Abstract
Purpose
Severe necrotizing soft-tissue infections (NSTIs) require immediate early surgical treatment to avoid adverse outcomes. This study aims to determine the impact of early surgery and comorbid conditions on the outcomes of NSTIs.
Methods
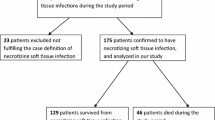
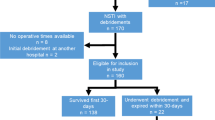
A retrospective cohort study was performed on all subjects presenting with NSTI at an academic medical center between 2005 and 2016. Patients were identified based on ICD codes. Those under the age of 18 or with intraoperative findings not consistent with NSTI diagnosis were excluded.
Results
There were 115 patients with a confirmed diagnosis of NSTI with a mean age of 55 ± 18 years; 41% were females and 55% were diabetics. Thirty percent of patients underwent early surgery (< 6 h). There were no significant differences between groups in baseline characteristics. The late group (≥ 6 h) had prolonged hospital stay (38 vs. 23 days, p < 0.008) in comparison to the early group (< 6 h). With every 1 h delay in time to surgery, there is a 0.268 day increase in length of stay, adjusted for these other variables: alcohol abuse, number of debridements, peripheral vascular disease, previous infection and clinical necrosis. Mortality was 16.5%. Multivariable analysis revealed that alcohol abuse, peripheral vascular disease, diabetes, obesity, hypothyroidism, and presence of COPD were associated with an increase in mortality.
Conclusions
Early surgical intervention in patients with severe necrotizing soft-tissue infections reduces length of hospital stay. Presence of comorbid conditions such as alcohol abuse, peripheral vascular disease, diabetes, obesity and hypothyroidism were associated with increased mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Necrotizing soft-tissue infection (NSTI) is associated with significant mortality and morbidity if surgical debridement is not performed adequately and in a timely fashion [1]. Based on a Texas population database of 12,172 necrotizing fasciitis (NF) hospitalizations between 2001 and 2010, Oud and Watkins [2] estimated the incidence of NF hospitalizations to be 6.9 per 100,000 patient-years. Moreover, the annual frequency of deaths in the US due to NF is approximately 1000 [3]. Microbiological classification of NSTIs is usually according to three or four types based on organism and severity of infection is used to guide management [4, 5].
Early diagnosis and intervention of NF are considered critical to preventing severe adverse outcomes. The time to initiation of first surgical intervention has been found to be a predictor of ICU and length of hospital stay [5], as well as mortality [6, 7]. Identification and management of factors that predict adverse outcomes among patients admitted for NSTI may improve the hospital course.
A broad range of retrospective cohort studies published in the past 15 years have reported mortality rates among NSTI patients between 4.9 and 48.8% [2, 5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44]. Moreover, there has been considerable variation in the independent predictors of mortality identified by studies with 50 or more patients. We found 13 studies that observed age as a significant independent predictor [6, 9, 12, 13, 17, 19, 23, 25, 26, 28, 31, 35, 45]. Seven studies showed that renal dysfunction was a significant predictor in multivariable analyses [9, 10, 12, 17, 18, 24, 26]. Other variables found to be independent predictors in isolated studies were generally not confirmed by other studies [7, 15, 25].
Timing from presentation and diagnosis to surgery is the most important modifiable element in the outcomes of patients with NSTI. However, published reports are inconsistent with regard to whether time to surgical intervention is a significant independent predictor. A large French nationwide database study [6] found that day of surgery was a significant independent predictor of mortality. A study by Wong et al. [7] of 89 NSTI patients found delay from admission to surgery to predict adverse outcomes. Four studies also examined time to intervention but did not find it to be a significant predictor of mortality on multivariable modeling, mostly due to small sample size [5, 19, 20, 28]. A recent study from our group [5] reported that time to surgery was a predictor of increased length of ICU and hospital stay, whereas studies by Holena et al. [6] and Wong et al. [7] found time to surgery to be an independent predictor of mortality. Other studies have not confirmed these findings. The objectives of this study were to determine whether time to surgical intervention and other factors are predictors of mortality and length of hospital stay.
