Abstract
Background
Current recommendations for evaluation and safe discharge of penetrating chest trauma patients regarding pneumothorax (PTX) include a Chest X Ray (CXR) at the Emergency Department (ED) upon arrival and second CXR after 3 h if the first one is negative.
Purpose
To compare CXRs taken at the first and third hours of ED arrival and evaluate a 1 h period of observation instead of 3 h for safe discharge of patients with penetrating chest trauma.
Methods
In this cross-sectional study, all asymptomatic patients with penetrating chest trauma referred to a level 1 trauma center with negative initial Postero-Anterior (PA) CXRs (hour 0) were enrolled. Those with intoxication, tube thoracostomy, chest computed tomography, evidence of abdominal penetration, an overall elapsed timed of more than 1 h for admission to the ED, and refusal to take part in the study were excluded. Patients underwent subsequent PA CXRs at hours 1 and 3. A phone call follow up after 24 h was organized for each patient.
Results
A total of 68 patients were enrolled. There was 100 % concordance among CXRs performed at hours 1 and 3 in the study population. None of the patients showed clinical deterioration or PTX in CXR at hour 1 if remained asymptomatic during the first hour of observation.
Conclusion
Asymptomatic patients with penetrating chest trauma, negative initial PA CXR, no signs of intoxication, and no deterioration during the first hour of observation may be considered for discharge. Further evidence is required to make recommendations based on these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Penetrating thoracic trauma may be present with multiple immediate threats to patient survival. Prompt recognition and treatment of life-threatening injuries is critical in minimizing morbidity and mortality. Injuries may occur to pulmonary parenchyma, heart, tracheobronchial tree, esophagus, great vessels, or thoracic duct [1]. The vast majority of traumatic pulmonary injuries can be treated nonoperatively or with tube thoracostomy alone. The main indications for operative intervention are hemorrhage or large airway injury [2].
Although there is no question that advanced imaging provides superior resolution and diagnostic capability, there is still great utility in plain x-rays for rapid assessment of penetrating injuries to the chest [3]. The Advanced Trauma Life Support (ATLS) guidelines of the American College of Surgeons (ACS) include routine Chest X-Ray (CXR) in the adjuncts to primary survey section of trauma patient evaluation [4]. Although studies have shown higher sensitivity for Chest Computed Tomography (CCT) and Extended Focused Assessment by Sonography in Trauma (E-FAST) than plain CXR for pneumothorax (PTX) detection, performing CXR still remains the mainstay of initial evaluation and decision making for stable patients with penetrating trauma in many centers [5–7]. The presence of occult PTX, defined as recognizable PTX in CCT not identified by plain CXR, is shown to have little impact on clinicians’ decision making in many studies [8–10].
The incidence of PTX following chest trauma varies from 15 to 50 % [11]. After the initial negative CXR in penetrating chest trauma, the patient can be safely observed and a second CXR should be performed after a period of 3 h based on current recommendations. If clinical suspicion is not high and both CXRs are negative, the patient could be safely discharged after 3 h [12, 13]. However, a recent study has brought this 3 h period into question, raising the possibility that even a 1 h interval between the first negative CXR and the second film may be sufficient for clearance of patients with penetrating trauma in which a low clinical suspicion for PTX exists [14]. This cross sectional study was designed and performed for further evaluation of such a possibility in this group of patients. In this study we aimed to answer the following questions: (1) is there any difference between CXRs performed at hours 1 and 3 after a penetrating chest trauma in diagnosis of PTX? (2) Can asymptomatic patients with penetrating chest trauma be discharged safely after a negative CXR at hour 1 instead of hour 3?
Methods
Study design
This descriptive cross-sectional study was performed on a convenience sample of patients with penetrating trauma to the chest who were referred to Bahonar Hospital in Kerman, Iran. Bahonar Hospital, an academic level 1 trauma center, has an annual Emergency Department (ED) census of approximately 70,000 and is the main referral trauma center in Kerman, a city with a population of nearly 1 million in the southeast of Iran.
Patient management in Bahonar Hospital
Management of patients with penetrating trauma to the chest in our center begins with routine patient transfer to the critical care unit followed by patient assessment using ATLS guidelines. After the primary survey, if the condition of the patient permits, the first Postero-Anterior (PA) CXR is performed in an upright position in deep inspiration, followed by the second CXR after 3 h, given the first one reveals no abnormality requiring intervention. Both analog and digital systems are used in our center. In the study period, however, we used only the analog system for the study. CXRs in expiration are scarcely taken in our center, only if the routine protocol is interpreted as normal and the clinical suspicion is high. In such cases, however, most physicians prefer to perform a CT scan. If there is no evidence of PTX or other important abnormalities and the clinical impression implies no serious problem (including considerable symptoms, high risk for diaphragmatic injury, etc.) the patient will be discharged with a written warning sheet from the ED after 3 h. Proper wound care (dressings, sutures, oral or topical antibiotics) is done before discharge depending on the case. A surgery clinic follow-up visit is organized and recommended for all patients.
