Abstract
Purpose
The purpose of this work was to retrospectively determine the value of intensity-modulated radiotherapy (IMRT) in patients with laryngeal and hypopharyngeal squamous cell carcinoma (LHSCC), on outcome and treatment-related toxicity compared to 3-dimensional conformal radiotherapy (3D-CRT).
Materials and methods
A total of 175 consecutive patients were treated between 2007 and 2012 at our institution with curative intent RT and were included in this study: 90 were treated with 3D-CRT and 85 with IMRT. Oncologic outcomes were estimated using Kaplan–Meier statistics; acute and late toxicities were scored according to the Common Toxicity Criteria for Adverse Events scale v 3.0.
Results
Median follow-up was 35 months (range 32–42 months; 95% confidence interval 95 %). Two-year disease-free survival did not vary, regardless of the technique used (69 % for 3D-CRT vs. 72 %; for IMRT, p = 0.16). Variables evaluated as severe late toxicities were all statistically lower with IMRT compared with 3D-CRT: xerostomia (0 vs. 12 %; p < 0.0001), dysphagia (4 vs. 26 %; p < 0.0001), and feeding-tube dependency (1 vs 13 %; p = 0.0044). The rates of overall grade ≥ 3 late toxicities for the IMRT and 3D-CRT groups were 4.1 vs. 41.4 %, respectively (p < 0.0001).
Conclusion
IMRT for laryngeal and hypopharyngeal cancer minimizes late dysphagia without jeopardizing tumor control and outcome.
Zusammenfassung
Ziel
Das Ziel dieser Studie war es, retrospektiv den Nutzen der intensitätsmodulierten Strahlentherapie (IMRT) in der Behandlung von Patienten mit Plattenepithelkarzinom von Kehlkopf und Hypopharynx (LHSCC) zu bewerten und mit dem Outcome und den Spätfolgen der 3-D-konformalen Strahlentherapie (3D-CRT) zu vergleichen.
Material und Methoden
Insgesamt wurden zwischen Januar 2007 und Dezember 2012175 LHSCC-Patienten mit einer RT behandelt und in die Studie aufgenommen: 85 Patienten wurden mit 3D-CRT und 90 Patienten mit IMRT behandelt.Das onkologische Outcome wurde mittels Kaplan-Meier-Statistik ermittelt und Akut- und Spättoxizitäten anhand der CTCAE v.3 (Common Toxicity Criteria for Adverse Events v 3.0) bewertet.
Ergebnisse
In Dreiviertel der Fälle lag eine lokal fortgeschrittene Erkrankung vor. Die durchschnittliche Nachbeobachtungszeit lag bei35 Monaten (32–42 Monate, 95%-Konfidenzintervall 95 %). Unabhängig von der angewandten RT-Technik betrug das krankheitsfreie 2-Jahres-Überleben 71 % (69 % für 3D-CRT vs. 72 % für IMRT; p = 0,16). Alle bezüglich der Spättoxizität evaluierten Parameter zeigten nach IMRT signifikant günstigere Werte als nach 3D-CRT: Xerostomie (0 vs. 12 %; p < 0,0001), Dysphagie (4 vs. 26 %; p < 0,0001) und PEG-Abhängigkeit (1 vs. 13 %; p = 0,0044). Die Langzeittoxizität (Grad ≥ 3) war nach IMRT bedeutend geringer ausgeprägt als nach 3D-CRT (4,1 vs. 41,4 %; p < 0,0001).
Schlussfolgerung
Die IMRT von LHSCC führt zu einer vergleichbaren Tumorkontrolle wie 3D-CRT und verringert die Inzidenz und den Schweregrad von Spätfolgen wie Dysphagie deutlich.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Management of laryngeal and hypopharynx squamous cell carcinoma (LHSCC) represents a challenge due to the medical conditions of the patients, which frequently have a locally advanced stage disease at diagnosis plus the nearby location of critical structures (spinal cord, salivary glands, constrictors muscles). In the curative-intent setting, radiotherapy (RT) remains a cornerstone for the management of these patients, either alone or after surgery.
Recovery is achieved but has serious long-term consequences i.e., dysphagia and xerostomia [1], that lead to everyday impairment of quality of life. The incidence and impact of RT-induced late toxicity is generally evaluated in the literature from the follow-up of patients with laryngeal or hypopharyngeal cancer and that have been previously treated with conventional RT [2, 3].
