Abstract
Background
Open tibia fractures usually occur in high-energy mechanisms and are commonly associated with multiple traumas. The purposes of this study were to define the epidemiology of open tibia fractures in severely injured patients and to evaluate risk factors for major complications.
Methods
A cohort from a nationwide population-based prospective database was analyzed (TraumaRegister DGU®). Inclusion criteria were: (1) open or closed tibia fracture, (2) Injury Severity Score (ISS) ≥ 16 points, (3) age ≥ 16 years, and (4) survival until primary admission. According to the soft tissue status, patients were divided either in the closed (CTF) or into the open fracture (OTF) group. The OTF group was subdivided according to the Gustilo/Anderson classification. Demographic data, injury mechanisms, injury severity, surgical fracture management, hospital and ICU length of stay and systemic complications (e.g., multiple organ failure (MOF), sepsis, mortality) were collected and analyzed by SPSS (Version 23, IBM Inc., NY, USA).
Results
Out of 148.498 registered patients between 1/2002 and 12/2013; a total of 4.940 met the inclusion criteria (mean age 46.2 ± 19.4 years, ISS 30.4 ± 12.6 points). The CTF group included 2000 patients (40.5%), whereas 2940 patients (59.5%) sustained open tibia fractures (I°: 49.3%, II°: 27.5%, III°: 23.2%). High-energy trauma was the leading mechanism in case of open fractures. Despite comparable ISS and NISS values in patients with closed and open tibia fractures, open fractures were significantly associated with higher volume resuscitation (p < 0.001), more blood (p < 0.001), and mass transfusions (p = 0.006). While the rate of external fixation increased with the severity of soft tissue injury (37.6 to 76.5%), no major effect on mortality and other major complications was observed.
Conclusion
Open tibia fractures are common in multiple trauma patients and are therefore associated with increased resuscitation requirements, more surgical procedures and increased in-hospital length of stay. However, increased systemic complications are not observed if a soft tissue adapted surgical protocol is applied.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tibia fractures represent the most common long bone fracture. Furthermore, a high number of these fractures are associated with open soft tissue injuries due to a limited soft tissue envelope [1,2,3].
Open fractures are considered as an orthopedic emergency even in isolated injuries. General management principles of these injuries include early antibiotic coverage, meticulous debridement and lavage, classification of the soft tissue injury, temporary or definitive skeletal stabilization and soft tissue coverage or reconstruction [4,5,6,7,8]. However, treatment of open fractures in multiple trauma patients represents even a more sophisticated surgical challenge [7, 9,10,11].
In these patients, the fracture pattern and extend of open soft tissue injury particularly affects the amount of acute blood loss, the timing and type of skeletal fixation as well as the associated risk for late complications (e.g., non-union, infection) [3, 5, 12,13,14]. Therefore, treatment strategies have to consider associated injuries and the general condition of the severely injured patient [15].
Recently, Connelly et al. have already investigated the relevance of open tibia fractures on long-term outcome [13]. They identified a significant impact of tibia fractures on posttraumatic outcome. Among other factors, the presence of open fractures was significantly associated with mortality (OR 1.46, 95% CI 1.13–1.88, p = 0.004).
However, despite the results of that study, the relevance of open tibia fractures particularly in multiple trauma patients remains unknown. Specifically, the prevalence of open fractures and the risk of acute complications still remains unclear. To elucidate these aspects, we conducted the present registry study using data from one of largest databases of severely injured patients, the TraumaRegister DGU®.
We sought to answer the following questions:
-
What is the current epidemiology of open tibia fractures in multiply injured patients and the prevalence of different degrees of severity (grade I–III).
-
Is the severity of an open fracture type associated with clinical complications and outcome?
-
Can implications on management of these fractures be derived from the information gathered from a nationwide trauma registry?
