Abstract
Background
Trauma centers require reliable metrics to better compare the quality of care delivered. We compared mortality after a reported complication, termed failure to rescue (FTR), and FTR in the elderly (age >65 years) (FTRE) to determine which is a superior metric to assess quality of care delivered by trauma centers.
Methods
This was a retrospective review of the National Trauma Databank (NTDB) research data sets 2010 and 2011. Patients ≥16 years admitted to centers reporting ≥80% of AIS and/or ≥ 20% of comorbidities with > 200 subjects in the NTDB were selected. Centers were classified based on the rate of FTR and FTRE (<5 vs. 5–14 vs. ≥15%). The primary outcome was adjusted mortality for each group of trauma centers based on FTR and FTRE classifications.
Results
The overall mean ± SD FTR rate was 7.2 ± 5.2% and FTRE was 10.4 ± 7.9%. The adjusted odds ratio (AOR) for mortality was not different when centers with FTR <5% were compared to those with FTR of 5–14 or ≥15%. In contrast, a stepwise increase in FTRE predicted a significantly higher mortality when centers with FTRE 5% were compared to those with 5–14% (AOR: 1.05, p = 0.031) and ≥15% (AOR: 1.13, p < 0.001). Similarly, stepwise increase in FTRE predicted higher adjusted mortality for severely and critically injured patients, whereas FTR did not.
Conclusions and relevance
Higher FTRE predicts increased adjusted mortality better than FTR after trauma and should, therefore, be considered an important metric when comparing quality care delivered by trauma centers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The American College of Surgeons-Committee on Trauma (ACS-COT) is the leading authority at improving trauma-related outcomes. Trauma was the first medical specialty to develop regionalized systems of care by first establishing dedicated trauma centers in the 1970s and then systematically measuring health care outcomes at those centers [1]. Through the Major Trauma Outcomes Study (MTOS), the Trauma Injury Severity Score (TRISS) was developed to predict the probability of survival of a trauma patient, leading to comparison of observed to expected outcomes and to a more concise evaluation of trauma centers [2]. The Trauma Quality Improvement Program was developed in 2008 and is the latest major effort by the committee aiming to measure and improve the quality of care provided to trauma patients [3]. Within this process, quality metrics for trauma centers continue to be under focused investigation, as in-hospital mortality appears to be a problematic measure to assess the care provided [4].
Elderly patients are known to be at a high risk for mortality following trauma [5, 6]. We have previously demonstrated that increasing age is not only associated with a higher mortality, but also with a stepwise increase in the risk for failure to rescue (FTR), defined as a mortality following any in-hospital complication [7]. Rapid recognition and treatment of complications are critical determinants of patient outcome and likely constitute an indicator of quality care provided by trauma centers. FTR elderly (FTRE) is possibly a more accurate measure of this care, as elderly patients require even more resources compared to younger trauma patients. Therefore, the trauma centers’ ability to respond to complications in the elderly and provide treatment to prevent mortality should be the focus of quality improvement for organizations and policy makers.
The aim of this study was to evaluate whether FTRE is a superior metric compared to FTR in assessing quality care provided by trauma centers based on adjusted mortality. We hypothesized that admission to a trauma center with high FTRE would be associated with a significantly higher adjusted mortality compared to high FTR.
Methods
The National Trauma Databank (NTDB) Research Data Sets 2010 and 2011 were combined for the purposes of the analysis. Subjects who were younger than 16 years, those who expired in the emergency department (ED), those with lethal injuries including any body region abbreviated injury scale (AIS) of 6 or injury severity score (ISS) of 75, and those with unknown hospital disposition were excluded. The data were then aggregated and patients admitted to trauma centers reporting less than 200 subjects over the age of 65 years to the NTDB over the 2-year study period were also excluded. A database combining the variables age, gender, ACS trauma center designation, ED systolic blood pressure (SBP), ED Glasgow Coma Scale (GCS), all body regions AIS, ISS, comorbid conditions, complications, and hospital disposition was created. Clinically, relevant cut points were created, including ED SBP <90 mmHg, ED GCS ≤8, and AIS all body regions ≥3. Cardiac disease was defined as history of congestive heart failure, angina, and/or myocardial infarction, and liver disease was defined as history of cirrhosis, esophageal varices, and/or ascites.