Study population and protocol
A convenience sample of asymptomatic patients with isolated penetrating trauma to the chest admitted to Bahonar Hospital ED between 1 December 2012 and 30 November 2013 with a negative initial CXR regarding PTX or other life threatening conditions comprise our study population. We defined “asymptomatic” as having no symptoms regarding PTX such as shortness of breath or chest pain (excluding a mild to moderate local pain restricted to the wound) [11]. Data collection was performed prospectively for all patients. Exclusion criteria were defined as more than 1 h interval between trauma and presentation to the ED, evidence of abdominal penetration (e.g. free fluid in the FAST exam or abdominal tenderness), thoracostomy by chest tube or needle during the first 3 h of presentation at the discretion of surgical managing team (e.g. because of severe dyspnea, marked decreased breath sounds, or hemodynamic instability), signs of intoxication by alcohol or drugs with unreliable symptoms, CCT performed in the first 3 h at the discretion of managing team, and patients’ refusal to participate in the study.
The collector of cases in this study was a resident of Emergency Medicine (Post Graduate Year 3), acting as an observer except for organizing an additional CXR 1 h after the first one (the presenting time or hour 0 CXR). By taking patients’ informed consents (or their legal caretakers in case of patients under 18) to participate in the study (see Compliance with Ethical Requirements) after the initial negative CXR, the following radiographs were performed in hours 1 and 3. All of the 3 CXRs (hours 0, 1, and 3) were evaluated by a resident of radiology before discharge and a board certified attending physician of radiology (a single person) after discharge, both were blinded to our study objectives, patient names, and the hour the radiographs were taken in. The radiology attending physician’s reports were set as the final diagnosis. The agreement among the managing team, radiology resident, and the attending physician of radiology for each case was also documented. A 24 h follow up by phone call was done for each patient after discharge in addition to documentation of surgery clinic records.
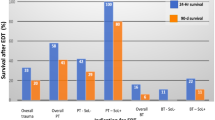
Results
Of 134 patients with penetrating chest injuries, a total of 68 patients were enrolled in the study period (Fig. 1). The mean (SD) age was 25.6 (7.4), with minimum of 15 and maximum of 68 years. Only 1 patient was female and only 1 patient was under 18 years of age. For 12 (17 %) patients, there were more than one wound, 8 of which were in the upper limbs and none were limb or life threatening. As a total, there were 75 thoracic wounds in 68 patients. All injuries were caused by stab wounds (Table 1).
The mean (SD) time from admission to the first CXR (hour 0) was 17.9 (9.8) min. CXRs for hours 1 and 3 were done after a mean (SD) time of 63.2 (15.7) and 184.9 (7.7) min from admission, respectively.
Regarding PTX, all patients included in the study had negative CXRs in hours 1 and 3: there was 100 % compatibility among CXRs in hours 1 and 3 in all asymptomatic patients with negative entrance time CXR, no evidence of abdominal penetration, and no clinical deterioration in the observation period. Two patients underwent tube thoracostomy in the first hour of ED arrival at the discretion of surgical managing team (Fig. 1). All symptomatic patients requiring intervention developed the symptoms in the first hour of ED arrival, and all cases diagnosed with PTX in CXR revealed the diagnosis in the entrance time CXR (hour 0).
We had the report of radiology resident before discharge, but we also matched all the reports and diagnoses with the report of radiology attending physician after patient’s discharge. Except for two cases with small volume pleural fluid (probably hemothoraces), no disagreement was observed among the attending physician of radiology, radiology residents, and the management team including surgeons and emergency physicians (Table 2). There were, however, some abnormalities reported only by the radiologist; none of them were considered by the surgical team to alter the treatment strategy. These included the following: parenchymal calcification (two cases), aortic arch calcification (three cases), pulmonary hilar vessels engorgement (three cases), pulmonary congestion (five cases), and hyperaerated lungs (12 cases).
For each patient, a follow up phone call was performed 24 h after discharge. Unfortunately, only 55 patients were available for follow up, none of them reported any problems after discharge. No readmissions for these patients were recorded in the admission system of hospital 1 week after patients’ discharge (admission systems of hospitals are not inter-connected in Iran). According to the surgery post-op clinic records, 46 patients attended for a post-op visit or suture removal, none of them showed complications. Overall, 11 patients were totally lost for follow up.
