Abstract
Introduction
Intravascular volume and fluid replacement are still cornerstones to correct fluid deficits during early trauma resuscitation, but optimum strategies remain under debate.
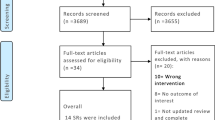
Methods
A synopsis of best current knowledge with reference to the following guidelines and recommendations is presented: (1) The European Guideline on Management of Major Bleeding and Coagulopathy following Trauma (fourth edition), (2) S3 Guideline on Treatment of Patients with Severe and Multiple Injuries [English Version of the German Guideline S3 Leitlinie Polytrauma/Schwerverletzten-Behandlung/AWMF Register-Nr. 012/019 sponsored by the German Society for Trauma Surgery/Deutsche Gesellschaft für Unfallchirurgie (DGU)], and (3) S3 Guideline Intravascular Volume Treatment in the Adult [AWMF Register-Nr 001/020 sponsored by the German Society for Anesthesiology and Intensive Medicine/Deutsche Gesellschaft für Anästhesiologie und Intensivmedizin (DGAI)].
Results and conclusions
Volume replacement at a reduced level in severely injured and bleeding trauma patients is advocated (permissive hypotension) until the bleeding is controlled. ATLS principles with Hb, BE, and/or lactate can assess perfusion, estimate/monitor the extent of bleeding/shock, and guide therapy. Isotonic crystalloid solutions are first-line and specific recommendations apply for patients with TBI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intravascular volume and fluid replacement are still cornerstones to correct fluid deficits during early trauma resuscitation [1, 2]. Volume replacement principally aims to increase intravascular volume, cardiac preload and output, global oxygenation, and microvascular perfusion [3, 4]. The potentially detrimental effects of early and aggressive volume replacement including (1) dilution and hypothermia deteriorating coagulation function, (2) volume overload triggering lung injury and abdominal compartment syndrome (ACS), and (3) increase in blood and hydrostatic pressure to interfere with wound healing and further blood loss have equally been recognized [5–7], and resulted in the introduction of the damage control resuscitation (DCR) concept [8]. This concept represents the natural evolution of the initial concept of damage control surgery tolerating lower than normal systolic blood pressure (permissive hypotension) during early trauma resuscitation via restricted volume replacement [8, 9].
Retrospective data confirmed liberal volume administration during the pre-hospital phase of care still as an independent risk factor for mortality in trauma [10]. In recognizing the detrimental effects associated with the liberal use of resuscitation fluids during early trauma resuscitation, the total amount of fluids administered to trauma patients captured into the German TraumaRegister DGU® (TR-DGU®; ISS ≥16) was reduced by 50% between 2002 and 2014 (Fig. 1). During the same time interval and in the same cohort, the occurrence of coagulopathy upon Emergency Room (ER) arrival as reflected by standard coagulation assays decreased from 35% in 2002 to 18% in 2014, while mean ER haemoglobin levels increased (Fig. 1). Substantial differences in trauma fluid resuscitation practice during both pre- and early in-hospital phases of care exist between TR-DGU®-affiliated trauma centers and Emergency Medical Services (EMS; Fig. 2).
