Abstract
Objective
The purpose of this study was to compare the asymmetry index determined on digital panoramic radiographic (PR) images and posteroanterior cephalometric (PACR) images.
Methods
This study included 100 patients whose PR and PACR images were registered in a database. Condylar height, ramus height, and condylar height plus ramus height measurements were measured bilaterally. Condylar asymmetry, ramus asymmetry, and total asymmetry were evaluated.
Results
There was a statistically significant difference between the right and left side for all measurements when evaluated on the PR and also on the PACR images (p < 0.01). When calculating the asymmetry index, the resulting condylar asymmetry and ramus asymmetry values did not show significant differences between PR and PACR images. On the other hand, only the presence of total asymmetry showed a statistically significant difference between techniques (p = 0.013).
Conclusion
Asymmetry indices can be reliably obtained from both PR and PACR images.
Zusammenfassung
Zielsetzung
Ziel dieser Studie war es, den anhand von digitalen Panoramaröntgenbildern (PR) mit dem anhand von posteroanterioren Fernröntgenbildern (PACR) ermittelten Asymmetrieindex zu vergleichen.
Methoden
An dieser Studie nahmen 100 Patienten teil, deren PR- und PACR-Aufnahmen in einer Datenbank registriert waren. Kondylenhöhe, Ramushöhe und Kondylenhöhe plus Ramushöhe wurden beidseitig gemessen. Kondylenasymmetrie, Ramusasymmetrie und Gesamtasymmetrie wurden bewertet.
Ergebnisse
Bei allen Messungen gab es einen statistisch signifikanten Unterschied zwischen der rechten und der linken Seite, sowohl bei der Auswertung der PR- als auch der PACR-Aufnahmen (p < 0,01). Bei der Berechnung des Asymmetrieindexes zeigten die resultierenden Werte für die Kondylenasymmetrie und die Ramusasymmetrie keine signifikanten Unterschiede zwischen PR- und PACR-Aufnahmen. Andererseits zeigte nur das Vorhandensein einer Gesamtasymmetrie einen statistisch signifikanten Unterschied zwischen den Techniken (p = 0,013).
Schlussfolgerung
Asymmetrieindizes können sowohl aus PR- als auch aus PACR-Aufnahmen zuverlässig ermittelt werden.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In vertebrates, bilateral structures are generally symmetrical with each other. However, perfect symmetry is a theoretical concept. For example, the face has a natural degree of asymmetry [1].
Mandibular asymmetry or that of the lower third of the face has a direct effect on the appearance of the face [2]. Diagnosis of mandibular asymmetry is complex [3]. Although minor mandibular asymmetries have been reported to be a common feature in growing patients, greater differences of more than 2–3 mm between the left and right sides of the mandible are considered to have clinical relevance [4]. For clinical diagnosis, different radiographic techniques have been described [2, 3, 5,6,7,8].
In 1988, Habets et al. [9] published an asymmetry index to evaluate dimensional asymmetries of the mandibular condyle and mandibular ramus in panoramic radiographs (PR). As the asymmetry index can be calculated from routine PR taken for orthodontic purposes, exposure to additional radiation when taking additional X‑rays is avoided. In some studies in the literature, this index has also been applied to posteroanterior cephalometric radiographs (PACR) [10, 11]. However, due to superimposition of anatomical structures in the area of the condyles, calculating the asymmetry index from PACR images may result in clinical misinterpretation. Although it has been shown that vertical measurements made in PR and PACR images are compatible with each other [3], to our knowledge there is no study comparing digital PR images with respect to the asymmetry index. The hypothesis of this study was that there would be statistically significant differences for asymmetry index values if determined from digital PR images or PACR images.
Materials and methods
Data collection
This study was approved by the Clinical Research Ethics Committee of the Faculty of Medicine Akdeniz University, and the study was carried out in accordance with the ethical rules of the Declaration of Helsinki (ethics approval number 70904504/90).
The records of patients who presented to the Faculty of Dentistry, Oral and Maxillofacial Radiology Department, Akdeniz University, for orthodontic treatment between 2014 and 2017 were assessed; 152 patients who had PR and PACR images were identified.