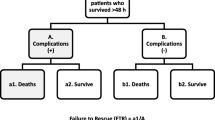
Complications and mortality were then reviewed, and FTR was defined as a mortality following any reported complication. Complications that are captured by the NTDB include abdominal compartment syndrome, extremity compartment syndrome, open abdomen, acute renal failure, acute respiratory distress syndrome (ARDS), bleeding, coagulopathy, cerebrovascular accident (CVA), cardiac arrest, myocardial infarction, severe sepsis, systemic sepsis, pneumonia, urinary tract infection, catheter-related blood-stream infection, superficial surgical site infection, deep surgical site infection, organ surgical site infection, osteomyelitis, decubitus ulcer, deep venous thrombosis (DVT), pulmonary embolus, graft failure, unplanned intubation, unplanned take back to the operating room, dehiscence, elevated intracranial pressure, and alcohol withdrawal. The rates of FTR and FTRE (defined as mortality following any reported complication in a patient over the age of 65 years) were calculated for each trauma center. All centers were then classified into three groups based on their FTR (<5, 5–14 and ≥15%) and FTRE rates (<5, 5–14 and ≥15%). Patients admitted to each group of trauma centers based on FTR rate were then compared using analysis of variance (ANOVA) or Chi square. A logistic regression model was utilized to adjust for differences between the three groups (variables with p < 0.05). The group of patients that was admitted to centers with the lowest FTR rate (<5%) was used as the reference group to calculate the adjusted odds ratio (AOR) and 95% confidence intervals (95% CI) for mortality in the groups of patients that were admitted to centers with FTR 5–14% and FTR ≥15%. The same process was then applied for the groups of patients admitted to centers classified based on their FTRE rate, and the adjusted mortality was obtained in the same manner. Finally, the adjusted mortality was also examined within subgroups of patients with severe (ISS >16) and critical injuries (ISS ≥25).
All statistical analyses were performed using the IBM SPSS Statistics for Windows, Version 19.0 (Armonk, NY: IBM Corp.).
Results
Baseline characteristics of included trauma centers
A total of 1,496,135 subjects were included in the NTDB over the 2-year study period. After excluding patients younger than 16 years, ED deaths, patients with lethal injuries (any body region AIS of 6 and/or ISS of 75), patients with unknown hospital disposition, and patients admitted to centers reporting less than 200 patients over the age of 65 years to the NTDB during the 2-year study period, 937,483 subjects (62.7%) were left for analysis (Fig. 1).
In this process of excluding subjects who did not meet criteria, 334 of the 753 trauma centers included in the original data set were excluded. The mean ± SD overall admissions for each of the remaining 419 centers over the 2-year period were 2232 ± 1518 patients, while admissions of patients >65 years were 642 ± 379. The overall mean ± SD mortality per center was 3.4 ± 1.1%, and mortality for patients >65 years was higher, at 5.5 ± 2.6%. Similarly, the FTR rate was 7.2 ± 5.2% and FTRE was 10.4 ± 7.9%. All centers were classified into three groups based on their FTR and FTRE rates.
Comparison based on FTR and FTRE rates
Patients were compared by FTR classification of the trauma centers (Table 1). Patients admitted to high-risk centers for FTR (≥15%) were more likely to have an ED GCS ≤8 (6.6 vs. 7.3 vs. 7.9%, p < 0.001), severe thoracic trauma with an AIS chest ≥3 (15.4 vs. 16.3 vs. 16.6%, p < 0.001), and a history of cardiac disease (6.0 vs. 7.4 vs. 7.8%, p < 0.001); however, they were less likely to have severe lower extremity injury with AIS ≥3 (18.0 vs. 17.2 vs. 16.7%, p < 0.001). Patients were then compared based on FTRE classification of the trauma centers (Table 2). Patients admitted to high-risk FTRE centers (≥15%) were more likely to be male (58.2 vs. 62.7 vs. 65.2%, p < 0.001), to have penetrating trauma (6.6 vs. 8.8 vs. 10.7%, p < 0.001), ED GCS ≤8 (5.7 vs. 7.2 vs. 7.9%, p < 0.001), and a history of pulmonary disease (9.1 vs. 10.8 vs. 11.2%, p < 0.001); however, they were less likely to have a bleeding disorder (6.6 vs. 7.2 vs. 5.9%, p < 0.001).