Materials and methods
TraumaRegister DGU®
The TraumaRegister DGU® of the German Trauma Society (Deutsche Gesellschaft für Unfallchirurgie, DGU) was established in 1993. Data are collected prospectively in four consecutive time phases from the site of the accident until discharge from hospital including emergency room, initial surgery, and ICU phase. The documentation includes detailed information on demographics, injury pattern, comorbidities, pre- and in-hospital management, course on intensive care unit, relevant laboratory findings including data on transfusion and outcome of each individual. The inclusion criterion is admission via emergency room with subsequent ICU/ICM care or death after admission but before admission to ICU. The infrastructure for documentation, data management, and data analysis is provided by AUC—Academy for Trauma Surgery (AUC—Akademie der Unfallchirurgie GmbH), a company affiliated to the German Trauma Society. The scientific leadership is provided by the Committee on Emergency Medicine, Intensive Care and Trauma Management (Sektion NIS) of the German Trauma Society. The participating hospitals submit their data pseudomised into a central database via a web-based application. Scientific data analysis is approved according to a peer review procedure established by Sektion NIS.
Participation in TraumaRegister DGU® is voluntary. For hospitals associated with TraumaNetzwerk DGU® however, the entry of at least a basic data set is obligatory for reasons of quality assurance (QM form). Participants of TraumaNetzwerk DGU® can choose whether they use the standard form (regular form with full coverage of all items) or the QM-form, which includes a limited number of items for quality management purposes, only. Overall, 12.6% of the registry cohort was documented using QM-form and was therefore not available for detailed clinical outcome analyses. Furthermore, data from non-European trauma centers in (e.g., China, United Arab Emirates) were excluded from analysis. As part of a sophisticated protocol for data quality control, single centers that submitted inconsistent surgical data in single years were excluded from analysis. This group was referred to as “missing surgical data”. A total of 1.7% of the TR-DGU database was disqualified for this reason. The present study is in line with the publication guidelines of the TraumaRegister DGU® and registered as TR-DGU project ID 2011-040.
Definitions
-
Mechanisms of injury: (1) motor vehicle, (2) motorcycle, (3) bicycle accidents, (4) pedestrians struck, (5) high (≥ 3 m) and (6) low falls (< 3 m) and (7) other.
-
Injuries were coded according to Abbreviated Injury Scale (AIS, Version 2005); the Injury Severity Score (ISS) and the New Injury Severity Score (NISS) [16,17,18,19].
-
Open fractures were classified according to the Gustilo and Anderson system [4].
-
Hemorrhagic shock was defined as bleeding with a systolic blood pressure equal or below 90 mmHg (a) in pre-hospital setting and (b) at emergency room admission.
-
Pre-/In-hospital fluid administration was defined as those fluids administered before/after hospital admission and until arrival at the intensive care unit (ICU).
-
Number of packed red blood cell (pRBC) units transfused until ICU admission.
-
The Trauma Associated Severe Hemorrhage (TASH) Score [20, 21] is provided to describe the predicted risk for severe hemorrhage in points, whereas the pTASH indicates the predicted risk for mass transfusion (≥ 10 pRBCs) in Percent (e.g., TASH score: 18 points, pTASH: 50% risk for mass transfusion).
-
Organ failure was defined using the Sequential Organ Failure Assessment (SOFA) score [22] where three or four points were defined as failure, for each organ.
-
Multiple organ failure (MOF) was defined by a simultaneous organ failure of at least two organ systems [23].
-
Sepsis was defined according to the ACCP/SCCM consensus [24].
-
The Revised Injury Severity Classification (RISC) Score was calculated to compare predicted and observed mortality [25].
-
Mortality was defined as overall in-hospital death from any cause.
Inclusion criteria
-
ISS ≥ 16 points.
-
Age ≥ 16 years.
-
Emergency room (ER) admission between 01/2002 until 12/2013.
-
Tibia fracture: coding according to AIS-98, AIS-2005 and/or AO/OTA classification or by keyword (“tibia fracture”) in free text description [26].
Exclusion criteria
-
Transfers (in/out)
-
Missing surgical data
-
Short version of data entry sheet utilized
-
Non-European Trauma Centers
Statistical analysis
All data were tested for normal distribution. Continuous variables are shown as mean with standard deviation (SD), while categorical data are presented as frequencies and percentages. For variables with a large standard deviation, the median is provided. The Chi-square test was used for comparison of categorical variables. The Mann–Whitney U test was applied to test differences between the groups. The Kolmogorov–Smirnov test was applied for normal distribution. Results were considered statistically significant if p < 0.05. Linear regression analysis was performed for the three subgroups of open fractures. Differences between the subgroups were evaluated with the Chi-square test for trends. No imputation was performed. The analysis was performed with SPSS for Windows (Version 22, IBM Inc., Armonk, NY, USA).