The following inclusion and exclusion criteria were used for the study. Inclusion criteria were (1) patients aged 10–17 years who were in the growth and development period, (2) pretreatment PR and PACR images, (3) presence of normal anatomic condyle and coronoid processes in radiographic images, (4) absence of systemic diseases affecting bone structure, (5) presence or absence of the third molar tooth and presence of all teeth or teeth germs, and (6) absence of trauma affecting bone structure. Exclusion criteria were (1) PR and PACR images, wherein anatomical points needed to perform linear measurements were not clearly visualized, (2) poor image quality with horizontal distortions, and (3) images wherein temporomandibular joint pathology was suspected. When these criteria were taken into consideration, the radiographic images of 38 patients with anatomical points that were not clearly visualized on PR or PACR, 8 patients with missing teeth, and 6 patients with poor image quality were excluded from the study. Thus, PR and PACR images of 100 patients were included in the study.
Both PR and PACR were taken on the same day for routine evaluation of preorthodontic treatment. All PR and PACR images were obtained by the same X‑ray technician using the same Planmeca ProMax panoramic-cephalometric device (Planmeca Oy, Helsinki, Finland), in accordance with the manufacturer’s instructions (for PR: 66 kVp, 7 mA, and 16 s exposure and for PACR: 64 kVp, 5 mA, and 18 s exposure). All PR and PACR images were evaluated in a reduced-light room using the same LED monitor, held approximately 30–40 cm away from the LED monitor, by the same investigator, who is an expert in dental radiology and has 7 years of experience. A maximum of five PR and maximum of five PACR images were evaluated per day to avoid investigator fatigue.
Mandibular measurements
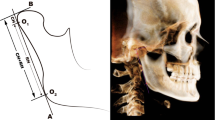
A line, B line, O1 point, O2 point, condylar height (CH), and ramus height (RH) were determined according to Habets et al. [9] for PR (Fig. 1) and PACR (Fig. 2).
Anatomical points, definitions, and linear measurements on a panoramic radiographic image. Co Most superior part of the condylar image, O1 and O2 Most lateral points of the image, A line Ramus tangent, B line Perpendicular line from Co to A line, CH Condylar height, RH Ramal height, CH + RH Total height
Anatomische Punkte, Definitionen und lineare Messungen auf einem Panoramaröntgenbild. Co oberster Teil des Kondylenbildes, O1 und O2 am weitesten seitliche Punkte des Bildes, A-Linie Ramustangente, B‑Linie senkrechte Linie von Co zur A‑Linie, CH Kondylenhöhe, RH Ramushöhe, CH + RH Gesamthöhe
Anatomical points, definitions, and linear measurements on a posteroanterior cephalometry image. Co Most superior part of the condylar image, O1 and O2 Most lateral points of the image, A line Ramus tangent, B line Perpendicular line from Co to A line, CH Condylar height, RH Ramal height, CH + RH Total height
Anatomische Punkte, Definitionen und lineare Messungen auf einem Panoramaröntgenbild. Co oberster Teil des Kondylenbildes, O1 und O2 am weitesten seitliche Punkte des Bildes, A-Linie Ramustangente, B‑Linie senkrechte Linie von Co zur A‑Linie, CH Kondylenhöhe, RH Ramushöhe, CH + RH Gesamthöhe
Linear measurements taken from the PR and PACR images were as follows:
-
CH: distance between points Co and O1,
-
RH: distance between points O1 and O2, and
-
CH + RH: distance between points Co and O2.
Measurements were performed bilaterally for both radiographic methods. Measurements were automatically calibrated with the Planmeca Romexis 4.0 software program developed for the Planmeca ProMax device (Planmeca Oy, Helsinki, Finland), according to the manufacturer’s instructions. The asymmetry indices were determined using the formula developed by Habets et al. [9] and a > 3% difference was recorded as condylar asymmetry, ramus asymmetry, and total asymmetry:
After 4 weeks, all measurements were repeated in 30 randomly selected patients, and intraobserver variability was assessed.
Statistical analysis
Data were statistically analysed using SPSS Statistics (version 23.0, IBM, Armonk, NY, USA). The normality assumption was evaluated using the Shapiro–Wilk test. While the paired-samples t‑test was applied to data with a normal distribution, the Wilcoxon signed ranks test was used for data not displaying a normal distribution. The McNemar test was used to analyze the difference between two dependent ratios. Intraobserver reliability was assessed by intraclass correlation coefficient. A p value of < 0.05 was considered significant.
