Abstract
Objective
To evaluate the effect of prophylactic cranial irradiation (PCI) on overall survival (OS) in patients with extensive small cell lung cancer (ESCLC).
Methods
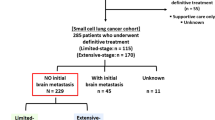
Between April 2005 and May 2014, 204 patients with ESCLC who had any response (according to RECIST 1.1) to initial chemotherapy were reviewed. All patients had undergone appropriate imaging tests to exclude brain metastases before initial chemotherapy. PCI was performed on 45 patients (22.1 %) and the remaining patients (77.9 %) received no such treatment (control group). Primary endpoint was OS. The incidence of brain metastases, brain metastases-free survival (BMFS), and adverse effects were also evaluated.
Results
Survival data of the 204 patients were analyzed statistically. PCI significantly prolonged median OS from 12.6 to 16.5 months as compared to the control group (hazard ratio, HR, 0.63; 95 % confidence interval, CI, 0.41 to 0.96; p = 0.033). PCI significantly lowered the risk of brain metastases (HR 0.48; 95 % CI 0.30 to 0.76; p = 0.001). The 1‑year incidence of brain metastases was 17.1 and 55.9 % in the PCI and control group, respectively. PCI significantly correlated with the increased median BMFS (p = 0.002). Additionally, multivariate analyses demonstrated that PCI was a favorable independent predictor of OS, BMFS, and the incidence of brain metastases. Acute and chronic adverse effects were generally low grade and well tolerated in patients receiving PCI.
Conclusion
PCI after any response to initial chemotherapy significantly improved OS of ESCLC patients analyzed in this study.
Zusammenfassung
Ziel
Beurteilung des Effekts der prophylaktischen kranialen Bestrahlung (PCI) auf das Gesamtüberleben (OS) bei Patienten mit ausgedehntem kleinzelligem Lungenkarzinom (ESCLC).
Methoden
Zwischen April 2005 und Mai 2014 wurden 204 Patienten mit ESCLC nach Ansprechen auf eine initiale Chemotherapie (gemäß RECIST 1.1) untersucht. Vor der Chemotherapie wurden bei allen Patienten Untersuchungen mit entsprechenden Bildgebungsverfahren durchgeführt, um Metastasen im Gehirn auszuschließen. 45 Patienten (22,1 %) wurden anschließend mit PCI behandelt, die übrigen (77,9 %) erhielten keine Behandlung (Kontrollgruppe). Der primäre Endpunkt der Studie war das OS. Ebenfalls beurteilt wurden das Auftreten von Hirnmetastasen, das hirnmetastasenfreie Überleben (BMFS) und Nebenwirkungen.
Ergebnisse
Die Daten zum Überleben der 204 Patienten wurden statistisch ausgewertet. Die PCI verlängerte das mittlere OS im Vergleich zur Kontrollgruppe signifikant von 12,6 Monaten auf 16,5 Monate (Hazard Ratio [HR]: 0,63; 95 %-Konfidenzintervall [KI]: 0,41–0,96; p = 0,033). Das Risiko von Hirnmetastasen wurde signifikant verringert (HR: 0,48; 95 %-KI: 0,30–0,76; p = 0,001). Die 1‑Jahres-Inzidenz von Hirnmetastasen betrug dabei 17,1 % in der PCI- und 55,9 % in der Kontrollgruppe. Zudem konnte ein signifikanter Zusammenhang zwischen PCI und dem mittleren BMFS festgestellt werden (p = 0,002). Multivariate Analysen zeigten zusätzlich, dass die PCI ein günstiger, unabhängiger Prädiktor für OS, BMFS und die Inzidenz von Hirnmetastasen ist. Akute und chronische Nebenwirkungen waren gering und wurden gut von den mit PCI behandelten Patienten vertragen.
Schlussfolgerungen
Das OS der in dieser Studie untersuchten Patienten mit ESCLC nach Ansprechen auf eine initiale Chemotherapie konnte durch PCI signifikant verbessert werden.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Small cell lung cancer (SCLC) accounts for nearly 14 % of all primary lung cancers [1–4] and approximately two thirds of these present as extensive SCLC (ESCLC) due to the rapid doubling time and early wide dissemination. Combined chemotherapy and thoracic radiotherapy have improved response rates and short-term survival [2, 5–10], but long-term survival is still disappointing [1].
