Abstract
Background
Trauma registries (TR) collect information about trauma patients according to inclusion criteria, and it helps to establish protocols to improve care. However, all TR deal with incompleteness. The aim of this study is to assess the number of patients not included despite fulfilling inclusion criteria in our regional TR and identifying the predictors for being missing.
Methods
The sample was randomly selected. Two months of each year from 2010 to 2014 (5 years) were selected, and medical files of all patients attended in the emergency department room during those months were studied. Patients who were already correctly included in the TR were assigned to the ‘included’ group, and patients who should have been but were not to the ‘missing’ group. The multivariable logistic regression analysis was performed to identify predictors for being missed from the TR.
Results
Of a total of 200, 79 (40 % approximately) were identified as missing. We defined the characteristic profiles of missing patients and found that the hospital RTS and the number of injuries are independent predictors to be missing in our trauma registry, with an adjusted odds ratio of 1844 [95 % (1092–3114) and 0.574 (95 % CI 0.428–0.770)], respectively.
Conclusions
Overall, 40 % of the patients who met the inclusion criteria of the TR were not included in the registry. Our results can be generalized to other trauma records based on Utstein style, because we think probably that this fact is also happening in other databases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trauma records are regional databases aimed at knowing the magnitude of the problem of major trauma and its characteristics, assessing the quality of medical care provided by emergency systems and identifying areas for improvement to enhance the survival of the victims [1, 2]. Such registries also allow comparative assessment with other regional systems of the same or different countries to draw meaningful conclusions and compare results (benchmarking) [3–6].
To this purpose, the recorded data should be accurate, reliable, and complete. Several studies have shown that the reliability of the most important result variables of such registries (injury encoding and severity of injury and survival) is high [7–9].
Several research teams have also shown that all trauma registries have different variables with incomplete values and this may be an obstacle to meaningful analysis of the data. For example, obtaining comprehensive data on response times, physiological data, such as Respiratory Rate (RR), Glasgow Coma Scale (GCS), or excess bases, might be difficult [8, 9].
In addition, not complying with the inclusion criteria may be a significant factor to obtain biased and incorrect results [10]. Therefore, adherence to the inclusion and exclusion criteria is critical for the consistency of the records of trauma [10]. The number of patients incorrectly included (i.e., those who do not meet the criteria of severity and have been included) is relatively important, as they may be excluded when analyzing.
However, the number of patients who should have been included in the database and are not (missing) should be minimized, and their characteristics known, so that we can know if a specific pattern of systematic error occurs or it happens randomly [7, 11].
Navarre is a region in northern Spain with an area of 10,421 km2 and a population of 637,000. The emergency medical services are managed by a coordination center, which mobilizes the resources to assist the accident victim (medicalized and non-medicalized ambulances and helicopter) and deliver patients to the appropriate hospital emergency services. Navarre has a tertiary hospital working as a reference center for major trauma (Navarre Hospital Complex) and two county general hospitals (Hospital García Orcoyen of Estella and Hospital Reina Sofía of Tudela) [12].
In recent years, several publications of our group have been focused on the magnitude of the problem in our community and in different variables regarding the survival of our patients [12–14]. However, the data on the patients who are missing are not available. In addition, we do not know if their characteristics, and severity and type of injuries differ from those in patients included.
Knowing the number of patients missing and comparing this group of patients with the group of patients included is important, as the conclusions drawn from our studies are used to provide quality standards in our community and to compare our system with other systems.
This study has been aimed at evaluating the number of patients not included in our regional trauma registry and identifying the predictors to be included.
Method
Major Trauma Registry of Navarre
Since 2010, the Healthcare System of Navarra has a Registry for major trauma called “Major Trauma Registry of Navarre” (MTRN). This is a database strictly tailored to the variables and categories defined by Utstein style [14, 15]. The injuries suffered by each patient are entered using a computer application based on the Abbreviated Injury Scale (AIS) version 2008.
Database inclusion criteria were patients injured by external agents of any kind with a New Injury Severity Score (NISS) >15 [14, 15]. Exclusion criteria were: patients admitted in hospital more than 24 h after injury; patients declared dead before arrival at hospital or showing no signs of life upon arrival and no response to resuscitation; and patients injured by hanging or burnt patients with no other trauma injuries [14, 15].
