Abstract
Purpose
The most commonly used mobility assessments for screening risk of falls among older adults are rating scales such as the Tinetti performance oriented mobility assessment (POMA). However, its correlation with falls is not always predictable and disadvantages of the scale include difficulty to assess many of the items on a 3-point scale and poor specificity. The purpose of this study was to describe the ability of the new Aachen Mobility and Balance Index (AMBI) to discriminate between subjects with a fall history and subjects without such events in comparison to the Tinetti POMA Scale.
Methods
For this prospective cohort study, 24 participants in the study group and 10 in the control group were selected from a population of patients in our hospital who had met the stringent inclusion criteria. Both groups completed the Tinetti POMA Scale (gait and balance component) and the AMBI (tandem stance, tandem walk, ten-meter-walk-test, sit-to-stand with five repetitions, 360° turns, timed-up-and-go-test and measurement of the dominant hand grip strength). A history of falls and hospitalization in the past year were evaluated retrospectively. The relationships among the mobility tests were examined with Bland–Altmananalysis. Receiver-operated characteristics curves, sensitivity and specificity were calculated.
Results
The study showed a strong negative correlation between the AMBI (17 points max., highest fall risk) and Tinetti POMA Scale (28 points max., lowest fall risk; r = −0.78, p < 0.001) with an excellent discrimination between community-dwelling older people and a younger control group. However, there were no differences in any of the mobility and balance measurements between participants with and without a fall history with equal characteristics in test comparison (AMBI vs. Tinetti POMA Scale: AUC 0.570 vs. 0.598; p = 0.762). The Tinetti POMA Scale (cut-off <20 points) showed a sensitivity of 0.45 and a specificity of 0.69, the AMBI a sensitivity of 0.64 and a specificity of 0.46 (cut-off >5 points).
Conclusion
The AMBI comprises mobility and balance tasks with increasing difficulty as well as a measurement of the dominant hand-grip strength. Its ability to identify fallers was comparable to the Tinetti POMA Scale. However, both measurement sets showed shortcomings in discrimination between fallers and non-fallers based on a self-reported retrospective falls-status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple studies have described the demographic changes in western societies. An increasing number of traumatic events are associated with these changes [1–6]. The incidence of falls in the elderly population is difficult to determine and therefore potentially underestimated. Even in the cognitively fit patients, reconstructing the chain of events is demanding [7]. Previous falls, strength, gait and balance impairments, and use of specific medications range amongst the strongest predictors [8]. By identifying individuals with a high risk of falling, targeted fall prevention interventions could be directed at those most likely to benefit from them. The American Geriatric Society/British Geriatric Society guideline therefore suggests that all older individuals should be assessed regarding the incidence and number of falls in the last year. Furthermore, the evaluation should include a detailed physical examination and a timed performance test [9, 10]. Numerous simple and composite physical performance tests have been used for screening risk of falls among older adults [11–15]. However, most tests have not been validated prospectively in large representative samples of community-dwelling older people, making their predictive accuracy uncertain [15].
The most commonly used mobility assessments are rating scales such as the Tinetti performance oriented mobility assessment (POMA) [8, 13]. Rating scales utilize subjective categorical determinations to create ordinal measurements, may be time-consuming, and are subjected to inter-rater reliability concerns. Different versions of the test were used by different studies and its correlation with falls in the future is not always predictable [16, 17]. Disadvantages of the scale include difficulty to assess many of the items on a 3-point scale and its poor specificity. Furthermore, despite being widely used in gerontology, the gait section is seldom used [18]. Objective performance indices (e.g. timed-up-and-go-test (TUG)) are also commonly used. The TUG uses agreement in stop-watch durations instead of rating scales, probably making it the most reliable test [18–20]. These continuous measures offer interval or ratio measurements and, therefore, finer performance distinctions [20]. However, specific tasks or single tests may offer limited challenge to high-functioning individuals or include elements that are too difficult for impaired older adults [17]. To address these issues, we developed a mobility and balance index that includes tasks representing progressively more difficult mobility and balance components. The tasks progress with increasing complexity and are designed to challenge performance abilities across the spectrum of older adults. Using progressively complex tasks including standing balance, walking balance, gait speed, sit-to-stand, 360 degree turns and the more complex TUG offers the potential to avoid ceiling and floor effects and specific correlates of falling can be identified to define those people at risk. In addition, impaired muscle strength is associated with falls, especially in older adults [21]. Low dominant hand-grip strength (DHGS) is a strong predictor for both long-term and short-term disability and mortality. DHGS has been reported to have a good-to-excellent reliability in older adults and correlates with the static balance in geriatric patients, which was an independent predictor of physiological fall risk [17]. Given these considerations, the DHGS is a reasonable parameter in fall risk stratification and was included in the mobility and balance index.
