Abstract
Purpose
The aim of this retrospective study was to evaluate the effects of functional orthopedic treatment on mandibular bone structure using fractal dimension (FD) analysis of panoramic radiographs.
Methods
The study material consisted of the pre- and posttreatment digital panoramic radiographs of 80 patients (mean age 10.1 ± 2.01 years; 45 girls, 35 boys) with class II malocclusion who were treated with the monoblock or twin block appliances. The following regions of interest (ROI) were selected: ROI1, condylar process; ROI2, angulus mandibulae; ROI3, corpus mandibulae; and ROI4, mental foramen. Pre- and posttreatment FD values were compared for each ROI.
Results
FD values of the mandibular condyle did not change with the functional orthodontic treatment. FD values of the mandibular corpus region had the highest pretreatment values and significantly decreased with treatment (p < 0.05).
Conclusion
Functional orthopedic treatment altered the trabeculation of the mandibular bone, but it is speculated that the changes in the occlusal forces seemed to be of primary significance for this effect.
Zusammenfassung
Zielsetzung
Ziel dieser retrospektiven Studie war es, die Auswirkungen einer funktionellen kieferorthopädischen Behandlung auf die Knochenstruktur des Unterkiefers anhand der Analyse der fraktalen Dimension (FD) von Panoramaröntgenaufnahmen zu untersuchen.
Methoden
Das Material für die Studie bestand aus den digitalen Panoramabildern vor und nach der Behandlung von 80 Patienten (Durchschnittsalter 10,1 ± 2,01 Jahre; 45 Mädchen, 35 Jungen) mit Klasse-II-Malokklusion, die mit Monoblock- bzw. Twin-Block-Geräten behandelt worden waren. Als ROI („regions of interest“) wurden ausgewählt: ROI1, Kondylenfortsatz; ROI2, Angulus mandibulae; ROI3, Corpus mandibulae; und ROI4, Foramen mentale. Die FD-Werte vor und nach der Behandlung wurden für jede ROI verglichen.
Ergebnisse
Die FD-Werte der Unterkieferkondylen änderten sich durch die funktionskieferorthopädische Behandlung nicht. Die FD-Werte im Bereich des Unterkieferkorpus wiesen die höchsten Werte vor der Behandlung auf und nahmen mit der Behandlung signifikant ab (p < 0,05).
Schlussfolgerung
Die funktionskieferorthopädische Behandlung veränderte die Trabekulierung des Unterkieferknochens, doch es wird vermutet, dass die Veränderungen der Okklusionskräfte für diesen Effekt von primärer Bedeutung zu sein scheinen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The concept of fractals was used for the first time in the 1960s and 1970s to describe complex structures whose morphology and size cannot be determined [1]. Fractals are structures that cannot be defined using shapes such as triangles, squares or circles in classical geometry, but are similar to each other. Mathematical fractals are isotropic fractals that exhibit similar properties when examined at different scales. Natural and biological fractals, such as pulmonary branching lungs and trabecular bone, are anisotropic and exhibit different properties under different observation conditions. Biological fractals show self-similarity only on a limited scale [2, 3]. Fractal analysis is a method that expresses the degree of complexity of structures with fractal dimensions [4]. The fractal analysis method is used to obtain information about the severity and progress of a current disease or to diagnose a potential disease, especially in the field of medicine, since it is not affected by projection geometry and radiodensity, and is an easily accessible and noninvasive method. It has been stated that the fractal dimension (FD) detected on radiographs reflects the changes in trabecular bone density and bone mineral loss [3, 5, 6]. Low FDs indicate that there are many spaces within the mineralized bone and that it is more porous, while high FDs indicate that the bone structure is denser and hollower [7]. It has been concluded that the anisotropic property of trabecular bone and variations in trabecular alignment and trabecular thickness lead to differing results on FD analysis [8]. Based on the ability of the fractal analysis method to detect changes in the trabecular bone-rich structure of the mandibula and the maxilla, studies have been conducted in various fields using fractal analysis in dentistry. These studies included the evaluation of apical lesions after endodontic therapy [9], the examination of the effects of periodontal diseases on alveolar bone [10], the examination of recovery after implant surgery [11], the examination of temporomandibular joint disorders [12] and the examination of pathologies associated with osteoporosis [13]. The mandibular bone structure has also been evaluated using fractal analysis in different conditions such as bruxism and lactation [14, 15].