Furthermore, central nervous system metastases are often observed in this disease. The incidence of brain metastases is about 18 % at diagnosis [11] and reaches approximately 58 % within 2 years [12]. Most of these patients die from such brain metastases [13].
Previous studies [14–17] and meta-analyses [18, 19] have demonstrated that prophylactic cranial irradiation (PCI) can reduce the incidence of brain metastases and improve overall survival (OS) in patients with limited small cell lung cancer (LSCLC). However, for ESCLC patients, the effect of PCI on OS remains highly controversial.
One meta-analysis [18] reported an increased 3‑year survival rate from 15.3 to 20.6 % in patients receiving PCI, but the population with ESCLC was rather small. In 2007, a randomized trial [20] from the European Organization for Research and Treatment of Cancer (EORTC) reported that PCI could lower the risk of brain metastases and improve OS of ESCLC patients with a response to initial chemotherapy. In 2011, these results were considered category-1 evidence by the National Comprehensive Cancer Network (NCCN) clinical practice guideline, recommending PCI for ESCLC patients showing a response to initial chemotherapy. However, the EORCT trial was questioned for not performing brain imaging on patients without symptoms of brain metastases before randomization [20]; hence, some asymptomatic patients who should have received irradiation with 30–34 Gy in 15–17 fractions were underdosed. The dose fractionation of the EORCT study was also challenged (mostly 20 Gy in 5 fractions), which was not a common prescription for PCI in North America.
In contrast, the latest preliminary data of a phase III randomized trial from Japan [21] indicated that PCI had a detrimental effect on OS in ESCLC patients. Therefore, the revised NCCN guideline degraded the evidence level from 1 to 2A in 2016, awaiting more upcoming data to strengthen or deny such a recommendation.
By including the patients without the aforementioned limitations, this retrospective study aims to investigate whether PCI could improve OS in ESCLC patients.
Patients and methods
Patients
A study on ESCLC patients was initiated with valid approval from the hospital Ethics Committee. A total of 204 patients were reviewed, all of whom were pathologically diagnosed with ESCLC and had a complete (CR) or partial response (PR) to initial chemotherapy between April 2005 and May 2014. For 187 out of 204 patients, the absence of brain metastases was confirmed using cranial MRI. The remaining 17 patients were confirmed with cranial CT instead, due to MRI contraindications such as artificial implants, cardiac pacemakers, dental prostheses, contraceptive ring, etc. Written informed consent was provided by each patient before treatment.
Inclusion criteria
The main inclusion criteria were: 1) pathologically diagnosed ESCLC; 2) Eastern Cooperative Oncology Group Performance Status (ECOG-PS) ≤2; 3) age ≥18 years; 4) a response to initial chemotherapy; 5) no evidence of brain metastases at baseline; 6) no previous radiotherapy in the head and neck region; 7) no other cancer; 8) complete follow-up data.
Performance status, diagnosis, and staging
As mentioned above, performance status was assessed according to the ECOG-PS scale. The diagnosis of SCLC was determined by the outcomes of bronchofiberoscopy, mediastinoscopy, percutaneous lung biopsy, or lymph node biopsy. The staging of patients was based on the criteria of the US Veterans Administration Lung Cancer Group. ESCLC referred to the lesion beyond the ipsilateral hemithorax, including contralateral supraclavicular nodes, malignant pericardial or pleural effusion, and distant hematogenous metastases, and also included patients with extensive local disease that was not covered by a reasonable radiation portal. Stage determination was also assisted by other available initial examinations including CT, MRI, abdominal ultrasonography, bone scan, and positron-emission tomography (PET)/CT.
Treatment and treatment response
All involved patients had received four to six cycles of initial chemotherapy and showed positive responses, including CR and PR. Treatment response was defined according to the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1 criteria. CR: disappearance of all target lesions. Any pathological lymph nodes (whether target or non-target) must show a reduction in the short axis to <10 mm. PR: at least a 30-% decrease in the sum of diameters of target lesions, taking as reference the baseline summed diameters.
