Abstract
Background
The Kailuan Study examined cardiovascular risk factors in a Chinese cohort comprising employees of the Kailuan Coal Group who underwent regular health examinations.
Patients and methods
Normotensive participants in the Kailuan study were enrolled in the present work and followed up for a median of 5.8 years to assess the development of hypertension (systolic blood pressure [SBP] ≥140 mmHg, diastolic blood pressure [DBP] ≥90 mmHg, or initiation of blood pressure [BP] medications).
Results
This study comprised a total of 50,024 participants (age, 47.9 ± 12.0 years; male/female, 37,429/12,595), of whom 22,176 (44.3%) developed hypertension. In both male and female subjects, there was an increase in multivariable-adjusted hazard ratios for hypertension in all waist circumference (WC) groups (group 1, <70 cm; group 2, 70–79 cm; group 3, 80–89 cm; group 4, 90–99 cm; group 5, ≥100 cm). Results of a stratified analysis of subjects with normal body mass index (BMI; <24 kg/m2) showed that hazard ratios for hypertension still increased across WC groups. Significant interactions were found between WC groups and gender (p <0.001), as well as between WC groups and BP categories (p <0.001). Increased WC was associated with a significantly higher risk of hypertension incidence in men compared with women and in subjects with a high–normal BP vs. those with an ideal BP.
Conclusion
WC is an independent predictor of hypertension incidence. The association between WC and hypertension incidence is affected by gender and baseline BP levels.
Zusammenfassung
Hintergrund
In der Kailuan-Studie wurden die kardiovaskulären Risikofaktoren in einer chinesischen Kohorte untersucht, die aus Mitarbeitern der Kailuan Coal Group bestand und regelmäßig auf ihren Gesundheitszustand hin untersucht wurde.
Patienten und Methoden
Normotensive Teilnehmer der Kailuan-Studie wurden in die vorliegende Studie aufgenommen und im Mittel 5,8 Jahre lang nachbeobachtet, um zu ermitteln, ob sich eine Hypertonie entwickelte (systolischer Blutdruck ≥140 mmHg, diastolischer Blutdruck ≥90 mmHg oder Beginn der Gabe von Blutdruckmedikamenten).
Ergebnisse
Insgesamt wurden 50.024 Teilnehmer in diese Studie aufgenommen (Alter: 47,9 ± 12,0 Jahre; m./w.: 37.429/12.595), davon entwickelten 22.176 (44,3%) eine Hypertonie. Sowohl bei männlichen als auch bei weiblichen Probanden gab es einen Anstieg der multivariabel angepassten Hazard-Ratio für Hypertonie in allen nach Taillenumfang unterteilten Gruppen (Gruppe 1: <70 cm; Gruppe 2: 70–79 cm; Gruppe 3: 80–89 cm; Gruppe 4: 90–99 cm; Gruppe 5: ≥100 cm). Ergebnisse einer stratifizierten Auswertung von Probanden mit normalem Body-Mass-Index (BMI; <24 kg/m2) zeigten, dass die Hazard-Ratio für Hypertonie quer durch die nach Taillenumfang unterteilten Gruppen weiterhin anstieg. Signifikante Wechselwirkungen fanden sich zwischen nach Taillenumfang unterteilten Gruppen und Geschlecht (p <0,001) sowie zwischen nach Taillenumfang unterteilten Gruppen und Blutdruckkategorie (p <0,001). Ein erhöhter Taillenumfang ging mit einem signifikant erhöhten Inzidenzrisiko für Hypertonie bei Männern im Vergleich zu Frauen sowie bei Probanden mit einem hochnormalen Blutdruck gegenüber Probanden mit idealen Blutdruckwerten einher.
Schlussfolgerung
Der Taillenumfang ist ein unabhängiger Prädiktor für die Inzidenz der Hypertonie. Der Zusammenhang zwischen Taillenumfang und Inzidenz der Hypertonie wird durch Geschlecht und Ausgangsblutdruckwerte beeinflusst.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Waist circumference (WC) has been shown to be, independent of body mass index (BMI), associated with an increased risk of multiple chronic noncommunicable diseases (NCDs, such as hypertension, stroke, heart disease, and diabetes mellitus) [1–6]. However, as an index of central obesity, WC has not yet been included in the final recommendations for diagnostic criteria or disease classifications by the World Health Organization [7]. Studies have considered the variations in WC by age, sex, and ethnicity, and the levels at which WC predicted the risk of different NCDs or total mortality. In fact, WC appears to increase the risk of obesity-related complications in a graded fashion rather than only at high WC thresholds.