A Web application that allowed users to collaborate in the provision of data for trauma cases was developed to register patients. The users were the physicians in the inpatient and outpatient Emergency Services and Intensive Care Services of the Public Healthcare System of Navarre with approximately 150 users. The overall supervision and administration of the system was conducted by a data manager that ensured compliance with the inclusion criteria and the introduction of data for each patient.
A typical scenario of collaboration is as follows: a prehospital user identifies a possible case of trauma (personal data, date, and receiving center) and prehospital information: Revised Trauma Score (RTS), score on the GCS, mechanism, and intent of the injury. Then, a hospital user diagnoses the patient and completes the patient’s records: Injury Severity Score (ISS), NISS, RTS, and previous comorbidity. Then, the data manager supervises the inclusion criteria and maintains or removes the patient from the database, checks the variables, and closes the case when the patient is discharged or dies.
Since a patient can be treated in different hospitals, the system supports the collaboration of several hospitals, enabling the possible management of transfers. Thus, a case of trauma may consist of several hospital records (one for each hospital) in which the system summarizes according to a predefined algorithm after analyzing the different hospital records.
The legislation in force on safety and confidentiality of personal data were particularly taken into account for software development, and security measures classified as high level (data backup was performed in a different place to the server residence and encryption of the media containing this information) were implemented [14]. Confidentiality was guaranteed using SSL 3.0/TLS 1.0 encryption. The system records access date and time and if access has been possible. As for authentication, each user received a signature file (provided by the system administrator) to enter the system and ensure their identity [14].
Design and sample size
The required sample size (consisting of patients included and missing patients) is calculated with the formula:
Being n = required sample size; z = 1.96 (confidence level of 95 %); p estimated percentage of missing patients; q = 100 − p and e = sampling error accepted.
The size of the sample was calculated with a hypothesis of 20 % of missing patients with a confidence interval between 0.15 and 0.25 and a 95 % of reliability.
The required sample size was 198 patients. Since each month 20 patients were included, checking 10 months chosen randomly in the three hospitals was required. The 10 months randomly checked to study patients at the emergency service and trauma registry from 2010 to 2014 were:
-
2010: January and October
-
2011: March and August
-
2012: May and November
-
2013: July and December
-
2014: February and June.
Compilation of missing patients
Data collection was performed by a doctor of our team, specialist, and well trained in trauma. These patients were collected through computerized records of the emergency services of each hospital. The medical records of all patients having some trauma in those months were studied through the Historia Clínica Informatizada (HCI) computer software.
To that purpose, we chose 1 month in the first semester and another month in the second semester for each year mentioned. Medical records of patients assisted in the emergency room for any trauma through triage grounds were reviewed. Consultation encoded by medical personnel as head, limb, thoracoabdominal, and multiple injuries has been included in the search in relation to the patient destination (Exitus, observation, hospitalization, Intensive Care Unit [ICU], surgery, and home).
Patients meeting the inclusion criteria of the trauma registry and not being included in the database were assigned to the “missing” group. The patients who were already included in the trauma registry were assigned to the “included” group.
To both groups, the following data were collected: Age, sex, type of accident (blunt or penetrating), mechanism of injury (traffic accidents, fall from low/high height, others), physiological parameters, characteristics of injuries (number of injuries and number of injured areas), injury severity (ISS and NISS), length of hospital stay, highest level of hospital care, previous comorbidity, and hospital mortality. The probability of survival was calculated with Trauma and Injury Severity Score (TRISS) method, combining ISS, RTS, and patient’s age [16].
Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 21.0. The qualitative variables were described with the frequency distribution of each category. Categorical data were expressed as proportions and percentages. Quantitative variables were described using the mean and standard deviation (SD) if following a normal distribution, and the median and interquartile range (IQR) otherwise.
The study of the association among qualitative variables was performed using the Chi-square test. The Mann–Whitney test and mean comparison for independent samples were used for continuous variables (not normally distributed and normally distributed, respectively). A value of p < 0.05 was considered statistically significant.
