Abstract
Introduction
The traditional 24-h call model faces pressure from competing needs between emergency and elective services. Recognizing this, a dedicated ESAT service was developed in Khoo Teck Puat Hospital in Singapore, with improved clinical outcomes. It was initially led by a single consultant (SC) in 2014, and subsequently evolved to a weekly consultant rotation (WC) roster in 2017 to achieve sustainability.
Methods
Each consultant led the ESAT WC service for a week and maintained ownership of their patients thereafter. All emergency surgical admissions between two distinct 6-month periods were reviewed, from May to October 2014 (pre-ESAT) and January to June 2017 (ESAT WC). Patient demographics, diagnoses, and operations were compared. Efficiency and clinical outcomes were evaluated.
Results
There were 1248 and 1284 patients in the pre-ESAT and ESAT WC group, respectively. Majority were males and in their 50s. Acute appendicitis, gallstone conditions, and soft-tissue infections made up half of the admissions. Trauma workload was comparable (7.8% pre-ESAT vs 9.5% ESAT WC). Cholecystectomies doubled during the ESAT period, 14.2% vs 7.2%, (p = 0.01). More consultants were involved in major cases (95.9% vs 86%), (p = 0.01) and more operations were performed during the day (52.1% vs 47.9%), (p = 0.01). Average time to OT was shorter and there were less major surgical complications (p = 0.02). Mortality (p = 0.08) and length of stay were reduced (4 vs 4.5 days), (p = 0.01).
Conclusion
The ESAT WC service has sustained improved outcomes in our institution.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute care surgery (ACS) as a distinct subspecialty within general surgical practice has been in existence for over a decade. Despite being widely accepted in many centers over the world, the delivery of care is variable depending on the hospital’s resources and need of local population [1]. Acute surgical care encompasses three segments, namely, trauma care, surgical critical care, and emergency general surgery. The American Association for the Surgery of Trauma defined an emergency general surgery patient as one requiring emergency surgical evaluation for diseases within the realm of general surgery [2].
The creation of ACS services aims to ensure that these groups of patients receive dedicated care while enabling other subspecialties to focus on their elective work. The ACS services have demonstrated decreased time to surgical intervention for common emergency surgery and improved physician satisfaction and clinical productivity [3,4,5,6].
In Singapore, Khoo Teck Puat Hospital (KTPH) has developed the first consultant-led dedicated Emergency Surgery and Trauma (ESAT) unit. The ESAT unit is adopted from Acute Care Surgery model to ensure efficient, coordinated and accessible care for emergency surgical, trauma, and acute care patients [7].
Prior to the advent of ESAT service, acute general surgery admissions followed a typical 24-h call model, where each consultant on call evaluated and provided operative management if required for all emergency admissions and inpatient consults. This is in addition to the daily elective workload comprising of outpatient clinics, elective endoscopies, and operating theatres.
This traditional model of care hence faces a myriad of pressures arising from the need to juggle competing needs between elective and emergency services. These pressures include timely review of emergency and trauma patients, availability of consultant on call in critical scenarios and appropriate supervision of junior staff. Coupled with general surgical emergency workload increasingly is being neglected due to trend towards subspecialisation, these pose concerns regarding patients’ outcomes and providers’ satisfaction [7].
Recognizing these pressures, the concept of a dedicated team providing ESAT service was developed with aims to improve quality of care in face of the constant demand of unpredictable and complex emergency and trauma care [8].
The structure of an ESAT service was previously described in Singapore Medical Journal [9]. Our ESAT service functions with this structure and has showed improved outcomes in 2014 when led by a single consultant. In 2017, our ESAT service evolved to include more consultants while preserving its underlying principles. The adaptation of delivery of ESAT service was in response to changing demands of our department’s manpower. In 2014, a single consultant trained in acute care surgery established and ran the ESAT unit. A year after the implementation of the ESAT service, it has led to improvement in efficiency of workflow, supervision rates, and patients’ outcomes [10]. Promising, as it may seem, the challenge of the service then face is to sustain these improvements.
In January 2017, the ESAT team evolved to a weekly consultant rotation (WC) roster instead of a single-consultant-led (SC) team while preserving the fundamental characteristics of the ESAT service (Table 1). In ESAT SC, a single consultant runs the ESAT service daily during weekdays from 7:30 am through 4:00 pm. Acute care surgery needs that occurs after 4:00 pm and on weekends will be managed by a scheduled consultant from the remaining pool of surgeons in the department. In the WC roster, consultants are scheduled in turns to run the service for a week each, fulfilling the same requirements during weekdays. During their week of involvement, they are given dedicated time away from other regular commitments in their subspecialty. Each consultant maintains ownership of their patients even after their scheduled week in ESAT is over. The ESAT service will then begin each working week anew, with the next consultant. This ensures comparable patient ownership and continuity of care in both models.