Class II malocclusions are frequently encountered anomalies in orthodontic practice and affect approximately 30% of the population [16]. The etiology of class II malocclusion is multifactorial. It is known to be caused by genetic or environmental factors, or a combination of both [17]. The treatment of patients with skeletal class II division 1 malocclusion, who are in the peak growth-development period and have mandibular retrognathia, is achieved by allowing forward growth of the mandibula using various appliances. This treatment type is called functional orthopedic therapy [18]. According to Wolf’s theory, which is also related to functional therapy, functional stimuli are transmitted directly or indirectly to the jawbones and trigger resorption–apposition events. Creating these changes in the microstructure of the bone causes overall morphological changes [19].
There are a few studies in the literature that evaluated the trabecular bone changes related to different orthodontic treatments [20, 22]. Wagle et al. [21] found that mechanical loading led to an increase in FD at the periodontal ligament–bone interface in their experimental animal study. However, Kang et al. [22] concluded that bone density decreased after the combination of orthodontic treatment and orthognathic surgery. Although functional appliances have been frequently used in orthodontic clinical practice for many years, there is still no consensus on how they affect bone structure. The aim of the present study was to determine the effects of the forces caused by functional orthopedic treatment on the mandibular trabecular structure using the fractal dimension analysis method on pre- and posttreatment digital panoramic radiographs of growing class II patients. The results of the present study may present a new perspective on clarifying the effects of functional orthopedic treatment.
Materials and methods
This retrospective study was approved by the ethics committee of the Akdeniz University Faculty of Medicine (Approval Date and No.: 08 July 2020, 508). The study material was selected from the archives of the Akdeniz University Faculty of Dentistry, Department of Orthodontics.
The G*Power 3.1.9 [23] software package was used to determine the adequate sample size for the study. The minimum sample size to be included in the study for 80% power was calculated as 44. Therefore, pre- and posttreatment digital lateral cephalometric and panoramic radiographs of 80 patients (mean age 10.1 ± 2.01 years; 45 girls, 35 boys) whose orthodontic treatment was completed between years 2018 and 2020 and who met the following inclusion criteria were included in the study. The patients’ numbers at every stage of the study are shown in Fig. 1 as a flow chart.
-
Pre- and posttreatment radiographs and records are fully available,
-
Pretreatment skeletal and dental class II malocclusion due to mandibular retrognathia (ANB ≥ 4°, Wits appraisal ≥ 1 mm and SNB ≤ 80°; pretreatment dental casts were used for the determination of dental relationships),
-
Being treated with functional orthopedic appliances (twin block or monoblock),
-
Being at peak pubertal growth period at the beginning of treatment (hand–wrist stage S and MP3cap),
-
Good cooperation during treatment (clinic records were evaluated), and
-
Angle class I dental occlusion after treatment (posttreatment dental casts were evaluated).
Radiographs of individuals with craniofacial anomaly, hereditary disease, dentoalveolar pathology, mandibular asymmetry, temporomandibular joint disorders, history of trauma and/or any systemic disease affecting the bone structure (patient records were evaluated); radiographs with poor image quality, or ghost images that would prevent image analysis were excluded from the study.
The present study was conducted and approved by the ethics committee as a retrospective study and the study material that includes hand–wrist radiographs of the patients was selected from the archive records.
All lateral cephalometric radiographic images were obtained with the same device (Planmeca 2002CCProline Pan/Ceph X‑Ray, Helsinki, Finland) in accordance with the manufacturer’s instructions (66 kVp, 5 mA and 18 s). Dental panoramic radiographs (DPRs) were obtained using the same Planmeca ProMax panoramic devices (Planmeca Oy, 00880 Helsinki, Finland) in accordance with the manufacturer’s instructions (66 kVp, 7 mA and 16 s), by the same X‑ray technician in a standardized manner. The Frankfurt horizontal plane was parallel to the floor and the vertical plane produced by the device was aligned with the sagittal plane.