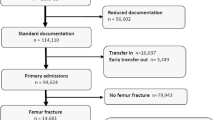
A flow diagram (Fig. 1) is provided to characterize the study cohort including related sample sizes.
Results
From a total of 148.498 documented patients between 1/2002 and 12/2013, we identified 4.940 individuals who met the inclusion criteria (mean age 46.2 ± 19.4 years, ISS 30.4 ± 12.6 points). In both groups, patients were predominantly young and male. The CTF group included 2000 closed fractures (40.5%), whereas the OTF group included 2940 (59.5%) open tibia fracture patients. High-energy trauma, often related to road traffic accidents, was the leading cause of injury in open fractures: motor vehicle (n = 927) and motorcycle accidents (n = 656) were the two predominant mechanisms. In motorcycle accidents, riders sustained open tibial fractures significantly more often (p ≤ 0.001), when compared to closed fractures. The third group included 195 pedestrians struck by a vehicle. Bicycle-related injuries, falls and other mechanisms were less common (Table 1).
Injury pattern, injury severity and management
Both groups showed no significant differences with respect to ISS and NISS (Table 2). The incidence of severe (AIS > 3) concomitant injuries of the head and abdomen as well as pelvic and femoral fractures was higher in the CTF group. Although the hemodynamic status in the pre-hospital setting was comparable between both groups (Table 3), patients with open fractures received significantly higher pre-hospital volume resuscitation (p < 0.001). The OTF group also received more volume in the hospital, more blood (p < 0.001), and a higher incidence of mass transfusions was observed (p = 0.006). The higher risk for trauma associated severe hemorrhage and increased resuscitation efforts were indicated by an elevated TASH Score (p < 0.001) in the open fracture group. The majority of open fractures were primarily stabilized by external fixation (Table 4). The total number of surgical procedures related to the tibial fracture was increased in the OTF group (1.2 vs. 2.3 procedures, p < 0.001).
Outcome measures
Ventilation time and LOS on ICU (p = 0.040) was shorter in the OTF group, whereas total in-hospital LOS was prolonged in these patients (p < 0.001). The risk for sepsis (12.7 vs. 12.9%) and multiple organ failure (38.5 vs. 39.2%) was comparable between the CTF and OTF groups. However, mortality was decreased in open fracture patients (p = 0.040).
Subgroup analysis
According to Gustilo and Anderson, open fractures were divided into subgroups (Table 5): I° (OTF I: n = 1450, 49.3%), II° (OTF II: n = 809, 27.5%) and III° (OTF III: n = 681, 23.2%). Median ISS was measured 27 points and median NISS measured 34 points for all three types of open fractures. While the rate of external fixation increased with the degree of soft tissue injury from 37.6 to 76.5%; mortality and the incidence of sepsis was comparable between the subgroups. The incidence of MOF increased from type I (38.0%) to type III (44.2%) in open fractures (p < 0.001). The highest risk for hemorrhagic shock (28.3%) and mass transfusion (19.5%) was found in OTF III (p < 0.001). The elevated risk for mass transfusion according to the TASH score was accurately predicted (18.2%; p < 0.001). In subgroup OTF II, the lowest incidences of pre-hospital shock (23.9%) and mass transfusion (12.1%) was observed. This was accompanied by the lowest mortality (14.3%) of all subgroups.
Discussion
Open long bone fractures are frequently related to complex fracture patterns, limb-threatening soft tissue destruction and even exsanguinating arterial hemorrhage [1, 27,28,29,30]. Previous studies well described the systemic burden (e.g., hemorrhagic shock, sepsis, organ failure) associated with major long bone fractures [3, 8, 10, 12,13,14, 31, 32], which in return promotes and interacts with subsequent local and late complications (e.g., infection, non-union).
Although open fractures particularly appear after high-energy trauma mechanisms, little is known about the relevance of open tibia fractures in multiple trauma patients. Based on one of the largest databases of severely injured patients (TraumaRegister DGU®), we were able to include the highest number of patients for evaluation of the relevance of open tibia fractures after multiple traumas.