A recent history of falls has been used as an indicator of functional decline [20, 22]. The purpose of this study was to describe the ability of the Aachen Mobility and Balance Index (AMBI) to discriminate between (1) community-dwelling elders and healthy controls and (2) subjects with balance disorders (history of falls in the past year) and subjects without such disorders. In addition, POMA scores were compared with AMBI scores. Sensitivity rather than specificity was emphasized, as the focus was on recognizing individuals requiring intervention rather than screening those who did not.
Methods
Study group
This study was approved by the Institutional Review Board at the RWTH Aachen University. Participants were contacted by letter using a mailing list provided by several Departments of Internal Medicine and Surgery, following a pre-screening interview via telephone. On their first visit 24 community-dwelling elders (CDE) provided informed consent, mental status, medical and falls histories and underwent physical examination by a physician. Exclusion criteria were: cognitive impairment (mini mental status exam, score <24 [23]), legal blindness, obesity (BMI >30), and insufficient command of German language. To eliminate the influence of known pathology, volunteers with a diagnosis of neurological, orthopedic or visual disorders (e.g. Parkinson’s disease, knee replacement or macular degeneration) directly impairing mobility were excluded. Utilizing falls-risk screening criteria, participants reporting ≥2 non-injury falls in the past year or ≥1 injury fall were categorized as ‘fallers’; remaining subjects were considered ‘non-fallers’ [20]. The Charlson comorbidity index (CCI), score of frailty (Fried) and the DemTect score were calculated.
Control group
A healthy control group was included to determine and validate the time limits of the specific mobility tests available in the literature. Recruitment was achieved via flyers posted on bulletin boards, as well as by e-mail. Informed consent was obtained from each participant and participation was voluntary (ethical approval EK 171/14). Subjects had to meet the following stringent criteria to be eligible to participate: (1) no history of musculoskeletal disease in general; and (2) no history of lower-extremity or spine pathology that would influence the ability to stand and turn. All subjects were screened by a board-certified orthopedic surgeon. Vision and hearing was also tested to ensure that it was within normal age limits.
Functional mobility tests
Aachen Mobility and Balance Index (AMBI) (higher scores represent a higher level of fall risk)
Standing balance (tandem stance)
The tandem stance is reported to have poor discriminatory ability and sensitivity but good specificity [24, 25]. This clinical test of standing balance was carried out with eyes open and standing on a line without additional help. Time was measured until correctional movement was done. A standing time shorter than 10 s was considered a balance disorder (2 points) [26].
Walking balance (tandem walk)
Two studies have shown that poor tandem walk ability was a predictor of falls [11, 27]. After adjustment for bone density, poor tandem walk ability as well as slow gait speed and poor vision, were independent predictors of hip fracture [28]. Given a distance of 8 m, a side deviation of more than a half foot breadth was considered a balance disorder (2 points) [11, 27].
Gait speed (ten-meter-walk-test)
Slow gait speed is associated with an increased risk of falls [29, 30] and is a measure included in fall risk assessment scales [31, 32]. Subjects completed a ten-meter-walk-test measured in seconds along a corridor at their normal walking speed. A time between 8 and 10 s was considered a slightly impaired gait speed (1 point) and greater than 10 s an insufficient gait speed (2 points).
