Abstract
Background
Pooled data of randomized controlled trials investigating mechanical thrombectomy (MT) to treat anterior circulation large vessel occlusion have demonstrated safety and effectiveness across all age groups, including ≥ 80 years of age; however, only a few nonagenarians were in the ≥ 80 years subgroup. Therefore, the benefit of MT in nonagenarians is mostly unknown.
Methods
Two comprehensive stroke centers retrospectively reviewed all acute ischemic stroke patients who underwent MT for anterior circulation large vessel occlusion (LVO) stroke between February 2016 and August 2020. Revascularization TICI2b/3, symptomatic intracranial hemorrhage (ICH), and functional outcome using modified Rankin scale (mRS) were assessed for cases aged < 80 years, 80–89 years, and 90–99 years. Favorable functional outcome was defined as mRS 0–2 or reaching the prestroke mRS and moderate as mRS 0–3.
Results
The final data set comprised a total of 736 cases. Of these, 466 aged < 80 years, 219 aged 80–89 years, and 51 aged 90–99 years. In nonagenarians, TICI 2b/3 revascularization was observed in 84.3% while symptomatic ICH was observed in 4%. These rates were similar to 80–89 years and < 80 years age groups. Favorable and moderate functional outcome as well as death rates differed significantly between nonagenarians and < 80 years (19.6%, 29.4%, 51.0% vs 47.9%, 60.7%, 18.7%, respectively, p < 0.001), but were similar between nonagenarians and octogenarians (29.7%, 38.8%, 38.8%, p = 0.112–0.211).
Conclusion
A moderate outcome among nonagenarians was observed in about 30%, while mortality rates were about 50%. Withholding mechanical thrombectomy does not appear justifiable, although the absolute treatment effect among nonagenarians remains unknown.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pooled data of randomized controlled trials (RCTs) investigating mechanical thrombectomy to treat anterior circulation large vessel occlusion (LVO) has demonstrated efficacy across all age groups [1]. Current guidelines provide class I recommendation for mechanical thrombectomy in patients aged 80 years or older [2]; however, since some of the RCTs excluded patients older than 80 years [3, 4] or 85 years [5], the role of mechanical thrombectomy in nonagenarians is essentially unknown [2]. To date, a few case series in nonagenarians and comparative analyses of nonagenarians to younger subgroups exist. There is heterogeneity in study periods, with only few recent publications studying cohorts beginning in or after 2015. Recently, Bai et al. systematically reviewed mechanical thrombectomy in nonagenarians and identified 13 observational studies. The authors reported successful revascularization in about 81% of patients, a modified Rankin scale (mRS) 0–2 in about 22%, an mRS 0–3 in about 23%, and a 90-day mortality rate of about 44%; however, standardized functional as well as safety outcomes were inconsistently reported and therefore calculated only from a subset of these studies. Furthermore, sample sizes of the studies varied considerably [6]. Due to scarcity of standardized safety and outcome data of patients aged 90–99 years undergoing mechanical thrombectomy for LVO stroke, we sought to evaluate these in nonagenarians, and compared outcomes to octogenarians and patients aged < 80 years.
Methods
Consecutive patients who underwent mechanical thrombectomy for anterior circulation LVO at two comprehensive stroke centers between February 2016 and August 2020 were retrospectively reviewed. Each center obtained approval from the IRB. Following exclusion of patients with missing data and patients treated for posterior circulation large vessel occlusion, patients were grouped according to age at index into age < 80 years, 80–89 years (octogenarians), and age 90–99 years (nonagenarians). Age subgroup analysis was performed for nonagenarians compared to octogenarians. Functional outcome was assessed utilizing the modified Rankin scale (mRS) 90 days after index. To account for overall morbidity among nonagenarians, the achievement of mRS of 0–2 or achieving pre-stroke mRS was defined as a favorable functional outcome, whereas mRS 0–3 or achieving pre-stroke mRS were defined as a moderate functional outcome. Symptomatic intracranial hemorrhage (sICH) was evaluated on 24–48 h postthrombectomy computed tomography (CT) or magnetic resonance imaging (MRI) and classified according to ECASS and the Heidelberg bleeding classification. A new ICH on CT or MRI (i) associated with a total NIHSS deterioration of ≥ 4 or NIHSS subcategory deterioration ≥ 2; and/or (ii) demanding intubation and/or surgical intervention, such as hemicraniectomy, hematoma removal or external ventricular drain placement in absence of alternative events for deterioration were considered sICH [7].