Previous studies mainly focused on the predictive value of high WC in the risk of obesity-related chronic diseases [8–12]. A number of expert groups have attempted to develop unifying criteria for high WC in diagnosing central obesity, but they appear to be ineffective. Taking the Chinese population as an example, the consensus statement of metabolic syndrome definition at the International Diabetes Federation workshop [13] suggested abdominal obesity based on sex-specific criteria for high WC were over 80 cm and over 90 cm for Chinese women and men, respectively. However, the Chinese Guideline for Prevention and Treatment of Patients with Hypertension recommended a WC over 85 cm for women and over 90 cm for men as the boundary values. And the results from a meta-analysis organized by the Working Group on Obesity in China [14] showed that the cut-off points of WC for central obesity were over 80 cm and over 85 cm for Chinese women and men, respectively, in predicting obesity-related diseases.
In the present study, we examined the association between WC and the risk of hypertension incidence, discussing the predictive value of low/medium/high levels of WC for hypertension in Chinese adults. Moreover, we evaluated the effects of other factors (such as BMI) on the association between WC and hypertension.
Patients and methods
Study setting and participants
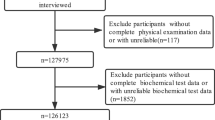
All subjects were participants of the Kailuan Study (registration number: ChiCTR-TNRC-11001489) from the Kailuan community in Tangshan, a city in the north of China. The Kailuan community is a functional and comprehensive community owned and managed by the Kailuan Group. There are 11 hospitals responsible for the health care of the community. The health records of 101,510 participants (81,110 men and 20,400 women; 18–98 years of age) from 11 hospitals during the period June 2006 to October 2007 were used. The participants met the following criteria: (1) age ≥18 years; (2) provided informed consent; and (3) updated their health status every 2 years according to the follow-up protocol. All participants completed a questionnaire and underwent clinical examination and laboratory assessment. Standard protocols were used for all of the measurements as described earlier [15–18] and were administered by specially trained doctors and nurses. The study was performed according to the guidelines of Helsinki Declaration and was approved jointly by the Ethics Committee of the Kailuan General Hospital and Beijing Chaoyang Hospital. Written informed consent was obtained from all participants.
Until December 2013, three follow-up visits were completed for all participants. In our analysis, we excluded patients who had a history of hypertension at baseline (n = 45,789) and who never showed up to the three follow-up visits (n = 5214). After excluding those with missing values for WC (n = 483), a total of 50,024 participants (37,429 men and 12,595 women) were analyzed.
Data collection
Anthropometric measurements
Anthropometric indices included WC, height, and weight. All the individuals were measured wearing light clothing without shoes and hats. WC was measured to the nearest 0.1 cm at the midpoint between the subcostal margin and the margin of the supracristal plane according to the diagnostic criteria of the International Diabetes Federation (IDF). Height was measured to the nearest 0.1 cm using a portable stadiometer and weight was measured to the nearest 0.1 kg using calibrated platform scales. BMI was calculated as body weight (kg) divided by the square of height (m2).
Blood pressure measurements
Blood pressure (BP) was measured in the sitting position using a mercury sphygmomanometer with an appropriate cuff size. After a 5-min rest period, BP was measured three times, and the average of the three measurements was used for statistical analyses.
Questionnaire
All participants were administered a standardized questionnaire that provided information relating to occupation, medical history, past and current medication use, and personal habits such as cigarette and alcohol consumption.
Laboratory tests
Fasting venous blood samples were collected to measure glucose, uric acid, creatinine, and lipid levels (including total cholesterol, high-density lipoprotein cholesterol [HDL-C], and triglycerides).
Hypertension definition
Hypertension was defined as SBP ≥140 mmHg, DBP ≥90 mmHg, or the participant taking any antihypertensive medications. Antihypertensive medications were defined as any diuretic, alpha blocker, beta blocker, calcium channel blocker, angiotensin-converting enzyme inhibitor or angiotensin receptor blocker, nitrate, and hydralazine.