Sit-to-stand (STS-5)
Csuka and McCarty first described the use of the sit-to-stand-test as a measure of lower-extremity strength [33]. The ability to stand from a chair is a crucial factor in independence in older adults living in the community and is related to falls [11, 34]. For the sit-to-stand-test with five repetitions (STS-5), subjects were asked to rise from a standard height (43 cm) chair without armrests, five times, as fast as possible with their arms folded. Subjects undertook the test barefoot and performance was measured in seconds, as the time from the initial seated position to the final seated position after completing five stands. A performance between 12 and 15 s was considered a slightly impaired lower limb strength (1 point) and a time span greater than 15 s a severely impaired strength (2 points) [15, 35].
360-degree turns
The ability to turn around in an efficient manner has been included in assessments of mobility and balance in older people [31, 36]. Investigating the segmental coordination, subjects were asked to take a few steps turning around. The number of steps taken to complete this 360-degree turn was counted. A number of steps between 5 and 8 were considered a slightly impaired turn (1 point), greater than eight steps a severely impaired turn (2 points) and all characteristics of tumbling were considered a missing ability to turn (3 points).
Timed-up-and-go-test (TUG)
The timed-up-and-go-test (TUG) is useful in an outpatient setting, because it takes only a few minutes, is easy to administer, and requires little equipment. Importantly, the TUG test is highly correlated with functional mobility, gait speed, and falls in older adults [37]. Patients were instructed to stand up from a chair and walk forward at their normative speed for 3 m, then turn around and walk back to the chair and sit down. The whole procedure was timed in seconds from the command to go until the participant made contact sitting in the chair. If the patient could not perform the task without using their hands to push off, they were allowed to do it a second time while using their hands to push off the chair. Use of assistant devices was not allowed. In a recent study, the best predictive value for discriminating elderly individuals who fell was 12.5 s [19]. Based on these results, we considered a time span of 10–19 s a slightly impaired mobility (1 point), 20–29 s a moderately impaired mobility with probable impairments in daily living (2 points) and greater than 29 s a severely impaired mobility with strong affection of activities in daily life (4 points).
Dominant hand-grip strength (DHGS)
Measurement of dominant hand-grip strength (DHGS) is a simple, inexpensive risk-stratifying method for all-cause death and cardiovascular disease [38]. Grip strength was measured with a hydraulic hand dynamometer (SH5001, SAEHAN Corporation, Gyeongsangnam-do, South Korea) with the elbow at 90° and the forearm neutral. Participants were instructed to squeeze the handle of the dynamometer and maintain for 5 s. Three trials were performed with adequate rest in between and the best reading was taken as the DHGS in kilograms (kg). Age-adjusted tables were used to determine if the DHGS was normal or impaired (2 points) [39].
Tinetti POMA Scale
(Higher scores represent a lower level of fall risk.)
We also used the Tinetti POMA Scale to assess the gait with seven components (initiation of gait, step length, step symmetry, step continuity, path, trunk and walking stance; maximum 12 points) and balance abilities of participants with nine components (sitting balance, arises, attempts to arise, immediate standing balance, standing balance, nudged, eyes closed, turning 360°, and sitting down; maximum 16 points) [8, 13]. Each subscale was measured as abnormal = 0 or normal = 1; in some cases, adaptive = 1 and normal = 2. The maximum sum-score of both gait and balance components are 28 points. If a clinician desires to optimize both sensitivity and specificity to identify only those who are at high risk of falling, a cut-off score of 20 is supported [40].
Statistical analysis
Analysis was performed using SPSS™ 21.0 (SPSS Inc., Chicago, IL, USA). Continuous data were summarized by means, range and corresponding SD, and categorical data by frequencies and percentages. Differences in sociodemographic and clinical variables between the groups were tested with the Chi-square test. The linear relationships among the mobility tests (all mobility and balance measurements including Tinetti POMA Scale, AMBI and its components) were examined with Pearson correlations. Unpaired t tests were used to assess differences in mobility task performance for study group versus control group, fallers and non-fallers based on the retrospective falls data. Receiver-operated characteristics (ROC) curves and AUC´s were calculated and pairwise comparison of ROC curves was performed with Bland–Altmananalysis. Sensitivity and specificity were then calculated for the cut-off points (MedCalc® version 16.2.1, Ostend, Belgium).