PCI was delivered using a three-dimensional conformal radiation therapy (3DCRT) technique comprising two opposing lateral fields. Most patients in the PCI group received a total prescribed dose of 25 Gy in 10 fractions. All the 204 patients involved were eligible and may potentially benefit from PCI according to NCCN criteria (attaining CR or PR; good PS of 0–2; acute toxicities of initial therapy have resolved; no impaired neurocognitive function). As a retrospective study, only 45 patients were finally treated with PCI and the remaining were not, because: 1) PCI was not a clinical routine at the authors’ center when the patients were treated and 2) some patients refused PCI due to concerns of side effects or financial burden.
Follow-up
Patients were followed up every 6 weeks during initial chemotherapy and every 3 months after recovery from primary therapy. The median follow-up period was 11.2 months (range 2.9–71.7 months).
Definition of endpoints
The primary endpoint of this study was OS, defined as the interval from the date of diagnosis to the date of death or patient censored at the last follow-up. The secondary endpoints were the incidence of brain metastases, brain metastases-free survival (BMFS), and adverse effects. Brain metastases during the course of disease should be testified by imaging evidence. BMFS was defined as the interval from the date of diagnosis to the date of development of brain metastases or death or patient censored at the last follow-up. Acute adverse effects were assessed by the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0. To evaluate late adverse effects, the internationally accepted “LENT-SOMA” scoring system (Late Effects Normal Tissue Task Force-Subjective, Objective, Management, Analytic) was used.
Statistical analysis
Patients’ characteristics were described by median values and the interquartile range (IQR) for non-normally distributed continuous variables. Categorical variables were compared by chi-square or Fisher’s exact test. Survival curves were generated by the Kaplan–Meier method and compared using log-rank tests. Univariate and multivariate analyses of OS and BMFS were performed with the Cox proportional hazard regression model; univariate and multivariate analyses of the incidence of brain metastases were performed by logistic regression analysis. P < 0.05 was considered statistically significant. SPSS 21.0 software (IBM; Armonk, NY, USA) was used for statistical analysis.
Results
Patient characteristics
The 204 reviewed patients included 172 males and 32 females. Median age was 58 years (IQR 52–63 years). PCI was delivered to 45 (22.1 %) patients. General characteristics of the cohort stratified according to PCI and control groups are shown in Table 1. The baseline characteristics of the two groups were well balanced.
Patient treatment
All patients received initial chemotherapy and showed a response to the treatment. Of the 45 patients treated with PCI, 42 received 25 Gy in 10 fractions, 1 patient received 30 Gy in 10 fractions, and 2 patients received 22.5 Gy in 9 fractions (the last fraction was rejected by these 2 patients). During the observation period, 11 out of 45 patients receiving PCI developed brain metastases, 22.2 % of whom were treated with whole-brain radiation therapy (WBRT) after brain metastases. Of the 159 cases in the control group, 91 patients developed brain metastases, 43.2 % of whom were treated with WBRT.
Overall survival
During the follow-up period, 29 out of 45 patients in the PCI group died, as did 83 out of 159 patients in the control group. As shown in Fig. 1, patients receiving PCI had significantly longer OS (median 16.5 months) than those in control group (median 12.6 months; p = 0.033). The hazard ratio (HR) for death was 0.63 (95% confidence interval, CI, 0.41 to 0.96) among the patients receiving PCI.
Incidence of brain metastases and PCI
Development of brain metastases was observed in 11 out of 45 patients receiving PCI (24.4 %) and in 91 out of 159 control patients (57.2 %). The cumulative incidence of brain metastases in the PCI and control groups is shown in Fig. 2. The results indicated that the incidence of brain metastases was significantly lower in the PCI group than in controls (HR 0.48; 95 % CI 0.30 to 0.76; p = 0.001). The 1‑year cumulative risk of brain metastases was 17.1 and 55.9 % in the PCI and control group, respectively.
Cumulative incidence of brain metastases. The solid line suggests that the cumulative incidence of brain metastases for the patients receiving prophylactic cranial irradiation (PCI) increases with time. The dotted line shows that the cumulative incidence of brain metastases for patients not receiving PCI also increases with time. The difference between the cumulative incidences of brain metastases between patients in PCI and control groups was significant (p = 0.001)
Brain metastases-free survival
As shown in Fig. 3, BMFS in the PCI group was significantly prolonged compared to the control group (p = 0.002). Median BMFS was 14.1 months for the patients receiving PCI and 10.7 months for the patients as control.