Discussion
A complete concordance between the first and third hour radiographs in all patients with no initial symptoms, negative initial (entrance time) CXRs, no clinical deterioration during the 3 h follow up period, and no evidence of abdominal penetration is the main result of this study. As mentioned earlier, current recommendations in the workup for penetrating trauma to the chest include two CXRs 3 h apart; one at the entrance time and one 3 h later [12, 13]. A few decades ago, the evidence in the literature reported delayed occurrence of PTX and HTX, yielding the recommendation of at least a 6 h follow- up in both blunt and penetrating trauma patients [15, 16]. More recent evidence, however, decreased this period to 3 h in penetrating trauma, but the recommended follow up time for PTX in blunt trauma is still 6 h based on the current evidence [11]. In 2013, Berg et al. [14] evaluated a 1 h follow up period for asymptomatic patients with penetrating chest trauma. They found two cases (2.6 %) of delayed PTX in the third hour CXR, both of them were successfully managed without observation. They concluded that a 1 h period of observation may be sufficient for asymptomatic patients with penetrating chest trauma.
In the present study, the incidence of PTX in penetrating trauma patients at the ED presentation time was 24 % (33 of the initial 134 patients). When added to the 1 PTX and 2 hemopneumothoraces found in CCT, one may conclude that the incidence of PTX in the first hour of ED arrival was 26.8 % in this study. The two patients underwent tube thoracostomy at the discretion of surgical team were considered as unknown diagnoses, because there was no documentation on air egress during pleural penetration by the surgical team. After the documented findings in the first hour of patients’ arrival, there was no additional event in the asymptomatic study group. In other words, we did not find any delayed event in the patients who were asymptomatic and remained so in the observation period. This discrepancy between our study and the study performed by Berg et al. can be explained by the initial method of standing PA CXR instead of a supine Antero-Posterior (AP) one, enabling us to detect probably all the abnormalities found in the second CXR (hour 1) in that study at ED entrance time (hour 0). In contrast to Berg et al., we did not find any additional abnormalities in the 3rd hour CXR; fortunately, those PTX cases found in the 3rd hour in that study did not need any intervention.
Using the analog system to obtain CXRs was another difference between our study and the recent published ones which may be considered to be responsible for the discrepancies in the results. In fact, we had the facility of digital radiography in our center except for the first 3 months of this study due to a technical problem. Although the digital systems are proven to be faster and more cost effective than the analog ones, there is no difference between the accuracy of digital and analog systems in the literature [17–19]. As a result, we decided to continue the research with the analog system.
The high number of patients who refused to take part in the study (13 cases) limited our study population size. Patients underwent tube thoracostomy without a specific diagnosis, intoxicated patients with unreliable symptoms, those with CCTs performed in the first hour, and those presented more than 1 h from trauma added to this limitation. We could not find a considerable number of patients in the phone call follow up or post-op clinic (11 patients), but since Bahonar Hospital is the only trauma center in Kerman and there was no recorded readmissions 1 week after trauma, the incidence of complications may be concluded to be low or zero. Although we performed our data collection in a prospective manner, the final evaluation of CXRs by the attending physician of radiology after discharge of the patients contributes a retrospective part to our method. However, no disagreement was found between radiology residents and the attending physician in critical diagnoses important to our management.
As a conclusion, asymptomatic patients with penetrating chest trauma with negative initial PA CXR, no signs of intoxication, and no deterioration during the first hour of observation may be considered for discharge based on our study results. This conclusion should not be used as a recommendation in this step because this is an exploratory study and there is a more conservative approach which is currently advised based on previous reports in the literature. If approved by future studies, however, the proposed approach can be helpful in managing a busy ED with less crowding of patients being observed.
References
Wright FL, Esposito TJ. Penetrating trauma to the chest. In: Di Saverito S, Tugnoli G, Catena F, Ansaloni L, Naidoo N, editors. Trauma surgery. Milan: Springer; 2014. p. 275–94.
Fagenholz P, Velmahos G. Surgical treatment of thoracic trauma: lung. In: Di Saverito S, Tugnoli G, Catena F, Ansaloni L, Naidoo N, editors. Trauma surgery. Milan: Springer; 2014. p. 77–90.
Bukur M, Green DJ. Plain X-rays for penetrating trauma. In: Velmahos GC, Degiannis E, Doll D, editors. Penetrating trauma. Berlin: Springer; 2012. p.93–100. doi:10.1007/978-3-642-20453-1_13.
American College of Surgeons. Advanced trauma life support for doctors, student course manual. 9th ed. Chicago, IL: ACS; 2012.
