Abstract
Purpose
The purpose of this study was to compare clinical and radiographic outcomes of bipolar and monopolar radial head arthroplasty in treatment of radial head fracture at a mean follow-up of 6 years.
Methods
A retrospective multicentre cohort study of 30 patients treated for unreconstructable radial head fractures. Patients were treated either with a cemented bipolar or an uncemented monopolar radial head arthroplasty. All patients included were evaluated with patient-rated outcome questionnaire, physical examination, and radiographic evaluation at a mean of 6 years (range, 2–12 years) postoperatively.
Results
There was no statistical difference in QuickDASH between the bipolar or monopolar groups. The majority of patients had no to little pain during rest. Neither flexion nor extension of the injured arm was significantly affected by the type of prosthesis. None of the patients in the bipolar group had any secondary surgery at the time of follow-up. In the monopolar group, four patients required removal of the arthroplasty. Signs of ulnohumeral degenerative changes were seen in the majority of patients in both groups (55% in the monopolar group, 92% in the bipolar group).
Conclusion
In this retrospective cohort study comparing a bipolar and a monopolar radial head arthroplasty for treatment of radial head fractures, we found comparable functional outcome but more revision procedures in the monopolar group at a mean follow-up of 6 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
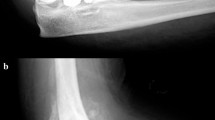
Fractures of the radial head are among the most common fractures of the elbow and represent one-third of all elbow fractures [1]. Radial head arthroplasty (RHA) is used for unreconstructable Mason III or IV fractures of the radial head and for chronic lesions including pseudarthrosis, malunion, post-traumatic osteoarthritis, and patients with symptomatic instability after radial head resection [1]. Unreconstructable radial head fractures treated with radial head resection can often result in progressive valgus instability, potential radial migration, secondary ulnocarpal injury and may be potentiated with the addition of altered elbow biomechanics resulting in degenerative osteoarthritis [2,3,4]. RHA is an alternative when osteosynthesis is futile and also allows for maintenance of the stability of the elbow joint [1, 5].Currently there is a broad range of radial head arthroplasties on the market. Implants can be classified according to polarity, either unipolar or bipolar, smooth-stemmed or in-growth and with or without an anatomical stem [Fig. 1].
There are few studies in the literature comparing prosthesis polarity [6, 7]. A systematic review, involving mostly observational studies of a single prosthetic design, showed satisfactory clinical outcomes [8]. There is limited information in the literature concerning the outcomes comparing the functional results of different designs of RHA, due to small sample sizes and the heterogenous injuries as indications for surgery. At present, it is still unknown whether a unipolar or bipolar prosthesis is preferable in the treatment of complex caput radii fractures. The aim of this study was to evaluate clinical and radiological differences between patients treated with either a monopolar or bipolar RHA.
Materials and methods
Study setting and patients
Study setting
This retrospective cohort study was performed between 2004 and 2014 at Sundsvall teaching hospital and Umeå University hospital, Sweden. Sundsvall teaching hospital provides medical care to a catchment area of approximately 160,000 inhabitants and Umeå University hospital is a level 3 trauma referral centre with a catchment area of 900,000 inhabitants.
Patients
The operative database was reviewed to identify all patients who were operated on between 2004 and 2014 with RHA for an acute or sequelae due to a caput radii fracture. Patients were treated either with an uncemented monopolar [Explor, Biomet, USA] or a bipolar modular cemented smooth-stemmed radial head implant [RHS, Tornier, France]. Exclusion criteria were patients with dementia, neurological deficit, patients who do not give their informed consent and ongoing drug abuse. 27 patients agreed out of 30 patients, to participate and gave their informed consent: 13 patients who received a bipolar prosthesis in Umeå and 14 patients in Sundsvall who received a monopolar prosthesis.
Data collection
Using the Swedish personal identification number, we collected data retrospectively by a combination of a search of our in-hospital medical records and follow-up visits. All patients were followedup until 2016 or until death by a search in the medical database with a minimum follow-up of 24 months. We collected patient data including demographic and baseline data, indication for radial head arthroplasty, age, sex, type of arthroplasty [unipolar or bipolar], date of surgery and secondary surgery. Preoperative radiographs were collected and used to classify radial head fractures according to the Mason-Johnston classification system [9].