Aim
The objective of this study is to compare the efficiency and clinical outcomes before the introduction of ESAT service and after the implementation of the ESAT weekly consultant rotation (WC) roster. Our hypothesis is that the current ESAT WC roster has improved outcomes and hence achieved sustainability after 3 years since its establishment.
Materials and methods
Hospital ethical approval was obtained from the National Healthcare Group (NHG) prior to conduct of the study. A review of all emergency general surgical admissions in KTPH during two distinct 6-month time periods was made, from May to October 2014 and January to June 2017. The former time period corresponds to the pre-ESAT period, while they latter correspond to the first 6 months of ESAT WC roster. The annual volume of tier 1 and 2 trauma cases defined as injury severity score of above 15 and between 9 and 15, respectively, was recorded for 2012–2017.
A retrospective review of patient demographics, discharge diagnosis, and operative interventions was performed. Efficiency outcomes such as the number of admissions and operations, time to initial assessment, time to surgery, and hospital length of stay (LOS) were collected. Priority (P) status of surgeries was recorded and compared to waiting time to surgery. Priority (P) status of surgeries is used for booking the emergency cases for OT in our hospital. P1 refers to operations to be performed within 60 min (criteria: immediate life-saving operation, e.g., trauma laparotomy for exsanguinating abdominal injuries, ruptured aortic aneurysm), P2 within 4 h (criteria: operation as soon as possible after resuscitation, e.g., laparotomy for perforated viscus), and P3 within 24 h (criteria: urgent operation: e.g., appendicitis and incarcerated hernia). Clinical outcomes studied included readmission, complication, and mortality rates. Readmissions were defined by admissions within 30 days of discharge, attributed to conditions or complications related to the original diagnosis or surgical intervention. Complications were reported based on Clavien–Dindo classification and obtained from case records. Data regarding the presence of consultant in the operative theatres, time of day for which the surgery was performed was obtained from operative notes. Patients aged 18 and below were excluded, as they were transferred to the nearest pediatric hospital as soon as their conditions were deemed stable.
Statistics
Patient demographics, efficiency, and clinical outcomes were compared between the two time periods, pre- and post-ESAT establishment. For categorical variables, counts and percentages were reported, while for continuous variables, median and quartiles were reported. Differences were assessed using Student’s t test for continuous data and Chi-squared test for categorical data. A p value of < 0.05 was considered statistically significant. Analyses were performed using IBM SPSS, Version 22.0.
Results
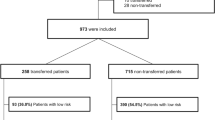
Major trauma load has increased over the period of 2012–2017, as shown in Fig. 1 and Table 2. After the implementation of the ESAT service, the crude death rate has decreased over the corresponding period (Fig. 2). The two distinct 6-month cohorts included 2532 patients of which 1248 of them were managed prior to establishment of the ESAT service. Baseline characteristics for these two groups are shown in Table 3. Majority of the patients were in their fifties, and two-thirds were males. No significant differences in age or gender distribution were observed. There were significantly more patients with colitis, gastritis, gastroenteritis managed in the ESAT period and less with non-specific abdominal pain as compared to the pre-ESAT period. Acute appendicitis, hepatico-pancreatico-biliary diseases, and soft-tissue infections made up half of the admissions. Trauma discharges were comparable, 7.8% during the pre-ESAT period vs 9.5% during the ESAT period. The most common operations performed include incision and drainage, appendicectomies, cholecystectomies, and exploratory laparotomies, as shown in Table 3. There was significantly higher number of cholecystectomies performed during the ESAT period, 83 (14.2%) vs 41 (7.2%). Emergency endoscopies were comparable between the two periods (Table 4).
The average time to ED review by the surgical team was shorter in the ESAT period, 75 min as compared to 81 min in the pre-ESAT period; however, this did not reach statistical significance (p = 0.09) (Table 5). There was significantly greater involvement of consultants in major cases (95.9% vs 86%) and higher number of cases performed in the day (7.30 am–4 pm) in the ESAT period (52.1% vs 47.9%). Surgeries were significantly increased in the daytime include appendicectomies, cholecystectomies, and drainage of abscesses (p < 0.05) (Table 6). The average time to OT allocation (min) was significantly reduced in the ESAT period. The average time was halved for P1 cases − 26 vs 47 min in the ESAT period as compared to pre-ESAT, respectively, P2–63 vs 98 min and P3–76 vs 225 min (p = 0.001).
Comparing key outcome indicators between the two periods, there were fewer Clavien–Dindo grade three and four surgical complications and lower overall mortality in the ESAT period (Table 7). The length of stay was significantly reduced in the ESAT period (4 vs 4.5 days), with shorter stays in high dependency and intensive care units. There was also a reduction in readmission rates (p = 0.1) in the ESAT period.