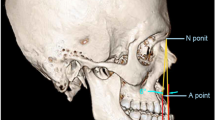
Dental and skeletal measurements were performed by the same orthodontist (C.T.) using the same image analysis program (Dolphin Imaging Software, version 8.0, Los Angeles, CA, USA) on pre- and posttreatment lateral cephalometric radiographs (Fig. 2).
Cephalometric measurements. Skeletal angular measurements (°): (1) SNA; (2) SNB; (3) ANB; (4) Wits appraisal measurement; (5) Pog-NB; (6) SN/GoGn; skeletal linear measurements (mm): (7) Go-Me; (8) Co-Go; (9) Co-Gn; dental angular measurements (°): (10) IMPA. S sella, N nasion, Co condylon, A point A, B point B, Go gonion, Me Menton, Pg Pogonion
Kephalometrische Messungen. Skelettale Winkelmessungen (°): (1) SNA; (2) SNB; (3) ANB; (4) Wits appraisal; (5) Pog-NB; (6) SN/GoGn; lineare skelettale Maße (m): (7) Go-Me; (8) Co-Go; (9) Co-Gn; dentale Winkelmaße (°): (10) IMPA. S Sella, N Nasion, Co Condylon, A Punkt A, B Punkt B, Go Gonion, Me Menton, Pg Pogonion
Pre- and posttreatment DPRs were used for the FD analysis of the mandibular bones of the patients treated with functional orthopedic appliances. DPRs in TIFF format were transferred to the Image J analysis program (Image J, 1.3 V Version, National Institutes of Health, Bethesda, MD, USA) for fractal size calculation. FD analysis of each sample was performed using the method suggested by White and Rudolph, and fractal size was calculated by the box counting method [24]. All DPRs were evaluated using the same LED monitor by the same investigator (E.Y.). Evaluation was made in a dimly lit room approximately 30–40 cm away from the LED monitor and tonal adjustments were made on images to maximize the view. Only ten DPRs were evaluated per day in order to prevent investigator fatigue. The observer was blinded to the clinical status of patients during the analysis of the radiographic images.
Measurements were made on four regions of interest (ROI) determined on the right side of the mandible on each digital panoramic radiograph (Fig. 3):
-
ROI 1: Condylar process, the subcortical area of the mandibular condyle,
-
ROI 2: Angulus mandibulae, above the supracortical area in the angulus mandibulae,
-
ROI 3: Corpus mandibulae, above the mandibular canal, distal to the second premolar tooth, and
-
ROI 4: Mental foramen, anterior side of the mental foramen.
FD analysis was performed on a total of 640 ROIs of the pre- and posttreatment panoramic radiographs of 80 patients.
While determining ROIs, only trabecular bone was included, and dental tissue, lamina dura, periodontal ligament and cortical bone were avoided. The operation was carried out sequentially as follows (Fig. 4):
-
1.
Regions of interest were determined by measuring by hand in a square shape, consisting of 64 × 64 pixels.
-
2.
The designated region of interest was cut.
-
3.
The cut region of interest was copied.
-
4.
The image was blurred with a Gaussian filter to eliminate small and medium density differences in the copy.
-
5.
The new image created was subtracted from the original image.
-
6.
Bone marrow voids and trabeculae were separated by adding 128 shades of grey to each pixel location.
-
7.
The image was binarized (black, white) by applying a 128 brightness threshold process to the image obtained. Bone marrow cavities and trabeculae were outlined.
-
8.
Erode and dilatation processes were applied to eliminate the noise in the obtained image. Thus, the structures in the image were made more visible.
-
9.
In the last step, inversion and “skeletonize” were applied to the image in order to apply fractal analysis. Thus, the outline of the skeletal trabecular structure was determined on the binary image obtained. The skeletal structure on the binary image (black) represented the bone pattern and the extra-skeletal area of the binary image (white) represented the bone and its cavity.