While recent studies included both patients with isolated and multisystem injuries, the authors reported a lower rate of open soft tissue injuries (15–33%) associated with tibia fractures [33, 34]. We found a rate of 59.5% for open fractures in multiple trauma patients in our cohort. This might be explained by a greater proportion of high-energy trauma in multiple trauma patients in this study, when compared to the literature data of patients with a single trauma. Among multiple trauma patients, particularly motorcyclists seem to be at special risk to sustain open tibia fractures. These findings underline the well-described association between high-energy mechanisms and soft tissue injuries [28, 35]. Our epidemiologic findings are in accordance with the landmark study published by Court-Brown et al. in 1998 [1]. As we only included patients with an ISS ≥ 16, the ISS in this study was significantly higher than described by Court-Brown et al. However, also these authors found a high incidence of concomitant injuries (52.5%) in patients with open tibia fractures (1,35). In the comprehensive analysis also published by Court-Brown in 2012 [36], only 13.8% of patients with lower limb open fractures presented with an ISS ≥ 16. Despite comparable ISS and NISS values between patients with closed and open fractures, the presence of open fractures was associated with both, a significantly higher volume replacement in the pre-hospital as well as in the early clinical phase (until admission to ICU) and an increased requirement of (mass) transfusions. Accordingly, the TASH Score (p < 0.001) was elevated for open fractures and indicated an increased risk for severe hemorrhage. The more aggressive approach for volume replacement in patients with open fractures might explain why the incidence of hemorrhagic shock was comparable between patients with closed and open fractures. We therefore conclude that the presence of an open fracture affects the resuscitation protocol in the pre- and early clinical phase.
We further subdivided the OTF group in three subgroups according to the widespread-used classification system of Gustilo and Anderson. The system was primarily developed for open tibia fractures, but consecutively adapted to other long bone fractures. It is the most frequently used and universally accepted system because it is relevant for the initial management, complication rates and functional prognosis. However, we acknowledge specific limitations that have been identified over time, including its subjective nature, inter-observer agreement and its accuracy depending on the expertise of the surgeon [37,38,39]. The distribution of open fractures in our study (I°: 49.3%, II° 27.5%, III°: 23.2%) was different from the results of a recent meta-analysis including 32 articles [30] that described a higher incidence of severe open fractures (I°: 17.2%; II°: 25.5%; III°: 57.3%).
Furthermore, the enormous treatment costs of severe open fractures have attracted special attention in the past [40]. Open fractures are a well-known cost driver, due to multiple reconstructive procedures, an increased hospital length of stay (LOS) and a delayed return to work because of poor functional results. In accordance to previous studies, we also found a higher number of surgical procedures related to the tibia fracture that is clearly associated with the severity of the soft tissue damage (closed: 1.2; open I°: 1.8; II°: 2.4; III°: 3.3) These factors must be considered as surrogates for increased treatment costs for open fractures. While the number of surgeries increased with the degree of soft tissue injury, open fractures remain a major socioeconomic issue for health care systems and societies [41, 42].
Our group therefore developed an algorithm to improve and accelerate the management of these patients, to allow safe conversion from temporary external fixation to definitive internal fixation [43]. We demonstrated that the implementation of a standard algorithm directly affected the LOS as major cost driver: hospital LOS was reduced from 25.4 to 16.3 days significantly (p = 0.008).
Gill et al. recently studied the effects of early conversion from external to intramedullary fixation in 84 types III A/B open tibia fractures and identified a reduced risk for pin tract infections. Furthermore, the authors reported an excellent union rate of 95% (80) within the 24-month follow-up period [31]. Unfortunately, TR-DGU does not provide us with detailed information on local complications such as wound infection or healing disorders.
With regard to intensive care, Scalea et al. reported an increased ICU-LOS (11.0 vs. 8.0 days) for severely injured patients (ISS 26.8), who received temporary external fixation. In our data, the rate for external fixation increased with the severity of open injury (I: 54.6%; II: 67.0%, 76.5%), while the median ISS remained constant. However, in our severely injured cohort, the higher rate of external fixation in open fractures (37.6 vs. 63.1%) was even associated with a reduced ICU-LOS (p = 0.040).
Among the drawbacks of our study is the fact that we are unable to provide data for the further breakdown of type III open fractures, the timing of conversion from EF to IMN and late complications (e.g., non-union rates); limitations based on the nature of the TraumaRegister DGU®. On the other hand, we are able to describe the treatment reality of open major fractures based on the largest cohort analyzed to date.