Discussion
Despite the plethora of evidence on improved outcomes with adoption of Acute Care Surgery model of care, recent surveys of University Hospitals in the US revealed that only a third had adopted the model [3]. KTPH is the first hospital in Singapore to adopt the ACS model which is known as ESAT unit since 2014. While the initial ESAT SC has shown improved efficiency and outcomes [10], its long-term sustainability remains a concern over the years. In face of ongoing issues of increased acute care workload and need for a sustainable pool of acute care surgeons, the ESAT SC was modified to the WC roster to achieve sustainability of the service.
After establishment of the ESAT WC roster, there is improved access to surgical review and treatment as compared to the pre-ESAT period. Coupled with higher consultant supervision rates, patient safety outcomes such as complication rates and mortality have reduced. There was also reduction in hospital length of stay. Despite increasing trauma workload over the years, we also observed reduction in crude mortality from trauma.
We attribute the achievement of these outcomes to four main reasons:
-
1.
Improved resource allocation and productivity after separating elective and emergency work streams.
-
2.
Consistent senior supervision of management decisions, discharge planning and operative cases.
-
3.
Consistent team access by staff from multiple disciplines such as the emergency department, radiological department, intensive care unit and operating theatre.
-
4.
The trauma and emergency surgical skills and experience complement each other allowing extensive experience to provide care to complex emergency or trauma care.
The enforcement of routine consultant-led rounds in the afternoon facilitates timely review of patients’ clinical updates and investigations’ results led to appropriate and efficient management. Similarly, handover meetings in the morning regarding overnight admissions ensures robust continuity of care for patients. This is essential for identification of ongoing issues and hence facilitating planning of treatment and manpower for the day. Our findings of improved clinical outcomes were comparable with that illustrated in the current literature [3,4,5,6].
About 10% of workload was trauma related of which most were managed non-operatively, while the remainder comprised of emergency surgery. Therefore, it is ideal to incorporate both emergency surgery and trauma as a combined service in our institute. It provides an opportunity to maintain operative skills and experience in our unit due to more common non-operative management of injuries in trauma. Comparing pre-ESAT and post-ESAT periods, majority of diagnoses was comparable. There is a trend towards lower rates of non-specific diagnoses in the ESAT period. This could be due to improved communication with ED colleagues, timely review of patients triaged to surgical care and early computed tomography scans prior to admission. We also observed doubling of cholecystectomies performed in the acute setting in the post-ESAT period without increased complication rates.
Prior to the implementation of ESAT unit, the management of acute gallbladder conditions was not standardised and was shared amongst hepatobiliary and general surgeons. There were constraints to perform index admission cholecystectomy during the pre-ESAT period such as concurrent elective clinics, endoscopies, and elective OT for the general surgeon on call. One of the benefits of ESAT unit is the availability of the emergency consultant surgeon without elective commitment to manage the acute gallbladder conditions effectively and efficiently. The ESAT service hence provides more index admission laparoscopic cholecystectomy and potentially reduces readmission rates and overall length of stay in patients that would have been managed with interval cholecystectomies in the pre-ESAT period.
Our study highlights the potential for adaptability in the manpower arrangement of the ESAT unit without compromise on outcomes. The current WC roster involves consultants who are committed to both acute care service as well as their own individual surgical subspecialties. This enables them to hone their skills and accumulate experience in acute care surgery while at the same time continuing their elective surgical work during off periods. For the department, it ensures an adequate trained pool of surgeons in acute care surgery. The advantages of this include opportunities to establish a larger network with relevant health care professionals, permit flexibility for manpower shifts and prevention of burnout of surgeons.
It is evident in our study that the outcomes of the ESAT unit in KTPH are sustainable even after the adoption of a weekly consultant rotation roster. Underlying the success of the ESAT unit in our institute is the support from the hospital stakeholders as well as fellow surgical colleagues within the department. With sustained results, the development of ACS will hopefully gain traction in this region. The authors feel that the single-consultant-led ESAT unit can be adopted as a bridge to full implementation of the WC roster when there are sufficient committed ACS specialists and a rising workload. The ESAT WC roster can potentially be adopted in countries, where the subspecialty of acute care surgery has not been established.
Further areas of development of the current ESAT unit include maximizing training opportunities and encouraging further training for surgical residents interested in acute care surgery. It is essential to attract aspiring young surgeons into this emerging field to develop acute care surgery as a subspecialty in Singapore. The authors are also exploring protocol led pathways for common emergency surgeries (e.g., laparoscopic appendicectomies, cholecystectomies, or emergency laparotomies) and the incorporation of geriatric physicians to improve the care of elderly patients undergoing emergency general surgery [11,12,13,14].