Implant and surgery
Primary surgery was performed by two consultant orthopedic surgeons, one at Sundsvall teaching hospital and one at Umeå university hospital. Prophylactic antibiotics were administered 30 min preoperatively. Either a posterior or a lateral surgical approach to the elbow was performed. The radial head was exposed through a split in the extensor tendon origin or through the Kocher interval. The proximal radius was then prepared and inserted according to the implant product guide. Associated elbow injuries including fractures of the coronoid process, olecranon process, and ulnar shaft, and disruptions of the medial collateral ligament complex and distal triceps tendon were repaired at the preference of the treating surgeon. A long-arm [above elbow] splint was applied postoperatively and controlled motion exercises were initiated at 7 to 14 days.
Outcome variables
The primary outcome was QuickDASH, an abbreviated version of the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire [10], for evaluation of upper extremity disability. Secondary outcome measurements of elbow pain, at rest and during activity, were assessed by Visual Analogue Scales (VAS), measured with a 10-degree scale (0 represents no pain and 10 the worst pain imaginable) [11]. Range of motion (ROM) including flexion, extension, pronation and supination of the injured and uninjured elbow were obtained at follow-up visits using a goniometer. Secondary revision surgery was reported by patients at follow-up and by a search in the medical records.
Radiographic evaluation
Postoperative follow-up radiographs were taken with anteroposterior and lateral views with the forearm in neutral rotation. Radiographs were evaluated with regard to ulnohumeral degenerative changes and periprosthetic lucencies around the stem. Two independent observers evaluated clinical and radiological outcome of the entire cohort.
Statistical analysis
The Student’s t test was used for normally distributed data. The Chi square test was used to compare baseline data and ROM between groups. For the clinical outcome, QuickDASH, we used a generalized regression analysis to detect differences between groups and confounders such as the cause of injury, age and sex were included in the analysis. P values less than 0.05 were considered significant. SPSS version 22.0 was used for statistical analysis.
Ethics and registration
The study was conducted in accordance with the ethical principles of the Helsinki Declaration and was approved by the Ethics Committee of Umeå University (entry number 2016-508-31M).
The study was registered at clinicaltrials.gov (identifier: NCT03379935).
Results
Patient characteristics
The mean follow-up time was 6 [range 2–12] years after surgery. The mean age at surgery was similar between the groups (bipolar 52, range 20–60 years versus monopolar 45, range 24–69 years, p = 0.2). Low-energy trauma was the most common cause of injury in both groups. There was no difference in type of radial head fractures (p = 0.3). Most patients suffered type III and type IV injuries (Tables 1, 2, 3). One patient who had a Mason type II was initially treated non-surgically, but developed pseudarthrosis 1 year later. The patient was treated with monopolar RHA because of residual pain and instability.
Primary end-point
There was no statistical difference in QuickDASH between the bipolar and monopolar groups (Table Table 4). Using a generalized linear regression model, we did not find any statistical difference in Quick DASH between the two groups when adjusting QuickDASH for the following confounders: cause of injury, dominant or non-dominant hand and sex (Table 5).
Secondary end-points
Pain
There was no significant difference in pain between the groups (Table 4). The majority of patients had no or little pain during rest. When adjusting VAS at rest and VAS during activity to type of implant and confounders such as dominant or non-dominant hand and sex there were no statistical differences. VAS during rest was significantly higher in those suffering a high-energy trauma compared to low-energy trauma (p = 0.001) (Table 6).
Range of motion
Neither flexion nor extension of the injured arm was significantly affected by the type of prosthesis. The mean forearm pronation of unaffected and affected arm and supination of the injured arm in the monopolar group were significantly (p = 0.01) restricted (Table 6).
Secondary surgery
None of the patients in the bipolar group had any secondary surgery at the time of follow-up. In the monopolar group, four patients (29%) required removal of the arthroplasty. One patient had his implant removed after 9 years due to aseptic loosening. Of the remaining three patients, two had their prosthesis removed after 7 months and 17 months due to extension deficit and persistent pain and the third one after 3 months due to infection.