Data analysis
Statistical analyses were performed using R, version 3.1.1. Data are presented as mean (standard deviation [SD]) for continuous variables or proportions for categorical variables. We conducted Cox proportional-hazards analyses to estimate the hazard ratios and 95% confidence intervals for the development of hypertension in male and female subjects. WC was evaluated as a categorical variable (WC groups: group 1, <70 cm; group 2, 70–79 cm; group 3, 80–89 cm; group 4, 90–99 cm; group 5, ≥100 cm; or <80 cm, 80–89 cm, ≥90 cm in the Figure). Trend tests were computed by modeling the WC group medians as continuous variables. Interactions between covariables (as categorical variables) and WC were also evaluated. BMI categories were divided by 24 kg/m2 using the criteria established by the Working Group on Obesity in China [19]; BP groups were defined as high–normal BP (SBP ≥130 mmHg or DBP ≥80 mmHg) and ideal BP (SBP <130 mmHg and DBP <80 mmHg). Interaction terms were computed by modeling the medians of the WC groups as continuous variables.
Results
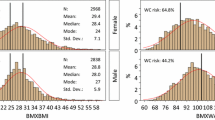
The present study included 50,024 subjects (age: 47.9 ± 12.0 years, male/female 37,429/12,595). As shown in Table 1, after a median follow-up of 5.8 years, 22,176 participants (44.3%) developed hypertension, including 18,301 (48.9%) men and 3875 (30.8%) women. The mean value of WC was 85.0 cm (in all subjects): 86.4 cm in male and 80.8 cm in female subjects. All the covariates in the study included BMI, age, SBP, DBP, resting heart rate, glucose, total cholesterol, triglycerides, low-density lipoprotein cholesterol (LDL-C), HDL-C, uric acid, creatinine, smoking, and alcohol consumption.
As shown in Table 2, in male subjects, age-adjusted hazard ratios for hypertension increased across the WC groups (group 1, <70 cm; group 2, 70–79 cm; group 3, 80–89 cm; group 4, 90–99 cm; group 5, ≥100 cm), reaching 2.60 (95% confidence interval, 2.28 to 2.96) for the top group as compared with the bottom group (p for trend <0.001). Further adjustments for BMI and BP (including SBP and DBP) attenuated the risk values. In a multivariate model further adjusted for resting heart rate, glucose, total cholesterol, triglycerides, LDL-C, HDL-C, uric acid, creatinine, smoking, and alcohol consumption (besides age, BMI, and BP) only mildly attenuated the risk values as compared with the previous model (adjusted for age, BMI, and BP). Similarly, in female subjects, age-adjusted hazard ratios for hypertension also increased across WC groups, reaching 3.46 (95% confidence interval, 2.83–4.23) for the top group as compared with the bottom group (p for trend <0.001). Further adjustments for BMI and BP also attenuated the risk values, which were only mildly attenuated in the multivariate model. The interaction term between WC groups and sex was significant (p for interaction <0.001): As shown in Fig. 1a, women in the bottom group (WC <80 cm) showed the lowest risk while men in the top group (WC ≥90 cm) showed the highest risk. As WC increased, men compared with women had significantly higher risk of hypertension incidence.
Joint effect of waist circumference values, gender, and blood pressure levels in predicting hypertension. a Hazard ratios for hypertension according to waist circumference levels and gender. b Hazard ratios according to blood pressure (BP) levels; ideal BP: systolic blood pressure (SBP) <130 mmHg and diastolic blood pressure (DBP) <80 mmHg; high–normal BP: SBP ≥130 mmHg or DBP ≥80 mmHg in male subjects. c Hazard ratios according to BP levels in female subjects. The multivariate Cox regression model was adjusted, if not stratified, for age, body mass index, systolic blood pressure, DBP, resting heart rate, glucose, total cholesterol, triglycerides, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, uric acid, creatinine, smoking, and alcohol consumption
The results of a stratified analysis of multivariate hazard ratios for hypertension according to WC groups are shown in Table 3. In male subjects with high–normal BP (SBP ≥130 mmHg or DBP ≥80 mmHg) or ideal BP (SBP <130 mmHg and DBP <80 mmHg) at baseline, hazard ratios for hypertension increased across WC groups (p for trend <0.001). However, compared with men with ideal BP, those with high–normal BP had significantly higher risk of hypertension incidence: As shown in Fig. 1b, men with ideal BP in the bottom group (WC <80 cm) showed the lowest risk while men with high–normal BP in the top group (WC ≥90 cm) showed the highest risk. Similarly, as shown in Fig. 1c, women with high–normal BP also had significantly higher risk of hypertension incidence than those with ideal BP.