Mortality analysis based on FTR and FTRE
The crude mortality among centers increased as the classification (<5, 5–14 and ≥15%) of FTR and FTRE increased: 3.1 vs. 3.5 vs. 3.8% for FTR compared to 2.8 vs. 3.4 vs. 3.7% for FTRE (Table 3). After adjusting for differences among the three groups, there was no difference in the adjusted mortality when centers with FTR <5% were compared to centers with FTR of 5–14 or ≥15% (Table 3). In contrast, a stepwise increase in FTRE was associated with a stepwise increase in the risk for death, with FTRE centers between 5–14% and those ≥15% having a significantly higher adjusted mortality (AOR 1.05; 95% CI 1.01, 1.09; p = 0.031 and AOR: 1.13; 95% CI 1.07, 1.18; p < 0.001, respectively) (Table 3). The adjusted odds for mortality were then calculated within the subgroup of patients with severe injuries (ISS >16). Similarly, increase in the FTR rate did not correlate with a significant increase in the adjusted odds for mortality; however, increase in the FTRE rate was associated with a significantly increased risk for adjusted mortality (Table 4). Even for critical injuries (ISS ≥25), increase in the FTRE rate was again associated with an increase in the adjusted risk for mortality (AOR: 1.16; [95% CI 1.08, 1.24]; adjusted p < 0.001 and AOR: 1.16; [95% CI 1.08, 1.26]; and adjusted p < 0.001 for FTRE 5–14 and ≥15%, respectively) (Table 5).
Discussion
We herein demonstrate that FTRE is a superior metric to FTR when assessing trauma centers’ quality of care. When trauma centers were classified by FTRE of <5, 5–14 or ≥15%, significant differences were noted in adjusted mortality, in contrast to the same FTR classification which was not associated with any differences in adjusted mortality. Our findings were similar for patients with severe (ISS >16) and critical injuries (ISS ≥25). Therefore, FTRE is likely a better and a more useful quality metric for trauma centers when compared to FTR (see Table 5).
The Centers for Medicare and Medicaid Services (CMS) developed value-based purchasing to reward providers who deliver better outcomes in healthcare at a lower cost [8], indicating a rapid advancement in how healthcare providers are evaluated. This transition arrives with new shifts in the demographics and characteristics of patients admitted to trauma centers. The United States (U.S.) Census Bureau projects a substantial increase in the population age 65 and older which is expected to exceed 90 million individuals and to represent one in five US residents by the year 2060, while those 85 and older will reach 4.3% of the total population by the same year [9]. Although trauma continues to represent one of the leading causes of death, the distribution of these deaths among the population is also being shifted. Individuals in their fifth decade of life had 118% proportional increase in crude trauma deaths over the decade 2000–2010 [10]. Trauma accounts for almost 3 million admissions and over 180,000 deaths annually [11], and these come with a staggering cost exceeding $400 billion [12, 13]. The quality of trauma care is not tied to hospital payments yet, and as of now, outcomes for trauma patients are not publicly reported. However, with these impending changes, an increasingly aging trauma patient population and rising healthcare costs, identifying quality metrics for trauma centers that can lead to improved outcomes and decreased costs remains a pressing issue.
Currently inter-hospital performance comparisons for trauma centers are based on external benchmarking utilizing a standardized methodology which accounts for observed to expected mortality ratios [14]. This information is then provided to trauma centers to guide them in the development of initiatives that may lead to quality improvement and enhanced outcomes. This methodology, however, has serious limitations and is a poor predictor of quality care [4, 15]. In addition, the current benchmarking has been questioned as a statistical tool, as it results in variation in risk-adjusted mortality that leads to nearly one of every six hospitals in the NTDB being inappropriately placed among the very best or very worst quintile of rankings [16]. Shafi et al. examined the charts of a random sample of 1,000 patients admitted to a Level I trauma center and found that despite availability of adequate resources, almost half of these patients did not receive trauma-specific clinical processes of care with the median compliance score being 60 (interquartile range 29–100), suggesting that half of the patients only received 60% of the care they needed. In this patient population, every 10% increase in compliance was associated with a 14% reduction in risk-adjusted in-hospital mortality [17]. These findings suggest that examining only adjusted mortality to identify high performers among trauma centers is at least problematic and the conclusions made based upon this outcome may be potentially misleading.