Statistical Analysis
Mann-Whitney‑U, Kruskal-Wallis, χ2 and Fisher’s exact tests were performed, as appropriate, to compare variables between groups. Stepwise backward elimination multivariable analysis was performed to assess independent predictors of functional outcome. P-values of < 0.05 were considered statistically significant. IBM SPSS version 25 (Chicago, IL, USA) and GraphPad Prism 9 (San Diego, CA, USA) were used for data analysis and presentation.
Results
Collectively, 828 mechanical thrombectomies were identified in the study period. Posterior circulation large vessel occlusion stroke (n = 77) and cases with missing premorbid mRS or 90-day mRS data sets (n = 15) were excluded. The final data set comprised a total of 736 cases. Of these, 466 aged < 80 years, 219 aged 80–89 years, and 51 aged 90–99 years (Table 1).
Baseline Characteristics
Distinct baseline characteristics such as sex, risk factors, and premorbid mRS differed significantly across all three age groups (Table 1). Comparing nonagenarians to octogenarians, the proportion of females was significantly higher among nonagenarians, whereas the proportion of coexisting type 2 diabetes and atrial fibrillation was significantly lower. The remaining baseline characteristics were equal between nonagenarians and octogenarians (Fig. 1).
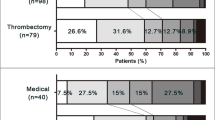
Baseline and outcome parameter among aged < 80 years, 80–89 years, and 90–99 years. b‑NIHSS baseline NIHSS, atrial fib atrial fibrillation, TTI time to intervention since symptom onset. Data missing in 64 patients beyond the 6‑h time window; mRS 0–3# refers to moderate outcome in reaching mRS 0–3 or pre-stroke mRS
Outcome Parameter
The Thrombolysis in Cerebral Infarction (TICI) 2b/3 revascularization rates were similar among all age groups. Symptomatic intracranial hemorrhage rates were also equal among age groups. A favorable functional outcome was observed in 19.6% of nonagenarians, 29.7% of octogenarians and 47.9% in age < 80 years (p < 0.001). A moderate functional outcome was observed in 29.4% of nonagenarians, 38.8% of octogenarians and 60.7% in age < 80 years (p < 0.001). Death was observed in 51.0% of nonagenarians, 38.8% of octogenarians and 18.7% in age < 80 years (p < 0.001). Comparing nonagenarians and octogenarians, a favorable and moderate functional outcome as well as death rates differed significantly between nonagenarians and < 80 years (19.6%, 29.4%, 51.0% vs. 47.9%, 60.7%, 18.7%, respectively, p < 0.001), but were similar between nonagenarians and octogenarians (29.7%, 38.8%, 38.8%, p = 0.112–0.211). (Table 2, Fig. 1 and 2).
Discussion
The current literature lacks standardized outcome data in patients in the ninth decade of life undergoing mechanical thrombectomy for acute large vessel occlusion ischemic stroke [6]. This retrospective two-center cohort study highlights that patient age, including the ninth decade, is not associated with the risk of symptomatic intracranial hemorrhage. A TICI 2b/3 revascularization was equally achieved across all age groups; however, patient age ≥ 80 years is associated with poorer functional outcomes compared to patient age < 80 years with a risk difference for a favorable functional outcome, moderate functional outcome, and death of about 20%. Although not statistically significant, nonagenarians compared to octogenarians experienced a further detrimental risk difference of about 10% for a favorable functional outcome, moderate functional outcome, or death.
