Abstract
Introduction
A pulmonary contusion is an entity defined as alveolar haemorrhage and pulmonary parenchymal destruction after blunt chest trauma. According to the literature, most pulmonary contusions can only be seen on a chest CT. The aim of this study was to evaluate the patients with pulmonary contusions, as well as their management, considering diagnostic and therapeutic options related to their outcomes, since we assumed, based on everyday clinical practice, that an ‘overdiagnosing’ and ‘overtreatment’ attitude towards this injury could be present.
Patients and methods
The research was a retrospective study including 5042 patients admitted to the Department of Traumatology in the Clinical Hospital Centre Osijek, during a 3-year period. The medical data of the patients who suffered pulmonary contusion were evaluated considering significant characteristics, known risk factors, procedures undergone, and outcomes.
Results
During the 3-year period, 2% of all the admitted patients were diagnosed with a pulmonary contusion. In 54% of the cases, the patient suffered polytraumatic injuries. The pulmonary contusion was an isolated injury in 7% of the patients. In 31% of the cases, there was no liquidothorax or pneumothorax (isolated pulmonary contusion). In 89% of the patients the pulmonary contusion was diagnosed using a CT scan. In 68% of the patients there were no interventions regarding the thorax; thoracocentesis was performed in 25% of the cases, and pleural punction in 14% of the cases. 25% of the patients developed respiratory insufficiency and 16% required mechanical ventilation. Regarding isolated pulmonary contusions, respiratory insufficiency was present in 8% of the cases.
Conclusions
We suggest that a pulmonary contusion seen on CT only has limited clinical significance and that the use of CT scans in diagnosing and follow-up of these patients should be re-evaluated. Further prospective and randomised studies should be conducted and the patients should be clinically evaluated, with the administration of supportive and antibiotic therapy, maintaining the fluid balance, the administration of diuretics, supportive oxygen therapy, pulmonary toilet, and physical therapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
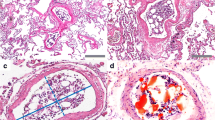
A pulmonary contusion (PC) is an entity defined as alveolar haemorrhage caused by an injury to the alveolar capillaries and pulmonary parenchymal destruction after blunt chest trauma. Lung tissue injury occurs when the chest wall bends inward following the trauma [1]. The possible mechanisms are based on inertial effects, mainly on different tissue densities—light alveolar tissue and heavy hilar structures [2]. A parenchymal lesion can occur during the 24 h after injury. It resolves within 3–14 days, depending on the size, the number of affected lobes has been reported to determine the outcome [1]. The injury of the lung tissue without a chest wall injury was first described by Giovanni Battista Morgagni, an Italian anatomist, in 1761, and the term “pulmonary contusion” dates from the nineteenth century and Guillaume Dupuytren, a French military surgeon. The incidence is 25–35% of all blunt chest trauma [2, 3]. Clinical manifestations include respiratory distress with hypoxemia and hypercarbia as a result of ventilation/perfusion difficulties, increased intrapulmonary shunting, increased lung water, segmental lung damage, and a loss of compliance [2]. According to the literature, most pulmonary contusions are only seen on a chest CT (SOCTO). Treatment of the PC is conservative and supportive; the goal is to prevent respiratory failure and hypoxia. Managing of the PC includes the maintenance of fluid balance, the administration of diuretics, supportive oxygen therapy, and pulmonary toilet and postural changes [3, 4]. The aim of this study was to evaluate pulmonary contusions in general, as well as the management of the patients, considering diagnostic and therapeutic options related to their outcomes, since we assumed, based on everyday clinical practice, that an ‘overdiagnosing’ and ‘overtreatment’ attitude towards this injury could be present.
Patients and methods
The research was done as a retrospective study including all the patients who suffered a PC and were admitted to the Department of Traumatology in the Clinical Hospital Centre Osijek during a 3-year period. The medical data were extracted from the database including 5042 patients admitted to the department in the period from 2010 to 2012, it was evaluated considering the patients’ age, sex, mechanism of injury, polytrauma, comorbidities, other pulmonary diagnoses, other injuries, serial rib fractures, pleural effusion or pneumothorax, confirmation of the clinical diagnosis using a CT scan and a control CT scan, interventions such as pleural punction or thoracocentesis, respiratory distress, mechanical ventilation, other surgical procedures following concomitant injuries, the length of the hospitalisation, consultations by a pulmonologist, anticoagulative therapy, physical therapy, and complications recorded during regular check-ups. We tested if the PC diagnoses affected the incidence of respiratory distress and the need for mechanical ventilation, if they prolonged the length of hospitalisation, if there was need for a pulmonologist consultation, and if there were adverse outcomes. The inclusive criteria were the diagnoses of pulmonary contusion on the admittance or during the hospitalisation. The statistical program SPSS 23.0 for Windows/Mac OS X (IBM Corp., Armonk, NY, USA) was used for the statistical analyses. P < 0.05 was considered a priori as statistically significant. All values were mean ± standard deviation (SD). The comparison among groups was done using a t test.