Previous studies recommended intramedullary nailing also for patients with severe open tibial fractures, even when limb salvage required the combination of external fixation and muscle flaps for wound coverage [44]. This general recommendation is not in line with our findings, indicating that external fixation remains the treatment reality at least for the majority of open tibia fractures in Germany, at least for severely injured patients with multiple traumas.
Okike and Bhattacharyya critically reviewed the management of open tibia fractures and found fair evidence for both external fixation and intramedullary nailing [45].
A recent review from Giovannini et al. reviewed five randomized controlled trials (RCTs) involving a total of 239 patients with type III A/B open tibial fractures [46]. All patients underwent surgical debridement, soft tissue repair and fracture fixation with intramedullary nailing (IMN) or external fixation (EF). The authors concluded that IMN is associated with lower rates of infection and non-union, and EF involves shorter operating times and is therefore more suitable in multiply injured patients.
While IMN offers benefits in patients with isolated fractures, our data shows that surgeons seem to favor external fixation in multiple trauma patients with severe open soft tissue injuries. The rationale for external fixation includes the lower surgical burden and time saving effects; and therefore facilitating simultaneous life-saving surgeries. Furthermore, we feel it remains crucial to assess the severity of soft tissue injuries associated with open long bone fractures and the patient general condition; in the process of clearing for definitive surgery and enhancing patient safety [47]. Also, it is critical to differentiate between isolated open fractures and patients who sustained multiple trauma including open long bone fractures in future studies [6, 29, 48, 49].
Conclusion
In multiply injured patients, open tibia fractures are common, and they are associated with increased resuscitation requirements, a higher number of surgical procedures and an increased in-hospital length of stay. However, increased systemic complications in severe open fractures are not observed if a soft tissue adapted surgical protocol is applied.
References
Court-Brown CM, Rimmer S, Prakash U, McQueen MM. The epidemiology of open long bone fractures. Injury. 1998;29(7):529–34.
Brown C, Henderson S, Moore S. Surgical treatment of patients with open tibial fractures. AORN J. 1996;63(5):875–81 (85–96; quiz 99–906).
Border JR. Death from severe trauma: open fractures to multiple organ dysfunction syndrome. J Trauma. 1995;39(1):12–22.
Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Jt Surg Am Vol. 1976;58(4):453–8.
Templeman DC, Gulli B, Tsukayama DT, Gustilo RB. Update on the management of open fractures of the tibial shaft. Clin Orthop Relat Res. 1998;350:18–25.
Townley WA, Nguyen DQ, Rooker JC, Dickson JK, Goroszeniuk DZ, Khan MS, et al. Management of open tibial fractures—a regional experience. Ann R Coll Surg Engl. 2010;92(8):693–6. https://doi.org/10.1308/003588410x12699663904592.
Trickett RW, Rahman S, Page P, Pallister I. From guidelines to standards of care for open tibial fractures. Ann R Coll Surg Engl. 2015;97(6):469–75. https://doi.org/10.1308/rcsann.2015.0020.
Willy C, Stichling M, Engelhardt M, Vogt D, Back DA. Acute therapeutic measures for limb salvage Part 1: haemorrhage control, emergency revascularization, compartment syndrome. Der Unfallchirurg. 2016;119(5):374–87. https://doi.org/10.1007/s00113-016-0179-z.
Campion EM, Mackersie RC. Recent developments in the assessment of the multiply injured trauma patient. Curr Opin Crit Care. 2014;20(6):620–5.
Wordsworth M, Lawton G, Nathwani D, Pearse M, Naique S, Dodds A, et al. Improving the care of patients with severe open fractures of the tibia: the effect of the introduction of Major Trauma Networks and national guidelines. Bone Jt J. 2016;98-b(3):420–4.
Weber CD, Lefering R, Dienstknecht T, Kobbe P, Sellei RM, Hildebrand F, et al. Classification of soft-tissue injuries in open femur fractures: relevant for systemic complications? J Trauma Acute Care Surg. 2016;81(5):824–33.
Milner SA, Davis TR, Muir KR, Greenwood DC, Doherty M. Long-term outcome after tibial shaft fracture: is malunion important? J Bone Jt Surg Am Vol. 2002;84-a(6):971–80.