Multivariate statistics were performed to estimate the risk of not being included. In the logistic regression model, the following variables were used: Gender, age, level of hospital care, comorbidity, hospital RTS, NISS, and number of lesions. As a dependent variable in the database not being included (1) was used and if being included (0) was used.
Covariables considered relevant from a clinical and epidemiological point of view and which had shown statistical significance in the bivariate analysis were included. The odds ratio (OR) was presented with a 95 % confidence interval.
The ability of the variables as predictors of missing patients in the trauma registry was presented with the Receiving Operating Characteristics (ROC) curve and the Area Under Curve (AUC) with their 95 % confidence intervals.
Results
Six patients who did not meet inclusion criteria (NISS > 15) were excluded. Finally, the sample included in this quality control was 200 patients, to whom the parameters defined in the methods section were evaluated. The most relevant characteristics of the patients are shown in Table 1.
A total of 618 injuries were encoded. The most frequently injured body region was the head (283 patients), chest (191), limbs (70), abdomen (36), face and neck (20), and external (18).
Comparison between patients not included and included
Seventy-nine (79) cases of patients, who met inclusion criteria (NISS > 15) were not included in our trauma registry (39.5 %), were identified.
Significant differences were observed between patients included and not included in the following variables: age, sex, vital parameters, highest level of hospital care, previous comorbidity, probability of survival, and number of injuries and injured regions (see Table 1).
For the injured body regions, it is observed that 63 % of the missing patients have a single body injury affected compared to 45 % of the included and 32 % of those not included have two affected regions versus 31 % of those included. In addition, only 5 % of the missing patients have three or more affected regions compared to 24 % of those included (p < 0.05).
Predictors of non-inclusion in the trauma registry
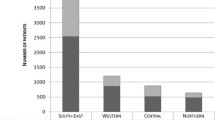
The results of the multivariate logistic regression are shown in Table 2. Having a high hospital RTS and high number of coded injuries is significant predictors for being missing with an OR of 1.84 (1.09–3.11) and 0.57 (0.43–0.77), respectively. The ability of Hosptial RTS and number of coded injuries as predictors of missing patients in the trauma registry was presented with the ROC curve and the AUC with their 95 % confidence intervals is shown in the Fig. 1.
Profile of missing vs. included patients
Table 3 show the profile of missing patients by the group of age. In this group, most patients (46) were over 65 years. Of these, (70 %) were women: (80 %) had previous comorbidity of moderate-to-severe systemic disease, (81 %) with an injury mechanism of low height fall, (48 %) arrived in hospital in conventional ambulance, anatomical indicators (ISS median [IQR], 16 [16], NISS median [IQR] 17 [16–22]), physiological indicators (Total hospital GCS median [IQR] 15 [15], Hospital RR median [IQR] 15 [15–18], Hospital SBP median [IQR] 150 [140–167], and Hospital RTS median [IQR] 7.8 [7.8–7.8]), characteristics of injuries (number of injured areas median[IQR] 1 [1, 2]), whose highest level of medical care was hospital admission, and/or observation (89 %) and (83 %) discharged home with good recovery (83 %).
On the other hand in the group of included patients, the majority (59) were under 50 years. Of these, 81 % were men: 55 % were healthy with no previous comorbidity, 56 % had an injury mechanism of traffic accident, and 70 % arrived in hospital in medicalized ambulance, anatomical indicators (ISS median [IQR], 17 [13–25], NISS median [IQR] 23 [17–32]), physiological indicators (Total hospital GCS median [IQR] 15 [10–15], Hospital RR median [IQR] 15 [15–20], Hospital SBP median [IQR] 130 [110–140], and Hospital RTS median [IQR] 7.8 [6.3–7.8]), and characteristics of injuries (number of injured areas median [IQR] 2 [1–3]), whose highest level of medical care was ICU (56 %) and (73 %) discharged home with good recovery (83 %).
In both groups, patients were transferred to another hospital after initial assessment [15/121 (12 %) vs. 9/79 (11 %; p = 0.070)]. Both the probability of survival (or expected mortality) and observed mortality, important outcome measures of the trauma registry are used for external benchmarking of risk-adjusted mortality, differ between the missing and the included patients, as shown in Table 1.