Methods
A retrospective cohort study was carried out in an academic tertiary/quaternary medical center with a Level 1 Trauma Center. The study was granted ethical approval according to the Westchester Medical Center Heath Network research committee and New York Medical College Institutional Review Board (IRB), project number 12018. Patients were identified through ICD codes for NSTI (ICD-9 728.86; ICD-10 M72.6), gas gangrene (ICD-9, 040.0; ICD-10 N49.3), and Fournier gangrene (ICD-9 608.83; ICD-10, A48.0). Those under the age of 18 or with intraoperative findings not consistent with NSTI diagnosis were excluded. Independent variables included patient demographics, such as age, sex, and race; clinical findings; anatomical location of NSTI; comorbidities; timing of admission to surgery; number of debridements; and laboratory results such as blood glucose, hemoglobin, and creatinine prior to debridement. Dependent variables were length of stay in the hospital, days to mortality for patients who died, and overall mortality. All data were de-identified prior to analysis and abstracted from the medical records into Microsoft Excel. Data were stored on password-protected hospital computers.
Statistical analysis
Descriptive analyses were conducted and data are presented as proportion, mean (± standard deviation), median, and range whenever applicable. Student’s t test was performed to compare continuous variables and Pearson’s Chi-squared (χ2) test was used for categorical variables. The Pearson correlation coefficient was used to assess correlations between predictor and outcome variables. Time to surgery was calculated based on admission and/or initial diagnosis to the time of first surgery. This variable was used to divide patients into two subgroups based on our previous study [5]. Group 1 included patients who had time to surgery < 6 h, whereas group 2 included patients who had time to surgery ≥ 6 h. Baseline characteristics and outcomes were compared for these two groups. Univariable analyses were conducted for independent variables on outcomes. Candidate variables to enter into multivariable models were selected based on univariable p values < 0.2. Multivariable analyses were conducted using the backward elimination method beginning with all candidate variables and eliminating the variable with the highest p value, rerunning the model and repeating the procedure until the final model included only predictors that were significant at the 0.05 level. Linear regression was used for the continuous outcome of hospital length of stay and logistic regression was used for the binary outcome of mortality. Analyses were performed using the SPSS version 24 (IBM, Armonk NY).
Results
There were 115 patients identified during the study period of 1/1/2005–12/31/2016 (59.1% were male and 40.9% were female). The overall average age of patients was 55.15 years (SD 17.90). Sixty-five percent of patients were white, 15% were black, and 11% were Hispanic. The average BMI was 30.45 (SD 9.21). The average time to intervention (from diagnosis to surgery) was 27.49 h with a range of 0.05–141.07. The average hospital length of stay was 33.26 (SD 39.77), median 24 and range 4–370 days. The average number of debridement was 3.261 (SD 2.44), median 3.0 and range 1–14. The majority of patients (65.21%) had time to intervention of less than 24 h. Diabetes mellitus was reported in 54.8%, while 54.8% had hypertension and 21.7% had hyperlipidemia. The majority of patients had lower extremity NSTI (52.2%) followed by 24.3% with Fournier gangrene.
Table 1 shows comparison of baseline characteristics between early and late intervention groups. There were no significant differences between groups in baseline characteristics; however, there was a significant difference between the two groups in hospital length of stay (t = − 2.696, p < 0.008). The early intervention group had non-significantly higher percentages of erythema (93.5 vs. 85.1%), induration (20.7 vs. 17.6%), tachypnea (31.0 vs. 14.9%) and foul smell (31.0 vs. 25.7%). Fournier’s gangrene was also more frequent in the early group (32.4 vs. 21.0%).
Table 2 presents comparison of laboratory test values for the two different groups. There were no significant differences between groups for white blood cell count, platelets, sodium, blood glucose, lactate, pH, or albumin; however, there were significant differences between groups on creatinine (p = 0.016) and blood urea nitrogen, (p = 0.013), showing higher values in the late intervention group. Non-significant differences were shown between groups in comorbidities (Table 3) except for renal insufficiency/failure, lower in the early intervention group vs. late (3.0 vs 23.7%, χ2 = 6.82, p = 0.011).