Mean total amounts of resuscitation fluids administered to trauma patients during the pre-hospital phase of care versus emergency room (ER) admission haemoglobin (g/dl; black squares) and ER frequency of coagulopathy (%; INR >1.3 and/or platelets <100,000/μl; black circles). The total amount of volume replacement decreased from mean 1604 ml in 2002 to 789 ml (50%) in 2014. Simultaneously, there was less coagulopathy and higher levels of haemoglobin observed upon ER admission (German TraumaRegister DGU®; German level 1 hospitals only; primary admissions with ISS ≥16; 2020–2014; n = 44,829)
Pre- and early in-hospital resuscitation fluids in milliliters (means ± SD in mls) administered to trauma patients [primary admissions; Injury Severity Score (ISS) ≥ 16] admitted and treated in level 1 trauma centers affiliated to the German TraumaRegister DGU® over the last 5 years (2010–2014; n = 35,807)
A recently updated Cochrane review on timing and volume of intravenous fluid administration for trauma patients with bleeding including six randomised trials (n = 2,128) found no evidence for or against early versus late and larger versus smaller volume replacement in uncontrolled haemorrhage [11], but prospective preliminary data suggest hypotensive resuscitation even tolerating mean arterial pressures (MAP) of as low as 50 mmHg to be safe resulting in a significant reduction in blood transfusion, intravenous fluid administration, coagulopathy, and early postoperative death [12]. Interestingly, the first version of the Cochrane review was published in 2000 and had already included the six cited trials; the authors have searched for new, relevant studies in 2003, 2008, and 2014, but no additional studies were found. The next search is planned for 2020.
Methods
As there is continuing uncertainty about the optimum fluid resuscitation strategy in bleeding trauma patients, a synopsis of best current knowledge with reference to the following guidelines and recommendations is presented:
-
1.
The European Guideline on Management of Major Bleeding and Coagulopathy following Trauma, fourth edition 2016 (EU GRADE) [13].
-
2.
S3 Guideline on Treatment of Patients with Severe and Multiple Injuries (English Version of the German Guideline S3 Leitlinie Polytrauma/Schwerverletzten-Behandlung/AWMF Register-Nr. 012/019 (07/2016) sponsored by the German Society for Trauma Surgery/Deutsche Gesellschaft für Unfallchirurgie (DGU); S3-DGU) [14].
-
3.
S3 Guideline Intravascular Volume Treatment in the Adult (AWMF Register-Nr 001/020 sponsored by the German Society for Anesthesiology and Intensive Medicine/Deutsche Gesellschaft für Anästhesiologie und Intensivmedizin (DGAI); S3-DGAI) [15].
The recommendations given by the European trauma guideline are graded according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system [16]. The number associated with the recommendation reflects the strength of the recommendation being Grade 1 considered as the authors group´s strong recommendation and being Grade 2 considered as the authors group's weak recommendation/suggestion; the following letter reflects the quality of the scientific evidence ranging from A (high-quality evidence) to C (low-quality evidence). The evidence statements for the recommendations given for the two S3 Guidelines (AWMF Register-Nr 012/019 and 001/020) are based upon the AWMF-Regelwerk Leitlinien and the evidence classification system of the Oxford Center of Evidence-Based Medicine (CEBM), Version March 2009, where priority is given to studies with the highest Level of Evidence (LoE) available [17]. Within this system, three grades of recommendations (GoR) are possible, e.g., A (strong recommendation), B (recommendation), and 0 (open recommendation), where the wording corresponds to must, should, or can. The GoRs indicate to what extent recommended actions lead to a patient-relevant benefit or avoidance of harm respectively.
The present synopsis is focused on intravascular volume replacement in the context of early trauma resuscitation; it does not consider the use of blood products. As an introductory statement, important and theoretical recommendations concerning fluid und volume therapies cannot be safely given at this stage due to lack of sound evidence (S3-DGAI GoR -). Pre-interventional volume deficiency should be balanced prior to intervention (S3-DGAI GoR B).
Current guidelines and recommendations
In normotensive trauma patients with absent signs for volume deficit, fluid replacement therapy can be neglected (S3-DGU GoR 0), but intravenous lines be inserted (S3-DGU GoR A). In severely injured and hypotensive trauma patients, volume replacement should be initiated, at a reduced level, if there is uncontrollable bleeding, to keep the circulation stable at target blood pressure and not exacerbate the bleeding until the bleeding can be controlled (S3-DGU GoR B; EU GRADE 1B). The updated S3-DGU guideline and the European trauma guideline suggest for adult trauma patients with active bleeding to conduct permissive hypotension with target MAP 65 mmHg and/or with target SBP (systolic blood pressure) 80–90 mmHg until major bleeding control has been achieved (S3-DGU GoR B; EU GRADE 1C). Recent data with low evidence suggest to tolerate even lower MAPs as 50 mmHg until surgical control is achieved but only after an injury to the central nervous system (CNS) or an underlying cardiovascular disease have been ruled out (S3-DGU GoR 0). If rapid volume resuscitation is needed in the peri-interventional setting, pressure infuser bags or rapid infusion pumps should be used (S3-DGAI GoR B).
