Abstract
Purpose
In the last 10 years, there has been an increasing tendency toward operative fixation of clavicle fractures. In this retrospective analysis, we will demographically assess all patients who sustained a clavicle fracture and were treated in our university hospital between 2004 and 2014.
Methods
We retrospectively updated our database and analyzed all adult patients who were diagnosed with a clavicle fracture in our hospital. The following parameters were included in the database: age, gender, Robinson classification, date of trauma, injury mechanism, time until surgery, and reason for delayed surgery. Descriptive statistics were used to describe differences between patient groups and linear regression was performed to identify trends over time.
Results
667 patients were included for analysis. The mean age was 43 ± 17.7 years. The majority of clavicle fractures occurred due to bicycle injuries (35.3%) and these increased from 2004 until 2014 (r = 0.738, R² = 0.545, p = 0.009). Patients with a midshaft clavicle fracture were increasingly treated primarily surgically (r = 0.928, R² = 0.861, p < 0.0001). There was an increased ratio of delayed surgery in relation to age from the age of 16 (9.1%) until the age of 70 years (37.2%).
Conclusions
There is an increasing number of fractures sustained by bicycle accidents and an increasing number of patients undergoing operative treatment. Middle-aged patients more often had delayed surgery compared with young adult patients. This could be due to an increased activity level of the elder population and the concomitant demand for a faster return to activities.
Level of evidence
III, retrospective comparative study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although clavicle fractures are one of the most common fractures of the shoulder girdle, there is conflicting evidence regarding which clavicle fractures should be treated operatively [1, 2]. Huttunen et al. reported an increasing rate of operatively treated clavicle fractures in Scandinavia in the last 10 years [3, 4]. They believed that this increase could be due to recent literature which suggests that there are benefits for operative fixation with regard to faster rehabilitation, faster return to work, and faster and better restoration of function regarding certain kinds of fractures [5,6,7]. The aim of this retrospective study was to describe the demographics of patients who sustained a clavicle fracture and treatment strategy in a level 1 trauma center in Belgium over the last 10 years.
Patients and methods
Patients
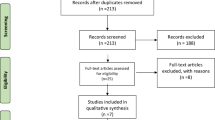
The study was performed in the only level 1 trauma center in Belgium. After obtaining approval from our local ethical committee, an electronic search string was set up to identify all emergency department reports between August 2004 and September 2016 which mentioned ‘clavicle’ and ‘fracture’. This query generated 1272 patient records, which were then identified for duplicates, and selected on patients being treated during the 2004–2015 period. Patients between the age of 16 and 90 years were of interest for our study. In total, 677 patient files were found eligible for inclusion. Data were collected manually from the electronic patient records and entered in a database form using Microsoft Excel.
Study variables
Age, gender, postal code, Robinson classification (type 1: medial fracture on the 1 fifth side of the bone [1A1: extra-articular undisplaced medial fracture; 1A2: intra-articular undisplaced medial fracture; 1B1: extra-articular displaced medial fracture; 1B2: intra-articular displaced medial fracture]; type 2: midshaft fracture [2A1: midshaft fracture with cortical alignment and undisplaced fragments; 2A2: midshaft fracture with cortical alignment and angulation; 2B1: displaced midshaft fracture—simple or wedge comminuted fracture; 2B2: displaced midshaft fracture—isolated or comminuted segmental fracture]; type 3: lateral fracture on the 1 fifth lateral end of the bone [3A1: extra-articular lateral fracture with cortical alignment; 3A2: intra-articular lateral fracture with cortical alignment; 3B1: extra-articular displaced lateral fracture; 3B2: intra-articular displaced lateral fracture—intra-articular] [8], open vs closed fractures, date of trauma X-ray, month of trauma, year of trauma, trauma mechanism [motorbike accident (MBA), motor vehicle accident (MVA), bicycle, sport, low-energy fall (LEF), high-energy fall (HEF), other, unknown mechanism], date of the surgical procedure, days until procedure, primary (< 14 days) vs delayed (< 14 days) surgery, reason for delayed surgery [non-union (radiographically assessed fractures which have not completely healed within 9 months of injury and without progression toward healing over the past three consecutive months) [9], delayed union (absence of clear radiographic signs of bone consolidation 4 months after the injury) [10], malunion (healing of the bone in a non-anatomical position which results in complaints from the patient), secondary displacement, pain, near skin perforation, second opinion, work/sport, pain + secondary displacement, unknown].