Profile of included vs. missing patients by hospitals
Table 4 shows the basic features of missing vs. included patients. By hospitals, missing group was elder than included patient groups [missing group; Navarra Hospital Complex, mean(SD) 70 (26), Hospital of Estella, mean(SD) 74 (25), Hospital of Tudela mean(SD) 62 (24) vs. included patients group; Navarra Hospital Complex, mean(SD) 53 (24), Hospital Estella, mean(SD) 68 (23.5), and Hospital of Tudela mean(SD) 61 (23.5)]. In the missing group, most of patients were female [missing group; Hospital Estella (64 %), and Hospital of Tudela (62 %)] regarding to the included group, where most of them were male [included patients group Hospital of Estella (92 %) and Hospital of Tudela (60 %)], except in Navarra Hospital Complex, where most of them were male in both the groups [missing patients (58 %) vs. included patients’ group (80 %)]. The majority of missing patients arrived in the conventional ambulance particularly in Hospital Estella (60 %) and Hospital Tudela (54 %), while in Hospital Navarra Complex, most of them (64 %) arrived in medicalized ambulance (64 %).
In all hospitals, the most common mechanism of injury among the missing patients was the fall form low height [Hospital Navarra Complex (54 %), Hospital Estella (60 %), and Hospital Tudela (69 %)], while the included patients’ group was traffic accident [Hospital Navarra Complex (60 %) and Hospital Estella (42 %)] except in Hospital Tudela, where the most common mechanism of injury was fall from low height (50 %). In the included patients group, Hospital Navarra Complex had more severely injured patients with anatomical indicators (ISS median [IQR] 16 [14–25] and NISS median [IQR] 29 [27–35]) than Hospital of Estella (ISS median [IQR] 17 [9–19] and NISS median [IQR] 26 [18–28]) and Hospital of Tudela (ISS median [IQR] 18 [15–25] and NISS median [IQR] 26[20–31]).
In the missing group also, Hospital Navarra Complex had more severely injured patients with anatomical indicators (ISS median [IQR] 16 [16–18] and NISS median [IQR] 20 [16–25]) regarding to Hospital Estella; ISS median [IQR] 16 [9–17] and NISS median [IQR] 16 [16–21], and Hospital of Tudela; ISS median [IQR] 16 [14–16] and NISS median [IQR] 16 [16–22]). Hospital of Tudela had a high percentage of missing patients with a significant previous comorbidity of moderate-to-severe systemic disease (54 %), whereas Hospital Navarra Complex and Hospital of Estella had a high number of healthy patients (51 %) and (60 %), respectively. A high percentage of healthy patients in the included group was treated in Hospital Complex Navarra (76 %), while in the same group, patients with previous comorbidity of moderate-to-severe systemic disease were treated in the Hospital of Tudela (67 %) and Hospital of Estella (58 %).
The highest level of care in all hospitals of both groups was hospitalization, as shown in Table 4; however, it should be mentioned that a high number of patients in the included patients group in Hospital Navarra Complex, Hospital of Estella and Hospital of Tudela were treated in ICU (31 %), (25 %), and (19 %), respectively.
Discussion
This study shows that nearly 40 % of all patients attending emergency room in any of the three hospitals of our regional network were not included in the trauma registry, even though they met the inclusion criteria. We have found that hospital RTS and the number of injuries are independent predictors to be missing in our trauma registry.
Several studies have addressed the problem of missing data or errors in trauma registries, such as variables with physiological data or injury encoding, and even statistical methods have been developed to treat them [10, 17, 18]. However, few studies are available analyzing compliance with inclusion criteria of a database, such as Olthof that quantifies by 15 % the number of patients missing, a percentage significantly lower than that found by our team [7].
There are several reasons that might justify this outcome together. On the one hand, the way patients are included in the records based on the collaboration of physicians taking care of patients in several health care levels and not at the hospital administration area, as stated in the method section. The hospital administration encodes the reasons through the ICD-10 codes and not through AIS injury codes (inclusion criteria as severe trauma patients according to Utstein model).
On the other hand, the missing patient’s profile has been shown in the results. These patients have comorbidity previous to the event, ranging from moderate to severe, with a single head injury (AIS = 4) that is usually cranial contusion with a small subdural hematoma. They are usually elder women, undergoing no specific treatment and admitted for observation and/or hospitalization with conservative treatment until death or until being discharged home with their baseline status.