Length of hospital stay
Significant univariable predictors of length of hospital stay included alcohol consumption, number of debridements, peripheral vascular disease, previous infection, time to surgery, renal insufficiency/failure, clinical necrosis, and white blood cell count (Table 4). Having a history of chronic alcohol abuse was associated with increased hospital length of stay by 49.904 added days (β = 49.904, 95% CI 26.359–73.448, p < 0.001). Having peripheral vascular disease was associated with increased length of hospital stay by 33.298 added days (β = 33.298, 95% CI 11.666–54.929, p < 0.01). History of previous infection was associated with increased length of hospital stay by 25.790 added days (β = 25.790, 95% CI 5.916–45.664, p < 0.05). Every additional hour until surgery was associated with 0.273 added days in the hospital (β = 0.273, 95% CI 0.048–0.499, p < 0.05).
Mortality
Nineteen (16.5%) patients died. The median day to death was 34, with a range of 1–371. Significant univariable predictors of mortality included renal insufficiency/failure, hypothyroidism, blood glucose, location of NSTI on the torso, white blood cell count, depression, and clinical tenderness (Table 5). Time to surgery (in hours) was not a statistically significant predictor; the odds ratio (OR) was 1.004 (95% CI 0.989–1.018). Hypothyroidism had the strongest impact among binary variables and was associated with an increase in the odds of mortality by 4.914 (OR 4.914, 95% CI 1.175–20.556, p < 0.05). Renal insufficiency/failure was associated with an increase in the odds of mortality by 4.189 (OR 4.189, 95% CI 1.359–12.911, p < 0.05). Having NSTI on the torso was associated with an increased odds of mortality by 3.566 (OR 3.566, 95% CI 1.126–11.301, p < 0.05).
Multivariable analysis
The final model of independent significant predictors for length of hospital stay included history of alcohol abuse, number of debridement, peripheral vascular disease, previous infection, time to surgery, and clinical necrosis. The strongest binary predictor of length of hospital stay, while taking into account the other predictors in the model, was alcohol (β = 30.098, 95% CI 4.685–55.510, p < 0.05). Peripheral vascular disease was associated with an increased length of stay by 29.084 days (β = 29.084, 95% CI 8.324–49.844, p < 0.01) (Table 4). For mortality, the final model of independent significant predictors included peripheral vascular disease, white blood cell count, blood glucose, obesity, hypothyroidism, and COPD. Peripheral vascular disease was a strong binary predictor of mortality while taking into account the other variables in the model (OR 20.78, 95% CI 2.582–167.239, p < 0.01). Hypothyroidism is associated with an increase in the odds of mortality by 13.292 (OR 13.292, 95% CI 1.348–131.067, p < 0.05). COPD increased the odds by 12.048 (OR 12.048, 95% CI 1.025–141.632, p < 0.05) (Table 5).
Discussion
A necrotizing soft-tissue infection is a surgical emergency and should be treated as such by an experienced surgical team immediately upon diagnosis. Our study focused on whether time to surgery and presence of comorbid conditions were important predictors of adverse outcomes among NSTI patients. We found that time to surgery is a significant independent predictor of length of hospital stay. With every 1 h delay in time to surgery, there is a 0.266 day increase in length of stay, adjusted for other variables retained in the multivariable model. Other significant predictors on multivariable analysis of hospital length of stay included: history of alcohol abuse, peripheral vascular disease, previous infection, and clinical necrosis. We also found that the odds of mortality non-significantly increase slightly with longer times to surgery. Significant independent predictors of mortality included peripheral vascular disease, hypothyroidism, COPD, obesity, blood glucose and white blood cell count.
Studies of NSTI conducted previously have addressed a variety of potential predictive factors. A paper by Jabbour et al. [25] assembled data from 331 patients identified across 14 years. Age and Sequential Organ Failure Assessment (SOFA) score were found to be significant independent predictors of morality on multivariable analysis. El-Menyar et al. [15] included 294 NSTI patients and focused on LRINEC score, dividing patients into those with scores < 6 and ≥ 6. In univariable analyses, age and LRINEC score were significant predictors of mortality and septic shock. Al-Thani et al. [8] measured inflammation biomarkers in 62 NSTI patients as tools for discriminating between patients with and without septic shock. They found that procalcitonin had a significantly favorable area under the receiver operating characteristic (ROC) curve, while C-reactive protein did not. Shaikh et al. [37] addressed patterns of patient factors and outcomes in males vs. females. Our group’s first examination of time to initiation of debridement occurred at the University of Arizona. Hadeed et al. [5] studied 87 NSTI patients, finding that time to surgical intervention was a significant univariable predictor of both ICU length of stay and hospital length of stay.