Results
Study population
The 24 participants of the study group (SG) and ten of the control group (CG) were selected from a population of patients in our hospital who had met the stringent inclusion criteria. The study group (17 women, 7 men) was different from the control group [(5 women, 5 men, age 26, 7 (21–32) years, BMI 23, 4 (20–27) kg/m2)] in terms of age [(79, 5 (66–93) years; p < 0.001) and BMI (25, 9 (17–33)] kg/m2; p = 0.030) (Table 1 shows the distribution of the study collective). The control group outperformed the study group in the standardized mobility and balance tests. The mean AMBI (0.7 vs. 6.3 points) as well as the Tinetti POMA Scale (gait and balance scale included; 28.0 vs. 22.2 points) showed superior results for the control group (p < 0.001). However, in terms of gait speed and 360-degree turn not all young participants could reach the optimum value (Table 1). Focusing on potential gender effects, no differences emerged between female and male participants of the SG or the CG assessing the AMBI and Tinetti scores. However, mobility competencies in terms of the sit-to-stand-test (STS-5) were better in females than in males in the SG (9.3 vs. 12.4 s; p = 0.012) despite an impaired hand-grip strength in females (17.9 vs. 23.1 kg; p = 0.030).
Test correlations
We found a significant negative correlation between the AMBI [(6.3 ± 2.9 points (17 points max., highest fall risk))] and the Tinetti Score [(22.4 ± 4.4 points (28 points max., lowest fall risk)]; r = −0.78, p < 0.001; Table 2; Fig. 1). A high frailty score (Fried) was associated with a low dominant hand grip strength (r = −0.64; p = 0.001) and a reduced Tinetti Score (r = −0.51; p = 0.010). The existence of comorbidities (Charlson comorbidity index, CCI) was associated with a low DemTect score (r = −0.51; p = 0.011) and a high number of steps in the 360-degree turn. Furthermore, an impaired dominant hand-grip strength showed an inverse correlation with the number of hospitalizations due to fall injuries.
Entry falls-status criterion in the study group
16 participants reported at least one single fall, 6 participants reported multiple falls (≥2 falls) and 9 participants reported fall-related hospitalization in the past year.
Participants reporting ≥2 non-injury falls in the past year or ≥1 injury fall (hospitalization) were categorized as ‘fallers’; remaining subjects were considered ‘non-fallers’ [20] leading to 13 ‘non-fallers’ [(age: range 69–93, 80.2 ± 6.5 (mean ± SD))] and 11 ‘fallers’ (age: range 66–93, 78.7 ± 6.2). Focusing on mobility and balance measurements, no differences emerged between fallers and non-fallers (AMBI, Tinetti POMA Scale, gait speed, ten-meter-walk-test, STS-5, 360-degree turn, TUG and DHGS; Table 3).
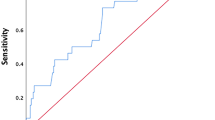
The sensitivity and specificity with which the two measurement sets, AMBI and Tinetti POMA Scale, identified entry falls-status group were calculated (Table 4). Using a cut-off criterion <20 points, the Tinetti POMA Scale showed a sensitivity of 0.45 and a specificity of 0.69 (AUC 0.598; 95 % CI 0.380–0.791). The AMBI showed a sensitivity of 0.64 and a specificity of 0.46 (AUC 0.570; 95 % CI 0.354–0.768) considering the best sensitivity/specificity ratio using a cut-off criterion of >5 points. Pairwise comparison of ROC curves showed no significant differences between AMBI and Tinetti POMA Scale (p = 0.762; Fig. 2).