This profile sometimes implies that the doctors treating these patients do not consider them as major multiple trauma patients, as there is no physiological effect (increased RTS, Glasgow 15 points, and normal blood pressures), and they do not require surgery or admission in ICU.
Almost 80 % of missing patients were admitted for observation and/or hospitalization, and only the remaining 20 % required surgery and/or ICU care compared to 65 % and 35 % of patients included. Most patients not included, 52 %, had previous moderate-to-severe comorbidity compared to 43 % of those included. Most of the patients not included have fewer injuries and a single-affected region (often the head), they are older, and their usual mechanism is a fall from their own height compared to the patients included. Therefore, the fragility of patients has determined that the traumatic disease is not a subsidiary of any specific treatment, and in most cases, it is left to its natural evolution. These are fragile, elderly patients who suffer accidental falls and sometimes die, because the therapeutic effort is limited.
Our profile is clearly different from Olthof study in which missing patients were related to certain hospitals in which there were figures of missing patients above 50 % and especially with the transfer of such patients from one hospital to another [7]. No statistics difference has been shown between hospitals of our study; however, the results show a higher figure than expected. Even in the Trauma Center (Hospital Navarra Complex), where the most severely ill patients are sent and where the medical care to most trauma patients is located, these figures are also high (71 %) regarding to Hospital Garcia Orcoyen of Estella (13 %) and Hospital Reina Sofia of Tudela (16 %).
Injured patients who may need neurosurgical treatment were sent from the Hospital of Estella and Hospital of Tudela to Hospital Navarra Complex; however, transfer of these patients after initial assessment between hospitals was not related to the missingness of these patients. The reason that explains the high percentage found in our Trauma Centre (Hospital Navarra Complex) was the profile of missing patients. It has shown in Table 1 that there was a high percentage of head injury in both groups, especially in the missing group (70 %), so most of them were transferred to Hospital Navarra Complex, but given their characteristics, the doctors treating these patients did not consider them severely injured patients, since there was no physiological effect and they did not need surgery or admission in ICU, and therefore, they were not included in the trauma registry. The majority of them were elder women, with previous moderate-to-severe comorbidity, fell from low height, no physiological effect, and single-affected region (often the head), whose highest level of medical care was hospital admission and/or observation and discharged home with good recovery.
The profile of trauma patients has changed significantly in our community due to the gradual intensification of surveillance, fines, and publicity given to questions of road safety [19]. These actions have reduced mortality in younger patients injured in accidents in our community, but the proportion of older patients injured in falls has risen [19]. Due to their fragility (previous comorbidity and different treatments), patients over 65 years with similar degrees of injury have twice mortality rate than young people and they are more likely to die of medical complications during admission [20].
Our findings do not mean that these patients are treated inappropriately, but merely therapeutic efforts are limited due to their fragile conditions, because it is known that aggressive interventions would not improve their quality of life.
At this point, a new question should be set out: should elder patients, with accidental low fall and with severe brain injury and obtaining limited therapeutic efforts, be included?
The aging population in developed countries makes the profile of trauma patient’s change and this may change the inclusion criteria of patients in the registries or build specific registries (geriatric trauma, hip fractures in the elderly). Efforts should be focused on creating specific registries segmenting the databases for these patients and analyze specifically excluding these patients if the purpose is to check to what extent the early medical interventions improve survival of patients.
Perhaps, this same fact is happening in other databases; therefore, it should not necessarily be considered bad management of trauma registries, but steps should be taken towards creating specific records for these fragile patients, which would also help to improve comprehensive care of these patients.
The results of this study have relevant epidemiological implications that force us to correct our previous results focused on how important the problem of falls in the elderly is becoming in our society in recent years [13].
The results obtained force us to make efforts to improve the registry. These actions should be focused on:
-
1.
Providing the “trauma patient” code from administration to all patients who arrive in the emergency services as a trauma patient by ambulance or helicopter;
-
2.
To sensitize those responsible for entering the data in the trauma registry keeping them informed of the percentage of current missing patients and the profile of these patients;
-
3.
