Abstract
Background
The incidence of supraventricular arrhythmia (SVA) is high in patients with mitral valve prolapse (MVP). The purpose of our study was to determine the role of parameters showing atrial conduction heterogeneity such as P‑wave dispersion (PWD) and atrial electromechanical delay (AEMD) in predicting the development of SVA in MVP patients.
Methods
A total of 76 patients with MVP (56 female, 20 male) were included in the study. The patients were divided into two groups according to the presence or absence of SVA: 36 patients were allocated to the non-SVA group and 40 patients to the SVA group. Heart rate variability (HRV), PWD, and AEMD values were determined and compared.
Results
The PWD was found to be higher in the SVA group. Interatrial EMD was 32.00 ms (25.00–35.00) in patients with SVA while it was 18.00 ms in patients without SVA (11.00–23.75); the intra-atrial EMD was 17.0 ms (10.00–20.00) in patients with SVA whereas it was 10.00 ms (4.00–14.00) in patients without SVA. Lower HRV was found in the SVA group.
Conclusion
In the SVA group, PWD and AEMD were increased while HRV values were decreased. Noninvasive parameters may help predict the presence and incidence of SVA during the follow-up of this group of patients.
Zusammenfassung
Hintergrund
Die Inzidenz supraventrikulärer Arrhythmien (SVA) ist bei Patienten mit Mitralklappenprolaps (MVP) hoch. Ziel der vorliegenden Arbeit war es, für die Vorhersage der Entwicklung von SVA bei MVP-Patienten die Bedeutung von Parametern zu ermitteln, welche den Nachweis einer Heterogenität der Vorhofüberleitung liefern, z. B. die P‑Wellen-Dispersion (PWD) und die atriale elektromechanische Verzögerung (AEMD).
Methoden
Dazu wurden 76 Patienten mit MVP (56 Frauen, 20 Männer) in die Studie einbezogen. Die Patienten wurden – je nach Vorliegen von SVA oder nicht – in 2 Gruppen unterteilt: Der Non-SVA-Gruppe wurden 36 Patienten zugewiesen und der SVA-Gruppe 40 Patienten. Herzfrequenzvariabilität (HRV), PWD und AEMD-Werte wurden ermittelt und verglichen.
Ergebnisse
In der SVA-Gruppe erwies sich die PWD als höher denn in der Vergleichsgruppe. Die interatriale EMD betrug 32,00 ms (25,00–35,00) bei Patienten mit SVA, während sie 18,00 ms bei Patienten ohne SVA betrug (11,00–23,75); die intraatriale EMD lag bei 17,0 ms (10,00–20,00) bei Patienten mit SVA, dagegen bei 10,00 ms (4,00–14,00) für Patienten ohne SVA. In der SVA-Gruppe wurde eine niedrigere HRV festgestellt.
Schlussfolgerung
In der SVA-Gruppe waren PWD und AEMD erhöht, während die HRV-Werte niedriger waren. Noninvasive Parameter können möglicherweise zur Vorhersage des Vorliegens und der Inzidenz von SVA im Rahmen der Nachuntersuchung bei dieser Patientengruppe beitragen.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Mitral valve prolapse (MVP) is one of the most common valvular abnormalities with an incidence in the general population of approximately 2–6% [1, 2]. Cardiac tachyarrhythmia is common among MVP patients. Supraventricular arrhythmias such as frequent supraventricular extrasystoles (SVEs, an atrial early beat frequency of >10% of total beats registered on Holter monitoring), paroxysmal atrial fibrillation, paroxysmal atrial flutter, and other paroxysmal supraventricular tachycardias as well as ventricular extrasystoles (VES), multiform and couplet VES, and ventricular tachycardia may also be present [3,4,5,6,7]. Various studies found that the incidence of SVA was 14% in MVP patients while that of ventricular arrhythmia was 30% [8]. Several studies investigated the pathophysiology of increased arrhythmogenesis but could not explain it fully [5]. The development of arrhythmia has been associated with age, female sex, mitral regurgitation, left atrial diameter, left ventricular end diastolic diameter, mitral anterior leaflet thickness in several studies [3,4,5,6,7]. Zouridakis et al. revealed that QT and ST dispersion and the incidence of complex ventricular arrhythmia increased in patients with severe prolapse and increased anterior leaflet thickness [9]. Markiewicz-Loskot et al. showed that the QT interval was prolonged in young athletes with MVP, which was associated with increased cardiac vagal tonus [10].