Observations by Alawieh et al. were in the scope of our findings. They compared patients aged 60–79 years to patients aged ≥ 80 years (including a subset of nonagenarians) and found an about 24% difference in favorable functional outcomes (mRS 0–2) and 14% difference in death. A TICI2b/3 revascularization and intracranial hemorrhage rates were equal [8] A meta-analysis by Duffis et al. portrayed octogenarians as less likely to achieve functional independence and have an increased risk of mortality. Additionally, they observed higher rates of intracerebral hemorrhage [9]. The discrepancy regarding the intracerebral hemorrhage rates compared to our findings might partially be explained by the utilization of new generation devices in our post-2015 cohorts and the strict inclusion of patients with favorable ASPECTS among octogenarians and specifically nonagenarians (compare Fig. 1). While only including patients with pre-stroke mRS < 3, Meyer et al. did not find an increased risk for sICH in nonagenarians in a 3-center analysis. A 90-day mortality rate of about 47% is in line with our observations [10]. In a subsequent registry analysis, these outcome rates were substantiated. Among 203 nonagenarians, an mRS of 0–3 was independently predicted by lower baseline NIHSS and higher ASPECTS [11]. In our study cohort, nonagenarians had a high TICI 2b/3 revascularization rate, almost uniform ASPECT scores ≥ 6 (98.0%) and a low sICH rate. Still, every second patient died within 90 days, and about 30% achieved independent walking or baseline (pre-stroke) function. These comparably poor outcome rates among older people have to be appreciated. At the same time, they do not appear to justify withholding mechanical thrombectomy since almost every third patient can achieve a moderate functional outcome in terms of independent walking or reaching pre-stroke mRS. Since no randomized controlled data are available for a standard medical treatment group, the absolute treatment effect of mechanical thrombectomy for LVO stroke among nonagenarians remains unknown.
Limitations
The study is primarily limited by its retrospective character. Notably, patient selection, specifically among the old, is highly biased by the center and treating physician. Females being overrepresented in nonagenarians (82.4% in the present study) treated with mechanical thrombectomy has also been observed by others and is likely attributed to different life expectancies [10, 11]. Frailty and coexisting comorbidities causing higher pre-stroke baseline mRS represent a significant driver of individual patient selection. Also, baseline imaging likely substantially influences decision making in this age group, which is also represented by our observation that 50/51 (98.0%) nonagenarians treated with mechanical thrombectomy had an ASPECTS ≥ 6. Although the proportion of benign ASPECTS was relatively high among nonagenarians, outcomes were still unsatisfactory, reflecting that a more liberal selection of patients in the ninth decade of life might result in even poorer outcomes. This study could not explore the value of advanced imaging to guide patient selection. Further exploration of in-hospital fatality and post-discharge (time from discharge to case fatality) is required. In this context, the role of the clinical course quantified by 24 h NIHSS, discharge NIHSS, as well as primary presentation to a comprehensive stroke center compared to a primary stroke center require elucidation.
Conclusion
A moderate functional outcome (mRS 0–3) among nonagenarians undergoing mechanical thrombectomy for LVO stroke was observed in about 30%, while mortality rates were as high as 50%. Nevertheless, withholding mechanical thrombectomy does not appear justifiable since absolute treatment effects among nonagenarians remain unknown.
References
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al.; HERMES collaborators. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–31.
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2019;50:e344–418. Erratum in: Stroke. 2019;50:e440–1.
Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, Guillemin F; THRACE investigators. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016;15:1138–47. Erratum in: Lancet Neurol. 2016;15:1203.
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, Albers GW, et al.; SWIFT PRIME Investigators. Stent-retriever thrombectomy after intravenous t‑PA vs. t‑PA alone in stroke. N Engl J Med. 2015;372:2285–95.
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al.; REVASCAT Trial Investigators. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372:2296–306.
Bai X, Zhang X, Zhang Y, Yang W, Wang T, Feng Y, et al. Mechanical Thrombectomy in Nonagenarians: a Systematic Review and Meta-analysis. Transl Stroke Res. 2021;12:394–405.
von Kummer R, Broderick JP, Campbell BC, Demchuk A, Goyal M, Hill MD, et al. The Heidelberg Bleeding Classification: Classification of Bleeding Events After Ischemic Stroke and Reperfusion Therapy. Stroke. 2015;46:2981–6.