In recent years, intensity-modulated RT (IMRT) has emerged as a new technique allowing a higher conforming dose distribution to the target volumes and avoidance of nearby critical structures [4]. Numerous retrospective studies and one prospective study have reported on the clinical benefits of IMRT for different sites within the head and neck [5–8]; however, the literature related to laryngeal and hypopharyngeal tumors are scanty and some questions remain unanswered. First, given its high dose gradient, the implementation of IMRT raises concerns about the potential risk of local failures at the margin of the planned-target volume (PTV) that would have been covered by a conventional RT-treatment RT field. Second, what are the real quality-of-life benefits of IMRT for patients with laryngeal or hypopharyngeal cancer?
At our institution, as in many others, the technical evolution of RT raises the possibility of implementing IMRT in routine practice for all potentially curative patients with squamous-cell carcinoma of the head and neck. The primary objective of our study was to determine the clinical benefits of IMRT compared 3D-CRT to manage laryngeal or hypopharyngeal cancer. The secondary objective was to compare the carcinological results of each technique.
Materials and methods
The medical charts from all consecutive patients (n = 240) who received radiation therapy for laryngeal or hypopharyngeal squamous-cell carcinoma at our institution, between January 2007 and December 2012, were retrospectively reviewed.
A total of 175 patients were eligible to be included in this study: 90 were treated with 3D-CRT and 85 were treated with IMRT. Patient, tumor, and treatment characteristics from the overall cohort and according to RT technique are depicted in Table 1.
Sixty-five patients were excluded for the following reasons: palliative intent RT (n = 17), salvage RT after surgical failure (n = 10), multiple synchronous tumor sites (n = 16), history of prior head-and-neck irradiation (n = 12), follow-up of < 6 months (early death, n = 6, and lost to follow-up, n = 4).
At the end of RT, dermatitis, mucositis, weight loss, and dysphagia were prospectively registered and scored using the Common Toxicity Criteria for Adverse Events (CTCAE) scale (version 3.0) by the treating physician.
Variables evaluated as late toxicities were xerostomia, dysphagia, and feeding-tube dependency retrospectively graded using the (CTCAE scale, version 3.0), at the last follow-up or before any local failure within a 6-month minimal delay after completing RT. A total of 165 patients were locally free from any active disease and were eligible for evaluation of late toxicity. Indeed, 10 patients presented with a local unresectable disease without any response to definitive chemoradiotherapy.
Pretherapeutic evaluation included the following:
-
a physical examination of the head and neck by a surgeon and radiation oncologist,
-
endoscopy under general anesthesia,
-
biopsies,
-
cervical and thoracic tomodensitometry (FDG PET was optional),
-
orthopantomogram and a dedicated dental consultation,
-
biological tests,
-
nutritional assessment by a dietitian, and
-
vocal and swallowing evaluation by a dedicated speech and swallowing therapist.
Tumors were staged according to the American Joint Committee on Cancer (AJCC; 6th and 7th edition) and each case was discussed in a multidisciplinary head-and-neck cancer board before treatment initiation.
During RT, all patients were immobilized supine using a thermoplastic 5-point mask. A contrast-enhanced computed tomography scan (CT scan) was obtained for treatment planning. All available diagnostic MRI and/or PET scans were fused to the treatment-planning CT scans.
A definitive RT was indicated in T1–T3 and unresectable T4 tumors. All patients underwent bilateral lymph-node irradiation (level II, III, IV, V, and additional VI for advanced laryngeal cancer and retropharyngeal nodes for hypopharyngeal cancer) except for glottic carcinoma. A concomitant chemotherapy was performed when there was a large tumor or nodal involvement of ≥ 3. An induction chemotherapy [Taxotere, cisplatin, 5-fluorouracil (5FU)] was performed in case of T3 tumor.
In the definitive setting, patients were prescribed a dose of 66–70 Gy in 30–35 fractions to a high-risk planned-target volume (PTV) and 54–56 Gy in 30–35 fractions to low-risk PTV. Alternatively, a laryngectomy (LT) was performed if there was a T4 tumor or after insufficient response to the induction chemotherapy. Postoperative RT was indicated in case of T4 tumor, after a suboptimal resection, a nodal involvement of ≥ 3, or extracapsular spread. In the postoperative setting, the prescription dose was 54–63 Gy in 27–30 fractions to high-risk PTV and 54 Gy in 30 fractions to low-risk PTV.