Autonomic dysfunction was also associated with both SVA and ventricular arrhythmia. Since the pathogenesis of arrhythmia in MVP patients has not been explained fully, we conducted this study with the aim of determining the role of simple yet important markers such as heart rate variability (HRV), P‑wave dispersion (PWD), and atrial electromechanical delay (AEMD) in order to assess the presence of supraventricular arrhythmia (SVA) in these patients. It is important to collect new information about this topic in order to identify and follow up high-risk MVP patients who may present with a more severe clinical course.
Patients and methods
A total of 76 patients admitted to the cardiology polyclinic for various complaints from 2018 to 2019 and found to have primary MVP at transthoracic echocardiography (TTE) were included in the study. Our study was a single-center retrospective study. Medical history investigation, physical examination, anthropometric evaluation, 12-lead surface electrocardiography (ECG), two-dimensional (2D) color Doppler TTE with tissue Doppler and 24‑h Holter monitoring were performed.
All patients were in sinus rhythm and were not on beta-blockers, calcium channel blockers, or digoxin treatment. None of the patients had a pacemaker. Those with left ventricular systolic dysfunction, chronic pulmonary and renal disease, anemia, hypertension, obesity, diabetes, rheumatic disease, and severe mitral annular calcification were excluded from the study.
All tests were examined and recorded by two different cardiologists. The patients were divided into two groups depending on whether they had supraventricular arrhythmia according to the Holter examination. For each group, PWD, HRV, as well as interatrial and intra-atrial EMD were calculated, compared, and interpreted.
At the planning phase of the study, approval was obtained from the ethics committee of Antalya Training and Research Hospital. Moreover, written consent was obtained from all patients included in the study.
12-Lead ECG
We recorded 12-lead body-surface ECG at a paper speed of 50 mm/s and gain of 10 mm/mV with patients in the supine position where they could breathe freely but were not allowed to speak during the ECG recording. To avoid diurnal variations, we generally evaluated the ECG recordings at the same time (9:00–10:00 a.m.). The analysis was performed by one investigator only, without knowledge of the patient’s clinical status. All ECGs were transferred to a personal computer by an optical scanner and then magnified 400% with Adobe Photoshop software (Adobe Systems Inc., San Jose, CA, USA). P‑wave duration was measured manually from all 12 ECG leads with the help of computer software (ImageJ, NIH, Bethesda, MD, USA). In each ECG lead, the analysis included three consecutive heart cycles wherever possible. The onset of the P wave was defined as the junction between the isoelectric line and the start of P‑wave deflection; the offset of the P wave was the junction between the end of the P‑wave deflection and the isoelectric line. Maximum and minimum P‑wave durations were measured. Maximum P‑wave duration was defined as the longest P‑wave duration, and minimum P‑wave duration was defined as the shortest P‑wave duration. P‑wave dispersion was defined as the difference between the maximum P‑wave duration and the minimum P‑wave duration.
Echocardiography
All patients were examined in the left lateral and supine position with precordial M‑mode, 2D, Doppler and Doppler tissue echocardiography. A one-lead ECG was recorded continuously. Left ventricular end-diastolic and end-systolic diameters as well as end-systolic left atrial (LA) diameter were measured from M‑mode images in the parasternal long-axis views.
Mitral valve anterior and posterior leaflet thicknesses and the degree of prolapse toward the left atrium were measured. Mitral valve prolapse is described as a condition in which one of the leaflets collapses 2 mm or more toward the left atrium starting from the mitral annular line on the parasternal long-axis and apical thee-chamber views of 2D TTE.
The degree of mitral regurgitation was recorded. The degree of mitral regurgitation was assessed as maximal regurgitant jet area/LA area ratio in the parasternal, apical long-axis and apical four-chamber views. Mild [1], moderate [2], and severe [3] mitral regurgitation were classified on the basis of jet area/LA area ratios of >10–20%, >20–40%, and >40%, respectively.
Doppler tissue echocardiography was performed with transducer frequencies of 3.5–4.0 MHz, adjusting the spectral pulsed Doppler signal filters until a Nyquist limit of 15–20 cm/s was reached, and using the minimal optimal gain. The monitor sweep speed was set at 50–100 mm/s to optimize the spectral display of myocardial velocities. In apical four-chamber view, the pulsed Doppler sample volume was placed at the level of the LV lateral mitral annulus, septal mitral annulus, and right ventricular (RV) tricuspid annulus. The Doppler tissue pattern was characterized by a positive myocardial systolic wave and two negative diastolic waves, which were early and atrial. The time interval from the onset of the P wave on surface ECG to the beginning of late diastolic wave (A wave), which is termed “PA,” was obtained from the lateral mitral annulus, septal mitral annulus, and tricuspid annulus, termed “lateral PA,” “septal PA,” and “RV PA,” respectively. The difference between septal PA and RV PA was defined as the intra-atrial EMD and the difference between lateral PA and RV PA was defined as interatrial EMD.