To perform regular quality controls and include statistics reports within the hospital system to show the usefulness of trauma registry to medical staff and health providers and thus motivate data collection;
-
4.
Insist on the importance of the trauma registry and fill out the forms prepared with the basic data (Annex 1) for the capture of trauma cases admitted for observation and hospitalization;
-
5.
Further collaboration with the hospital administrative area when encoding the grounds of admission, including the possibility of database crossing for detecting possible missing patients;
-
6.
Report on the existence of a trauma registry to the hospital medical personnel and facilitate access (email of trauma registry users) to capture unreported cases;
-
7.
Compulsorily encode trauma injuries in the basic form (Annex 1) of all “trauma patient” through AIS codes while preparing the discharge report. Therefore, the program will automatically calculate the ISS and NISS;
-
8.
Create an application in the HCI to send the basic form (Annex 1) to the data manager with the patient’s clinical history whenever a patient has an NISS > 15, so that the case may be analyzed and entered in the database.
The great value of trauma registries is to design intervention strategies to reduce morbidity and mortality related to trauma which basically depends on the quality of the collected data, so it should be attempted to reach a database with the highest quality within the limits imposed by available resources. Thus, quality controls are necessary to ensure that the data introduced in the trauma registries are precise, reliable, complete, and concordant with the medical record of patients.
Lefering et al. [21]. mentioned three aspects to take in account to assess trauma registries. One of them refers to the completeness regarding the number of cases (i.e., are all, or at least most, of the appropriate cases actually included in the registry?) that was analyzed here. All trauma registries should evaluated, if any, the incidence and patterns of missing patients, as it influences the quality of the collected data and thus the quality of the results.
Limitations
This study has a number of limitations, such as being a relatively small sample of patients when compared with large international databases. Another limitation is the low number of published studies to evaluate the completeness of a trauma registry, and therefore, there is no standard method for quality control [7, 8, 10]. The effects of intubation, sedation, and alcohol intoxication on the RTS parameters could not be controlled for.
In the logistic regression, we can only work with a limited number of variables [7]. The two variables identified in this study should not be considered as the only significant predictors of missing records. Since it is the first study on a regional basis of trauma based on Utstein style, similar studies will be necessary to find other variables that can influence this issue and, therefore, establish specifically which variables are most sensitive for this kind of study [14, 15].
Conclusions
In total, 40 % of patients assisted by our healthcare system meeting inclusion criteria were not included in the trauma registry. Although this percentage is higher than expected, we detected the non-inclusion predictors, and likewise, we have described the profile of patients not included in the database. These problems show an undeniable need to provide protocols for internal quality controls, since trauma registries are important sources of information for the assessment of medical care, injury prevention, clinical and epidemiological research, and provision of protocols and they can be used to quality control and health planning.
References
Pfeifer R, Tarkin IS, Rocos B, Pape HC. Patterns of mortality and causes of death in polytrauma patients–has anything changed? Injury. 2009;40(9):907–11.
Lefering R, Huber-Wagner S, Nienaber U, Maegele M, Bouillon B. Update of the trauma risk adjustment model of the TraumaRegister DGUTM: the Revised Injury Severity Classification, version II. Crit Care. 2014;18(5):476.
Morrissey BE, Delaney RA, Johnstone AJ, Petrovick L, Smith RM. Do trauma systems work? A comparison of major trauma outcomes between Aberdeen Royal Infirmary and Massachusetts General Hospital. Injury. 2015;46(1):150–5.
Heim C, Bosisio F, Roth A, et al. Is trauma in Switzerland any different? epidemiology and patterns of injury in major trauma—a 5-year review from a swiss trauma centre. Swiss Med Wkly. 2014;144:w13958.
Watts HF, Kerem Y, Kulstad EB. Evaluation of the revised trauma and injury severity scores in elderly trauma patients. J Emerg Trauma Shock. 2012;5(2):131–4.
O’Mullane PA, Mikocka-Walus AA, Gabbe BJ, Cameron PA. Incidence and outcomes of major trauma assaults: a population-based study in Victoria. Public Health. 2009;190(3):129–32.
Olthof DC, Peters RW, Klooster M, Goslings JC. Missing patients in a regional trauma registry: incidence and predictors. Injury. 2014;45(9):1488–92.