In all subjects (both male and female) with normal BMI (BMI <24 kg/m2), hazard ratios for hypertension increased across WC groups (group 1, <70 cm; group 2, 70–79 cm; group 3, 80–89 cm; group 4, 90–99 cm; group 5, ≥100 cm). Compared with group 1 (WC <70 cm), group 2 (70 cm ≤ WC < 80 cm) already showed significantly higher risk of hypertension incidence, suggesting a much more tight control of WC is needed for decreasing hypertension risk. Interaction terms between WC groups with BMI or other factors were also evaluated in both male and female subjects, but none was found to be significant.
Discussion
This prospective study contributes several important findings. First, it shows that WC appears to be an important obesity-related predictor of hypertension incidence, and it increases the risk of hypertension in a dose-response fashion rather than only at high WC thresholds. Second, the association between WC and hypertension incidence is also affected by gender and baseline BP levels; as WC increased, men compared with women, and subjects (both male and female) with high–normal BP (SBP ≥130 mmHg or DBP ≥80 mmHg) compared with those with ideal BP (SBP <130 mmHg and DBP <80 mmHg), showed significantly higher risk of hypertension incidence. Third, stratified analysis also showed that, in subjects (both male and female) with normal BMI (BMI <24 kg/m2) and low WC (WC <80 cm), the risk of hypertension still increased as WC increased.
Consistent with previous studies [20–23], the present research showed that WC, independent of BMI, was an important predictor of hypertension incidence in a Chinese population. For predicting obesity-related diseases (such as hypertension, stroke, heart disease, diabetes mellitus, and lipoprotein disorders), previous studies recommended Chinese-specific WC values ranging from 80.5 to 95.1 cm for men and 71.5 to 83.7 cm for women. However, in the present study, we found that, as WC increases, the risk of hypertension increases in a dose-response fashion, and both men and women in WC group 2 (70 cm ≤ WC <80 cm) had a higher risk than those in WC group 1 (WC <70 cm), which suggested a lower WC cut-off point. Moreover, even in subjects with normal BMI (BMI <24 kg/m2), hazard ratios for hypertension still increased across WC groups (group 1, <70 cm; group 2, 70–79 cm; group 3, 80–89 cm; group 4, 90–99 cm; group 5, ≥100 cm).
Interestingly, all previous studies in Chinese populations [22–29] suggested lower WC values in women than in men, that is, a much more rigorous control of WC is needed in women than in men. However, in the present study, joint effects of gender and WC on hypertension risk showed that men had significantly higher risk of hypertension incidence as WC increased compared with women. Additionally, the association between WC and hypertension incidence is also affected by baseline BP levels, and subjects with high–normal BP compared with those with ideal BP showed a significantly higher risk of hypertension incidence, which suggests a much more rigorous control of WC in subjects with high–normal BP than those with ideal BP.
Although the biological mechanisms responsible for the association between WC and hypertension are still unknown, metabolic products of intra-abdominal adipose tissue, such as inflammatory adipokines, angiotensinogen (AGN), or cortisol, have been proposed [30]. Visceral adipose tissue produces a large amount of proinflammatory cytokines, AGN [31], leptin, reactive oxygen species [32], etc., and by doing so promotes activation of the sympathetic nervous system [33] and the renin-angiotensin system [34], insulin resistance, and metabolic syndrome [32], which are further linked to hypertension incidence.
Our study was limited in the following aspects. First, the Kailuan Study participants were predominantly from the Kailuan community in Tangshan, a city in the north of China, and thus the generalizability of our findings to other populations requires caution. Second, the present study mainly focused on the relationship between WC and hypertension incidence; future studies should further analyze the associations between WC and other obesity-related diseases.
Conclusion
In summary, our findings suggest that WC is an independent predictor of hypertension incidence, and it increases the risk of hypertension in a dose-response fashion rather than only at high WC thresholds. The association between WC and hypertension incidence is also affected by gender and baseline BP levels. Males and subjects with high–normal BP (SBP ≥130 mmHg or DBP ≥80 mmHg) should have a much more rigorous control of WC.