Our present findings on time to surgery as an independent predictor of hospital length of stay agree with our previous study [5] and that of Holena et al. [6] We have not found other large cohort studies that have addressed time to surgery as a potential predictor of hospital length of stay.
Our study and four others [5, 19, 20, 28] have failed to find time to surgery to be significant on multivariable modeling to define the predictors of mortality. We believe that the retrospective nature of the studies and small sample sizes are responsible for these results. The odds ratio of 1.004 observed in our study for time to surgery predicting mortality suggests a slight non-significant increase in odds with longer time to surgery that could be detected as significant by a larger study. Details are missing from the other four studies on the magnitude of the association between time to surgery and mortality and the width of confidence intervals.
Time to surgery is a complex variable with multiple components defying straightforward interpretation. In our study, time to surgery was generally defined as the interval from presentation at the ED to the beginning of first debridement. Other intervals include the point when symptoms arise to the point of presentation, the point of presentation to being seen by the surgeon, the point of being seen to the decision to perform surgery, and the point of the decision to when surgery is performed. The last three intervals are components of time to surgery as we measured it in our study, but we did not estimate them separately. Time from symptom onset to presentation could reflect various factors such as tolerance for discomfort, how serious the patient considered symptoms to be, insurance status, mobility, and accessibility to medical facilities. Time from presentation to first debridement could also reflect multiple factors including: the degree to which clinicians at the hospital are familiar with diagnosis of NSTI or guidelines for managing patients with suspicious findings for NSTI; clinician uncertainty of whether the patient fits the diagnosis, independent of experience/knowledge; efficiency of management pathways at a facility and availability of a surgeon/operating room to perform the debridement. The impact of inter-hospital transfer and ED boarding stay were found to be associated with increased mortality [6, 46]. These two time factors were not addressed in our study.
Severity of infection may not have a simple positive correlation with time to surgery. While some patients with severe infections on presentation will be immediately recognized as NSTI and undergo surgery quickly, other difficult-to-diagnose cases may not be recognized as severe until later and would undergo delayed surgery. Thus, the critical factors may not be time to surgery but rather time to diagnosis and time to decision to perform surgery.
A very recent state-of-the-art review outlines the complexities of etiology, clinical presentations, treatment and the effect of delays in surgical intervention on mortality [1]. Understanding the role of comorbid conditions, and the need for surgical treatment in the timeliest manner should be the modus operandi of these complex and deadly infections.
Clinicians would benefit from risk scoring systems that permit estimation of the probability of adverse outcomes given the characteristics of specific patients. Table 6 shows mortality scoring systems derived from our study and three other reports [17, 19, 44]. Three used multivariable logistic regression and one used classification and regression tree (CART) analysis. Our study and the Faraklas study reported how well scoring systems discriminated between survival and death using area under the receiver operating characteristic curve (AUC). Faraklas et al. [17] used data from 1392 patients extracted from NSQIP files between 2005 and 2010. Their validated logistic model included age, functional dependence, dialysis, ASA class, emergent surgery, septic shock and platelet count, achieving a development phase AUC of 0.85. Our mortality model included peripheral vascular disease, white blood cell count, blood glucose, obesity, hypothyroidism and COPD, yielding an AUC of 0.904. Our study compares favorably with the Faraklas study on discrimination.
Our study has a number of limitations such as retrospective design with small sample size. A larger sample would have permitted addressing potential outcome differences by subgroup factors such as site of infection and pathogen. Time to surgery in this study was calculated based on available information on admission and/or initial diagnosis to time of first surgery. More precise measurement of time would have been desirable. Moreover, variables such as time of symptom onset, time of diagnosis and time from decision to perform surgery to actual surgery itself were not recorded. Furthermore, the subspecialty of the operating surgeons was not recorded. Analysis of length of hospital stay can be problematic, because it can be influenced by “non-medical” factors that can prolong stay.
We conclude that time to surgery is a significant independent predictor of length of hospital stay. Given conflicting findings on whether time to surgery is an independent predictor of mortality and length of hospital stay in NSTI patients, prospective studies should be conducted in the future to collect detailed measurements of several intervals between time of symptom onset and time of surgery. In patients with NSTIs and with other comorbid conditions surgical treatment should be performed as soon as possible, best within the first 6 h of presentation. This time should be used for aggressive resuscitation. Each patient with NSTI should be studied prospectively and rigorous multivariable statistical procedures should be carried out to help identify factors that are significant independent predictors of adverse outcomes in NSTI patients.