Although FTR was defined almost 20 years ago [18], it has recently emerged again as a quality metric for trauma and other healthcare centers, especially with implementation of the Affordable Care Act. FTR has been shown to better explain variations in mortality among surgical patients admitted to different surgical centers [19–21]. In Cardiac Surgery, FTR appears to be the sole determinant of quality care, even among pediatric patients [22, 23]. For trauma centers in particular, Glance et al. showed that the primary driver of differences in hospital quality for trauma patients is FTR, as opposed to differences in complication rates [24]. FTR may, therefore, be a better determinant of quality care compared to adjusted mortality risk. Nonetheless, the role of age in FTR rates for healthcare centers has not been well delineated. We previously demonstrated that for trauma patients, increasing age is associated with a stepwise increase in the risk for FTR and in the risk for increasing number of complications [7]. Herein, we explored the role of FTRE as a quality metric and we determined that for trauma centers, compared to the rate of FTR, the rate of FTRE is a better predictor of overall adjusted mortality, indicating that FTRE is a better determinant of quality of care. This applied to trauma patients with varied injuries, including those with severe (ISS >16) and critical injuries (ISS ≥25).
Timely recognition and effective management of a complication in a trauma patient are probably the two most important factors in preventing FTR. These two factors are even more critical when it comes to an elderly injured patient, as the risk for death in this setting is significantly higher [5, 6, 25]. Elderly patients are more prone to underlying comorbidities and more likely to require added resources when they experience in-hospital complications [26]. Based on our results, trauma centers with established structures, teams, and tools that can facilitate early recognition of complications, allow for fast and aggressive actions to prevent FTRE, and appear to provide higher level of care overall, as patients treated at these centers have a significantly higher chance of survival, independent of their injury severity and age. These findings are in line with the work published by Haas et al. demonstrating that trauma centers with low overall mortality are more successful at rescuing patients who experience complications [27].
Identification of practices, tools, and structures that allow trauma centers to provide a higher level of care is not feasible using the NTDB. A plethora of literature offers protocols and procedures that improve outcomes for medical geriatric patients [28, 29]; however, very little is currently known about how elderly trauma patients may benefit from institutional programs that specifically address the issues of early recognition and effective management of an in-hospital complication to prevent FTRE. Geriatric trauma consultation service for trauma patients older than 60 years has been shown to decrease the incidence of delirium and increase the likelihood of discharge to home [30]. A geriatric trauma protocol at the Lancaster General Hospital in Pennsylvania which included a geriatric medicine consultation and monitoring in an intensive care setting was associated with a 31% reduction in the risk for death [31]. Matsushima et al. highlighted the importance of differentiated pathways of care for these injured patients in a study showing the association between a higher volume of geriatric trauma patients with improved overall survival [32]. Compliance of trauma centers with practice management guidelines is essential for improving survival [17], and this is of predominant importance when it comes to the management of the elderly trauma patient.
We recognize the limitations of our analysis, as it is well known that the NTDB does not contain a nationwide representative sample population, although the high number of subjects included in the data set allows for risk-adjusted analyses. Under-reporting of data elements in the data set is possible; we, therefore, sought to minimize its impact by excluding subjects admitted to trauma centers which under-report AIS and complications. The validity of reported complications cannot be assessed and no measure of the severity of these complications is available. The association between the reported complication and subsequent death cannot be verified. Do not resuscitate (DNR) status was not accounted for, and it is unknown whether this status was present prior to or after the development of complications. The data analyzed were not from recent data sets, and these findings may not apply if more recent data sets were utilized. Moreover, morbidity and complications usually precede a mortality; however, most deaths in this data set did not have a reported complication, possibly due to under-reporting. As noted in our results, centers with the higher FTR and FTRE had decreased incidence of reported complications. Therefore, a low FTR or FTRE rate might be an indicator for more aggressive and intensive care in patients developing a complication, but might also indicate a more detailed documentation and reporting of these complications. Often, treatment decisions might also lead to complications and these decisions could not be accounted for. Most importantly, however, our study design did not allow for identification of those common practices among trauma centers that provided higher quality care and improved survival.