Fractal analysis process: a crop; b duplicate; c blurred image of the duplicated region of interest; d subtracted blurred image from the original image; e addition of 128 Gy values; f binarization; g erosion; h dilatation; i inversion; j skeletonization
Verfahren der Fraktalanalyse: a Ausschneiden; b Duplizieren; c unscharfes Bild der duplizierten ROI („region of interest“); d vom Originalbild subtrahiertes Originalbild; e Addition von 128-Gy-Werten; f Binarisierung; g Erosion; h Dilatation; i Inversion; j Skelettierung
For fractal dimension measurement, the fractal box counting method under the analysis tab was used. With this technique, the image was divided into squares with dimensions of 2, 3, 4, 6, 8, 12, 16, 32, and 64 pixels for measurement. The frames representing the trabeculae and the frames in the total image were calculated for pixels of each different size. These values were plotted on a logarithmic scale and the line of best fit was plotted. As a result, the fractal dimension of the trabecular structure of the ROIs was calculated from the slope of the line.
After 2 weeks, cephalometric measurements, dental (class I/II occlusion) and FD analysis of randomly selected 20% of the patients were repeated in order to permit calculation of the intraobserver reliability which was assessed by using the intraclass correlation coefficient (ICC), with a confidence interval (CI) of 95%.
Statistical analysis
Data obtained in the study were statistically analyzed using the IBM SPSS 23.0 package (IBM Corp., Armonk, NY, USA). Descriptive statistics were presented as mean ± standard deviation (SD) and median (min–max) values. The Shapiro–Wilk test was used for the analysis of normality. The Mann–Whitney U test and student’s t‑test were used for the analysis of nonnormally and normally distributed numerical data, respectively. For the analysis of the difference between pre- and posttreatment measurements, the paired samples t‑test was performed when the assumption of normal distribution was met, and the Wilcoxon signed rank test and Friedman test were performed otherwise. Spearman’s correlation test was used for relationships between ordinal or continuous variables that did not conform to the normal distribution, and Pearson’s correlation test was used for normally distributed variables. P-values less than 0.05 were considered statistically significant.
Results
The ICC calculations for the measurements indicated excellent reliability (p < 0.05).
The mean and standard deviations of the chronological ages, treatment durations and gender distributions of the patients are presented in Table 1. Pre- and posttreatment radiographic images of 45 girls and 35 boys were included in the study. The mean age of the patients was 10.1 ± 2.01 years (min 6.33, max 15.83) and average treatment times were calculated to be 11.28 ± 3.34 months (min 6.3, max 22.2).
Cephalometric measurements
Pre- and posttreatment cephalometric measurements and their comparisons are shown in Table 2. Analysis of cephalometric measurements from pre- and posttreatment revealed a significant increase in SNB, Co-Gn, Co-Go, Go-Me, and incisor mandibular plane angle (IMPA) values (p < 0.001). Pog-NB, ANB, and Wits appraisal measurements were significantly decreased after functional orthopedic treatment (p < 0.005, p < 0.001, and p < 0.001, respectively). Although an increase was observed for the mean SN-GoGn values of the patients after treatment, this difference was not statistically significant (p = 0.070).
Fractal dimension analysis
The FD analysis of the ROIs of the pre- and posttreatment panoramic radiographs and their comparisons are shown in Table 3. When the pre- and posttreatment FD analysis values were evaluated separately, it was determined that ROI 3 (corpus mandibulae) presented the highest pre- and posttreatment values and ROI 2 (angulus mandibulae) the lowest pre- and posttreatment values (p < 0.001). Analysis of the changes of the FD values between the pre- and posttreatment radiographs revealed a statistically significant decrease in FD values of ROI 3 (corpus mandibulae; p = 0.048) and a significant increase of the FD values of ROI 4 (mental foramen; p = 0.005). Pre- and posttreatment FD values of ROI 1 (condylar process) were found not to be significantly different (p = 0.140). A decrease of the FD values of ROI 2 (angulus mandibulae) was observed between the pre- and posttreatment radiographs; however, this difference was not statistically significant (p = 0.081).