Statistical methods
Data were analyzed using SPSS 23. We decided to focus on descriptive statistics, correlation coefficients and linear regression analysis to obtain logical and clearly interpretable results. The patient’s geographical data were analyzed using QGIS 2.18.
Results
Demographics
677 patients were included in our retrospective cohort study: 141 women and 536 men with a mean age of 51.9 (SD 19.3) years for women and a mean age of 40.6 (SD 16.5) years for men (p < 0.001). The majority of patients came from the region around the University Hospital of Leuven which is the only level one trauma center in our country. The line dividing the country in half is the language border (Flemish–French speaking region) and the majority of our patients came from the Flemish-speaking region around our hospital (Fig. 1).
83.6% of all clavicle fractures occurred in patients between the age of 16 and 61 years. In the male patient group, there were two peaks regarding the age of injury: a first peak in the 21–30 years old age group and a second peak in the 41–50 years old age group (Fig. 2).
Trauma mechanism
In the 21–30 years old age group, the most important injury mechanisms were: bicycle accidents (30.5%), MBA (10.2%), MVA (18.8%) and sport-related injuries (18%). The majority of injuries occurred in the 41–50 years old age group and were mainly a consequence of bicycle (41.1%) and motorbike (17.8%) injuries (Table 1 and Fig. 3).
The mean age of our patients was different with regard to the trauma mechanism: MBA (39.2 ± 12.6), MVA (39.7 ± 17.3), bicycle (42.9 ± 14.3), sport (30.1 ± 12.9), LEF (51.4 ± 22.0) (HEF 54.6 ± 19.2), other mechanisms (42.2 ± 12.6) and unknown (43 ± 21.7). The differences in average age between bicycle accidents, sport-related injuries, low- and high-energy falls were statistically significant (p < 0.001). The difference in mean age between MBA, MVA, other mechanisms and unknown mechanisms was not statistically significant. Overall, from the age of 21 until the age of 70 years, the majority of injuries in our patient population was bicycle related (Table 1, Fig. 3).
The total number of clavicle fractures over the years did not increase significantly (Pearson’s r = 0.4326; R² = 0.1871; p = 0.1839) for the entire cohort. However, there was an increase in the absolute numbers of cycling-related injuries between 2004 and 2014 (Fig. 4). A linear regression analysis was performed and Pearsons’ r correlation coefficient was calculated for the different trauma mechanisms in function of the year. There was a small but statistically significant decrease in the number of MBA (r = − 0.612, R² = 0.374, p = 0.045), a large and significant increase in the number of cycling-related injuries (r = 0.738, R² = 0.545, p = 0.009), a small but significant increase in the number of sport-related injuries (r = 0.7, R² = 0.49, p = 0.016) and a decrease in high-energy falls (r = − 0.755, R² = 0.57, p = 0.007) between 2004 and 2014. The increase in the number of bicycle accidents was the most notable (Fig. 4).
Distribution of fracture type
There were 13 type 1 Robinson fractures: 8 male (1.2%), 5 female (0.7%); 518 type 2 Robinson fractures [422 male (62.3%), 96 female (14.2%)]; and 146 type 3 Robinson fractures [406 male (15.7%), 40 female (5.9%)]. Subgroup classification can be found in Table 2. The mean age of patients with a type 3 Robinson fracture (47.9 ± 18.8) was significantly higher than the mean age of patients with a type 2 Robinson fracture (41.23 ± 17.0, p < 0.001). There was no statistically significant difference in the mean age between type 1 and the two other types of Robinson fractures.
Treatment strategy
The treatment strategies will be presented according to the Robinson fracture type. Patients were grouped into those who had primary surgery (< 14 days), delayed surgery (> 14 days) or conservative treatment.
Robinson Type 1 The mean age of patients (13 cases) with a type 1 Robinson fracture was 56.8 (± 18) years. Three patients underwent primary surgery, one underwent delayed surgery and nine underwent conservative treatment. Due to the small number of patients with a type 1 fracture, these cases were excluded from further analysis.