Results
The intraclass correlation coefficient was found to be greater than 80% for all parameters (right CH, left CH, right RH, left RH, right CH + RH, and left CH + RH) and for both radiographic techniques (PR and PACR).
The CH, RH, and CH + RH measurements were performed bilaterally on PR and PACR images of 100 patients in this study: 46 (46%) were male and 54 (54%) were female. The age of the patients ranged between 10 and 17 years (mean age 12.59 ± 1.6 years).
Right CH and left CH measurements in PR were higher than right CH and left CH measurements in PACR in 80 and 83 patients, respectively. In all patients, right RH, left RH, right CH + RH, and left CH + RH measurements in PR were higher than right RH, left RH, right CH + RH, and left CH + RH measurements in PACR. There was a statistically significant difference between right and left PR and right and left PACR measurements for all parameters (p < 0.01). Table 1 shows the minimum, maximum, mean, standard deviation, and p values of left and right measurements for both radiographic techniques.
Table 2 shows the minimum, maximum, mean, standard deviation, median, and p values for the AI values obtained as a result of the AI formula in both radiographic techniques. AI values did not show a significant difference between PR and PACR images. Table 3 shows the number of patients with asymmetry and without asymmetry in PR, PACR, and both radiographic techniques. While the presence of condylar asymmetry and of ramus asymmetry between PR and PACR did not show a statistically significant difference (p = 0.5 and 0.203, respectively), the presence of total asymmetry showed a statistically significant difference between the two radiographic techniques (p = 0.013). While total asymmetry was found in 45 individuals in PACR, this number was 27 in PR. The intraclass correlation coefficient was found to be greater than 0.90 in all parameters.
Discussion
Asymmetries are complex anomalies which can affect all components of the stomatognathic system in all three planes [1]. Mandibular asymmetry is important because it directly affects facial esthetics and can cause functional problems due to its stomatognathic role [2]. While asymmetry can be diagnosed clinically with frontal and side photos [3], it can be detected radiographically using PR, lateral cephalometric radiography, PACR, 45° oblique radiography of the mandible [3], and submentovertex radiography [5], or by computed tomography [7], cone-beam computed tomography [8], and magnetic resonance imaging [2, 3, 5, 6].
PR is considered the standard for orthodontic treatment planning and dental diagnostics [12]. It is also used to measure condyle, ramus, and total height to diagnose dimensional differences and asymmetries [2, 12, 13]. Kjellberg et al. [14] and Habets et al. [9, 15] developed techniques to determine mandibular asymmetry in PR. While the first of these techniques compares CH and RH ratios on both sides to determine asymmetry, the other uses a linear calculation method [16].
In 1988, Habets et al. [9] used an AI formula to evaluate the mandibular condyle and mandibular ramus. This formula is based on CH and RH measurements. According to this formula, a 3% index rate may originate from a 1 cm displacement in head position during PR, whereas a > 3% difference indicates the existence of asymmetry.
While asymmetry determination is frequently performed on PR [2, 12, 13, 17,18,19,20,21], PACR can be used as the first choice in the diagnosis of facial asymmetry [10, 22]. PACR allows comparison of both sides of the face and provides mediolateral information which is useful for the evaluation of facial asymmetry [3]. Agrawal et al. [3] compared linear measurements between PR and PACR, and they found a strong correlation between these radiographs. However, both types of radiography are affected by head position or beam angulation [3]. The use of PR for measurements is controversial because of the magnification and distortion; however, many studies support the use of PR to detect mandibular asymmetry as a result of such advantages as low cost and being a standard procedure that exposes the patient to a relatively low dose of radiation [13, 17]. In addition, if the patient is positioned properly, angular and vertical measurements may be accurately performed using PR [18]. On the other hand, for PACR, while head position changes have a small effect on vertical measurements, they have a greater effect on horizontal measurements in the vertical plane [23]. The patient’s head position in which the Frankfort plane is parallel to the ground and the patient looks directly forward or slightly downward is considered to be the appropriate position for PACR [24]. It is difficult to determine anatomical landmarks in PACR because of the superposition of other structures [25, 26]. Thus, it is recommended to repeat the analysis in order to reduce the errors in detection and measurement of the landmarks in the cephalometric measurements [27]. In the current study, all measurements were repeated in 30 patients for both radiographic techniques, and the correlation coefficient was found to be high.