References
Stevens DL, Bryant AE. Necrotizing soft-tissue infections. N Engl J Med. 2017;377(23):2253–65. https://doi.org/10.1056/NEJMra1600673.
Oud L, Watkins P. Contemporary trends of the epidemiology, clinical characteristics, and resource utilization of necrotizing fasciitis in Texas: a population-based cohort study. Crit Care Res Pract. 2015;2015:618067. https://doi.org/10.1155/2015/618067.
Arif N, Yousfi S, Vinnard C. Deaths from necrotizing fasciitis in the United States, 2003–2013. Epidemiol Infect. 2016;144(6):1338–44. https://doi.org/10.1017/S0950268815002745.
Bonne SL, Kadri SS. Evaluation and management of necrotizing soft tissue infections. Infect Dis Clin N Am. 2017;31(3):497–511. https://doi.org/10.1016/j.idc.2017.05.011.
Hadeed GJ, Smith J, O’Keeffe T, et al. Early surgical intervention and its impact on patients presenting with necrotizing soft tissue infections: a single academic center experience. J Emerg Trauma Shock. 2016;9(1):22–7. https://doi.org/10.4103/0974-2700.173868.
Holena DN, Mills AM, Carr BG, et al. Transfer status: a risk factor for mortality in patients with necrotizing fasciitis. Surgery. 2011;150(3):363–70. https://doi.org/10.1016/j.surg.2011.06.005.
Wong C-H, Chang H-C, Pasupathy S, Khin L-W, Tan J-L, Low C-O. Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. J Bone Jt Surg Am. 2003;85-A(8):1454–60.
Al-Thani H, El-Menyar A, Shaikh N, et al. Risk stratification of necrotizing fasciitis based on the initial procalcitonin concentration: a single center observational study. Surg Infect. 2015;16(6):806–12. https://doi.org/10.1089/sur.2014.249.
Anaya DA, Bulger EM, Kwon YS, Kao LS, Evans H, Nathens AB. Predicting death in necrotizing soft tissue infections: a clinical score. Surg Infect. 2009;10(6):517–22. https://doi.org/10.1089/sur.2008.112.
Anaya DA, McMahon K, Nathens AB, Sullivan SR, Foy H, Bulger E. Predictors of mortality and limb loss in necrotizing soft tissue infections. Arch Surg Chic Ill 1960. 2005;140(2):151–7. https://doi.org/10.1001/archsurg.140.2.151. discussion 158.
Bair M-J, Chi H, Wang W-S, Hsiao Y-C, Chiang R-A, Chang K-Y. Necrotizing fasciitis in southeast Taiwan: clinical features, microbiology, and prognosis. Int J Infect Dis IJID Off Publ Int Soc Infect Dis. 2009;13(2):255–60. https://doi.org/10.1016/j.ijid.2008.04.015.
Childers BJ, Potyondy LD, Nachreiner R, et al. Necrotizing fasciitis: a fourteen-year retrospective study of 163 consecutive patients. Am Surg. 2002;68(2):109–16.
Dworkin MS, Westercamp MD, Park L, McIntyre A. The epidemiology of necrotizing fasciitis including factors associated with death and amputation. Epidemiol Infect. 2009;137(11):1609–14. https://doi.org/10.1017/S0950268809002532.
Eggerstedt M, Gamelli RL, Mosier MJ. The care of necrotizing soft-tissue infections: patterns of definitive intervention at a large referral center. J Burn Care Res Off Publ Am Burn Assoc. 2015;36(1):105–10. https://doi.org/10.1097/BCR.0000000000000203.
El-Menyar A, Asim M, Mudali IN, Mekkodathil A, Latifi R, Al-Thani H. The laboratory risk indicator for necrotizing fasciitis (LRINEC) scoring: the diagnostic and potential prognostic role. Scand J Trauma Resusc Emerg Med. 2017;25(1):28. https://doi.org/10.1186/s13049-017-0359-z.
Ertl CW, Carpp NC, Johnson J, Burke L. Evaluation of factors associated with death in patients with necrotizing fasciitis of the abdominal wall. Surg Infect. 2017;18(2):176–80. https://doi.org/10.1089/sur.2016.167.