Robinson Type 2 Patients with a midshaft clavicle fracture were increasingly treated surgically (r = 0.928, R² = 0.861, p < 0.0001) over the years. There was a linear decrease over time regarding the number of patients who was primarily treated conservatively. (r = − 0.761, R² = 0.579, p = 0.007). There was no significant variation in the number of patients who underwent delayed surgery (r = 0.5033, R² = 0.2534, p = 0.1145) as shown in Fig. 5. Reasons for delayed surgery in type 2 Robinson fractures were: non-union n = 12, 9.2%; delayed union n = 14, 10.7%; malunion n = 1, 0.8%; pain n = 25, 19.1%; pain and secondary displacement n = 13, 9.9%; secondary displacement n = 24, 18.3%; near skin perforation n = 9, 6.9%; work related n = 13, 9.9%; other n = 8, 6.1%; unknown n = 12, 9.2%. When the data were represented as the relative percentage of treatment type (primary, delayed or conservative treatment) per age group, there was an increasing percentage of patients undergoing delayed surgery until the age category of 61–70 years. After the age of 70, the total number of type 2 clavicle fractures diminished and the majority were treated conservatively (Fig. 6). This delay in surgery was mainly prominent in the Robinson type 2B clavicle fracture group for the 61–70 years old group (Table 3). The delayed surgeries in this age group were due to three non-unions, three delayed unions, two unresolved pain problems, three pain problems in combination with secondary displacement of the fracture fragments, two secondary displacements of the fracture fragments, two work-related reasons, two unknown reasons and one undefined reason (Table 4).
Robinson type 3 there were 147 type 3 Robinson fractures identified, consisting of 67 3A1 (45.6%), 5 3A2 (3.4%), 66 3B1 (44.9%) and 9 3B2 (6.12%) type fractures. The largest number of delayed surgery was within the 3B1 fracture group [11 cases (16.7%)]. There was no linear increase or decrease in the occurrence of type 3 clavicle fractures in the 2004–2014 period (r = − 0.019, R² = 0.004, p = 0.961). The number of primarily surgically treated type 3 clavicle fractures, however, did increase significantly in a linear way (r = 0.829, R² = 0.6872, p = 0.0016). This increase had an inverse relationship with the percentage of conservatively treated patients (Fig. 7). The total number of delayed surgeries in Robinson type 3 clavicle fractures was significantly lower in type 3 fractures compared with type 2 fractures (107 vs 13 delayed surgeries, or 20.7% vs. 8.9%). The reasons for delayed surgery per age category can be found in Table 5.
Discussion
Clavicle fractures have been considered as common fractures in young adults with a peak incidence under the age of 30 years for midshaft fractures and above the age of 70 for medial and lateral fractures [2, 11, 12]. Robinson et al. and Nordqvist et al. described a decreasing incidence of clavicle fractures until the age of 35 years, a more or less stable incidence until the age of 75 years and then again an increasing incidence with higher age [8, 13]. In our database, we identified two age peaks that should be taken into consideration: first, the earlier described peak in young male athletes and, second, the peak in middle-aged men (41–50 years old). Although we reported our results as the total number of patients per age group and not as the incidence/100,000 people, we believe that due to the constrictive age pyramid our data are in line with the age shift toward the middle aged. This age shift has also been reported in the Scandinavian population [3, 14]. Huttunen et al. described an increasing incidence of clavicle fractures in older age groups in the Swedish population. In their study, they suggested that the increased rate of injuries in older age groups may be caused by more active lifestyles of the middle aged [3]. Our data support this theory, as in our 51–60 years age group, 44.6% of all clavicle fractures were sustained due to bicycle injuries and 15.7% due to motorbike injuries.
The largest retrospective epidemiological study has reported an increasing number of clavicle fractures between 2001 and 2012 in Sweden [3]. Nordqvist et al. also reported this increasing incidence between 1952 and 1987 [13]. In our retrospective study, we were not able to validate a similar increase in the total number of clavicle fractures between 2004 and 2014. This could be due to the fact that our study is not register based, but single center based. Over the 1987–2012 period, two large Scandinavian studies reported a seven to ninefold increase in the surgical treatment of clavicle fractures [3, 4]. In our study, we also saw a linear increase in the number of midshaft and lateral clavicle fractures that were treated operatively.