Univariate and multivariate analyses of OS, BMFS, and incidence of brain metastases
All factors influencing the decision whether to perform PCI or not were included in the multivariate analyses, the results of which are shown in Table 2. These analyses suggested that PCI, ECOG, and liver metastases were independent prognostic factors of OS. Additionally, multivariate analysis demonstrated that PCI and liver metastases were independent predictors of BMFS (Table 2). What’s more, PCI was significantly associated with the incidence of brain metastases and could become a favorable independent factor for predicting the incidence of brain metastases.
Adverse effects
The observed primary acute adverse effects included mainly headache, nausea and vomiting, fatigue and lethargy, and skin reactions, which were graded according to the CTCAE version 4.0 scoring scale (Table 3). Late adverse effects mainly included headache and somnolence, both of which were below grade 2 according to the LENT-SOMA scale for brain (Table 4).
Discussion
Up until now, no consensus has been reached regarding the impact of PCI on OS in ESCLC, due to inconsistent results from previous randomized trials [20, 21]. The current study observed that PCI significantly prolonged OS in ESCLC patients, from 12.6 months in the control group to 16.5 months in the PCI group (from the date of diagnosis; HR 0.63; 95 % CI 0.41 to 0.96; p = 0.034). In addition, multivariate analyses indicated that PCI was a favorable independent prognostic factor of OS. The favorable survival results in this study were consistent with the EORCT trial [20], which reported that PCI could significantly improve OS in ESCLC patients (p = 0.003), from 5.4 months in the control group to 6.7 months in the PCI group (from the date of randomization rather than the date of diagnosis; the interval between diagnosis and randomization was 4.2 months; HR, 0.68; 95 % CI 0.52 to 0.88). However, adverse results were released as an abstract at the 2014 ASCO Annual Meeting [21], reporting that PCI significantly deteriorated the OS of ESCLC patients, from 15.1 months in the control group to 10.1 months in the PCI group (from the date of diagnosis; HR 1.38; 95 % CI 0.95 to 2.01; p < 0.001). Unfortunately, the full article has not been published [21], which prevents its comparison with the EORCT trail [20] and the current study which report opposing conclusions.
Relative to the EORCT trial [20], the patients in this study had modestly better baseline conditions of younger age, better performance status, and less patients with distant metastases (Table 1). Patients in both the current study and the EORCT trial [20] received four to six cycles of initial chemotherapy and had a response to the treatment. Although a beneficial impact on OS was observed in both the EORTC and the present study, the current work has overcome several deficiencies of the EORTC trial. Firstly, the EORTC trial did not perform brain imaging for each patient before randomization. Seute et al. [22] reported that approximately 13 % of patients with SCLC presented with asymptomatic brain metastases at the time of diagnosis. Such patients need a therapeutic radiation dose rather than a lower dose for PCI. Therefore, the current study excluded brain metastases before initial chemotherapy. Secondly, the PCI fractionalization for the majority of patients in the present study (93.3 %) was closer to the clinical routine of North America (25 Gy/10 fractions) than in the EORCT trial (mostly 20 Gy/5 fractions). Thirdly, Takashi et al. [21] have questioned the wide variations of total dose from 20 to 39 Gy in the EORCT study, whereas this range was much smaller in the current study (22.5 to 30 Gy). Last but not least, Takashi et al. [21] pointed out that the initial chemotherapy did not include platinum in the EORCT trial, whereas a platinum-based chemotherapy regimen was administered in 97.8 % of patients in the PCI group and 95.6 % of patients in the control group of the current study. Based on comparable patient baseline conditions but avoiding some limitations, this retrospective study echoed the EORTC trial findings that PCI could significantly improve OS in ESCLC patients.
The inconsistent conclusions of the three studies may suggest that not all patients with a response to chemotherapy would benefit from PCI in terms of OS. Maybe some other unconsidered characteristics of patients or treatment have contaminated the PCI effect on OS of ESCLC patients. For instance, a study conducted by Greenspoon et al. [23] reported that patients with baseline weight loss of less than 5 kg and a response to chemotherapy may benefit most from PCI. Further comparison should be made after final publication of the Japanese trial [21], and further similar studies may be needed to clarify the indications for PCI in ESCLC patients.