Faraklas I, Stoddard GJ, Neumayer LA, Cochran A. Development and validation of a necrotizing soft-tissue infection mortality risk calculator using NSQIP. J Am Coll Surg. 2013;217(1):153–60.e3. https://doi.org/10.1016/j.jamcollsurg.2013.02.029. discussion 160–161.
Frazee BW, Fee C, Lynn J, et al. Community-acquired necrotizing soft tissue infections: a review of 122 cases presenting to a single emergency department over 12 years. J Emerg Med. 2008;34(2):139–46. https://doi.org/10.1016/j.jemermed.2007.03.041.
Golger A, Ching S, Goldsmith CH, Pennie RA, Bain JR. Mortality in patients with necrotizing fasciitis. Plast Reconstr Surg. 2007;119(6):1803–7. https://doi.org/10.1097/01.prs.0000259040.71478.27.
Gunter OL, Guillamondegui OD, May AK, Diaz JJ. Outcome of necrotizing skin and soft tissue infections. Surg Infect. 2008;9(4):443–50. https://doi.org/10.1089/sur.2007.053.
Hansen MB. Biomarkers of necrotising soft tissue infections aspects of the innate immune response. Dan Med J. 2017;64(7):1–17.
Hansen MB, Rasmussen LS, Garred P, Bidstrup D, Madsen MB, Hyldegaard O. Pentraxin-3 as a marker of disease severity and risk of death in patients with necrotizing soft tissue infections: a nationwide, prospective, observational study. Crit Care Lond Engl. 2016;20:40. https://doi.org/10.1186/s13054-016-1210-z.
Hua C, Sbidian E, Hemery F, et al. Prognostic factors in necrotizing soft-tissue infections (NSTI): a cohort study. J Am Acad Dermatol. 2015;73(6):1006.e8–12.e8. https://doi.org/10.1016/j.jaad.2015.08.054.
Huang K-F, Hung M-H, Lin Y-S, et al. Independent predictors of mortality for necrotizing fasciitis: a retrospective analysis in a single institution. J Trauma. 2011;71(2):467–73. https://doi.org/10.1097/TA.0b013e318220d7fa (discussion 473).
Jabbour G, El-Menyar A, Peralta R, et al. Pattern and predictors of mortality in necrotizing fasciitis patients in a single tertiary hospital. World J Emerg Surg WJES. 2016;11:40. https://doi.org/10.1186/s13017-016-0097-y.
Kao LS, Lew DF, Arab SN, et al. Local variations in the epidemiology, microbiology, and outcome of necrotizing soft-tissue infections: a multicenter study. Am J Surg. 2011;202(2):139–45. https://doi.org/10.1016/j.amjsurg.2010.07.041.
Keeley J, Kaji A, Kim D, et al. Predictors of mortality in necrotizing soft tissue infection. Am Surg. 2014;80(10):989–93.
Keung EZ, Liu X, Nuzhad A, Adams C, Ashley SW, Askari R. Immunocompromised status in patients with necrotizing soft-tissue infection. JAMA Surg. 2013;148(5):419–26. https://doi.org/10.1001/jamasurg.2013.173.
Krieg A, Dizdar L, Verde PE, Knoefel WT. Predictors of mortality for necrotizing soft-tissue infections: a retrospective analysis of 64 cases. Langenbecks Arch Surg. 2014;399(3):333–41. https://doi.org/10.1007/s00423-014-1162-1.
Moore SA, Levy BH, Prematilake C, Dissanaike S. The prediction predicament: rethinking necrotizing soft tissue infections mortality. Surg Infect. 2015;16(6):813–21. https://doi.org/10.1089/sur.2015.002.
Mulla ZD, Gibbs SG, Aronoff DM. Correlates of length of stay, cost of care, and mortality among patients hospitalized for necrotizing fasciitis. Epidemiol Infect. 2007;135(5):868–76. https://doi.org/10.1017/S0950268806007448.
Nisbet M, Ansell G, Lang S, Taylor S, Dzendrowskyj P, Holland D. Necrotizing fasciitis: review of 82 cases in South Auckland. Intern Med J. 2011;41(7):543–8. https://doi.org/10.1111/j.1445-5994.2009.02137.x.