The pre- and posttreatment FD values and their changes were also evaluated for both genders separately. Pre- and posttreatment FD values of ROIs 1, 2, 3, and 4 did not show any significant difference according to gender (p > 0.05). A statistically significant decrease was observed for the fractal dimensions obtained from ROI 2 in girls (p = 0.036) and the FD obtained from ROI 3 in boys (p = 0.861) after treatment. While a statistically significant increase was determined in the FD obtained from ROI 4 in girls after treatment (p = 0.019), the increase in boys was not significant (p = 0.129; Table 4).
The differences in FD measurements of ROI 1 (p = 0.873), ROI 2 (p = 0.185) and ROI 4 (p = 0.486) after functional treatment were found not to be significantly different according to gender. It was observed that the decrease in FD measured in ROI 3 after functional treatment was significantly more pronounced in boys than in girls (p = 0.038; Table 5).
Table 6 presents the correlation analysis between the cephalometric and the FD measurements. Pretreatment FD measurements of ROI 2 were positively correlated with the SNA and SNB value (p = 0.002 and p = 0.007, respectively) and posttreatment FD measurements of ROI 2 were positively correlated with the value for the ANB (p = 0.035). Posttreatment FD measurements of ROI 3 were negatively correlated with the SNA value (p = 0.044) and positively correlated with that for the SNB and the SN-GoGn (p = 0.049 and p = 0.048, respectively). In addition, a positive correlation between the FD measurements of ROI 4 and the value for Go-Me was found (p = 0.023).
Discussion
Although functional therapy has been used for many years, there is still no consensus regarding its effectiveness on craniofacial structures. It has been reported that functional therapy induces mandibular growth by increasing the cell activity and remodeling of the mandibular condyle [25] and that these changes in the microstructure of the bone created by the functional stimulus can cause morphological changes [19]. On the contrary, some researchers claim that the main effect of functional treatment is on the dentoalveolar region and that it has little effect on bony structures [26, 27]. Since the trabecular bone has higher metabolic activity than the cortical bone, it has been reported to be more decisive in the evaluation of changes in the bone structure [28]. In the present study, FD analysis was used to evaluate mandibular trabecular bone changes in panoramic radiographs of patients treated with functional appliances in order to create a new perspective on the effects of functional treatment.
FD analysis has been suggested as a useful non-invasive method for detecting various diseases or conditions that affect the trabecular bone structure [29]. In the literature, a generally increased complexity of bone structure was associated with an increase in its FD, while low FD values were associated with a simpler internal order [15]. Especially in dental research, studies have indicated that FD analysis by the box counting method can successfully be used as a diagnostic tool for trabecular changes in the mandible of patients [15, 30, 31]. Panoramic radiographs were utilized for the measurements of FD in the present study to evaluate the chosen ROIs (condylar process, angulus, and corpus mandibula) because of their sufficiency to show the trabecular pattern [15]. Since no significant difference was found between the ROIs selected from the same region on the right and left sides of individuals in previous studies [15], the FD measurements were obtained from the right side of all samples in the present study. Not using an average value for the right and left side measurements and not comparing the right and left side FD values may be a limitation for the current study. However, exclusion of patients with conditions such as mandibular asymmetry and temporomandibular disorders that can affect the development of the right or left sides of the mandibular bone may reduce the negative effects of this limitation.
The effects of the monoblock and twin block on mandibular growth, which are the most commonly used functional appliances in the treatment of skeletal class II malocclusions, have been found to be similar [32]. Therefore, the patients treated with either monoblock or twin block appliances were included in the current study and were not evaluated separately. Pretreatment hand–wrist radiographs of all patients were also considered and patients who were at or just entering peak pubertal growth were selected.