In addition, the current study found that PCI significantly lowered the risk of brain metastases (p = 0.001), where the 1‑year cumulative risk of brain metastases was 17.1 vs. 55.9 % for the PCI and control groups, respectively. Slotman et al. [20] also assessed the role of PCI in reducing the incidence of brain metastases in ESCLC. The results showed that the 1‑year incidence rate of brain metastases in PCI group was 14.6 %, which was significantly lower than that in the control group (40.4 %, p < 0.001). Soon afterwards, Takashi et al. [21] reported that PCI significantly reduced the incidence of brain metastases compared to the control group (p < 0.001) in ESCLC, where the 1‑year incidence of brain metastases was 32.4 % in the PCI group vs. 58.0 % in the control group. Consistent with the results of previous trials, the present study reconfirmed that PCI lowered the incidence of brain metastases significantly for ESCLC patients. Moreover, multivariate analyses further proved that PCI was an independent predictor of the incidence of brain metastases. Subgroup analysis suggested no significant differences in the development of brain metastases between the patients receiving CT or MRI.
Kiricuta et al. [24] and Sas-Korczynska et al. [25] reported that PCI could delay development of brain metastases. Gregor et al. [17] and Seute et al. [11] echoed these findings in their trials, reporting that PCI indeed postponed development of brain metastases. However, the previous studies were based on LSCLC patients, and thus may not be applicable to ESCLC. The current study compared BMFS in two groups, finding that PCI improved BMFS in ESCLC patients (p = 0.002). Further multivariate analysis indicated that PCI was a positive prognostic factor for BMFS.
The primary acute and late adverse effects observed in this work are in line with previous studies [20] and generally well tolerated.
In addition to PCI, a study [26, 27] on prophylactic thoracic irradiation (PTI) was presented at the 2014 ASCO Annual Meeting, reporting that PTI improved progression-free and 2‑year survival, although PTI did not influence the risk of death in the first year; therefore recommending PTI for all ESCLC patients with a response to chemotherapy. Considering the limited existing data, more studies on PTI might be needed in the future.
As to limitations, this retrospective single-center study involved a limited sample size. More well-designed prospective studies are recommended to determine whether PCI could improve OS in ESCLC. These studies shall include and analyze more patient risk factors to establish appropriate indications for PCI aimed at a maximum patient benefit.
Conclusion
This study indicated that PCI, for patients with any response to the initial chemotherapy, significantly improved OS, reduced the incidence of brain metastases, and delayed development of brain metastases in ESCLC patients. It should be noted that these results are only representative of the analyzed patient population, as this was a single-center retrospective analysis.
References
Govindan R, Page N, Morgensztern D, Read W, Tierney R, Vlahiotis A et al (2006) Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. J Clin Oncol 24:4539–4544
Feld R, Pringle JF, Evans WK, Keen CW, Quirt IC, Curtis JE et al (1981) Combined modality treatment of small cell carcinoma of the lung. Arch Intern Med 141:469–473
Oberg K, Hellman P, Kwekkeboom D, Jelic S (2010) Neuroendocrine bronchial and thymic tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 21(Suppl 5):v220–v222
Simon GR, Wagner H (2003) Small cell lung cancer. Chest 123:259S–271S
Socinski MA, Bogart JA (2007) Limited-stage small-cell lung cancer: the current status of combined-modality therapy. J Clin Oncol 25:4137–4145
Simon M, Argiris A, Murren JR (2004) Progress in the therapy of small cell lung cancer. Crit Rev Oncol Hematol 49:119–133
Chua YJ, Steer C, Yip D (2004) Recent advances in management of small-cell lung cancer. Cancer Treat Rev 30:521–543
Stupp R, Monnerat C, Turrisi AR, Perry MC, Leyvraz S (2004) Small cell lung cancer: state of the art and future perspectives. Lung Cancer 45:105–117
Schnabel T, Schmitt G (1993) The role of radiotherapy in the management of small cell lung cancer (SCLC). Strahlenther Onkol 169:329–338
Kurup A, Hanna NH (2004) Treatment of small cell lung cancer. Crit Rev Oncol Hematol 52:117–126