The literature includes studies wherein the AI formula is used in PACR [10, 11]. While Almasan et al. [10] adapted the formula to PACR in temporomandibular joint disorder patients in 2013, Alkis and Bilge [11] adapted this formula to PACR in Angle malocclusion samples in 2019. However, to our knowledge there is no study showing comparison of the AI with digital PR images and PACR images. In the current study, AI values did not show a significant difference between PR and PACR images. On the other hand, while the presence of condylar and ramus asymmetry was found to be compatible in PR and PACR, the two radiographic techniques were not compatible with each other for total asymmetry. This can be explained by the fact that more anatomical structures are superposed on the mandible in PACR than in PR and this situation may have resulted in the observer’s incorrect assessment of the condyle apex when CH + RH measurements were performed. In addition, the AI formula basically has been developed to evaluate condylar and ramus asymmetries [9] and has been applied to different anatomical points by different authors [2, 12, 13, 17,18,19,20,21].
One of the limitations of this study is that measurements were made on conventional radiographic images. Disadvantages of conventional radiographs include superposition of anatomical structures and distortion and magnification in radiographs. However, if the patient is accurately positioned, vertical measurements may be accurately performed. In the present study, radiographic images that were thought to be distorted and in which the anatomical structures to be used for measurements were not clearly visible were excluded from the study.
The AI values obtained from the two radiographic methods were compared and found to be compatible with each other in the current study; however, this could not be compared with clinical data, since the study was conducted only radiologically and retrospectively. This may be another limitation of the study. But this cannot be translated unreservedly to the clinical situation. More general and accurate results could be obtained by comparison with the information obtained from extraoral facial photographs of the patients. Despite all these limitations, the current study is the first to compare the AI formula in two radiographic methods.
Conclusion
Although the condylar height (CH), ramus height (RH), and CH + RH measurements on the right and left sides in panoramic radiographs (PR) and posteroanterior cephalometric radiographs (PACR) showed statistically significant differences, AI values did not show a significant difference between PR and PACR images when the measurement values were placed in the AI formula. From the results of this study, it can be concluded that the AI can be used for both diagnostic PR and PACR radiographic techniques. Both types of radiographic images can be used to determine asymmetry before orthodontic treatment and comparisons can be made with images after orthodontic treatment.
References
Anistoroaei D, Golovcencu L, Saveanu IC, Zegan G (2014) The prevalence of facial asymmetry in preorthodontic treatment. Int J Med Dent 18(3):210–215
Sezgin OS, Celenk P, Arici S (2007) Mandibular asymmetry in different occlusion patterns. Angle Orthod 77(5):803–807
Agrawal A, Bagga DK, Agrawal P, Bhutani RK (2015) An evaluation of panoramic radiograph to assess mandibular asymmetry as compared to posteroanterior cephalogram. APOS Trends Orthod 5(5):197–201
Ramirez-Yanez GO, Stewart A, Franken E, Campos K (2011) Prevalence of mandibular asymmetries in growing patients. Eur J Orthod 33(3):236–242
Rose JM, Sadowsky C, BeGole EA, Moles R (1994) Mandibular skeletal and dental asymmetry in class II subdivision malocclusions. Am J Orthod Dentofacial Orthop 105(5):489–495
Westesson PL, Tallents RH, Katzberg RW, Guay JA (1994) Radiographic assessment of asymmetry of the mandible. Ajnr Am J Neuroradiol 15(5):991–999
Vitral RW, Telles Cde S (2002) Computed tomography evaluation of temporomandibular joint alterations in class II division 1 subdivision patients: condylar symmetry. Am J Orthod Dentofacial Orthop 121(4):369–375
Huang M, Hu Y, Yu J, Sun J, Ming Y, Zheng L (2017) Cone-beam computed tomographic evaluation of the temporomandibular joint and dental characteristics of patients with class II subdivision malocclusion and asymmetry. Korean J Orthod 47(5):277–288