Holter analysis
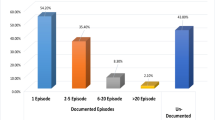
All patients underwent several 24‑h Holter monitoring sessions during the 6‑month follow-up. All patients were in sinus rhythm throughout the recording period. Supraventricular arrhythmias were classified as frequent supraventricular extrasystoles (SVEs, an atrial early beat frequency of >10% of total beats registered on Holter monitoring), paroxysmal atrial fibrillation, paroxysmal atrial flutter, and other paroxysmal supraventricular tachycardias. Overall, 60% of the patients had frequent SVE, 25% had paroxysmal atrial fibrillation, and 15% had paroxysmal supraventricular tachycardias.
The HRV analysis was performed over a 24‑h period in the domains according to the guidelines of the European Society of Cardiology/North American Society of Pacing and Electrophysiology. The following time-domain parameters were calculated: standard deviations of all NN intervals (SDNN); standard deviation of the averages of NN intervals in all 5‑min segments of the entire recording (SDANN); the square root of the mean of the sum of the squares of differences between adjacent NN intervals (rMSSD); the numbers of pairs of adjacent NN intervals differing by more than 50 ms divided by the total number of all NN intervals (pNN50).
Statistical analysis
Data were analyzed with SPSS 24.0 (IBM Corp., Armonk, NY, USA). Continuous variables are expressed as mean ± standard deviation, and categorical variables are expressed as percentage. The chi-square test and Fisher’s exact test were used to compare categorical variables. The Shapiro–Wilk test was used to assess the distribution of continuous variables. Student’s t test was used for variables with normal distribution and the values are presented as mean ± standard deviation. Continuous variables without normal distribution were analyzed using the Mann–Whitney U test and the values obtained are presented as median (50th) values and interquartile ranges (25th and 75th). The effects of different variables on each aortic elasticity parameter were calculated in linear regression analysis. A two-tailed p value of < 0.05 was considered as statistically significant.
Results
In total, 76 patients with primary MVP were included in our study, of whom 56 were female and 20 were male. The patients were divided into two groups according to the presence or absence of SVA: 36 patients in the non-SVA group and 40 patients in the SVA group. The SVA group included 26 female patients, with a mean age of 42.4 ± 16.8 years. In the non-SVA group, however, the rate of female patients was 83.3% and the mean age was 27.3 ± 7.2 years. In the SVA group, the percentage of older patients was significant (p = 0.003). There was no difference between the groups regarding symptoms and underlying diseases (Table 1).
The ECG examination revealed that P max was 100 ms (80.00–100.00), P min was 40 ms (40.00–60.00), PWD was 55.00 msn (40.00–75.00) in the SVA group. However, P max was 80.00 (80.00–100.00) and P min was 40.00 (20.00–60.00) in the non-SVA group. The PWD increased in both groups whereas PWD was significantly higher in the SVA group (p = 0.006; Table 2).
Transthoracic echocardiographic examination demonstrated that the degree of MR was 1.5 ± 1.26 in the SVA group while it was 0.94 ± 1.12 in the non-SVA group. The mean anterior leaflet thickness was 5.35 mm, and the posterior leaflet thickness was 5.10 mm in the SVA group. Leaflet thickness and the degree of mitral regurgitation were found to be significantly higher in the SVA group (p = 0.006, p = <0.001, p = 0.038; Table 3).
Tissue Doppler examination showed that intra-atrial EMD was 10.00 (4.00–14.00) and interatrial EMD was 18.00 (11.00–23.75) in the non-SVA group, whereas intra-atrial EMD was 17.00 (10.00–20.00) and interatrial EMD was 32.00 (25.00–35.00) in the SVA group. Interatrial and intra-atrial EMD was significantly prolonged in the SVA group (p = 0.001, p = <0.001; Table 2).