Results
During the 3-year period, there were 101 diagnosed cases of PCs in the Department of Traumatology, Surgery Clinic, in the Hospital Centre Osijek, which makes for 2% of all the admitted patients. 88% were male and 12% were female. The oldest patient was 84 and the youngest patient was 17 years old, the average age was 47. In 56% of the cases, the trauma was caused by a traffic accident; other causes were falling from a height, falling off from a bicycle, fighting, or getting hit in the chest by an animal. In 54% of the cases the patient suffered polytraumatic injuries. In 42% of the cases the PC was bilateral and in the rest of the cases both the right and the left lung were equally affected. There were no comorbidities in 52% of the patients, 19% had hypertension and diabetes, and the rest of the patients had various joined conditions, such as psychoorganic syndrome, epilepsy, and liver lesions. There was no joined pulmonological diagnosis in 94% of the cases, while pneumonia was present in the rest of the patients. The PC was an isolated injury in 7% of the patients; others had multiple injuries, intracranial in 43% of the cases. 75% of the patients had a rib fracture; a serial rib fracture was present in 52% of the cases. In 79% of the cases there was no subcutaneous emphysema. In 31% of the cases there was no liquidothorax or pneumothorax. Pneumomediastinum was present in 7% of the patients. In 89% of the patients the PC was diagnosed using a CT scan, and in the rest of the cases it was diagnosed using an X-ray. Follow-up CT scans were performed in 18% of the patients. In 68% of the patients there were no interventions regarding the thorax, thoracocentesis was performed in 25% of the cases and pleural punction in 14% of the cases. 25% of the patients developed respiratory insufficiency and 16% required mechanical ventilation. The average duration of mechanical ventilation was 5 days. In cases with isolated PCs, without liquidothorax or pneumothorax, respiratory insufficiency was present in 8% of the cases. Complications during hospitalisation were defined as laboratory and X-ray changes, resembling pneumonia, a pulmonologist was consulted in 19% of the cases. Anticoagulant therapy was prescribed for 54% of the patients, while physical therapy was conducted with 25% of the patients. 23% of the patients were undergoing an operative procedure or an osteosynthesis of an extremity fracture, and a laparotomy for abdominal organ injuries was done in two cases. The length of hospitalisation was from 2 to 121 days, depending on the other injuries, for patients having only thoracic injuries the average hospital stay was 14 days.
Discussion
The incidence of PC in our study was slightly lower than the incidence found in the literature. The patients were a decade older in average compared to the literature data [5]. The young age is easily explainable by the mechanism of trauma—mostly traffic accidents and falling from a height, and in our data, the socio-demographic factors influence the older age of the patients—low natality and emigrations resulted in the ‘aging’ of the population. Our patients were mostly male, similar to the literature data, since most of the cases were caused by a traffic accident, mostly involving a motorcycle and it is considered that motorcycle drivers are mostly male [6].
In our patients the symptoms included dyspnoea, chest tightness, chest pain, and decreased exercise tolerance [4], also with subcutaneous emphysema in some cases. Half of the patients had polytraumatic injuries and consequentially a worse outcome—prolonged hospitalisation and complications. One-third of the patients had no liquidothorax or pneumothorax (isolated PC). The results show that liquidothorax or pneumothorax is generally associated with rib fractures and in most of the patients there were no interventions regarding the thorax, thoracocentesis or pleural punction was performed in small number of cases. These results show that in two-thirds of the patients there were no interventions regarding the thorax, even in cases with diagnosed pleural effusion or pneumothorax, since they were clinically insignificant and thoracic drainage was not required.