Type 1 Robinson fractures are rare fractures, as shown in our cohort where they accounted for only 1.8% of all fractures. The largest series of type 1 Robinson fractures was published by Kihlström et al. who reported a total of 109 medial clavicle fractures over 2 years in all Swedish hospitals [14]. Due to the limited number of patients in our study, we excluded these patients for further analysis.
The treatment of type 2 clavicle fractures has been under debate among orthopedic trauma surgeons. There is only one high-quality study which demonstrates a clear functional benefit in the surgical treatment of displaced midshaft clavicle fractures [6]. Other studies report higher non-union rates, increased discomfort and upper limb weakness [15, 16]. These results are inconsistent and not all studies have been able to confirm these results [17, 18]. Our data showed an increasing number of surgically treated midshaft fractures in the 2004–2014 period, as also reported by other authors [3, 4, 19]. What is most remarkable, however, is the increasing number of delayed surgery with the increasing age of our patients. Although the total number of secondary surgeries in this group was small, up to 35% of the patients in the 61–70 years old group underwent delayed surgery for a variety of reasons such as union problems, pain and a demand for a faster return to normal activities. We therefore hypothesize that the increasing rate of surgically treated fractures was not only due to the surgeons change in motivation to operate, but also due to the active elderly population which preferred a faster return to function [3, 19]. Therefore, we believe it is important to treat patients according to their biological age and activity level and not only based on their calendar age. We also believe that if the surgeon advises to consider an operative treatment, the patient should engage in an early active rehabilitation program. Furthermore, the patient’s calendar age is relative and treatment possibilities and complications should be extremely well discussed with the patient.
As for the type 3 Robinson fractures, our patients had a higher mean age compared to type 2 fractures and their fractures happened more often due to low-energy traumas such as a low-energy fall (24.5% in total). The literature suggests that unstable and displaced (type 3B) fractures should be primarily treated surgically [20]. In our cohort, we saw a low percentage of delayed surgery (5.6% for type 3A fractures and 13.3% for type 3B fractures) and we believe that this was due to the available scientific evidence which shows less complications for operatively treated displaced fracture types [2, 21].
In conclusion, the average age of patients with a clavicle fracture shifted with our aging and active population. This age shift was mainly seen for midshaft (Robinson type 2) clavicle fractures where the majority of patients were middle aged and sustained their injury during recreational activities. Although the indications for surgical treatment are under debate, we believe it is important to treat patients according to their needs and biological age.
Abbreviations
- MBA:
-
Motorbike accident
- MVA:
-
Motor vehicle accident
- LEF:
-
Low-energy fall
- HEF:
-
High-energy fall
References
Woltz S, Sengab A, Krijnen P, Schipper IB. Does clavicular shortening after nonoperative treatment of midshaft fractures affect shoulder function? A systematic review. Arch Orthop Trauma Surg. http://www.ncbi.nlm.nih.gov/pubmed/28639075.
Khan LAK, Bradnock TJ, Scott C, Robinson CM. Fractures of the clavicle. J Bone Joint Surg. Am [Internet]. The American Orthopedic Association. 2009;91:447–60. http://www.ncbi.nlm.nih.gov/pubmed/19181992.
Huttunen TT, Launonen AP, Berg HE, Lepola V, Felländer-Tsai L, Mattila VM. Trends in the incidence of clavicle fractures and surgical repair in Sweden: 2001–2012. J Bone Joint Surg Am. 2016;98:1837–42. http://jbjs.org/cgi/doi/10.2106/JBJS.15.01284.
Huttunen TT, Kannus P, Lepola V, Pihlajamäki H, Mattila VM. Surgical treatment of clavicular fractures in Finland—a register based study between 1987 and 2010. Injury. 2013;44:1899–903. http://www.ncbi.nlm.nih.gov/pubmed/24091259.
Althausen PL, Shannon S, Lu M, O’Mara TJ, Bray TJ. Clinical and financial comparison of operative and nonoperative treatment of displaced clavicle fractures. J Shoulder Elbow Surg. 2013;22:608–11. http://www.ncbi.nlm.nih.gov/pubmed/22960145.
Canadian Orthopaedic Trauma Society T. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89:1–10. http://www.ncbi.nlm.nih.gov/pubmed/17200303.