Alawieh A, Chatterjee A, Feng W, Porto G, Vargas J, Kellogg R, et al. Thrombectomy for acute ischemic stroke in the elderly: a “real world” experience. J Neurointerv Surg. 2018;10:1209–17.
Duffis EJ, He W, Prestigiacomo CJ, Gandhi CD. Endovascular treatment for acute ischemic stroke in octogenarians compared with younger patients: a meta-analysis. Int J Stroke. 2014;9:308–12.
Meyer L, Alexandrou M, Leischner H, Flottmann F, Deb-Chatterji M, Abdullayev N, et al. Mechanical thrombectomy in nonagenarians with acute ischemic stroke. J Neurointerv Surg. 2019;11:1091–4.
Meyer L, Alexandrou M, Flottmann F, Deb-Chatterji M, Abdullayev N, Maus V, et al. German Stroke Registry–Endovascular Treatment (GSR‐ET) †. Endovascular Treatment of Very Elderly Patients Aged ≥ 90 With Acute Ischemic Stroke. J Am Heart Assoc. 2020;9:e014447.
Funding
PH received salary support from Geisinger and Medtronic. There are no conflicts of interests related to this work.
Author information
Authors and Affiliations
Contributions
Conception and design: PH, CJG, acquisition of data: PH, MKO, EB, IM, VS, SM, SP, MC, NL, CH, CJG, analysis and interpretation of data: PH, CJG, drafting the article: PH, CJG, critically revising the article: all authors, reviewed submitted version of manuscript: all authors, approved the final version of the manuscript on behalf of all authors: CG, administrative/technical/material support: MKO, CMS, ET, CJG, study supervision: CJG
Corresponding author
Ethics declarations
Conflict of interest
P. Hendrix, M. Killer-Oberpfalzer, E. Broussalis, I. Melamed, V. Sharma, S. Mutzenbach, S. Pikija, M. Collins, N. Lieberman, C. Hecker, O. Goren, R. Zand, C.M. Schirmer, E. Trinka, and C.J. Griessenauer declare that they have no competing interests. The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article. C.J. Griessenauer has acted as consultant to Stryker and Microvention and received research funding from Medtronic and Penumbra. E. Trinka reports personal fees from EVER Pharma, Marinus, Argenix, Arvelle, Medtronic, Bial-Portela & Cª, S.A., NewBridge, GL Pharma, GlaxoSmithKline, Hikma, Boehringer Ingelheim, LivaNova, Eisai, UCB, Biogen, Genzyme Sanofi, GW Pharmaceuticals, and Actavis outside the submitted work; his institution received grants from Biogen, UCB Pharma, Eisai, Red Bull, Merck, Bayer, the European Union, FWF Osterreichischer Fond zur Wissenschaftsforderung, Bundesministerium für Wissenschaft und Forschung, and Jubilaumsfond der Österreichischen Nationalbank outside the submitted work.
Ethical standards
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Ethics approval: IRB approval for this retrospective analysis was obtained. Consent to participate: waived for retrospective analysis.
Additional information
Availability of Data and Material
Any data sharing requires the execution of a data sharing agreement between the requestor and Geisinger. For such requests, research contracts at Geisinger and Geisinger’s Institutional Review Board have to be contacted. Please direct requests to irb@geisinger.edu. Once appropriate data use agreements are executed, others will be able to access the data in the same manner. There are no special privileges others will not be able to get access to after appropriate data use agreements are executed.
Rights and permissions
About this article
Cite this article
Hendrix, P., Killer-Oberpfalzer, M., Broussalis, E. et al. Outcome Following Mechanical Thrombectomy for Anterior Circulation Large Vessel Occlusion Stroke in the Elderly. Clin Neuroradiol 32, 369–374 (2022). https://doi.org/10.1007/s00062-021-01063-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-021-01063-9