3D-CRT was delivered using parallel-opposed conformal fields for the upper part of the neck and an anterior supraclavicular field for the lower part using a (Varian®) linear accelerator. The organ at risk constraint was the spine at 44 Gy.
Since 2009, IMRT has been implemented for routine cases of laryngeal and hypopharyngeal cancer, due to availability constraints, priority was given to patients receiving definitive (chemo)radiotherapy for large disease, then starting from 2011 all patients underwent IMRT. The technique used was the step-and-shoot technique until May 2011 and Arc therapy using Varian® RapidArc afterwards. Simultaneously, some patients were treated with helical RT delivered by Tomotherapy® starting from 2010. IMRT dose was delivered using a simultaneous integrated boost technique [9]. For the 85 IMRT treatments, the parotid glands were delineated on the original planning CT scan. Starting from 2011, superior and middle pharyngeal constrictor muscles (SPCM) were also delineated when appropriate. The planned treatment was elaborated using the following constraints to the corresponding organs at risk: mean dose to the parotids, submandibular gland, and the SPCM were < 26, 40, and 45 Gy, respectively. The maximal dose to jaw, spine, and brainstem were 70, 45, and 55 Gy, respectively.
During RT, all patients underwent a close weekly medical follow-up by a member of the Radiation Oncology Department, a dedicated dentist, a speech and swallowing therapist, and a dietitian.
The follow-up consisted of three-monthly physical examinations, which included a direct fiberoptic nasopharyngeal–laryngoscopy by a radiation oncologist or a head-and-neck surgeon. Contrast-enhanced CT scan evaluation of the neck was performed at 3 months after RT or if failure was suspected.
All patients were followed by a dedicated dentist and a speech and swallowing therapist twice a year for the first year after RT completion and annually thereafter. Salivary and swallowing functions were closely monitored during the follow-up, and were classed as “normal” function, “moderate”, or “severe impairment”: they were retrospectively scored according to the CTCAE scale (version 3.0) at the last follow-up or before any local failure within a 6-month minimal delay after completing RT. Severe late toxicities were defined as grade 3 or higher, i.e., dysphagia, xerostomia, or feeding-tube dependency.
For patients with a locoregional failure, the recurrent tumor volume, identified at the time of recurrence, was compared and fused to treatment planning CT-scan, focusing on the 95 % isodose lines. Failures were categorized according to previously irradiated targets, defined as “in field” if > 95 % of the failure volume was within the 95 % isodose, as “marginal” if 20–95 % of the failure volume was within the 95 % isodose, or as “outside” if < 20 % of the failure volume was inside the 95 % isodose [10].
Data were summarized according to frequencies and percentages for categorical variables and by medians (and ranges) for continuous variables. The differences between groups were assessed using the χ2 or Fisher’s exact test for qualitative variables, and the Mann–Whitney test for continuous variables.
Survival times were calculated from the date of diagnosis and estimated by the Kaplan–Meier method, using the following first-event definitions: locoregional, distant metastasis, and death for disease-free survival (DFS), and death from any cause for overall survival (OS).
DFS was measured as the time from diagnosis until the first event using the following definitions: locoregional, distant metastasis, and death. Patients alive without a relapse at the time of analysis were censored at their last follow-up. Survival rates were estimated according to the Kaplan–Meier method. Univariate analyses using log-rank tests were performed to identify prognostic factors associated with DFS. All factors considered significant in the univariate analyses were included in Cox’s multivariate analysis.
All p-values were two-sided. For all statistical tests, differences were considered significant at the 0.05 level. Statistical analyses were performed using STATA 12.0 software.