Diagnosis and monitoring
The European trauma guideline recommends to assess the extent of traumatic haemorrhage via a combination of patient physiology, anatomical injury pattern, mechanism of injury, and the patient's response to the initial resuscitation according to the ATLS concept (Advanced Trauma Life Support; EU GRADE 1C). This concept suggests four classes of hypovolemic shock based upon the initial presentation which trigger specific strategies for the initial fluid replacement [18]. Functional haemodynamic monitoring including ventilation manoeuvers and fluid challenge via administration of defined volume boluses may increase the sensitivity to detect, assess, and guide volume deficits and replacement (S3-DGAI GoR 0). The ATLS concept describes three types of responses to the initial bolus administration using 2000 ml of isotonic crystalloid fluid challenge, i.e., (1) rapid response with vital signs to return to normal, (2) transient response with transient improvement, and (3) minimal to no response with vital signs to remain abnormal after the fluid challenge. If the source for haemodynamic instability is unclear, transthoracic echocardiography (TTE) is recommended, in particular if cardiac origin is suspected (S3-DGAI GoR A). Early and repeated ultrasound, e.g., in the context of focused assessment sonography in trauma (FAST), is recommended to detect or exclude extravasal fluid, e.g., in the pleural space, abdomen, interstitium, etc., in particular in patients with suspected torso trauma (S3-DGAI GoR B; EU GRADE 1B).
Laboratory and physiological parameters
Low initial haemoglobin (Hb) is considered indicative for severe bleeding and repeated Hb measurements are recommended as an initial value within reference ranges may mask the bleeding (EU GRADE 1B). Laboratory parameters to assess and monitor volume deficits and shock include lactate, ScvO2, haematocrit, and base excess (BE; S3-DGAI GoR A). The updated S3-DGU guideline as well as the European trauma guideline advocate repeated and independent measurements of BE and/or lactate as sensitive tests to assess adequate perfusion, to estimate and monitor the extent of bleeding and shock, and to guide volume replacement therapy (S3-DGU GoR A; EU GRADE 1B). The target BE to therapeutically aim for is less than −6 mEq/l. The reliability of lactate may be lower when trauma is coincidence with alcohol consumption; in these cases, BE may be a superior predictor. Recently, data derived from the TR-DGU® showed that BE upon ER admission may be superior over the ATLS classification of haemodynamic shock in predicting need for volume including transfusion and mortality [19].
In spontaneous breathing as well as in intubated and mechanically ventilated patients, the central venous pressure (CVP) to assess volume deficits in the perioperative setting as well in the intensive care setting should not be used (S3-DGAI GoR A). Repeated responses to volume challenge may be assessed via maneuvers that trigger autotransfusion, stroke volume measurement, and dynamic preload parameters (S3-DGAI GoR B) which should be preferred against static parameters, such as CVP (S3-DGAI GoR A). Parameters based upon blood flow to guide volume replacement should be incorporated into treatment algorithms (S3-DGAI GoR B). Functional haemodynamic parameters should be judged in context of the clinical presentation and history (S3-DGAI GoR A).