Pakula AM, Kapadia R, Freeman B, Skinner RA. A 3-year experience with necrotizing fasciitis: favorable outcomes despite operative delays in a busy acute care hospital. Am Surg. 2012;78(10):1059–62.
Proud D, Bruscino Raiola F, Holden D, Paul E, Capstick R, Khoo A. Are we getting necrotizing soft tissue infections right? A 10-year review. ANZ J Surg. 2014;84(6):468–72. https://doi.org/10.1111/ans.12412.
Psoinos CM, Flahive JM, Shaw JJ, et al. Contemporary trends in necrotizing soft-tissue infections in the United States. Surgery. 2013;153(6):819–27. https://doi.org/10.1016/j.surg.2012.11.026.
Schwartz S, Kightlinger E, de Virgilio C, et al. Predictors of mortality and limb loss in necrotizing soft tissue infections. Am Surg. 2013;79(10):1102–5.
Shaikh N, El-Menyar A, Mudali IN, Tabeb A, Al-Thani H. Clinical presentations and outcomes of necrotizing fasciitis in males and females over a 13-year period. Ann Med Surg 2012. 2015;4(4):355–60. https://doi.org/10.1016/j.amsu.2015.09.005.
Tan JH, Koh BTH, Hong CC, et al. A comparison of necrotising fasciitis in diabetics and non-diabetics: a review of 127 patients. Bone Jt J. 2016;98-B(11):1563–8. https://doi.org/10.1302/0301-620X.98B11.37526.
Tsai Y-H, Huang K-C, Shen S-H, Hsu W-H, Peng K-T, Huang T-J. Microbiology and surgical indicators of necrotizing fasciitis in a tertiary hospital of southwest Taiwan. Int J Infect Dis IJID Off Publ Int Soc Infect Dis. 2012;16(3):e159–65. https://doi.org/10.1016/j.ijid.2011.11.001.
Tunovic E, Gawaziuk J, Bzura T, Embil J, Esmail A, Logsetty S. Necrotizing fasciitis: a six-year experience. J Burn Care Res Off Publ Am Burn Assoc. 2012;33(1):93–100. https://doi.org/10.1097/BCR.0b013e318239d571.
Wang J-M, Lim H-K. Necrotizing fasciitis: eight-year experience and literature review. Braz J Infect Dis Off Publ Braz Soc Infect Dis. 2014;18(2):137–43. https://doi.org/10.1016/j.bjid.2013.08.003.
Weng C-L, Wang C-H, Chen I-C, et al. Red cell distribution width is an independent predictor of mortality in necrotizing fasciitis. Am J Emerg Med. 2014;32(10):1259–62. https://doi.org/10.1016/j.ajem.2014.08.001.
Willis RN, Guidry CA, Horn CB, et al. Predictors of monomicrobial necrotizing soft tissue infections. Surg Infect. 2015;16(5):533–7. https://doi.org/10.1089/sur.2014.189.
Yaghoubian A, de Virgilio C, Dauphine C, Lewis RJ, Lin M. Use of admission serum lactate and sodium levels to predict mortality in necrotizing soft-tissue infections. Arch Surg Chic Ill 1960. 2007;142(9):840–6. https://doi.org/10.1001/archsurg.142.9.840. (discussion 844–846).
Audureau E, Hua C, de Prost N, et al. Mortality of necrotizing fasciitis: relative influence of individual and hospital-level factors, a nationwide multilevel study, France, 2007–12. Br J Dermatol. 2017. https://doi.org/10.1111/bjd.15615.
Hong Y-C, Chou M-H, Liu EH, et al. The effect of prolonged ED stay on outcome in patients with necrotizing fasciitis. Am J Emerg Med. 2009;27(4):385–90. https://doi.org/10.1016/j.ajem.2008.03.010.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicts to disclose relating to the purpose of this study.
Ethical approval
This study was conducted under the oversight of the New York Medical College Institutional Review Board (IRB number: 12018).
Informed consent
As this study was retrospective in nature, using existing data from medical records, informed consent was not obtained.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Latifi, R., Patel, A.S., Samson, D.J. et al. The roles of early surgery and comorbid conditions on outcomes of severe necrotizing soft-tissue infections. Eur J Trauma Emerg Surg 45, 919–926 (2019). https://doi.org/10.1007/s00068-018-0958-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-018-0958-z