Results
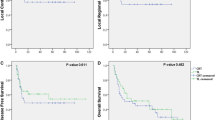
Overall cohort follow-up
The median time of follow-up of patients from the overall cohort was 35 months (95 % confidence interval [CI] 32–42 months). The 3-year overall survival rate was 71 %. Among the 50 deaths that occurred, 34 were due to progression of laryngeal or hypopharyngeal cancer. The 2-year DFS rate was 70 % (Fig. 1). Thirty-eight patients presented with a local and/or regional failure during the follow-up: among these, 10 were associated with synchronous metastatic progression. In all, 20 patients presented with a distant failure. The strongest prognostic factors for 2-year DFS were ECOG performance status (0 versus ≥ 1; p = 0.0003), primary location (larynx vs. hypopharynx, p = 0.018), tumor stage (T1–2 vs. T3–4; p = 0.04), nodal extension (N0 versus N ≥ 1; p = 0.0018), and overall stage (I–II vs. III–IV; p = 0.0007). In the multivariate analyses, ECOG performance status and overall stage remained the only predictors for DFS.
Univariate and multivariate analyses of prognostic factors for DFS are depicted in Table 2.
Comparison of techniques: IMRT vs. 3D-CRT
The two groups were comparable in terms of age, primary location, ECOG performance status, medical condition at diagnosis, and treatment modalities, i.e., induction chemotherapy, surgery, and mean delivered RT dose.
The main differences between the two groups were a significantly greater number of male patients (92 vs. 80 %; p = 0.02), nodal extension at diagnosis, (62 vs. 47 %; p = 0.04), a concomitant CT (58 vs. 46 %; p = 0.01) for IMRT patients, and a shorter follow-up time: 22 vs. 49 months, respectively (Table 1). For IMRT patients, mean doses delivered to the ipsilateral and contralateral parotid were 25 and 21 Gy, respectively. Mean dose delivered to the SPCM was 39 Gy (n = 28; range 1–55 Gy).
There was no difference in 3-year OS rates according to RT technique: IMRT vs 3D-CRT: 69 vs. 74 %; p = 0.25. The DFS did not statistically vary between the two techniques: 69 % for 3D-CRT vs. 72 %; for IMRT p = 0.16 (Fig. 1). Patients with a locoregional failure (n = 38) harbored comparable rates of in-field, margin-field, and out-of-field failures, irrespective of the technique used (IMRT or 3D-CRT: 90, 5, and 5 % vs. 84, 5, and 11 %, respectively). There was a trend towards less grade ≥ 3 acute dermatitis, mucositis, dysphagia, and weight loss in the IMRT group, but the differences were not significant. The detailed results are presented in Fig. 2. The incidence and severity of each variable was significantly increased by chemotherapy (neo-adjuvant or concomitant), i.e., overall acute grade ≥ 3 toxicities: 85 vs. 47 %; (p < 0.0001) regardless of the RT technique.
Regarding late grade ≥ 3 xerostomia, dysphagia, and feeding-tube dependency were significantly lower with IMRT compared to 3D-CRT: 0 vs. 12 % (p < 0.0001), 4 vs. 26 % (p < 0.0001) and 1 vs. 13 % (p = 0.0044), respectively. The results are displayed in Fig. 3. The rates of overall grade ≥ 3 toxicities, according to the Common Toxicity Criteria for Adverse Events scale v3.0 among the IMRT and 3D-CRT groups were 4.1 vs. 41.4 %, respectively (p < 0.0001).
Discussion
Given its high dose gradient, IMRT raises concerns about the potential risk of local failures at the margin of the planned-target volume (PTV) that would have been covered by a conventional RT-treatment field. Second, the real quality-of-life benefits of IMRT for patients has been documented only in one randomized study in general HNSCC but no comparison of clinical outcome was possible due to the sample size and short follow-up [11]. Moreover, very few dedicated studies were published for hypopharyngeal and laryngeal cancers. As the benefit on toxicity given by IMRT is now widely recognized, ethical concerns prevent from driving prospective trials comparing both techniques. Therefore, the information provided by restrospective single institution analysis remains mandatory in the evaluation on clinical benefits and tumor control.
As this study is retrospective, results must be analyzed with caution. However, both populations were treated in a 5-year time span with similar diagnostic and treatment procedures, i.e., surgical techniques, planned target volumes, chemotherapy regimens. The only difference remained in the radiotherapy technique. The retrospective nature of the grading of late toxicity is somewhat compensated by the practitioners stability, the good dedicated follow-up of patients, and the frequency of consultations during these years.