References
Folsom ARPR, Kaye SA, Munger RG (1990) Incidence of hypertension and stroke in relation to body fat distribution and other risk factors in older women. Stroke 21:701–706
Rimm EBSM, Giovannucci E, Ascherio A, Spiegelman D, Colditz GA, Willett WC (1995) Body size and fat distribution as predictors of coronary heart disease among middle-aged and older us men. Am J Epidemiol 141:1117–1127
Rexrode KMCV, Hennekens CH, Walters EE, Colditz GA, Stampfer MJ, Willett WC, Manson JE (1998) Abdominal adiposity and coronary heart disease in women. JAMA 280:1843–1848
Harris MMSJ, Thomas N, Schreiner P, Folsom AR (2000) Associations of fat distribution and obesity with hypertension in a bi-ethnic population: the aric study. Atherosclerosis risk in communities study. Obes Res 8:516–524
Wang YRE, Stampfer MJ, Willett WC, Hu FB (2005) Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am J Clin Nutr 81:555–563
Folsom ARKL, Anderson KE, Mink PJ, Olson JE, Hong CP, Sellers TA, Lazovich D, Prineas RJ (2000) Associations of general and abdominal obesity with multiple health outcomes in older women: The iowa women’s health study. Arch Intern Med 160:2117–2128
Nishida CGK (2010) S Kumanyika Body fat distribution and noncommunicable diseases in populations: overview of the 2008 who expert consultation on waist circumference and waist-hip ratio. Eur J Clin Nutr 64:2–5
Huxley RSM, Zheleznyakov E, Reddy S, Chan J (2010) Body mass index, waist circumference and waist:hip ratio as predictors of cardiovascular risk – a review of the literature. Eur J Clin Nutr 64:16–22
Lear SAPJ, Ko GT, Kumanyika S (2010) Appropriateness of waist circumference and waist-to-hip ratio cutoffs for different ethnic groups. Eur J Clin Nutr 64:42–61
Seidell J (2010) Waist circumference and waist/hip ratio in relation to all-cause mortality, cancer and sleep apnea. Eur J Clin Nutr 64:35–41
Qiao QRN (2010) The optimal cutoff values and their performance of waist circumference and waist-to-hip ratio for diagnosing type II diabetes. Eur J Clin Nutr 64:23–29
Stevens JEK, Huxley RR (2010) Associations between gender, age and waist circumference. Eur J Clin Nutr 64:6–15
Alberti KGMMPZ, Shaw J (2006) Metabolic syndrome-a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med 23:469–480
Bei-Fan Z, The Cooperative Meta-analysis Group of Working Group on Obesity in China (2002) Predictive values of body mass index and waist circumference for risk factors of certain related diseases in chinese adults: Study on optimal cut-off points of body mass index and waist circumference in chinese adults. Asia Pac J Clin Nutr 11:685–S693
Meng Peng SW, Jiang X, Jin C, Zhang W, Kailuan Cardiovascular Survey Group (2013) Long-term alcohol consumption is an independent risk factor of hypertension development in Northern China: Evidence from Kailuan Study. J Hypertens 31:2342–2347
Shouling Wu ZH, Yang X, Zhou Y, Wang A, Chen L, Zhao H, Ruan C, Wu Y, Xin A, Li K, Jin C, Cai J (2012) Prevalence of ideal cardiovascular health and its relationship with the 4‑year cardiovascular events in a northern chinese industrial city. Circ Cardiovasc Qual Outcomes 5:487–493
Shouling Wu YL, Jin C, Yang P, Li D, Li H, Shen C (2012) Intra-individual variability of high-sensitivity c‑reactive protein in chinese general population. Int J Cardiol 157:75–79
Wang FSW, Song Y, Tang X, Marshall R, Liang M, Wu Y, Qin X, Chen D, Hu Y (2009) Waist circumference, body mass index and waist to hip ratio for prediction of the metabolic syndrome in chinese. Nutrition Metab Cardiovasc Dis 19:542–547
Working Group on Obesity in China DoDC MoH (2004) The guidelines for prevention and control of overweight and obesity in chinese adults. Biomed Environ Sci 17:1–35
Bombelli MRF, Sega R, Carugo S, Fodri D, Brambilla G, Giannattasio C, Grassi G, Mancia G (2011) Impact of body mass index and waist circumference on the long-term risk of diabetes mellitus, hypertension, and cardiac organ damage. Hypertension 58:1029–1035