Figure 3 depicts the receiver operating characteristics (ROC curves) of the AMBI and Tinetti POMA Scale modifying the falls-status criterion (Fig. 3). The Tinetti POMA Scale produced the highest sensitivity values, identifying multiple fallers without taking “injury fall” into consideration. Focusing on multiple fallers and removing “hospitalization” lead to a markedly increased sensitivity (0.67 compared to 0.45) and slightly increased specificity (0.72 compared to 0.69) with a AUC of 0.699 (95 % CI 0.480–0.867).
Discussion
The correlation of the Tinetti test with falls in the future is not always predictable and disadvantages of the scale include difficulty to assess many of the items on a 3-point scale [16, 17]. Continuous measures offer interval or ratio measurements and therefore finer performance distinctions [20]. We developed a mobility and balance index (AMBI) that comprises tasks of continuous measurements representing progressively more difficult mobility and balance components as well as the dominant hand-grip strength. The study showed a strong negative correlation between the AMBI and Tinetti POMA Scale with an excellent discrimination between community-dwelling older people and a younger control group. However, no differences emerged in any mobility and balance measurement between participants with and without a fall history. The Tinetti Scale showed a moderate specificity but a poor sensitivity, the AMBI a better sensitivity than specificity. Albeit, removing the criterion “hospitalization”, multiple fallers could be detected using the Tinetti POMA Scale with a significant increased sensitivity and an acceptable specificity. A low dominant hand-grip strength was associated with frailty and a high hospitalization rate in the past.
Time constraints, competing demands, and inadequate reimbursement pose a challenge to incorporating fall prevention into practice [13, 41]. History of falls as well as gait or balance disabilities are strong and reliable predictors of future falls. In conclusion, further assessment is required if patients affirm more than one non-injurious fall or report difficulties with walking or balance [8, 10]. Assessment tools for gait and balance are straightforward, self-contained, fast to apply and can apparently be used to predict the risk of falling [36]. However, there is a lack of evidence that any of the available screening tests is clearly useful for identifying fallers [9]. Evaluation of these tests has mostly been performed in single studies or in multiple but diverse and incomparable studies in terms of sample size or study design [9]. The most frequently evaluated tool is the Tinetti POMA Scale. However, different versions of the test were used by different studies [16]. Despite being widely used in gerontology, the gait section is seldom used and disadvantages of the scale represent a poor specificity [18]. However, in our study the Tinetti Scale showed a moderate specificity of 69 % but a poor sensitivity of 45 %. Furthermore, if a clinician desires to optimize both sensitivity and specificity to identify only those who are at high risk of falling, a cut-off score of 20 is supported [40]. In a previous study, the Tinetti POMA Scale demonstrated also high specificity in terms of falls-status, supporting its value for screening those who may not require intervention. However, this widely used test provided disappointing sensitivity toward entry falls-status and subsequent injury falls, making it insufficient for situations requiring both sensitivity and specificity [20]. Using the Tinetti Scale in our study the discrimination between fallers and non-fallers was poor. A different study found the Tinetti POMA to be sensitive (70/52 specificity) to one or more falls among 225 community-dwelling older people [20, 42]. It was recommended to include more challenging items or those addressing medical factors associated with falls [20]. However, it is unlikely that any single mobility test will be shown to have excellent predictive accuracy, as it is known that the causes of falls are multifactorial with several factors unrelated to mobility. For example, poor vision, cardiovascular conditions and cognitive impairment can lead to falls independent of mobility limitations [15]. Based on assessments of feasibility, reliability and predictive validity for falls, the sit-to-stand-test with five repetitions (STS-5) and the six-meter-walk-test were recommended [15]. Besides, the timed-up-and-go-test (TUG) is the most frequently recommended screening test for mobility using agreement in stop-watch durations instead of rating scales [18, 19, 37]. The tandem stance is reported to have a good specificity for predicting falls [24, 25]. DHGS has been reported to have a good-to-excellent reliability in older adults and to correlate with the static balance in geriatric patients which was an independent predictor of physiological fall risk [17]. Kegelmeyer et al. recommended that clinicians perform a multifactorial fall risk assessment once they have screened individuals with the Tinetti Scale [40]. Furthermore, there was an enhanced predictive ability to discern subjects with balance dysfunction from subjects without balance dysfunction on the basis of a combination of the results from the STS-5, measurement of balance, and gait measurements [35]. In this light, we think the introduction of the combination of quick balance and mobility tools with continuous measurements including the hand-grip strength meets the criteria to identify whether or not a balance problem exists.