Seute T, Leffers P, Ten VG, Twijnstra A (2004) Neurologic disorders in 432 consecutive patients with small cell lung carcinoma. Cancer 100:801–806
Komaki R, Cox JD, Whitson W (1981) Risk of brain metastasis from small cell carcinoma of the lung related to length of survival and prophylactic irradiation. Cancer Treat Rep 65:811–814
Hardy J, Smith I, Cherryman G, Vincent M, Judson I, Perren T et al (1990) The value of computed tomographic (CT) scan surveillance in the detection and management of brain metastases in patients with small cell lung cancer. Br J Cancer 62:684–686
Arriagada R, Le Chevalier T, Riviere A, Chomy P, Monnet I, Bardet E et al (2002) Patterns of failure after prophylactic cranial irradiation in small-cell lung cancer: analysis of 505 randomized patients. Ann Oncol 13:748–754
Arriagada R, Le Chevalier T, Borie F, Riviere A, Chomy P, Monnet I et al (1995) Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. J Natl Cancer Inst 87:183–190
Yang GY, Matthews RH (2000) Prophylactic cranial irradiation in small-cell lung cancer. Oncologist 5:293–298
Gregor A, Cull A, Stephens RJ, Kirkpatrick JA, Yarnold JR, Girling DJ et al (1997) Prophylactic cranial irradiation is indicated following complete response to induction therapy in small cell lung cancer: results of a multicentre randomised trial. United Kingdom Coordinating Committee for Cancer Research (UKCCCR) and the European Organization for Research and Treatment of Cancer (EORTC). Eur J Cancer 33:1752–1758
Auperin A, Arriagada R, Pignon JP, Le Pechoux C, Gregor A, Stephens RJ et al (1999) Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. Prophylactic Cranial Irradiation Overview Collaborative Group. N Engl J Med 341:476–484
Meert AP, Paesmans M, Berghmans T, Martin B, Mascaux C, Vallot F et al (2001) Prophylactic cranial irradiation in small cell lung cancer: a systematic review of the literature with meta-analysis. BMC Cancer 1:5
Slotman B, Faivre-Finn C, Kramer G, Rankin E, Snee M, Hatton M et al (2007) Prophylactic cranial irradiation in extensive small-cell lung cancer. N Engl J Med 357:664–672
Seto T, Takahashi T, Yamanaka T, Harada H (2014) Prophylactic cranial irradiation (PCI) has a detrimental effect on the overall survival (OS) of patients (pts) with extensive disease small cell lung cancer (ED-SCLC):Results of a Japanese randomized phase III trial [abstract. J Clin Oncol 32(Suppl 5):Abstract 7503 (http://meetinglibrary.asco.org/content/129034-144)
Seute T, Leffers P, Wilmink JT, Ten VG, Twijnstra A (2006) Response of asymptomatic brain metastases from small-cell lung cancer to systemic first-line chemotherapy. J Clin Oncol 24:2079–2083
Greenspoon JN, Evans WK, Cai W, Wright JR (2011) Selecting patients with extensive-stage small cell lung cancer for prophylactic cranial irradiation by predicting brain metastases. J Thorac Oncol 6:808–812
Kiricuta IC, Bohndorf W (1996) Adjuvant whole-brain irradiation in small-cell bronchial carcinoma. Strahlenther Onkol 172:553–558
Sas-Korczynska B, Korzeniowski S, Wojcik E (2010) Comparison of the effectiveness of “late” and “early” prophylactic cranial irradiation in patients with limited-stage small cell lung cancer. Strahlenther Onkol 186:315–319
Slotman BJ, van Tinteren H, Praag JO et al (2015) Use of thoracic radiotherapy for extensive stage small-cell lung cancer: a phase 3 randomised controlled trial. Lancet 385:36–42
Griesinger F (2014) ASCO 2014-Neues zu Lungentumoren. http://www.trillium.de/fileadmin/user_upload/Zeitschriften/Trillium_Krebsmedizin/Archiv/2014_2/asco_lungentumoren_griesinger.pdf. Accessed 21 May 2016
Acknowledgements
This work was jointly supported by the National Natural Science Foundation of China (11505012) and the Beijing Municipal Administration of Hospitals’ Youth Programme (QML20151004).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Y. Chen, J. Li, Y. Hu, Y. Zhang, Z. Lin, Z. Zhao, and S. Jiao declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Yi Chen and Jinyu Li contributed equally to this work.
Rights and permissions
About this article
Cite this article
Chen, Y., Li, J., Hu, Y. et al. Prophylactic cranial irradiation could improve overall survival in patients with extensive small cell lung cancer. Strahlenther Onkol 192, 905–912 (2016). https://doi.org/10.1007/s00066-016-1038-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-016-1038-0