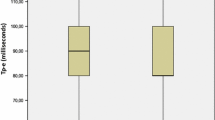
On the basis of 24‑h Holter monitoring, it was found that the maximum heart rate was 140.69 ± 19.56 and the mean heart rate was 75.48 ± 9.46 in the SVA group. In the non-SVA group, however, the maximum heart rate was 145.24 ± 12.42 and the mean heart rate was 77.63 ± 9.56. In the non-SVA group, SDANN was 145.24 ± 12.42 and pNN50 was 10.00 (8.00–18.00), whereas SDANN was 121.00 (104.00–169.00) and pNN50 was 6.5 (2.00–20.75) in the SVA group. The HRV decreased significantly in the SVA group (Table 2).
Univariate and multivariate analyses were conducted for MLTL and MSTL values (see Table 4). Age was found to be a parameter that affected both values (p = 0.005 and p = 0.003, respectively). No significant results were found in the univariate and multivariate analyses regarding the degree of MR and the LA diameter.
Discussion
Patients with MVP usually present with palpitations but it is not known in which cases the palpitations are associated with arrhythmias. Our literature review found several studies that reported on the association between MVP and ventricular arrhythmias; however, there are limited studies on supraventricular arrhythmias. Therefore, in this study, we aimed to find parameters that could predict the risk of SVA in MVP patients. We found that PWD and AEMD values could be used to predict SVA in MVP patients.
In several clinical and biochemical studies, autonomic dysfunction was demonstrated to be present in MVP patients. In many cardiac and noncardiac diseases, HRV was analyzed and autonomic functions were assessed [11]. Decreased HRV indicates decreased vagal activity and increased sympathetic activity. This plays a role in the pathogenesis of ventricular arrhythmia and SCD [12]. Similar to the findings in the literature, HRV parameters also decreased significantly in MVP patients with SVA in our study. Some studies argue that HRV has low sensitivity and low predictive value. These studies highlight that the importance of HRV is controversial, especially in MVP patients [11]. In light of the aforementioned findings, there is a need for more sensitive parameters that can be used to predict the development of SVA in MVP patients.
The most important purpose of our study was to determine the role and importance of PWD and AEMD parameters that have been used in several clinical studies to predict SVA but had not been investigated for MVP patients. P‑wave dispersion is a simple ECG index that shows the homogeneity of atrial electrical activity [13]. A meta-analysis conducted in 2012 demonstrated that the normal range of PWD in 6827 patients was 33.46 ± 9.65 ms [12]. Prolonged PWD indicates nonhomogeneous and noncontinuous atrial electrical activity [12]. Dilaveris et al. and Aytemir et al. showed that PWD was prolonged in patients with a history of paroxysmal atrial fibrillation compared with the control group [13]. Saravi et al. demonstrated that PWD was prolonged in patients with paroxysmal atrial fibrillation with normal left atrial diameter compared with the control group [14]. Our literature review revealed that the role of PWD in predicting the development of SVA in MVP patients had not been investigated at all. In our study, PWD was significantly prolonged in MVP patients who were found to have SVA. In other words, atrial electrical activity was not homogeneous in MVP patients. In our study, PWD was found to be prolonged in patients with SVA; however, there is a need for long-term studies to evaluate the effect of this finding on the development of atrial fibrillation.
For the conduction of the stimulant from the sinus node to the atrium, atrial myocytes must have electrical and functional continuity. Any pathological condition that affects atrial conduction leads to the development of re-entrant atrial arrhythmia. Prolonged interatrial conduction is measured as the gold standard during electrophysiological examinations, which is an invasive method; therefore, it is much easier to calculate it with tissue Doppler imaging. Interatrial conduction abnormalities play a role in the onset and continuation of atrial fibrillation [15]. Atrial dilation, atrial remodeling, and inflammation may lead to prolonged atrial conduction time [15]. Calik et al. reported that prolonged inter/intra-atrial conduction time was more valuable than the LA field and volume for determining the frequency of attacks in patients with atrial fibrillation alone [16]. Kumagai et al. compared patients with paroxysmal atrial fibrillation with a healthy control group in their study. They found that patients with paroxysmal atrial fibrillation were in sinus rhythm while their intra-atrial conduction time was prolonged; in this case, any emerging additional stimulant prolongs the intra-atrial concussion further and paves the way for the development of atrial fibrillation [16]. In our study group of patients, we thought that the diameter of LA and increased degree of MR might also elevate AEMD parameters; therefore, we conducted analyses of the factors that affect interatrial and intra-atrial EMD (Table 4) and demonstrated with univariate and multivariate analyses that AEMD was prolonged independently of the LA diameter and degree of MR. Thus, prolonged atrial conduction time in MVP patients with SVA can be used to predict atrial arrhythmias.