However, such as the Tinetti test, none of these tests alone or in combination (AMBI) was associated with the retrospective falls-status in the last year. Maybe the hand-grip strength could predict hospitalization, but this association should be interpreted with caution because of the retrospective nature of the trial and the reliance on self-reported data. However, a reliable and accurate falls-status as the underlying criterion has to be highlighted. Focusing on multiple fallers without considering hospitalization times [20] induced a significantly increased sensitivity of the Tinetti POMA Scale. Assessing the status of falls seems to be the key factor for comparing test batteries and their fall prediction abilities. In retrospective studies, verification of fall history is also in the responsibility of the elderly patient. The introduction of self-assessment tools, such as the ‘Aachen falls prevention scale’, could help to focus on balance problems making retrospective data more reliable [43].
Limitations
This report has several drawbacks. Firstly, it is acknowledged that as the participants comprised relatively healthy older people, the findings are unlikely to generalize to very frail older people. Secondly, the number of participants was limited diminishing the conclusions. Thirdly, further, predictive accuracy is limited by the retrospective and the inherently problematic nature of the outcome variable (i.e. falls), which relies on self-report. Further studies including a larger study group will have to assess the ability of the AMBI to estimate the individual falls risk on a longitudinal basis and possibly trigger the necessity for further assessment by a skilled physician.
Conclusion
The Aachen Mobility and Balance Index (AMBI) comprises mobility and balance tasks with increasing difficulty as well as a measurement of the dominant hand-grip strength.
The study showed a strong negative correlation between the AMBI and Tinetti POMA Scale with an excellent discrimination between community-dwelling older people and a younger control group. However, no differences emerged in any mobility and balance measurement between participants with and without a fall history. The Tinetti Scale showed a moderate specificity but a poor sensitivity (cut-off <20), the AMBI a better sensitivity than specificity (cut-off >5). Pairwise comparison of both AMBI and Tinetti POMA Scale showed no statistical differences.
References
Moore L, Turgeon AF, Sirois MJ, Lavoie A. Trauma centre outcome performance: a comparison of young adults and geriatric patients in an inclusive trauma system. Injury. 2012;43(9):1580–5.
Vlaeyen E, Deschodt M, Debard G, Dejaeger E, Boonen S, Goedemé T, Vanrumste B, Milisen K. Fall incidents unraveled: a series of 26 video-based real-life fall events in three frail older persons. BMC Geriatr. 2013;13:103.
Liem IS, Kammerlander C, Suhm N, Blauth M, Roth T, Gosch M, Hoang-Kim A, Mendelson D, Zuckerman J, Leung F, Burton J, Moran C, Parker M, Giusti A, Pioli G, Goldhahn J, Kates SL. Investigation performed with the assistance of the AOTrauma network: identifying a standard set of outcome parameters for the evaluation of orthogeriatric co-management for hip fractures. Injury. 2013;44(11):1403–12.
Kammerlander C, Gosch M, Blauth M, Lechleitner M, Luger TJ, Roth T. The tyrolean geriatric fracture center: an orthogeriatric co-management model. Z Gerontol Geriatr. 2011;44(6):363–7.
Bielza Galindo R, Ortiz Espada A, Arias Muñana E, Velasco Guzmán de Lázaro R, Mora Casado A, Moreno Martín R, Tapia Salinas B, Escalera Alonso J, Gómez Cerezo J. Opening of an acute orthogeriatric unit in a general hospital. Rev Esp Geriatr Gerontol. 2013;48(1):26–9.