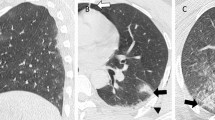
The following aspects were considered in order to diagnose a PC: mode of injury, physical examination, radiography, and arterial blood gasses which may show insufficient oxygen and excessive carbon dioxide [7,8,9,10]. A chest X-ray is the most common method used for the diagnosis of a PC [11]. Consolidated areas appear white on an X-ray film. The contusion is typically not restricted by the anatomical boundaries of the lobes or the segments of the lung [12,13,14]. The X-ray appearance of a PC is similar to that of an aspiration, and the presence of a haemothorax or a pneumothorax may obscure the contusion on a radiograph [15, 16]. The signs of contusion that progress after 48 h post-injury are likely to be actually caused by aspiration, pneumonia, or acute respiratory distress syndrome (ARDS) [17]. Although chest radiography is an important part of the diagnosis, it is often not sensitive enough to detect the condition early after the injury [18]. In one-third of the cases, the PC is not visible on the first chest radiograph performed [19]. It takes an average of 6 h for the characteristic white regions to show up on a chest X-ray, and the contusion may not become apparent for 48 h [12, 13, 19]. When a PC is apparent in an X-ray, it suggests that the trauma to the chest was severe and that a CT scan might reveal other injuries that were missed by the X-ray [20].
A CT is a more sensitive test for a PC and it can identify abdominal, chest, or other injuries that accompany the contusion [21,22,23]. Unlike an X-ray, a CT scan can detect the contusion almost immediately after the injury [22]. However, in both an X-ray and a CT scan, a contusion may become more visible over the first 24–48 h after trauma, as bleeding and oedema into lung tissues progress [24]. A CT scan also helps determine the size of a contusion, a larger volume of the contused lung on a CT scan is associated with an increased likelihood that ventilation will be needed [22]. The indication for mechanical ventilation is, of course, based on the clinical status of the patient. CT scans also help differentiate between a contusion and a pulmonary haematoma, which may be difficult to tell apart otherwise [25]. Findings on CT scans of contusions are non-segmental areas of consolidation and ground-glass opacification, which mostly involve the lung and are directed deeply into the area of trauma, often sparing 1–2 mm of sub-pleural lung parenchyma adjacent to the injured chest wall [26]. A CT is highly sensitive in detecting a PC, and the extent of lung involvement on a CT scan correlates with clinical outcomes [10, 27,28,29].
However, PCs visible on a CT but not on a chest X-ray, PC SOCTO, are usually not severe enough to affect the outcome or the treatment [11]. In nearly all of the patients the PC was diagnosed using a CT scan, and in the rest of the cases it was diagnosed using an X-ray. A follow-up CT scan was performed in very few patients mostly because of their clinical status—if there were symptoms of pneumonia or lack of clinical improvement.
The use of a pulmonary ultrasound, performed at the bedside or on the scene of the accident, is still not widespread, being limited to facilities which are comfortable with its use for other applications, like pneumothorax, airway management, and haemothorax. Its accuracy has been found to be comparable to CT scanning [30]. An ultrasound could be used in all cases with positive chest X-ray findings and for follow-up examinations. The ultrasound is useful in patients with X-ray-positive pleural effusion because of the possibility to mark the place on the skin for optimal pleural punction and for diagnosing the pleural effusion in patients with negative X-ray for pleural effusion.
In our study, some of the patients developed respiratory insufficiency and a very small number required mechanical ventilation, where the duration was under 48 h in most of the cases. There were no long-term complications in patients with a PC who developed ARDS. In cases with isolated PCs, without a liquidothorax or pneumothorax, respiratory insufficiency was present rarely. Hoff et al. reviewed patients having an isolated PC after blunt chest trauma, and the results showed that an isolated PC in healthy patients is not associated with mortality. Other authors associate a PC with a 10–25% mortality rate. Some patients develop complications depending on hypoxia on admission and a PC on the admission chest radiograph (large contusions). Complications that can possibly occur in patients with a PC are pneumonia, empyema, atelectasis, and bronchopleural fistula [2, 7].
The incidence of pneumomediastinum, according to the literature, in patients with blunt chest trauma and a PC is probably caused by the “Macklin effect” in all the cases where thoracic and abdominal viscus perforation has been ruled out. The “Macklin effect” is a result of increased intra-alveolar pressure, leading to alveolar rupture, with air dissection along the bronchovascular sheaths and the spreading of this pulmonary interstitial emphysema in the mediastinum. It is diagnosed using chest radiography and CT, and managed conservatively [8, 9].
