate as markers of occult hypoperfusion and outcome following cardiac surgery. J Cardiothorac Vasc Anaesth. 2012;26(1):52–7.
Meregalli A, Oliveira RP, Friedman G. Occult hypoperfusion is associated with increased mortality in hemodynamically stable, high-risk, surgical patients. Crit Care. 2004;8(2):R60–5.
Husain FA, Martin MJ, Mullenix PS, Steele SR, Elliott DC. Serum lactate and base deficit as predictors of mortality and morbidity. Am J Surg. 2003;185(5):485–91.
Kruse Ole, Grunnet Niels, Barfod Charlotte. Blood lactate as a predictor for in-hospital mortality in patients admitted acutely to hospital. Scand J Trauma Resusc Emerg Med. 2011;19:74. https://doi.org/10.1186/1757-7241-19-74.
Heinonen E, Hardcastle TC, Barle H, Jackson Muckart DJ. Lactate clearance predicts outcome after major trauma. Afr J Emerg Med. 2014;4:61–5.
Zante B, Kubik M, Reichenspurner H. ScvO2/lactate-ratio as prognostic factor of mortality in patients admitted to intensive care unit after cardiac surgery. Thorac Cardiovasc Surg. 2011. https://doi.org/10.1055/s-0030-1269315.
Saunders DI, Murray D, Pichel AC, Varley S, Peden CJ. Variations in mortality after emergency laparotomy: the first report of the UK Emergency Laparotomy Network. Br J Anaesth. 2012;109(3):368–75.
Clarke A, Murdoch H, Thomas MJ, Cook TM, Peden CJ. Mortality and postoperative care after emergency laparotomy. Eur J Anaesthesiol. 2011;28(1):16–9.
Vester-Andersen M, Lundstrøm LH, Buck DL, Møller MH. Association between surgical delay and survival in high-risk emergency abdominal surgery. A population-based Danish cohort study. Scand J Gastroenterol. 2016;51(1):121–8. https://doi.org/10.3109/00365521.2015.1066422.
Peden CJ, Stephens T, Martin G, Kahan BC, Thomson A, Rivett K, Enhanced Peri-Operative Care for High-risk patients (EPOCH) trial group, et al. Effectiveness of a national quality improvement programme to improve survival after emergency abdominal surgery (EPOCH): a stepped-wedge cluster-randomized trial. Lancet. 2019. https://doi.org/10.1016/s0140-6736(18)32521-2(Epub ahead of print).
Cooper Zara, Mitchell Susan L, Gorges Rebecca J, Rosenthal Ronnie A, Lipsitz Stuart R, Kelley Amy S. Predictors of mortality up to one year after emergent major abdominal surgery in older adults. J Am Geriatr Soc. 2015;63(12):2572–9. https://doi.org/10.1111/jgs.13785.
Sharoky CE, Bailey EA, Sellers MM, Kaufman EJ, Sinnamon AJ, Wirtalla CJ, et al. Outcomes of hospitalized patients undergoing emergency general surgery remote from admission. Surgery. 2017;162(3):612–9. https://doi.org/10.1016/j.surg.2017.05.008(Epub 2017 Jul 6).
Martin Niels D, Patel Sagar P, Chreiman Kristen, Pascual Jose L, Braslow Benjamin, Reilly Patrick M, et al. Emergency laparotomy in the critically ill: futility at the bedside. Crit Care Res Pract. 2018;2018:6398917. https://doi.org/10.1155/2018/6398917.
Funding
No funding was received for this medical research. It is a self-funded study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors confirm they have no conflict of interest.
Ethical approval
The research was approved by the local ethical committee of the Critical Care Department and then the Ethical committee of Faculty of Medicine Cairo University.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Salem, G., Abbas, N.I., Zakaria, A.Y. et al. Central venous oxygen saturation/lactate ratio: a novel predictor of outcome following emergency open laparotomy. Eur J Trauma Emerg Surg 47, 353–363 (2021). https://doi.org/10.1007/s00068-019-01188-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-019-01188-0