Patel NK, Sarraf KM, Joseph S, Lee C, Middleton FR. Implementing the national hip fracture database: an audit of care. Injury. 2013;44(12):1934–9.
Ungar A, Rafanelli M, Iacomelli I, Brunetti MA, Ceccofiglio A, Tesi F, Marchionni N. Fall prevention in the elderly. Clin Cases Miner Bone Metab. 2013;10(2):91–5.
Tinetti ME, Kumar C. The patient who falls: it’s always a trade-off. JAMA. 2010;303(3):258–66.
Gates S, Smith LA, Fisher JD, Lamb SE. Systematic review of accuracy of screening instruments for predicting fall risk among independently living older adults. J Rehabil Res Dev. 2008;45(8):1105–16.
American Geriatrics Society. British geriatrics society, American cademy of orthopaedic surgeons panel on falls prevention. Guideline for the prevention of falls in older persons. J Am Geriatr Soc. 2001;49(5):664–72.
Nevitt M, Cummings S, Kidd S, Black D. Risk factors for recurrent non-syncopal falls. JAMA. 1989;261:2663–8.
Berg KO, Maki BE, Williams JI, Holliday PJ, Wood-Dauphinee SL. Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil. 1992;73:1073–80.
Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34:119–26.
Chiu AY, Au-Yeung SS, Lo SK. A comparison of four functional tests in discriminating fallers from non-fallers in older people. Disabil Rehabil. 2003;25:45–50.
Tiedemann A, Shimada H, Sherrington C, Murray S, Lord S. The comparative ability of eight functional mobility tests for predicting falls in community-dwelling older people. Age Ageing. 2008;37(4):430–5.
Kopke S, Meyer G. The Tinetti test: babylon in geriatric assessment. Z Gerontol Geriatr. 2006;39(4):288–91.
Singh DK, Pillai SG, Tan ST, Tai CC, Shahar S. Association between physiological falls risk and physical performance tests among community-dwelling older adults. Clin Interv Aging. 2015;13(10):1319–26.
Yelnik A, Bonan I. Clinical tools for assessing balance disorders. Neurophysiol Clin. 2008;38:439–45.
Alexandre TS, Meira DM, Rico NC, Mizuta SK. Accuracy of timed up and go test for screening risk of falls among community-dwelling elderly. Rev Bras Fisioter. 2012;16(5):381–8.
Panzer VP, Wakefield DB, Hall CB, Wolfson LI. Mobility assessment: sensitivity and specificity of measurement sets in older adults. Arch Phys Med Rehabil. 2011;92(6):905–12.
American Geriatrics Society. Guidelines for the prevention of falls in older persons. J Am Geriatr Soc. 2001;49(5):664–72.
Ferrucci L, Guralnik JM, Studenski S, Fried LP, Cutler GB Jr. Interventions on frailty working group. designing randomized, controlled trials aimed at preventing or delaying functional decline and disability in frail, older persons. J Am Geriatr Soc. 2004;52:625–34.
Folstein MF, Folstein SE, McHugh PR. Mini-mental state a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Stel VS, Pluijm SM, Deeg DJ, Smit JH, Bouter M, Lips P. A classification tree for predicting recurrent falling in community-dwelling older persons. J Am Geriatr Soc. 2003;51(10):1356–64.
Murphy MA, Olson SL, Protas EJ, Overby AR. Screening for falls in community-dwelling elderly. J Aging Phys Act. 2003;11:66–80.
Gardner MM, Buchner DM, Robertson MC, Campbell AJ. Practical implementation of an exercise-based falls prevention programme. Age Ageing. 2001;30(1):77–83.
Chu LW, Pei CK, Chiu A, Liu K, Chu MM, Wong S, Wong A. Risk factors for falls in hospitalized older medical patients. J Gerontol Biol Sci. 1999;54:M38–43.
Dargent-Molina P, Favier F, Grandjean H, Baudoin C, Schott AM, Hausherr E, Meunier PJ, Bréart G. Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet. 1996;348:145–9.