This study compared the carcinological results and toxicity profiles for a large cohort of patients with laryngeal or hypopharyngeal cancer, treated in recent years with 3D-CRT or IMRT at a single institution and described similar outcome with less toxicity.
The present study did not find any significant differences between the two RT techniques in terms of LRC or DFS, despite a clear selection bias within the IMRT group, which was initially reserved for patients with larger targeted volumes: this suggests that the reduction of total irradiated volume did not compromise tumor control. The noninferiority of IMRT on tumor control was published in several studies on HNSCC [12–14] but few were dedicated to larynx and hypopharynx. Several retrospective series dedicated to outcome after laryngeal or hypopharyngeal IMRT have shown good locoregional control, which compares favorably with historical results [15–18], but the number of patients studied was inferior to the large number of patients described in our study.
In a recent study, Al Mamgani et al. [17] highlighted significantly lower acute grade-3 skin and mucositis toxicity in a IMRT group compared to a CRT group: 42 vs. 63 %, and 39 vs. 56 %, respectively, among hypopharyngeal patients. In our study, the trend towards lower acute skin and mucositis toxicities in the IMRT group remained insignificant, probably because of a higher rate of nodal extension at diagnosis in the IMRT group, which led to enlargement of target volumes and the increased use of concurrent chemotherapy.
Regarding late toxicities, the incidence and severity of xerostomia, dysphagia, and feeding-tube dependency were all significantly lower in the IMRT group compared to the 3D-CRT group, and the overall grade 3 late toxicities were 4.1 vs. 41.4 % respectively (p < 0.0001). More recently, several studies have been published with the aim of determining underlying clinical and dosimetric parameters important for dysphagia [19–22], to our knowledge, none has been dedicated exclusively to laryngeal or hypopharyngeal cancer patients. Our results are in accordance with Mortensen et al. [23] where a major favorable impact of IMRT was found with dysphagia, which resulted in the preservation of saliva as well as a significant dose reduction to dysphagia-related structures, i.e., the upper larynx and SCPM.
Xerostomia is one of the most severe and frequent late toxicities after head-and-neck RT and is responsible for gustatory dysfunction and dental complications. Salivary function relies on the parotid, submandibular, and accessory glands. Due to a frequent advanced stage at diagnosis and a median situation, patients with hypopharyngeal and laryngeal cancer often require bilateral cervical lymph-node RT, which enhances the risk of late xerostomia [24]. The dosimetric advantages of IMRT represent a means to prevent RT-induced xerostomia [11]. In our study, the rates of grade 0 and 3 xerostomia for IMRT and 3D-CRT patients were 67 and 0 % vs. 39 and 12 %, respectively (p < 0.0001).
Swallowing function relies on several structures that enable salivation, muscle contraction, and upper respiratory tract protection. Indeed, xerostomia, pharyngeal stricture, and laryngeal dysfunction contribute to dysphagia. Lee et al. [25] reported up to 21 % of pharyngeal strictures among patients with locally advanced hypopharyngeal cancer and treated with 3D-CRT. Haderlein et al. [26] suggested a role of dose to SPCM for late dysphagia after 3DRT for laryngeal and hypopharyngeal cancer. It has been previously demonstrated that each 10 Gy, up to 55 Gy, given to SPCM increases the risk of late dysphagia by 19 % [27]. Eisbruch et al. [20] described, in a prospective study, that the dose delivered to the SPCM and the larynx was correlated with dysphagia. One of the concerns with RT-induced dysphagia are the inconsistencies between the different methods of measurement [28]. It can be objectively measured by feeding-tube dependency. Indeed, in our study, the rates of feeding-tube dependency were significantly higher among 3D-CRT patients when compared to IMRT patients: 13 and 1 %, respectively (p = 0.0044).
At our institution, all patients with radiocurable laryngeal or hypopharyngeal SCC benefit from this technique in order to decrease the occurrence of toxicities in such a fragile population.
Conclusion
The present study shows in a large series of patients that the introduction of IMRT for laryngeal and hypopharyngeal cancer significantly minimizes late dysphagia when compared to 3D-CRT without jeopardizing tumor control and patient outcome.