In conclusion, trauma centers require reliable metrics to better compare the quality of care delivered. Higher FTRE predicts increased adjusted mortality better than FTR after any severe trauma or critical trauma. Rescuing an elderly trauma patient from death after the development of an in-hospital complication is a quality metric for trauma centers that indicates better overall survival for any trauma patient, independent of injury severity or age. Identification of those practices and interventions that result in a lower incidence of failure to rescue an elderly patient following a traumatic injury should be the focus of future research. Promoting and sponsoring interventional trials designed to establish measures that results in rapidly recognizing those patients who require urgent and emergent intervention following a complication are expected to result in the development of quality improvement practices.
References
American College of Surgeons. Resources for optimal care of the injured patient. Am Coll Surg. 2006;98.
Champion HR, Copes WS, Sacco WJ, et al. The major trauma outcome study: establishing national norms for trauma care. J Trauma. 1990;30(11):1356–65. http://www.ncbi.nlm.nih.gov/pubmed/2231804. Accessed 2 June 2014.
Hemmila MR, Nathens AB, Shafi S, et al. The trauma quality improvement program: pilot study and initial demonstration of feasibility. J Trauma. 2010;68(2):253–62.
Hashmi ZG, Schneider EB, Castillo R, et al. Benchmarking trauma centers on mortality alone does not reflect quality of care: implications for pay-for-performance. J Trauma Acute Care Surg. 2014;76(5):1184–91.
Demetriades D, Karaiskakis M, Velmahos G, et al. Effect on outcome of early intensive management of geriatric trauma patients. Br J Surg. 2002;89(10):1319–22.
Goodmanson NW, Rosengart MR, Barnato AE, Sperry JL, Peitzman AB, Marshall GT. Defining geriatric trauma: when does age make a difference? Surgery. 2012;152(4):668–74. (discussion 674–5).
Barmparas G, Martin M, Wiegmann DA, et al. Increased age predicts failure to rescue. Am Surg. 2016;82(11):1073–9. (7).
VanLare JM, Conway PH. Value-based purchasing–national programs to move from volume to value. N Engl J Med. 2012;367(4):292–5.
U.S. Census Bureau DIS. 2012 National Population Projections. http://www.census.gov/population/projections/data/national/2012.html. Accessed 20 Mar 2014.
Rhee P, Joseph B, Pandit V, et al. Increasing trauma deaths in the United States. Ann Surg. 2014;260(1):13–21.
WISQARS (Web-based Injury Statistics Query and Reporting System)|Injury Center|CDC. http://www.cdc.gov/injury/wisqars/. Accessed 15 June 2014.
Corso P, Finkelstein E, Miller T, Fiebelkorn I, Zaloshnja E. Incidence and lifetime costs of injuries in the United States. Inj Prev. 2006;12(4):212–8.
Velopulos CG, Enwerem NY, Obirieze A, et al. National cost of trauma care by payer status. J Surg Res. 2013;184(1):444–9.
Nathens AB, Cryer HG, Fildes J. The American college of surgeons trauma quality improvement program. Surg Clin North Am. 2012;92(2):441–54. x–xi.
Sharma S, de Mestral C, Hsiao M, et al. Benchmarking trauma center performance in traumatic brain injury: the limitations of mortality outcomes. J Trauma Acute Care Surg. 2013;74(3):890–4.
Hashmi ZG, Dimick JB, Efron DT, et al. Reliability adjustment: a necessity for trauma center ranking and benchmarking. J Trauma Acute Care Surg. 2013;75(1):166–72. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3989535&tool=pmcentrez&rendertype=abstract. Accessed 21 Dec 2014.