Radiographs
Periprosthetic radiolucency was seen in 25% of the bipolar group and 44% of the monopolar group (Fig. 2). In the bipolar group, two patients had a prosthesis that was considered loose after 8 and 7 years. However, these patients were not revised due to good functional outcome. Signs of ulnohumeral degenerative changes were seen in all patients except one patient in the bipolar group (92%) and in a majority in the monopolar group (55%).
Discussion
In this retrospective cohort study comparing a bipolar and a monopolar radial head arthroplasty for treatment of radial head fractures, we found comparable functional outcome but more revision procedures in the monopolar group at a mean of 6 years follow-up. Despite radiographic evidence of radiolucency around the stem, most patients had favourable clinical outcomes. None of the bipolar and 4 of the 14 monopolar implants had been revised at the time of final follow-up.
The patient-reported outcome scores (QuickDASH) in the current study are comparable with those reported in previous studies [12, 13]. We found no significant statistical difference between the two groups or when adjusting for type of trauma, sex and age. The arc of motion of the traumatized elbow was restricted in comparison to that of the unaffected elbow. The measured arc of motion is within the ranges described for both activities of daily living and contemporary tasks [14].
Reports during the past decade have indicated that monopolar implants are preferable to bipolar implants in patients with associated ligamentous injury due to superior radiocapitellar stability [15, 16]. In the present study, the selection of arthroplasty for each patient did not depend on the integrity of the soft tissues.
A literature search revealed two comparative clinical studies by Berschback et al. [6] with a mean follow-up of 33 months, and Rotini et al. [7] with a mean follow-up of 24 months; the number of patients per study were 27 and 30, respectively. Both Berschback et al. and Rotini et al. found acceptable clinical and radiological outcomes and no significant difference between implants in both short- and mid-term postoperative follow-up. These findings appear to contradict a biomechanical study suggesting that a monopolar prosthesis is superior to a bipolar prosthesis for elbow stability [17]. Berschback et al. [6] found a restricted pronation in the bipolar group that was statistically significant, possibly explained by the different measuring technique between observers. The majority of patients had no or little pain at rest. During activity, patients reported higher VAS scores in both groups.
Laumonerie et al. [18] recently presented a high rate of secondary surgery (41%) in a series of 70 patients with a bipolar prosthesis with a mean follow-up of 16 months; the prosthesis was removed in 18 patients and retained in 11 patients. Heijink et al. [8] present a lower incidence of revision in their systematic review, with a rate of revision ranging from 0 to 29% among studies, with an overall revision of 8%. In our study, four prostheses (14%) were removed. This revision rate agrees with previously published reports [8]. None of the patients in the bipolar group had secondary surgery. In a 4-year follow-up case series of 37 patients with a press-fit monopolar implant, Flinkkilä et al. [19] reported an implant removal rate of 24%. In a study of a cemented bipolar implant at 8-year follow-up, 37 patients had evidence of progressive osteolysis but none had required removal of the implant [20]. Most patients had minimal pain until the osteolysis became severe; however, the authors advised caution in using cemented bipolar implants.
Generalized arthritic changes were commonly observed. Signs of ulnohumeral degenerative changes were seen in all patients except one in the bipolar group (92%) and in a majority in the monopolar group (55%). These high rates of degenerative changes are in concordance with previous reports in the literature [6, 12, 18]. The interobserver variations may contribute to the differences in the incidence of degenerative changes reported in the literature. Progression of degenerative changes in the elbow is likely to develop in relation to the original injury and the altered radiocapitellar biomechanics [21, 22]. Over lengthening of the radiocapitellar joint has been linked to early development of degenerative changes, capitellar erosions, pain and loss of elbow flexion [23].
Radiolucency and osteolysis around the implants is a common finding, the incidence ranging widely in the literature [8, 18,19,20]. We found a relatively low incidence of radiolucency. One patient in the monopolar group was revised due to loosening. Two patients in the bipolar group had asymptomatic signs of loosening but were not revised due to good functional outcome. As reported in the review by Heijink et al. [8] most cases of the commonly encountered radiolucency and osteolysis seem to be asymptomatic. There is insufficient evidence in the literature to determine if radiolucency affects long-term outcome.