Mollberg NM, Wise SR, De Hoyos AL, Ju Lin F, Merlotti G, Massab MG. Chest computed tomography for penetrating thoracic trauma after normal screening chest roengenogram. Ann Thorac Surg. 2012;93(6):1830–5.
Nandipati KC, Allamaneni S, Kakarla R, Wong A, Richards N, Sattefield J, Turner JW, et al. Extended focused assessment with sonography for trauma (EFAST) in the diagnosis of pneumothorax: experience at a community based level I trauma center. Injury. 2011;42(5):511–4.
Ku BS, Fields JM, Carr B, Everett WW, Gracias VH, Dean AJ. Clinician-performed ultrasound for the diagnosis of traumatic pneumothorax. West J Emerg Med. 2013;14(2):103–8.
Ball CG, Kirkpatrick AW, Feliciano DV. The occult pneumothorax: What have we learned? Can J Surg. 2009;52(5):E173–9.
Moore FO, Goslar PW, Coimbra R, Velmahos G, Brown CVR, Thomas B Jr, et al. Blunt traumatic pneumothorax: is observation safe? Results of a prospective AAST multicenter study. J Trauma. 2011;70(5):1019–25.
Plurad D, Green D, Demetriades D, Rhee P. The increasing use of chest computed tomography in trauma: is it being overutilized? J Trauma. 2007;62(3):631–5.
Eckstein M, Henderson SO. Thoracic trauma. In: Marx JA, Hockberger RS, Walls RM, Biros MH, Danzl DF, Gausche-Hill M, Jagoda A, et al., editors. Rosen’s emergency medicine. 8th ed. New York: Elsevier Saunders; 2014. p. 431–58.
Shatz TV, De la Petraja J, Erbella J, Hameed M, Vail SJ. Efficacy of follow-up evaluation in penetrating thoracic injuries: 3 vs 6 hour radiographs of the chest. J Emerg Med. 2001;20(3):281–4.
Seamon MJ, Medina CR, Pieri PG, Fisher CA, Gaughan JP, Bradley KM, et al. Follow up after asymptomatic penetrating thoracic injury: 3 hours is enough. J Trauma. 2008;65(3):549–53.
Berg RJ, Inaba K, Recinos G, Barmparas G, Teixeira PG, Georgiou C. Prospective evaluation of early follow-up chest radiography after penetrating thoracic injury. W J Surg. 2013;37(6):1286–90. doi:10.1007/s00268-013-2002-0.
Weigelt JA, Aurbakken CM, Meier DE, Thal ER. Management of asymptomatic patients following stab wounds to the chest. J Trauma. 1982;22(4):290–4.
Shorr RM, Crittenden M, Indeck M, Hartunian SL, Rodrguez A. Blunt thoracic trauma: analysis of 515 patients. Ann Surg. 1987;206(2):200–5.
Dalla Palma L, Grisi G, Cuttin R, Rimondini A. Digital vs conventional radiography: cost and revenue analysis. Eur Radiol. 1999;9:1682–92.
Lai KW-S, Langlois S, Le P. A comparative study of a digital radiography system. Aust Radiol. 1999;43(2):197–200.
Colin C, Vergnon P, Guibaud L, Borson O, Pinaudeou D, Perret Du, Cray MH, et al. Comparative assessment of digital and analog radiography: diagnostic accuracy, cost analysis, and quality of care. Eur J Radiol. 1998;26(3):226–34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the Institutional Review Board of Kerman University of Medical Sciences and performed in accordance with declaration of Helsinky. Since this study involved a single CXR in addition to the standard of care (the hour 1 CXR), a statement was added to the consent form of the patients, including the translation of the following announcement into Persian: “This study involves radiation exposure from a chest X-ray. As part of everyday living, everyone is exposed to a small amount of background radiation that comes from the environment you live in. The radiation dose you will receive in this study is about the amount that you receive over 3 days from background radiation. The risk from this dose is small. This radiation exposure is not necessary for your medical care but is necessary to obtain the research information desired.”
Conflict of interest
Latifeh Seidzadeh Gooklan, Alireza Yari, Masoud Mayel, Mitra Movahedi, Sarir Nazemi, and Amirhossein Mirafzal report no conflicts of interests.
Rights and permissions
About this article
Cite this article
Seidzadeh Gooklan, L., Yari, A., Mayel, M. et al. Observation period for asymptomatic penetrating chest trauma: 1 or 3 h?. Eur J Trauma Emerg Surg 44, 829–833 (2018). https://doi.org/10.1007/s00068-015-0623-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-015-0623-8