References
Langendijk JA, Doornaert P, Verdonck-de Leeuw IM, Leemans CR, Aaronson NK, Slotman BJ (2008) Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncol 26:3770–3776
Forastiere AA, Zhang Q, Weber RS, Maor MH, Goepfert H, Pajak TF, Morrison W, Glisson B, Trotti A, Ridge JA et al (2013) Long-term results of RTOG 91-11: a comparison of three nonsurgical treatment strategies to preserve the larynx in patients with locally advanced larynx cancer. J Clin Oncol 31:845–852
Blanchard P, Tao Y, Veresezan O, Lusinchi A, Le Ridant AM, Janot F, Daly-Schveitzer N, Bourhis J (2012) Definitive radiotherapy for squamous cell carcinoma of the pyriform sinus. Radiother Oncol 105:232–237
Brahme A (1988) Optimization of stationary and moving beam radiation therapy techniques. Radiother Oncol 12:129–140
Gupta T, Agarwal J, Jain S, Phurailatpam R, Kannan S, Ghosh-Laskar S, Murthy V, Budrukkar A, Dinshaw K, Prabhash K et al (2012) Three-dimensional conformal radiotherapy (3D-CRT) versus intensity modulated radiation therapy (IMRT) in squamous cell carcinoma of the head and neck: a randomized controlled trial. Radiother Oncol 104:343–348
Ng WT, Lee MC, Hung WM, Choi CW, Lee KC, Chan OS, Lee AW (2011) Clinical outcomes and patterns of failure after intensity-modulated radiotherapy for nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 79:420–428
Daly ME, Le QT, Maxim PG, Loo BW, Jr, Kaplan MJ, Fischbein NJ, Pinto H, Chang DT (2010) Intensity-modulated radiotherapy in the treatment of oropharyngeal cancer: clinical outcomes and patterns of failure. Int J Radiat Oncol Biol Phys 76:1339–1346
Chen AM, Farwell DG, Luu Q, Vazquez EG, Lau DH, Purdy JA (2012) Intensity-modulated radiotherapy is associated with improved global quality of life among long-term survivors of head-and-neck cancer. Int J Radiat Oncol Biol Phys 84:170–175
Butler EB, Teh BS, Grant WH, 3rd, Uhl BM, Kuppersmith RB, Chiu JK, Donovan DT, Woo SY (1999) Smart (simultaneous modulated accelerated radiation therapy) boost: a new accelerated fractionation schedule for the treatment of head and neck cancer with intensity modulated radiotherapy. Int J Radiat Oncol Biol Phys 45:21–32
Chao KS, Ozyigit G, Tran BN, Cengiz M, Dempsey JF, Low DA (2003) Patterns of failure in patients receiving definitive and postoperative IMRT for head-and-neck cancer. Int J Radiat Oncol Biol Phys 55:312–321
Nutting CM, Morden JP, Harrington KJ, Urbano TG, Bhide SA, Clark C, Miles EA, Miah AB, Newbold K, Tanay M et al (2011) Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): a phase 3 multicentre randomised controlled trial. Lancet Oncol 12:127–136
Vergeer MR, Doornaert PA, Rietveld DH, Leemans CR, Slotman BJ, Langendijk JA (2009) Intensity-modulated radiotherapy reduces radiation-induced morbidity and improves health-related quality of life: results of a nonrandomized prospective study using a standardized follow-up program. Int J Radiat Oncol Biol Phys 74:1–8
Toledano I, Graff P, Serre A, Boisselier P, Bensadoun RJ, Ortholan C, Pommier P, Racadot S, Calais G, Alfonsi M et al (2012) Intensity-modulated radiotherapy in head and neck cancer: results of the prospective study GORTEC 2004-03. Radiother Oncol 103:57–62
Lambrecht M, Nevens D, Nuyts S (2013) Intensity-modulated radiotherapy vs. parotid-sparing 3D conformal radiotherapy. Effect on outcome and toxicity in locally advanced head and neck cancer. Strahlenther Onkol 189:223–229
Daly ME, Le QT, Jain AK, Maxim PG, Hsu A, Loo BW, Jr, Kaplan MJ, Fischbein NJ, Colevas AD, Pinto H et al (2011) Intensity-modulated radiotherapy for locally advanced cancers of the larynx and hypopharynx. Head Neck 33:103–111
Studer G, Lutolf UM, Davis JB, Glanzmann C (2006) IMRT in hypopharyngeal tumors. Strahlenther Onkol 182:331–335