We found a much lower rate of arthrosis in the monopolar group (55%) in comparison to the bipolar group (92%) but a higher rate of aseptic loosening (44%) in the monopolar group (55%) in comparison to the bipolar group (92%). One explanation as to why the bipolar group had lower radiolucency is the freedom of movement of the articulating component of the bipolar prosthesis on the intramedullary component. This may reduce stress at the implant-bone and bone–cement interfaces during forearm rotations [8]. High arthrosis in the bipolar group depends on more severe type of injury which usually are operated by a tertiary centre and also longer time to surgery which is also shown in the literature [3, 6, 7].
Failure of monopolar prosthetic radial heads can theoretically occur by a number of mechanisms. Ingrowth of a cementless radial head stem relies on minimising micromotion between the prosthesis and bone. Excess micromotion impairs osseous interdigitating and results in fibrous tissue formation which can be the explanation for aseptic loosening in the monopolar group [15].
The strengths of our study include a consecutive series of patients with radial head fracture treated with two different implants. The Swedish personal identification number enabled us to find complications and reoperations to increase the completeness of data.
The limitations of this study relate to its retrospective design and sample size. The small sample size did not allow us to find a statistically significant difference in outcome between the different designs. However, we had a similar sample size to the other two comparative studies [9, 10].
Conclusion
In this retrospective cohort study comparing a bipolar and a monopolar RHA for treatment of radial head fractures, we found comparable functional outcome but more revision procedures in the monopolar group at a mean follow-up of 6 years. Further studies with a larger sample size, long-term follow-up and randomized clinical trials are necessary to assess clinical and radiographic differences between implants.
References
Ring D. Displaced, unstable fractures of the radial head: fixation vs. replacement—what is the evidence? Injury. 2008;39(12):1329–37. https://doi.org/10.1016/j.injury.2008.04.011.
Herbertsson P, Josefsson PO, Hasserius R, Besjakov J, Nyqvist F, Karlsson MK. Fractures of the radial head and neck treated with radial head excision. J Bone Joint Surg Am. 2004;86-A(9):1925–30.
Ikeda M, Sugiyama K, Kang C, Takagaki T, Oka Y. Comminuted fractures of the radial head. Comparison of resection and internal fixation. J Bone Joint Surg Am. 2005;87(1):76–84.
Schiffern A, Bettwieser SP, Porucznik CA, Crim JR, Tashjian RZ. Proximal radial drift following radial head resection. J Shoulder Elbow Surg. 2011;20(3):426–33. https://doi.org/10.1016/j.jse.2010.11.008. (Epub 2011 Feb 15)
Moro JK1, Werier J, MacDermid JC, Patterson SD, King GJ. Arthroplasty with a metal radial head for unreconstructible fractures of the radial head. J Bone Joint Surg Am. 2011;83-A(8):1201–11.
Berschback JC1, Lynch TS, Kalainov DM, Wysocki RW, Merk BR, Cohen MS. Clinical and radiographic comparisons of two different radial head implant designs. J Shoulder Elbow Surg. 2013;22(8):1108–20. https://doi.org/10.1016/j.jse.2013.02.011.
Rotini R, Marinelli A, Guerra E, Bettelli G, Cavaciocchi M. Radial head replacement with unipolar and bipolar SBi system: a clinical and radiographic analysis after a 2-year mean follow-up. Musculoskelet Surg. 2012;96(Suppl 1):69–79. https://doi.org/10.1007/s12306-012-0198-z. (Epub 2012 Apr 18).
Heijink A, Kodde IF, Mulder PG, Veltman ES, Kaas L, van den Bekerom MP, Eygendaal D. Radial head arthroplasty: a systematic review. JBJS Rev. 2016;4(10): 01874474–201610000. https://doi.org/10.2106/JBJS.RVW.15.00095.
Johnston GW. A follow-up of one hundred cases of fracture of the head of the radius with a review of the literature. Ulster Med J. 1962;31:51–6.
Beaton DE, Wright JG, Katz JN, Upper Extremity Collaborative Group. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87(5):1038–46.
Scott J, Huskisson EC. Graphic representation of pain. Pain. 1976;2(2):175–84.
Marsh JP, Grewal R, Faber KJ, Drosdowech DS, Athwal GS, King GJ. Radial head fractures treated with modular metallic radial head replacement: outcomes at a mean follow-up of 8 years. J Bone Joint Surg Am. 2016;98(7):527–35. https://doi.org/10.2106/JBJS.15.00128.