Connelly CL, Bucknall V, Jenkins PJ, Court-Brown CM, McQueen MM, Biant LC. Outcome at 12 to 22 years of 1502 tibial shaft fractures. Bone Jt J. 2014;96-b(10):1370–7. https://doi.org/10.1302/0301-620x.96b10.32914.
Metsemakers WJ, Handojo K, Reynders P, Sermon A, Vanderschot P, Nijs S. Individual risk factors for deep infection and compromised fracture healing after intramedullary nailing of tibial shaft fractures: a single centre experience of 480 patients. Injury. 2015;46(4):740–5.
Hildebrand F, van Griensven M, Huber-Lang M, Flohe SB, Andruszkow H, Marzi I, et al. Is there an impact of concomitant injuries and timing of fixation of major fractures on fracture healing? A focused review of clinical and experimental evidence. J Orthop Trauma. 2016;30(3):104–12.
Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187 – 96.
Garthe E, States JD, Mango NK. Abbreviated injury scale unification: the case for a unified injury system for global use. J Trauma. 1999;47(2):309–23.
Greenspan L, McLellan BA, Greig H. Abbreviated Injury Scale and Injury Severity Score: a scoring chart. J Trauma. 1985;25(1):60–4.
Osler T, Baker SP, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma. 1997;43(6):922–5. (discussion 5–6).
Yucel N, Lefering R, Maegele M, Vorweg M, Tjardes T, Ruchholtz S, et al. Trauma associated severe hemorrhage (TASH)-Score: probability of mass transfusion as surrogate for life threatening hemorrhage after multiple trauma. J Trauma. 2006;60(6):1228–36. (discussion 36–7).
Maegele M, Lefering R, Wafaisade A, Theodorou P, Wutzler S, Fischer P, et al. Revalidation and update of the TASH-Score: a scoring system to predict the probability for massive transfusion as a surrogate for life-threatening haemorrhage after severe injury. Vox Sanguinis. 2011;100(2):231–8.
Vincent JL, de Mendonca A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26(11):1793–800.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644–55.
Bone RC. Let’s agree on terminology: definitions of sepsis. Crit Care Med. 1991;19(7):973–6.
Lefering R. Development and validation of the revised injury severity classification score for severely injured patients. Eur J Trauma Emerg Surg. 2009;35(5):437 – 47.
Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium—2007: orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma. 2007;21(10 Suppl):S1–133.
Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24(8):742–6.
Sarmiento A. Mechanism of injury may affect outcome after tibial shaft fracture. J Bone Jt Surg Am Vol. 2003;85-a(3):571; (author reply—2).
Penn-Barwell JG, Bennett PM, Fries CA, Kendrew JM, Midwinter MJ, Rickard RF. Severe open tibial fractures in combat trauma: management and preliminary outcomes. Bone Jt J. 2013;95-b(1):101–5.
Papakostidis C, Kanakaris NK, Pretel J, Faour O, Morell DJ, Giannoudis PV. Prevalence of complications of open tibial shaft fractures stratified as per the Gustilo–Anderson classification. Injury. 2011;42(12):1408–15.
Gill SP, Raj M, Kumar S, Singh P, Kumar D, Singh J, et al. Early conversion of external fixation to interlocked nailing in open fractures of both bone leg assisted with vacuum closure (VAC)—final outcome. J Clin Diagn Res. 2016;10(2):Rc10-4.
Pfeifer R, Darwiche S, Kohut L, Billiar TR, Pape HC. Cumulative effects of bone and soft tissue injury on systemic inflammation: a pilot study. Clin Orthop Relat Res. 2013;471(9):2815–21.
Weiss RJ, Montgomery SM, Ehlin A, Al Dabbagh Z, Stark A, Jansson KA. Decreasing incidence of tibial shaft fractures between 1998 and 2004: information based on 10,627 Swedish inpatients. Acta Orthop. 2008;79(4):526–33.
Donegan DJ, Akinleye S, Taylor RM, Baldwin K, Mehta S. IM nailing of tibial shaft fractures: size matters. J Orthop Trauma. 2016;3 0(7):377–80. https://doi.org/10.1097/BOT.0000000000000555.
Chapman MW. Role of bone stability in open fractures. Instr Course lect. 1982;31:75–87.
Court-Brown CM, Bugler KE, Clement ND, Duckworth AD, McQueen MM. The epidemiology of open fractures in adults. A 15-year review. Injury. 2012;43(6):891–7.