Choice of resuscitation fluid
Isotonic crystalloid solutions should be used as fluids of choice for volume replacement in hypotensive bleeding trauma (S3-DGU GoR B; EU GRADE 1A) and intensive care patients (S3-DGAI GoR B). Balanced crystalloid and isotonic full electrolyte solutions are recommended for trauma and critical ill ICU patients and for peri-interventional volume replacement (S3-DGU GoR B; S3-DGAI GoR A). In trauma, balanced infusion solutions containing acetate and malate may be considered (S3-DGU GoR 0). Balanced solutions should be used in respect to metabolic and other endpoints (BE, pH, Cl−; S3-DGAI GoR B). Isotonic normal saline (0.9% NaCl) is neither recommended for trauma patients (S3-DGU GoR A; EU GRADE 2C), nor for ICU patients nor for peri-interventional volume replacement (S3-DGAI GoR A). Low-level evidence suggests the use of hypertonic solutions in blunt multiple injured and hypotensive patients (S3-DGU GoR 0) as well as in penetrating trauma injuries in the context of pre-hospital volume replacement (S3-DGU GoR 0).
Until further evidence on the use of colloids (6% HES 130/gelatine/albumin) versus crystalloids becomes available, the S3-DGAI guideline argues against HES in critically ill patients (S3-DGAI GoR A). Its use in haemorrhagic shock should be critically evaluated (S3-DGAI GoR A), and according to the S3-DGU guideline, human albumin must not be used for pre-hospital volume replacement (S3-DGU GoR A). The European trauma guideline suggests that the use of colloids be restricted due to their potentially adverse effects on coagulation (EU GRADE 2C) as well as on renal function [20]. Patient-specific aspects such as allergenic potential, pre-existing renal impairment, impact of coagulation function, and co-morbidities should be considered (S3-DGAI GoR A).
In severe life-threatening hypotension, the administration of vasopressors in addition to resuscitation fluids may be considered to maintain target arterial pressure (EU GRADE 1C).
Traumatic brain injury (TBI)
Specific aspects need consideration in the context of volume replacement in patients with traumatic brain injury (TBI). In hypotensive TBI patients, volume replacement should be administered to maintain or restore normotension (S3-DGU GoR B). When haemorrhagic shock is combined with severe TBI (GCS <9) and/or spinal injury with neurological impairment, the updated S3-DGU guideline and the European trauma guideline suggest a target MAP (≥80 mmHg) 85–90 mmHg (S3-DGU GoR B; EU GRADE 1C). Hypoosmolar/Hypotonic solutions should not be used as volume replacement in TBI patients (S3-DGAI GoR A; EU GRADE 1C), but hypertonic solutions may be considered in hypotensive patients with severe TBI (S3-DGU GoR 0). The use of albumin for resuscitation in patients with severe TBI was associated with increased intracranial pressure (ICP) during the first week in the SAFE (Saline versus Albumine Fluid Efficacy) study and was considered as the most likely mechanism of increased mortality in these patients [21].
References
Spoerke N, Michalek J, Schreiber M, et al. Crystalloid resuscitation improves survival in trauma patients receiving low ratios of fresh frozen plasma to packed red blood cells. J Trauma. 2011;71(2 suppl 3):S380–3.
Hampton D, Fabricant L, Differding J, et al. Prehospital intravenous fluid is associated with increased survival in trauma patients. J Trauma Acute Care Surg. 2013;75(1 suppl 1):S9–15.
Conte MA. Fluid resuscitation in the trauma patient. CRNA. 1997;8:31–9.
Schöchl H, Voelkel W. Die Evidenz der Volumentherapie. Wiener Klin Mag. 2010;1:12–4.
Maegele M, Lefering R, Yücel N, et al. Early coagulopathy in multiple injury: an analysis from the Germn Trauma Registry on 8724 patients. Injury. 2007;38(3):298–304.
Haut F, Kalish B, Cotton B, et al. Prehospital intravenous fluid administration is associated with higher mortality in trauma patients: a National Trauma Databank analysis. Ann Surg. 2011;253(2):371–7.