Moro JK, Werier J, MacDermid JC, Patterson SD, King GJ. Arthroplasty with a metal radial head for unreconstructable fractures of the radial head. J Bone Joint Surg Am. 2001;83-A(8):1201–11.
Sardelli M, Tashjian RZ, MacWilliams BA. (2011) Functional elbow range of motion for contemporary tasks. Bone J Joint Surg Am 93(5):471–7. https://doi.org/10.2106/JBJS.I.01633.
Moon JG, Berglund LJ, Zachary D, An KN, O’Driscoll SW. Radiocapitellar joint stability with bipolar versus monopolar radial head prostheses. J Shoulder Elbow Surg. 2009;18(5):779–84. https://doi.org/10.1016/j.jse.2009.02.
Sahu D, Holmes DM, Fitzsimmons JS, Thoreson AR, Berglund LJ, An KN, O’Driscoll SW. Influence of radial head prosthetic design on radiocapitellar joint contact mechanics. J Shoulder Elbow Surg. 2014;23(4):456–62. https://doi.org/10.1016/j.jse.2013.11.028.
Chanlalit C, Shukla DR, Fitzsimmons JS, Thoreson AR, An KN, O’Driscoll SW. Radiocapitellar stability: the effect of soft tissue integrity on bipolar versus monopolar radial head prostheses. J Shoulder Elbow Surg. 2011;20(2):219–25. https://doi.org/10.1016/j.jse.2010.10.033.
Laumonerie P, Reina N, Ancelin D, Delclaux S, Tibbo ME, Bonnevialle N, Mansat P. (2017) Mid-term outcomes of 77 modular radial head prostheses. Bone Joint J 99-B(9):1197–203. https://doi.org/10.1302/0301620X.99B9.BJJ-2016-1043.R2.
Flinkkilä T, Kaisto T, Sirniö K, Hyvönen P, Leppilahti J. Short- to mid-term results of metallic press-fit radial head arthroplasty in unstable injuries of the elbow. J Bone Joint Surg Br. 2012;94(6):805–10. https://doi.org/10.1302/0301-620X.94B6.28176.
Popovic N, Lemaire R, Georis P, Gillet P. Midterm results with a bipolar radial head prosthesis: radiographic evidence of loosening at the bone-cement interface. J Bone Joint Surg Am. 2007;89(11):2469–76.
Burkhart KJ1, Mattyasovszky SG, Runkel M, Schwarz C, Küchle R, Hessmann MH, Rommens PM, Müller LP. Mid- to long-term results after bipolar radial head arthroplasty. J Shoulder Elbow Surg. 2010;19(7):965–72. https://doi.org/10.1016/j.jse.2010.05.022.
Yian E, Steens W, Lingenfelter E, Schneeberger AG. Malpositioning of radial head prostheses: an in vitro study. J Shoulder Elbow Surg. 2008;17(4):663–70. https://doi.org/10.1016/j.jse.2007.12.008. (Epub 2008 Apr 18).
Frank SG, Grewal R, Johnson J, Faber KJ, King GJ, Athwal GS. Determination of correct implant size in radial head arthroplasty to avoid overlengthening. J Bone Joint Surg Am. 2009;91(7):1738–46. https://doi.org/10.2106/JBJS.H.01161.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Sebastian Mukka, Pontus Sjöholm, Nikolaos Perisynakis, Per Wahlström, Hans Rahme and Bakir Kadum declare that they have no conflict of interest.
Ethical standards
The study was conducted in accordance with the ethical principles of the Helsinki Declaration and was approved by the Ethics Committee of Umeå University (Entry Number 2016-508-31M). The study was registered at clinicaltrials.gov (Identifier: NCT03379935).
Rights and permissions
About this article
Cite this article
Mukka, S., Sjöholm, P., Perisynakis, N. et al. Radial head arthroplasty for radial head fractures: a clinical and radiological comparison of monopolar and bipolar radial head arthroplasty at a mean follow-up of 6 years. Eur J Trauma Emerg Surg 46, 565–572 (2020). https://doi.org/10.1007/s00068-018-1042-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-018-1042-4