Habets LL, Bezuur JN, Naeiji M, Hansson TL (1988) The orthopantomogram, an aid in diagnosis of temporomandibular joint problems. II. The vertical symmetry. J Oral Rehabil 15(5):465–471
Almasan OC, Baciut M, Hedesiu M, Bran S, Almasan H, Baciut G (2013) Posteroanterior cephalometric changes in subjects with temporomandibular joint disorders. Dentomaxillofac Radiol 42(1):20120039
Alkis HT, Bilge OM (2019) Evaluation of mandibular asymmetry in angle malocclusion samples by posterioanterior cephalometric radiography: a preliminary study. Niger J Clin Pract 22(6):771–776
Kiki A, Kilic N, Oktay H (2007) Condylar asymmetry in bilateral posterior crossbite patients. Angle Orthod 77(1):77–81
Kurt G, Uysal T, Sisman Y, Ramoglu SI (2008) Mandibular asymmetry in class II subdivision malocclusion. Angle Orthod 78(1):32–37
Kjellberg H, Ekestubbe A, Kiliaridis S, Thilander B (1994) Condylar height on panoramic radiographs. A methodologic study with a clinical application. Acta Odontol Scand 52(1):43–50
Habets LL, Bezuur JN, van Ooij CP, Hansson TL (1987) The orthopantomogram, an aid in diagnosis of temporomandibular joint problems. I. The factor of vertical magnification. J Oral Rehabil 14(5):475–480
Iturriaga V, Navarro P, Cantin M, Fuentes R (2012) Prevalence of vertical condilar asymmetry of the temporomandibular joint in patients with signs and symptoms of temporomandibular disorder. Int J Morphol 30(1):315–321
Uysal T, Sisman Y, Kurt G, Ramoglu SI (2009) Condylar and ramal vertical asymmetry in unilateral and bilateral posterior crossbite patients and a normal occlusion sample. Am J Orthod Dentofacial Orthop 136(1):37–43
Kasimoglu Y, Tuna EB, Rahimi B, Marsan G, Gencay K (2015) Condylar asymmetry in different occlusion types. Cranio 33(1):10–14
Silvestrini-Biavati F, Ugolini A, Laffi N, Canevello C, Silvestrini-Biavati A (2014) Early diagnostic evaluation of mandibular symmetry using orthopantomogram. Indian J Dent Res 25(2):154–159
Kilic N, Kiki A, Oktay H (2008) Condylar asymmetry in unilateral posterior crossbite patients. Am J Orthod Dentofacial Orthop 133(3):382–387
Al Taki A, Ahmed MH, Ghani HA, Al Kaddah F (2015) Impact of different malocclusion types on the vertical mandibular asymmetry in young adult sample. Eur J Dent 9(3):373–377
Trpkova B, Prasad NG, Lam EW, Raboud D, Glover KE, Major PW (2003) Assessment of facial asymmetries from posteroanterior cephalograms: validity of reference lines. Am J Orthod Dentofacial Orthop 123(5):512–520
Eliasson S, Welander U, Ahlqvist J (1982) The cephalographic projection. Part I: general considerations. Dentomaxillofac Radiol 11(2):117–122
Grummons DC, Kappeyne van de Coppello MA (1987) A frontal asymmetry analysis. J Clin Orthod 21(7):448–465
Major PW, Johnson DE, Hesse KL, Glover KE (1994) Landmark identification error in posterior anterior cephalometrics. Angle Orthod 64(6):447–454
Leonardi R, Annunziata A, Caltabiano M (2008) Landmark identification error in posteroanterior cephalometric radiography. A systematic review. Angle Orthod 78(4):761–765
Houston WJ (1983) The analysis of errors in orthodontic measurements. Am J Orthod 83(5):382–390
Acknowledgements
Statistical analysis of this study was carried out by the Akdeniz University Statistical Consulting, Application and Research Center.
Funding
This study was not supported by any source of funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H.T. Alkis and K.A. Pekince declare that they have no competing interests.
Ethical standards
This study was approved by the Clinical Research Ethics Committee of the Faculty of Medicine Akdeniz University, and the study was carried out in accordance with the ethical rules of the Declaration of Helsinki (ethics approval number 70904504/90). Consent to participate: Due to retrospective study design and the anonymization of the patients’ data, written informed consent was not necessary.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alkis, H.T., Pekince, K.A. Comparison of the asymmetry index determined on digital panoramic radiographic images and on posteroanterior cephalometric images: a retrospective cross-sectional study. J Orofac Orthop 84 (Suppl 3), 244–250 (2023). https://doi.org/10.1007/s00056-022-00442-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00056-022-00442-2