Hwabejire JO, Nembhard CE, Oyetunji TA, et al. Abdominal compartment syndrome in traumatic hemorrhagic shock: is there a fluid resuscitation inflection point associated with increased risk? Am J Surg. 2016;211(4):733–8.
Ball CG. Damage control resuscitation: history, theory and technique. Can J Surg. 2014;57:55–60.
Dutton R, Mackenzie CF, Scalea TM. Hypotensive resuscitation during active hemorrhage: impact of in-hospital mortality. J Trauma. 2002;52:1141–6.
Hussmann B, Heuer M, Lefering R, et al. Prehospital volume therapy as an independent risk factor after trauma. Biomed Res Int. 2015;2015:354–367.
Kwan I, Bunn F, Chinnock P, Roberts I. Timing and volume of fluid administration for patients with bleeding. Cochrane Database of Systematic Reviews 2014; 3(Art):CD02245.
Morrison C, Carrick M, Norman M, et al. Hypotensive resuscitation strategy reduces transfusion requirements and severe postoperative coagulopathy in trauma patients with hemorrhagic shock: Preliminary results of a randomized controlled trial. J Trauma. 2011;70(3):652–63.
Rossaint R, Bouillon B, Cerny V, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition. Crit Care. 2016;20(1):100.
S3 Guideline on Treatment of Patients with Severe and Multiple Injuries. English Version of the German Guideline S3 Leitlinie Polytrauma/Schwerverletzten-Behandlung AWMF Register-Nr. 012/019. 2016. http://www.awmf.org.leitlinien/II/012-019.html. Accessed 29 September 2016.
S3 Guideline “Intravascular Volume Treatment in the Adult” AWMF Register-Nr 001/020. 2016. http://www.awmf.org/uploads/tx-szleitlinien/001-020k_S3_Intravasculare_Volumentherapie_Erwachsenen_2014-09.pdf. Accessed 29 Sept 2016
Guyatt G, Gutterman D, Baumann MH, et al. Grading strength of recommendations and quality of evidence in clinical guidelines: report from an American College of Chest Physicians task force. Chest. 2006;129(1):174–81.
AWMF (Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V.). AWMF-Regelwerk Leitlinien: Graduierung und Empfehlung. 2014.
American College of Surgeons Committee on Trauma. ATLS Student Manual 9th Edition. Chicago, IL: American College of Surgeons, 2012.
Mutschler M, Nienaber U, Brockamp T, et al. Renaissance of base deficit for the initial assessment of trauma patients: a base deficit-based classification for hypovolemic shock developed on data from 16,305 patients derived from the TraumaRegister DGU®. Crit Care. 2013;17(2):R42.
Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, Glass P, Lipman J, Liu B, McArthur C, McGuinness S, Rajbhandari D, Taylor CB, Webb SAR, for the CHEST Investigators and the Australian and New Zealand Intensive Care Society Clinical Trials Group. Hydroxyethyl Starch or Saline for Fluid Resuscitation in Intensive Care. N Engl J Med 2012; 367: 1901–1191.
Cooper DJ, Myburgh J, Heritier S, Finfer S, Bellomo R, Billot L, Murray L, Vallance S; SAFE-TBI Investigators; Australian and New Zealand Intensive Care Society Clinical Trials Group. Albumin resuscitation for traumatic brain injury: Is intracranial hypertension the cause of increased mortality? J Neurotrauma. 2013;30(7):512–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
There are no potential conflicts of interest associated with this article. The article does not include any research involving human participants and/or animals as is summarizes current guidelines and recommendations. Informed consent was not needed.
Conflict of interest
Marc Maegele, Matthias Fröhlich, Miachael Caspers, and Sigune Kaske all declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Maegele, M., Fröhlich, M., Caspers, M. et al. Volume replacement during trauma resuscitation: a brief synopsis of current guidelines and recommendations. Eur J Trauma Emerg Surg 43, 439–443 (2017). https://doi.org/10.1007/s00068-017-0771-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-017-0771-0