Levine DADAC, Prineas RJ, Cushman M, Howard VJ, Howard G (2011) Moderate waist circumference and hypertension prevalence: The regards study. Am J Hypertens 24:482–488
Bao YLJ, Wang C, Yang M, Li H, Zhang X, Zhu J, Lu H, Jia W, Xiang K (2008) Optimal waist circumference cutoffs for abdominal obesity in chinese. Atherosclerosis 201:378–384
Lin WYLL, Chen CY, Lo H, Hsia HH, Liu IL, Lin RS, Shau WY, Huang KC (2002) Optimal cut-off values for obesity: Using simple anthropometric indices to predict cardiovascular risk factors in taiwan. Int J Obes Relat Metab Disord 26:1232–1238
Ko GTCJ, Cockram CS, Woo J (1999) Prediction of hypertension, diabetes, dyslipidaemia or albuminuria using simple anthropometric indexes in hong kong chinese. Int J Obes Relat Metab Disord 23:1136–1142
Deurenberg-Yap MCS, Lin VF, Tan BY, van Staveren WA, Deurenberg P (2001) Relationships between indices of obesity and its co-morbidities in multi-ethnic singapore. Int J Obes Relat Metab Disord 25:1554–1562
Bei-Fan Z (2002) Predictive values of body mass index and waist circumference for risk factors of certain related diseases in chinese adults: Study on optimal cut-off points of body mass index and waist circumference in chinese adults. Asia Pac J Clin Nutr 11:S685–S693
Diaz VA, Baker R, Carnemolla M, Majeed A (2007) How does ethnicity affect the association between obesity and diabetes? Diabet Med 24:1199–1204
Ko GTTJ (2007) Waist circumference and bmi cut-off based on 10-year cardiovascular risk: evidence for ’central pre-obesity’. Obesity (Silver Spring) 15:2832–2839
Li RLW, Jia J, Zhang S, Shi L, Li Y, Yang Q, Kan H (2008) Relationships between indices of obesity and its cardiovascular comorbidities in a chinese population. Circ J 72:973–978
Mathieu PPP, Pibarot P, Lemieux I, Després JP (2009) Visceral obesity: The link among inflammation, hypertension, and cardiovascular disease. Hypertension 53:577–584
Paulmyer-Lacroix OBS, Oliver C, Alessi MC, Grino M (2002) Expression of the mrna coding for 11beta-hydroxysteroid dehydrogenase type 1 in adipose tissue from obese patients: an in situ hybridization study. J Clin Endocrinol Metab 87:2701–2705
Furukawa SFT, Shimabukuro M, Iwaki M, Yamada Y, Nakajima Y, Nakayama O, Makishima M, Matsuda M, Shimomura I (2004) Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest 114:1752–1761
DiBona GF (2004) The sympathetic nervous system and hypertension: Recent developments. Hypertension 43:147–150
Furuhashi MUN, Higashiura K, Murakami H, Tanaka M, Moniwa N, Yoshida D, Shimamoto K (2003) Blockade of the renin-angiotensin system increases adiponectin concentrations in patients with essential hypertension. Hypertension 42:76–81
Funding
The study was funded by China’s National Key Technology Support Program during the 12th 5‑year plan period: Study, Evaluation and Popularization of Hypertension Technologies in Prevention and Treatment Among Communities (SEP-HTC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H. Sun, M. Zheng, S. Wu, M. Chen, J. Cai, and X. Yang declare that they have no competing interests.
The study was performed according to the guidelines of Helsinki Declaration and was approved jointly by the Ethics Committee of the Kailuan General Hospital and Beijing Chaoyang Hospital. Written informed consent was obtained from all participants.
Additional information
Author contributions Study design: Xinchun Yang, Jun Cai; literature research: Hao Sun, Meili Zheng; data acquisition: Shouling Wu, Meili Zheng; data analysis/interpretation: Meili Zheng; manuscript editing: Hao Sun; manuscript revision/review: Xinchun Yang
Rights and permissions
About this article
Cite this article
Sun, H., Zheng, M., Wu, S. et al. Waist circumference and incidence of hypertension in Chinese adults. Herz 42, 677–683 (2017). https://doi.org/10.1007/s00059-016-4501-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-016-4501-x