Shafi S, Rayan N, Barnes S, Fleming N, Gentilello LM, Ballard D. Moving from “optimal resources” to “optimal care” at trauma centers. J Trauma Acute Care Surg. 2012;72(4):870–7.
Silber JH, Rosenbaum PR. A spurious correlation between hospital mortality and complication rates: the importance of severity adjustment. Med Care. 1997;35(10 Suppl):OS77–OS92. http://www.ncbi.nlm.nih.gov/pubmed/9339779. Accessed 21 Mar 2014.
Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009;361(14):1368–75.
Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Ann Surg. 2009;250(6):1029–34. http://www.ncbi.nlm.nih.gov/pubmed/19953723. Accessed 21 Mar 2014.
Ghaferi AA, Osborne NH, Birkmeyer JD, Dimick JB. Hospital characteristics associated with failure to rescue from complications after pancreatectomy. J Am Coll Surg. 2010;211(3):325–30.
Ahmed EO, Butler R, Novick RJ. Failure-to-rescue rate as a measure of quality of care in a cardiac surgery recovery unit: a five-year study. Ann Thorac Surg. 2014;97(1):147–52.
Pasquali SK, He X, Jacobs JP, Jacobs ML, O’Brien SM, Gaynor JW. Evaluation of failure to rescue as a quality metric in pediatric heart surgery: an analysis of the STS Congenital Heart Surgery Database. Ann Thorac Surg. 2012;94(2):573–9 (discussion 579–80).
Glance LG, Dick AW, Meredith JW, Mukamel DB. Variation in hospital complication rates and failure-to-rescue for trauma patients. Ann Surg. 2011;253(4):811–6.
Taylor MD, Tracy JK, Meyer W, Pasquale M, Napolitano LM. Trauma in the elderly: intensive care unit resource use and outcome. J Trauma. 2002;53(3):407–14.
McKevitt EC, Calvert E, Ng A, et al. Geriatric trauma: resource use and patient outcomes. Can J Surg. 2003;46(3):211–5. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3211738&tool=pmcentrez&rendertype=abstract. Accessed 21 Dec 2014.
Haas B, Gomez D, Hemmila MR, Nathens AB. Prevention of complications and successful rescue of patients with serious complications: characteristics of high-performing trauma centers. J Trauma. 2011;70(3):575–82.
Asplund K, Gustafson Y, Jacobsson C, et al. Geriatric-based versus general wards for older acute medical patients: a randomized comparison of outcomes and use of resources. J Am Geriatr Soc. 2000;48(11):1381–8. http://www.ncbi.nlm.nih.gov/pubmed/11083312. Accessed 22 Dec 2014.
Landefeld CS, Palmer RM, Kresevic DM, Fortinsky RH, Kowal J. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332(20):1338–44.
Lenartowicz M, Parkovnick M, McFarlan A, et al. An evaluation of a proactive geriatric trauma consultation service. Ann Surg. 2012;256(6):1098–101.
Bradburn E, Rogers FB, Krasne M, et al. High-risk geriatric protocol: improving mortality in the elderly. J Trauma Acute Care Surg. 2012;73(2):435–40.
Matsushima K, Schaefer EW, Won EJ, Armen SB, Indeck MC, Soybel DI. Positive and negative volume-outcome relationships in the geriatric trauma population. JAMA Surg. 2014;149(4):319–26.
Author contributions
Study conception and design: GB, MD; MM, MD; BLG, MD; and EJL, MD. Acquisition of data: GB, MD; AK, MD; MH, BS; and EJL, MD. Analysis and interpretation of data: GB, MD; MM, MD; and EJL, MD. Literature review: GB, MD; MM, MD; and EJL, MD. Drafting of manuscript: GB, MD; MM, MD; BLG, MD; and EJL, MD. Critical revision: DAW, PhD; KRC, PhD; BLG, MD; and EJL, MD.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to report and have received no financial support in relation to this manuscript.
Rights and permissions
About this article
Cite this article
Barmparas, G., Ley, E.J., Martin, M.J. et al. Failure to rescue the elderly: a superior quality metric for trauma centers. Eur J Trauma Emerg Surg 44, 377–384 (2018). https://doi.org/10.1007/s00068-017-0782-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-017-0782-x