Limitations
The limited number of patients included in the study, the absence of a control group, and the retrospective nature of the study are the limitations of our study. There is a need for further and prospective studies in order to gain more detailed information.
Conclusion
Heart rate variability, P‑wave dispersion (PWD), and atrial electromechanical delay (AEMD) are simple, noninvasive, and inexpensive parameters that can be used to predict the development of supraventricular arrhythmia in patients with mitral valve prolapse. These patients with prolonged interatrial EMD and PWD should be followed up closely and more stringently so as to provide timely prophylactic antiarrhythmic and anticoagulant treatment.
References
ACC-AHA guidelines for the management of patients with valvular heart disease. A report of the American College of Cardiology/American Heart Association. Task Force on Practice Guidelines. J Am Coll Cardiol 1998; 32:1486–588.
Yosefy C, Barak BA (2007) Floppy mitral valve/mitral valve prolapse and genetics. J Heart Valve Dis 16:590–595
Mson DT, Lee G, Chan MC, DeMaria AN (1984) Arrhytmias in patients with mitral valve prolapse. Types, evaluation, and therapy. Med Clin North Am 68(5):1039–1049
Van der Wall EE, Schalij MJ (2010) Mitral valve prolapse: a source of arrhytmias? Int J Cardiovasc Imaging 26(2):147–149
Zuppiroli A, Mori F, Favilli S et al (1994) Arrhythmias in mitral valve prolapse: relation to anterior mitral leaflet thickening , clinical variables, and color doppler echocardiographic parameters. Am Heart J 128(5):919–927
Turker Y, Ozaydın M, Acar G et al (2010) Predictors of ventricular arrhythmias in patients with mitral valve prolapse. Int J Cardiovasc Imaging 26(2):139–145
Turker Y, Ozaydın M, Acar G et al (2009) Predictors of atrial arrhythmias in patients with mitral valve prolapse. Acta Cardiol 64(6):755–760
Çetinkaya M, Semizel E, Bostan O, Çil E (2008) Risk of vasovagal syncope and cardiac arrhytmias in children with mitral valve prolapse. Acta Cardiol 63:395–398
Zouridakis EG, Parthenakis GE, Kochiadakis EM et al (2001) QT dispersion in patients with mitral valve prolapse is related to the echocardiographic degree of the prolapse and mitral leaflet thickness. Europace 3:292–298
Markiewicz-Loskot G, Loskot M, Moric-Janiszewska E et al (2009) Electrocardiographic abnormalities in young athletes with mitral valve prolapse. Clin Cardiol 32(8):E36–E39
Kleiger RE, Stein PK, Bigger JT Jr. (2005) Heart rate variability: measurement and clinical utility. Ann Noninvasive Electrocardiol 10:88–101
Nussinovitch U (2012) Meta-analysis of P‑wave dispersion values in healthy individuals: the influence of clinical characteristics. Ann Noninvasive Electrocardiol 17(1):28–35
Dilaveris PE, Gialafos EJ (2001) P wave dispersion: a novel predictor of paroxysmal atrşal fibrillation. Ann Noninvasive Electrocardiol 6(2):159–165
Saravi M, Montazeri M (2008) Effect of left atria size on p‑wave dispersion: a study in patients with paroxysmal atrial fibrillation. ARYA Atheroscler J 4(1):67–72
Bayes de Luna A, Cladellas M, Oter R et al (1988) Interatrial conduction block and retrograde activation of the left atrium and paroxysmal supraventricular tachyarrhythmia. Eur Heart J 9:1112–1118
Calık AN, Ozcan KS, Cagdas M et al (2014) Electromechanical delay detected by tissue doppler echocardiography is associated with the frequency of attacks in patients with lone atrial fibrillation. Cardiol J 21(2):138–143
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Z. Erkal, N. Bayar, E. Koklu, G. Cagırcı, S. Arslan, and R. Guven declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case. This retrospective study was performed after consultation with the institutional ethics committee and in accordance with national legal requirements.
Rights and permissions
About this article
Cite this article
Erkal, Z., Bayar, N., Koklu, E. et al. Supraventricular arrhythmia in mitral valve prolapse. Herz 47, 67–72 (2022). https://doi.org/10.1007/s00059-021-05034-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-021-05034-1