ARDS may occur in 50–60% of these patients according to the literature, in these cases mechanical ventilation is required, including lung protective ventilation, as per ARDS net protocols (low tidal volume with high PEEP), inverse ratio ventilation, individual lung ventilation with a double lumen tube, and high-frequency jet ventilation. The use of non-invasive positive pressure ventilation (NIPPV) has shown good results [2, 4].
The treatment for PCs includes supportive and antibiotic therapy, maintenance of fluid balance, administration of diuretics, supportive oxygen therapy, and pulmonary toilet and postural changes. The administration of fluids is considered controversial in these cases, considering the possibility of exacerbating the oedema. Chest physiotherapy includes breathing exercises, stimulation of coughing, suctioning, percussion, movement, and vibration [2, 4]. Our results show that anticoagulant therapy was prescribed for 54% of the patients, while physical therapy was conducted with 25% of the patients. All the patients with a diagnosed PC were on antibiotic therapy. In the cases with PC SOCTO where there were no clinical indications for antibiotic treatment, this protocol could be in the ‘overtreatment zone’ and should also be re-evaluated. There is no evidence that every pulmonary contusion causes complications if antibiotic therapy is not administered. The complications have been associated with the size of the lesion, which again leads us to the conclusion that if there is a possibility for complications, the lesion will be detected on the standard chest X-ray, and if it is PC SOCTO it will cause complications in exceptional cases. The clinical status of the patient should be the main guide for making decisions regarding the therapy and the course of treatment.
Physical therapy should be conducted whenever possible, in our case the limitations for physical therapy were polytraumatic and intracranial injuries. Some of the patients were undergoing an operative procedure or an osteosynthesis of an extremity fracture and laparotomy for abdominal organ injuries. The diagnosis of PC did not prolong the hospital stay for operated patients, which means the hospitalisation lasted the same number of days as in the patients undergoing the same operative procedures and not having a PC.
Research is being conducted regarding new treatment options, including intravenous corticosteroids, antioxidants, and exogenous surfactants, since the role of neutrophils and fibroblast proliferation in the inflammatory response to lung tissue injury has been established [2].
Since the main cause of blunt chest trauma and PCs are traffic accidents, prevention strategies include airbags, seat belts, and car seats for children [2].
Conclusions
We suggest that PC SOCTO has limited clinical significance and that the use of a CT scan in diagnosing and follow-up of these patients should be re-evaluated. There is no need for deep research of PC if no clinical sign arises. Further prospective and randomised studies should be conducted. Patients should be clinically evaluated, with the administration of supportive and antibiotic therapy, maintaining the fluid balance, the administration of diuretics, supportive oxygen therapy, pulmonary toilet, and physical therapy. Further research is needed regarding new therapy options and the more frequent use of the pulmonary ultrasound.
References
Cohn SM, DuBose JJ. Pulmonary contusion: an update on recent advances in clinical management. World J Surg. 2010;34(8):1959–70.
Ganie FA, Lone H, Lone GN, Wani ML, Singh S, Dar AM, et al. Lung contusion: a clinico-pathological entity with unpredictable clinical course. Bull Emerg Trauma. 2013;1(1):7–16.
Rodriguez RM, Friedman B, Langdorf MI, Baumann BM, Nishijima DK, Hendey GW, et al. Pulmonary contusion in the pan-scan era. Injury. 2016;47:1031–4.
Chaudhury A, Gaude G, Hattiholi J. Risk factors affecting the prognosis in patients with pulmonary contusion following chest trauma. J Clin Diagn Res. 2015; 9(8):OC17–9.
Jin H, Tang L, Pan Z, Peng N, Wen Q, Tang Y, et al. Ten-year retrospective analysis of multiple trauma complicated by pulmonary contusion. Mil Med Res. 2014;1:7.
Sant’Anna FL, Andrade SM, Sant’Anna FH, Liberatti CL. Motorcycle accidents: comparison between the years 1998 and 2010 in Londrina, Southern Brazil. Rev Saude Publica. 2013;47(3):607–15.
Hoff SJ, Shotts SD, Eddy VA, Morris JA. Outcome of isolated pulmonary contusion in blunt trauma patients. Am Surg. 1994;60(2):138–42.
Carzolio-Trujillo HA, Navarro-Tovar F, Padilla-Gómez CI, Hernández-Martínez IA, Herrera-Enríquez J. Blunt chest trauma with pneumomediastinum and pneumoperitoneum secondary to Macklin effect. Case report. Cir Cir. 2016;84(5):409–14.