Al-Mamgani A, Mehilal R, van Rooij PH, Tans L, Sewnaik A, Levendag PC (2012) Toxicity, quality of life, and functional outcomes of 176 hypopharyngeal cancer patients treated by (chemo)radiation: the impact of treatment modality and radiation technique. Laryngoscope 122:1789–1795
Lee NY, O’Meara W, Chan K, Della-Bianca C, Mechalakos JG, Zhung J, Wolden SL, Narayana A, Kraus D, Shah JP et al (2007) Concurrent chemotherapy and intensity-modulated radiotherapy for locoregionally advanced laryngeal and hypopharyngeal cancers. Int J Radiat Oncol Biol Phys 69:459–468
Feng FY, Kim HM, Lyden TH, Haxer MJ, Feng M, Worden FP, Chepeha DB, Eisbruch A (2007) Intensity-modulated radiotherapy of head and neck cancer aiming to reduce dysphagia: early dose-effect relationships for the swallowing structures. Int J Radiat Oncol Biol Phys 68:1289–1298
Eisbruch A, Kim HM, Feng FY, Lyden TH, Haxer MJ, Feng M, Worden FP, Bradford CR, Prince ME, Moyer JS et al (2011) Chemo-IMRT of oropharyngeal cancer aiming to reduce dysphagia: swallowing organs late complication probabilities and dosimetric correlates. Int J Radiat Oncol Biol Phys 81:e93–99
Caglar HB, Tishler RB, Othus M, Burke E, Li Y, Goguen L, Wirth LJ, Haddad RI, Norris CM, Court LE et al (2008) Dose to larynx predicts for swallowing complications after intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys 72:1110–1118
Dirix P, Abbeel S, Vanstraelen B, Hermans R, Nuyts S (2009) Dysphagia after chemoradiotherapy for head-and-neck squamous cell carcinoma: dose-effect relationships for the swallowing structures. Int J Radiat Oncol Biol Phys 75:385–392
Mortensen HR, Jensen K, Aksglaede K, Behrens M, Grau C (2013) Late dysphagia after IMRT for head and neck cancer and correlation with dose-volume parameters. Radiother Oncol 107:288–294
Astreinidou E, Dehnad H, Terhaard CH, Raaijmakers CP (2004) Level II lymph nodes and radiation-induced xerostomia. Int J Radiat Oncol Biol Phys 58:124–131
Lee WT, Akst LM, Adelstein DJ, Saxton JP, Wood BG, Strome M, Butler RS, Esclamado RM (2006) Risk factors for hypopharyngeal/upper esophageal stricture formation after concurrent chemoradiation. Head Neck 28:808–812
Haderlein M, Semrau S, Ott O, Speer S, Bohr C, Fietkau R (2014) Dose-dependent deterioration of swallowing function after induction chemotherapy and definitive chemoradiotherapy for laryngopharyngeal cancer. Strahlenther Onkol 190:192–198
Levendag PC, Teguh DN, Voet P, van der Est H, Noever I, de Kruijf WJ, Kolkman-Deurloo IK, Prevost JB, Poll J, Schmitz PI et al (2007) Dysphagia disorders in patients with cancer of the oropharynx are significantly affected by the radiation therapy dose to the superior and middle constrictor muscle: a dose-effect relationship. Radiother Oncol 85:64–73
Jensen K (2007) Measuring side effects after radiotherapy for pharynx cancer. Acta Oncol 46:1051–1063
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Acknowledgments
The authors would like to thank Newmed publishing for English editing and Ursula Nestle for German editing.
Conflict of interest
A. Modesto, A. Laprie, L. Vieillevigne, P. Graff, J. Sarini, S. Vergez, J.-P. Delord, J.-C. Farenc, E. Vigarios, T. Filleron, and M. Rives state that there are no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Rights and permissions
About this article
Cite this article
Modesto, A., Laprie, A., Vieillevigne, L. et al. Intensity-modulated radiotherapy for laryngeal and hypopharyngeal cancer. Strahlenther Onkol 191, 225–233 (2015). https://doi.org/10.1007/s00066-014-0767-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-014-0767-1
Keywords
- Squamous cell carcinoma of the head and neck
- Larynx
- Hypopharynx
- Intensity-modulated radiotherapy
- Deglutition disorders