The limitations of the study include its retrospective nature with potential biases. The presence of confounding effects that were difficult to adjust include differences in quality of care and surgical technology between the two time periods and the level of experience of surgeons rotating weekly in the ESAT WC roster. There were no adjustments performed for the different case mixes in both time periods, comorbidities, and time of the year. Despite this study’s early (third year) outcomes and limitations, the ESAT unit has potential to benefit the patients with further standardisation and improvement of acute care processes. Further studies with longer period for observation of outcomes and comparison between ESAT WC and SC frameworks may be worthwhile to undertake.
Conclusion
Acute care surgery model has shown sustained improvement in the clinical outcomes and efficiency of patient care in our institution. The ESAT unit has integrated into the General Surgery department successfully separating the emergency and elective workload.
References
Pearce L, Smith SR, Parkin E, Hall C, Kennedy J, Macdonald A. Emergency general surgery: evolution of a subspecialty by stealth. World J Emerg Surg WJES. 2016;11:2. https://doi.org/10.1186/s13017-015-0058-x.
The American Association for the Surgery of Trauma. http://www.aast.org/AcuteCareSurgery.aspx. Accessed 29 Apr 2018.
Ball CG, MacLean AR, Dixon E, Quan ML, Nicholson L, Kirkpatrick AW, Sutherland FR. Acute care surgery: the impact of an acute care surgeryservice on assessment, flow, and disposition in the emergency department. Am J Surg. 2012;203(5):578–83.
Cubas RF, Gomez NR, Rodriguez S, Wanis M, Sivanandam A. GarberoglioCA. Outcomes in the management of appendicitis and cholecystitis in the setting of a new acute care surgery service model: impact on timing and cost. J Am Coll Surg. 2012;215(5):715–21.
Barnes SL, Cooper CJ, Coughenour JP, MacIntyre AD, Kessel JW. Impact of acute care surgery to departmental productivity. J Trauma. 2011;71(4):1027–32 (discussion 1033–4).
Britt RC, Weirete LJ, Britt LD. Initial implementation of an acute care surgery model: implications for timeliness of care. J Am Coll Surg. 2009;209:421–4.
Quintin KM. An audit of the workload of an Acute Care Surgery Unit in a Tertiary Academic Hospital before and after the closure of a referring Community Hospital. Cape Town: University of Cape Town; 2015.
Committee to Develop the Reorganized Specialty of Trauma. Surgical critical care, and emergency surgery: acute care surgery: trauma, critical care, and emergency surgery. J Trauma. 2005;58:614–6.
Mathur S, Goo TT, Tan TJ, Tan KY, Mak KSW. Changing models of care for emergency surgical and trauma patients in Singapore. Singap Med J. 2016;57(6):282–6. https://doi.org/10.11622/smedj.2016101.
Mathur S, Lim WW, Goo TT. Emergency general surgery and trauma: Outcomes from the first consultant-led service in Singapore. Injury. 2018;49(1):130–4. https://doi.org/10.1016/j.injury.2017.09.002.
Warner BW, Kulick RM, Stoops MM, Mehta S, Stephan M, Kotagal UR. An evidenced-based clinical pathway for acute appendicitis decreases hospital duration and cost. J Pediatr Surg. 1998;33(9):1371–5.
Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland. Pathway for the Management of Acute Gallstone Diseases. Management of Acute Gallstone Diseases. (2015). http://www.augis.org/wp-content/uploads/2014/05/Acute-Gallstones-Pathway-Final-Sept-2015.pdf. Accessed 29 Apr 2018.
Huddart S, Mowat I, Sanusi S, Zuleika MA, Carvalho P, Bigham C, Scott MJP, Kirk-Bayley J, Dickinson M. Introduction of an integrated care pathway for emergency laparotomies saves lives. Anaesthesia. 2012;67:20. https://doi.org/10.1111/anae.12032.
Torrance ADW, Powell SL, Griffiths EA. Emergency surgery in the elderly: challenges and solutions. Open Access Emerg Med. 2015;7:55–68. https://doi.org/10.2147/OAEM.S68324(published online 2015 Sep 8)
Funding
There are no sources of funding in our study. There is no involvement of study sponsors in the study design; collection, analysis and interpretation of data; the writing of the manuscript; and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be submitted. There is no writing assistance to disclose.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no financial and personal relationships with other people or organisations that could inappropriately influence (bias) the work. Examples of potential conflicts of interest include employment, consultancies, stock ownership, honoraria, paid expert testimony, patent applications/registrations, and grants or other funding.
Rights and permissions
About this article
Cite this article
Goh, S.N.S., Lim, W.W., Rao, A.D. et al. Evolution of a Dedicated Emergency Surgery and Trauma (ESAT) unit over 3 years: sustained improved outcomes. Eur J Trauma Emerg Surg 46, 627–633 (2020). https://doi.org/10.1007/s00068-018-1049-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-018-1049-x