Prat S, Dominguez-Sampedro P, Koo M, Colilles C, Jimenez-Fabrega X, Espinosa L. TraumCat: preliminary analysis of a year of severe trauma registry in Catalonia. Emergency. 2014;26(4):267–74.
O’Reilly GM, Gabbe B, Cameron PA. Trauma registry methodology: a survey of trauma registry custodians to determine current approaches. Injury. 2015;46(2):201–6.
Hlaing T, Hollister L, Aaland M. Trauma registry data validation: essential for quality trauma care. J Trauma Acute Care Surg. 2006;61(6):1400–7.
O’Reilly GM, Jolley DJ, Cameron PA, Gabbe B. Missing in action: a case study of the application of methods for dealing with missing data to trauma system benchmarking. Acad Emerg Med. 2010;17(10):1122–9.
Fortún M, Ali B, Montes LM, Rey JM, Teijeira R, Belzunegui T. Inclusion of prehospital mortality statistics in severe trauma registries: a study of its influence on trauma lethality rates and survival prediction. Emergencias. 2016;28:173–8.
Belzunegui T, Gradín C, Fortún M, Cabodevilla A, Barbachano A, Sanz JA. Major trauma registry of Navarre (Spain): the accuracy of different survival prediction models. Am J Emerg Med. 2013;31(9):1382–8.
Belzunegui T, FortúnM, Reyero D, Teijeira R. Implementation of the first Spanish population-based register for multiple-injury cases in Navarre. Emergency. 2013;25:196–200.
Ringdal KG, Coats TJ, Lefering R, Di Bartolomeo S, Steen PA, Roise O, et al. The Utstein template for uniform reporting of data following major trauma: a joint revision by SCANTEM, TARN, DGU-TR and RITG. Scand J Trauma Resusc Emerg Med. 2008;16(1):7.
Champion HR, Copes WS, Sacco WJ, et al. The Major Trauma Outcome Study: establishing national norms for trauma care. J Trauma. 1990;30(11):1356–65.
Haider AH, Saleem T, Leow JJ, et al. Influence of the National Trauma Data Bank on the study of trauma outcomes: is it time to set research best practices to further enhance its impact? J Am Coll Surg. 2012;214(5):756–68.
Moore L, Hanley J, Lavoie A, Turgeon A. Evaluating the validity of multiple imputation for missing physiological data in the national trauma data bank. J Emerg Trauma Shock. 2009;2:73–9.
López-Ruiz M, Martínez JM, Pérez K, Novoa AM, Tobías A, Benavides FG. Impact of road safety interventions on traffic-related occupational injuries in Spain, 2004–2010. Accident Anal Prev. 2014;66:114–9.
Dinh MM, Roncal S, Byrne CM, Petchell J. Growing trend in older patients with severe injuries: mortality and mechanisms of injury between 1991 and 2010 at an inner city major trauma centre. ANZ J Surg. 2013;83:65–9.
Lefering R, Ruchholtz S. Trauma registries in Europe. Europ J Trauma Emerg Med. 2012;38:1–2.
Acknowledgments
The authors would like to thank the emergency department doctors and data managers from centres that participated in the research. We would also like to thank Silvia Ayerra and Imanol Pinto for their extremely valuable contribution to the implementation of the IT application.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Bismil Ali Ali, Mariano Fortun Moral, Tomas Belzunegui Otano, Berta Ibañez Beroiz, Koldo Iñaki Cambra Contin, and Arkaitz Jimenez Galbete declare that they have no conflict of interest.
Permission note (ethics)
The study has been approved by the Ethics Committee of the Department of Health of the government of Navarre. The subjects gave their informed consent to the work. The investigation carried out was approved and evaluated by the National Agency for Quality and Accreditation of Spain, ANECA.
Annex 1. Basic form
Annex 1. Basic form

Rights and permissions
About this article
Cite this article
Ali, B.A., Fortún, M., Belzunegui, T. et al. Missing patients in “Major Trauma Registry” of Navarre: incidence and pattern. Eur J Trauma Emerg Surg 43, 671–683 (2017). https://doi.org/10.1007/s00068-016-0717-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-016-0717-y