Imms FJ, Edholm OG. Studies of gait and mobility in the elderly. Age Ageing. 1981;10:147–56.
der Weil Bootsma-van. A, Gussekloo J, de Craen AJM, Van Exel E, Bloem BR, Westendorp RG. Common chronic diseases and general impairments as determinants of walking disability in the oldest-old population. J Am Geriatr Soc. 2002;50:1405–10.
Podsialdo D, Richardson S. The timed up and go: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–8.
Piotrowski A, Cole J. Clinical measures of balance and functional assessment in elderly persons. Aust J Physiother. 1994;40:183–8.
Csuka M, McCarty DJ. Simple method for measurement of lower extremity muscle strength. Am J Med. 1985;78:77–81.
Campbell AJ, Borrie MJ, Spears GF. Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol. 1989;44:M112–7.
Whitney SL, Wrisley DM, Marchetti GF, Gee MA, Redfern MS, Furman JM. Clinical measurement of sit-to-stand performance in people with balance disorders: validity of data for the five-times-sit-to-stand test. Phys Ther. 2005;85(10):1034–45.
Berg K, Wood-Dauphinee S, Williams JI, Maki B. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41:304–11.
Viccaro LJ, Perera S, Studenski SA. Is timed up and go better than gait speed in predicting health, function, and falls in older adults? J Am Geriatr Soc. 2011;59:887–92.
Leong DP, Teo KK, Rangarajan S, Lopez-Jaramillo P, Avezum A Jr, Orlandini A, Seron P, Ahmed SH, Rosengren A, Kelishadi R, Rahman O, Swaminathan S, Iqbal R, Gupta R, Lear SA, Oguz A, Yusoff K, Zatonska K, Chifamba J, Igumbor E, Mohan V, Anjana RM, Gu H, Li W, Yusuf S. Prospective urban rural epidemiology (PURE) study investigators. Prognostic value of grip strength: findings from the prospective urban rural epidemiology (PURE) study. Lancet. 2015;386(9990):266–73.
Mathiowetz V, Kashman N, Volland G, Weber K, Dowe M, Rogers S. Grip and pinch strength: normative data for adults. Arch Phys Med Rehabil. 1985;66(2):69–74.
Kegelmeyer DA, Kloos AD, Thomas KM, Kostyk SK. Reliability and validity of the Tinetti mobility test for individuals with Parkinson disease. Phys Ther. 2007;87(10):1369–78.
Baker DI, King MB, Fortinsky FH, Graff LG, Gottschalk M, Acampora D, Preston J, Brown CJ, Tineti ME. Dissemination of an evidence-based multi-component fall risk assessment and management strategy throughout a geographic area. J Am Geriatr Soc. 2005;53(4):675–80.
Raîche M, Hébert R, Prince F, Corriveau H. Screening older adults at risk of falling with the Tinetti balance scale. Lancet. 2000;356(9234):1001–2.
Pape HC, Schemmann U, Foerster J, Knobe M. The aachen falls prevention scale-development of a tool for self-assessment of elderly patients at risk for ground level falls. Patient Saf Surg. 2015;14(9):7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Matthias Knobe, Meike Giesen, Sarah Plate, Gertraud Gradl-Dietsch, Benjamin Bücking, Daphne Eschbach, Walter van Laack, and Hans-Christoph Pape declare that they have no competing interests. No funds were received by any of the authors in support of this study.
Ethical approval
This study was approved by the Institutional Review Board at the RWTH Aachen University (Ethical Approval EK 171/14).
Informed consent
Informed consent was obtained from each participant and participation was voluntary.
Rights and permissions
About this article
Cite this article
Knobe, M., Giesen, M., Plate, S. et al. The Aachen Mobility and Balance Index to measure physiological falls risk: a comparison with the Tinetti POMA Scale. Eur J Trauma Emerg Surg 42, 537–545 (2016). https://doi.org/10.1007/s00068-016-0693-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-016-0693-2