Rajasekaran S, Naresh Babu J, Dheenadhayalan J, Shetty AP, Sundararajan SR, Kumar M, et al. A score for predicting salvage and outcome in Gustilo type-IIIA and type-IIIB open tibial fractures. J Bone Jt Surg Br Vol. 2006;88(10):1351–60.
Brumback RJ, Jones AL. Interobserver agreement in the classification of open fractures of the tibia. The results of a survey of two hundred and forty-five orthopaedic surgeons. J Bone Jt Surg Am Vol. 1994;76(8):1162–6.
Horn BD, Rettig ME. Interobserver reliability in the Gustilo and Anderson classification of open fractures. J Orthop Trauma. 1993;7(4):357 – 60.
Bondurant FJ, Cotler HB, Buckle R, Miller-Crotchett P, Browner BD. The medical and economic impact of severely injured lower extremities. J Trauma. 1988;28(8):1270–3.
Schenker ML, Ahn J, Donegan D, Mehta S, Baldwin KD. The cost of after-hours operative debridement of open tibia fractures. J Orthop Trauma. 2014;28(11):626–31.
MacKenzie EJ, Jones AS, Bosse MJ, Castillo RC, Pollak AN, Webb LX, et al. Health-care costs associated with amputation or reconstruction of a limb-threatening injury. J Bone Jt Surg Am Vol. 2007;89(8):1685–92.
Horst K, Andruszkow H, Weber C, Dienstknecht T, Hildebrand F, Tarkin I, et al. Standards of external fixation in prolonged applications to allow safe conversion to definitive extremity surgery: the Aachen algorithm for acute ex fix conversion. Injury. 2015;46(Suppl 3):S13–8.
Webb LX, Bosse MJ, Castillo RC, MacKenzie EJ. Analysis of surgeon-controlled variables in the treatment of limb-threatening type-III open tibial diaphyseal fractures. J Bone Jt Surg Am Vol. 2007;89(5):923–8.
Okike K, Bhattacharyya T. Trends in the management of open fractures. A critical analysis. J Bone Jt Surg Am vol. 2006;88(12):2739–48.
Giovannini F, de Palma L, Panfighi A, Marinelli M. Intramedullary nailing versus external fixation in Gustilo type III open tibial shaft fractures: a meta-analysis of randomised controlled trials. Strat Trauma Limb Reconstr (Online). 2016;11(1):1–4.
Pape HC, Andruszkow H, Pfeifer R, Hildebrand F, Barkatali BM. Options and hazards of the early appropriate care protocol for trauma patients with major fractures: towards safe definitive surgery. Injury. 2016;47(4):787–91.
Scalea TM, Boswell SA, Scott JD, Mitchell KA, Kramer ME, Pollak AN. External fixation as a bridge to intramedullary nailing for patients with multiple injuries and with femur fractures: damage control orthopedics. J Trauma. 2000;48(4):613–21 (discussion 21–3).
Tornetta P 3rd, Bergman M, Watnik N, Berkowitz G, Steuer J. Treatment of grade-IIIb open tibial fractures. A prospective randomised comparison of external fixation and non-reamed locked nailing. J Bone Jt Surg Br Vol. 1994;76(1):13–9.
Funding
The TraumaRegister DGU® was previously partly funded by the Deutsche Forschungsgemeinschaft (Ne 385/5) and by a grant from Novo Nordisk A/S, Bagsvaerd, Denmark. It is now supported by fees from the participating hospitals (a list of hospitals is available at http://www.traumaregister.de) and hosted by the AUC—Academy for Trauma Surgery (AUC).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest. This study was performed without any financial or other support.
Compliance with ethical requirements
The present study follows the publication guidelines of the TraumaRegister DGU® and is registered as TR-DGU project ID 2011-040. In accordance with the institutional guidelines, informed consent was not required, because the documentation and data analysis within the trauma registry is mandatory for certified trauma centers to perform external quality assessment.
Rights and permissions
About this article
Cite this article
Weber, C.D., Hildebrand, F., Kobbe, P. et al. Epidemiology of open tibia fractures in a population-based database: update on current risk factors and clinical implications. Eur J Trauma Emerg Surg 45, 445–453 (2019). https://doi.org/10.1007/s00068-018-0916-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-018-0916-9