Woltz S, Stegeman SA, Krijnen P, van Dijkman BA, van Thiel TPH, Schep NWL, et al. Plate fixation compared with nonoperative treatment for displaced midshaft clavicular fractures. J Bone Jt Surg. 2017;99:106–12. http://www.ncbi.nlm.nih.gov/pubmed/28099300.
Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br Engl. 1998;80:476–84.
Brinker M. Nonunions: evalution and treatment. In: Browner BD, Levine AM, Jupiter JB, Trafton PG, editors. Skeletal trauma basic science management reconstruction. 3rd ed. Philadelphia: Saunders, W.B.; 2003. pp. 507–604.
Acosta-Olivo C, Garza-Borjon A, Simental-Mendia M, Vilchez-Cavazos F, Tamez-Mata Y, Peña-Martinez V. Delayed union of humeral shaft fractures: comparison of autograft with and without platelet-rich plasma treatment: a randomized, single blinded clinical trial. Arch Orthop Trauma Surg. 2017. http://www.ncbi.nlm.nih.gov/pubmed/28667397.
Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. 1998;80:476–84. http://www.ncbi.nlm.nih.gov/pubmed/9619941.
Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37:691–7. http://www.ncbi.nlm.nih.gov/pubmed/16814787.
Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994;127–32. http://www.ncbi.nlm.nih.gov/pubmed/8131324.
Kihlström C, Möller M, Lönn K, Wolf O. Clavicle fractures: epidemiology, classification and treatment of 2422 fractures in the Swedish Fracture Register; an observational study. BMC Musculoskelet Disord. 2017;18:82. http://www.ncbi.nlm.nih.gov/pubmed/28202071.
Nowak J, Holgersson M, Larsson S. Can we predict long-term sequelae after fractures of the clavicle based on initial findings? A prospective study with nine to ten years of follow-up. J shoulder Elb Surg. 2004;13:479–86. http://www.ncbi.nlm.nih.gov/pubmed/15383801.
Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997;79:537–9. http://www.ncbi.nlm.nih.gov/pubmed/9250733.
Virtanen KJ, Remes V, Pajarinen J, Savolainen V, Björkenheim J-M, Paavola M. Sling compared with plate osteosynthesis for treatment of displaced midshaft clavicular fractures. J Bone Jt Surg Am Vol. 2012;94:1546–53. http://www.ncbi.nlm.nih.gov/pubmed/22832887.
Zhao J-G, Wang J, Long L. Surgical versus conservative treatments for displaced midshaft clavicular fractures: a systematic review of overlapping meta-analyses. Medicine (Baltimore). 2015;94:e1057. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4504624&tool=pmcentrez&rendertype=abstract.
Ban I, Nowak J, Virtanen K, Troelsen A. Overtreatment of displaced midshaft clavicle fractures. Acta Orthop. 2016;87:541–5. http://www.ncbi.nlm.nih.gov/pubmed/27225678.
van der Meijden OA, Gaskill TR, Millett PJ. Treatment of clavicle fractures: current concepts review. J Shoulder Elb Surg. 2012;21:423–9. https://www.ncbi.nlm.nih.gov/pubmed/22063756.
Kona J, Bosse MJ, Staeheli JW, Rosseau RL. Type II distal clavicle fractures: a retrospective review of surgical treatment. J Orthop Trauma. 1990;4:115–20. http://www.ncbi.nlm.nih.gov/pubmed/2358923.
Acknowledgements
The authors would like to thank Inge Meex, Mathias Roobroeck and Lisa ten Kate for helping with setting up the preliminary database. The authors would also like to thank Catherine Wickham for proofreading the final version of the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Michiel Herteleer, Thomas Winckelmans, Harm Hoekstra and Stefaan Nijs have no conflicts of interest.
Research involving human participants
This research has been approved by the ethical committee and their approval is added as file “59661 Nijs BD1 16NOV2016 GK signed.pdf”.
Informed consent
No informed consent was necessary, as this research is a retrospective chart review and approval by the ethical committee was obtained.
Rights and permissions
About this article
Cite this article
Herteleer, M., Winckelmans, T., Hoekstra, H. et al. Epidemiology of clavicle fractures in a level 1 trauma center in Belgium. Eur J Trauma Emerg Surg 44, 717–726 (2018). https://doi.org/10.1007/s00068-017-0858-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-017-0858-7