Mansella G, Bingisser R, Nickel CH. Pneumomediastinum in blunt chest trauma: a case report and review of the literature. Case Rep Emerg Med. 2014;2014:685381.
Ullman EA, Donley LP, Brady WJ. Pulmonary trauma emergency department evaluation and management. Emerg Med Clin N Am. 2003;21(2):291–313.
Klein Y, Cohn SM, Proctor KG. Lung contusion: Pathophysiology and management. Curr Opin Anaesthesiol. 2002;15(1):65–8.
Allen GS, Coates NE. Pulmonary contusion: a collective review. Am Surg. 1996;62(11):895–900.
Johnson SB. Tracheobronchial injury. Semin Thorac Cardiovasc Surg. 2008;20(1):52–7.
Donnelly LF, Strife JL, Lucaya J. Pediatric chest imaging: chest imaging in infants and children. Berlin: Springer; 2002.
Sartorelli KH, Vane DW. The diagnosis and management of children with blunt injury of the chest. Semin Pediatr Surg. 2004;13(2):98–105.
Stern EJ, White C. Chest radiology companion. Hagerstown: Lippincott Williams & Wilkins; 1999. p. 80.
Boyd AD. Lung injuries. In: Hood RM, Boyd AD, Culliford AT, editors. Thoracic trauma. Philadelphia: Saunders. 1989. p. 153–5.
Keough V, Pudelek B. Blunt chest trauma: review of selected pulmonary injuries focusing on pulmonary contusion. AACN Clin Issues. 2001;12(2):270–81.
Wanek S, Mayberry JC. Blunt thoracic trauma: flail chest, pulmonary contusion, and blast injury. Crit Care Clin. 2004;20(1):71–81.
Wicky S, Wintermark M, Schnyder P, Capasso P, Denys A. Imaging of blunt chest trauma. Eur Radiol. 2000;10(10):1524–38.
Miller DL, Mansour KA. Blunt traumatic lung injuries. Thorac Surg Clin. 2007;17(1):57–61.
Fleisher GR, Ludwig S, Henretig FM, Ruddy RM, Silverman BK. Thoracic trauma. Textbook of pediatric emergency medicine. Hagerstown: Lippincott Williams & Wilkins; 2006. p. 1434–41.
Bastos R, Calhoon JH, Baisden CE. Flail chest and pulmonary contusion. Semin Thorac Cardiovasc Surg. 2008;20(1):39–45.
Miller LA. Chest wall, lung, and pleural space trauma. Radiol Clin N Am. 2006;44(2):213–24.
Grueber GM, Prabhakar G, Shields TW. Blunt and penetrating injuries of the chest wall, pleura, and lungs. In: Shields TW. General thoracic surgery. Philadelphia: Lippincott Williams & Wilkins; 2005. p. 959.
Wiot JF. The radiologic manifestations of blunt chest trauma. JAMA. 1975;231(5):500–3.
Donnelly LF, Klosterman LA. Subpleural sparing: a CT finding of lung contusion in children. Radiology. 1997;204(2):385–7.
Wylie J, Morrison GC, Nalk K, Kornecki A, Kotylak TB, Fraser DD, et al. Lung contusion in children—early computed tomography versus radiography. Pediatr Crit Care Med. 2009;10(6):643–7.
Deunk J, Poels TC, Brink M, Dekker HM, Kool DR, Blickman JG, et al. The clinical outcome of occult pulmonary contusion on multidetector-row computed tomography in blunt trauma patients. J Trauma. 2010;68(2):387–94.
Soldati G, Testa A, Silva F. Chest ultrasonography in pulmonary contusion. Chest. 2006;130(2):533–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Požgain Zrinka, Kristek Dalibor, Lovrić Ivan, Kondža Goran, Jelavić Mario, Kocur Josip and Danilović Milijana state that they have no conflict of interest to declare.
Ethical approval
The study was approved by the local ethics committee at the Clinical Hospital Centre Osijek, Osijek University Hospital, and the Faculty of Medicine of the J.J. Strossmayer University of Osijek, Croatia, according to the Helsinki Declaration.
Rights and permissions
About this article
Cite this article
Požgain, Z., Kristek, D., Lovrić, I. et al. Pulmonary contusions after blunt chest trauma: clinical significance and evaluation of patient management. Eur J Trauma Emerg Surg 44, 773–777 (2018). https://doi.org/10.1007/s00068-017-0876-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-017-0876-5