A possible relationship between the gender and the FD values of mandibular bone was also evaluated in the present study, but pretreatment FD values did not show any significant difference by gender (Table 4). Similar to the present study, Updike et al. [10] investigated the effects of chronic periodontitis on FD, indicating that there was no correlation between the FD and gender. The results of a study that evaluated anatomical variations of trabecular bone with different techniques were also similar [33]. On the contrary, some researchers found lower FD values in women and attributed this finding to a more porous structure of trabecular bone in women, and more complex trabecular structures and higher trabeculation in men [12, 15]. The studies that indicated gender differences in FD values may have been able to do so due to larger sample sizes [15]. The differences in sample size and inequality in the distribution of females and males or different age distributions of the study groups may be responsible for these controversial results.
When the pretreatment FD values of all individuals were examined, it was observed that the mandibular corpus (ROI 3) demonstrated the highest FD values (Table 3). As mentioned previously, higher FD values were associated with more trabecular complexity [23]. This ROI was located in the region of the posterior teeth and the higher values of the FD may be due to the necessity to resist higher occlusal forces [15]. Another significant result of the present study was the decrease in the FD values of the mandibular corpus region after functional appliance usage (Table 3). The decrease of occlusal forces on the posterior teeth during functional treatment due to the design of the posterior acrylic of the appliances may be one of the reasons for this result [31]. Reducing the acrylic of the posterior region of the appliances to improve the occlusal relationship with the eruption of molar teeth may be another factor which may have been responsible for the decrease of the FD values associated with the decrease in the trabecular complexity in this ROI.
The lowest FD values were obtained in the angulus mandibulae region (ROI 2, Table 3) and there were no significant differences between the pre- and posttreatment FD values for ROI 2 (Table 3) in the present study. It is also noteworthy that the angulus mandibulae was the ROI furthest from the teeth and occlusal forces that may affect the trabecular structure.
The cephalometric findings of the study demonstrated that mandibular advancement was obtained and mandibular length increased with functional appliance usage in the growing class II patients (Table 2). The adaptive changes in the mandibular condyle, especially in the posterior and posterosuperior region, in response to the protrusive functional position of the mandibulae have previously been demonstrated [34]. Although it was reported that the remodeling activities of the mandibular condyle due to functional stimuli are primarily responsible for the increase in mandibular length [25], the pre- and posttreatment FD values of the condylar region did not show any significant difference in the present study, indicating that the pre- and posttreatment trabecular structures of the condyles were similar. Gulec et al. [15] investigated the bilateral mandibular trabecular bone changes using FD analysis in patients with bruxism and found significantly lower FD values for only the right mandibular condyle. The authors concluded that lower FD values might be related to resorptive changes in the condylar region caused by bruxism-associated nonfunctional occlusal forces [15]. However, significant results were only seen on the right side and the authors suggested that this difference may be due to possible unilateral mastication habits. Similarly, Arsan et al. [12] reported that the FD values of the mandibular condyles of patients with temporomandibular disorders such as disc displacements with or without reduction showed lower FD values compared to the control group. They also stated that the FD values of the condyles decreased when more erosive and sclerotic changes were present. According to the results of the current study, functional orthopedic forces did not change the trabecular structure of the mandibular condyle. In this case, it can be concluded that nonfunctional occlusal forces and temporomandibular disorders are more effective on the trabecular structure of the mandibular condyle compared to the functional orthopedic forces occurring during functional orthopedic treatment.
Wagle et al. [21], who investigated the FD of the periodontal ligament–bone interface during orthodontic tooth movement in rats, reported that mechanical loading changed the FD values proportional to the magnitude of the force and the FD response varied between the apical, middle, and cervical thirds of the teeth. In line with this, the FD of sutures has been previously shown to be associated with the local stress pattern [35]. These findings further suggest that FD changes are generally caused by local mechanical factors; in other words, mechanical loading or orthodontic force application seems to be more effective on local FD values.
In addition to the skeletal effects, functional orthopedic appliances also have dentoalveolar effects such as protrusion of mandibular incisors, and eruption and mesial movement of mandibular posterior teeth [19]. The cephalometric findings of the current study also presented these dentoalveolar effects. The anterior side of the mental foramen (ROI 4) was the most mesial ROI of the present study, located in the toothed region. The significant increase in the FD values of ROI 4 (Table 3) can be explained by dental movements resulting from the functional orthopedic forces.
Although FD analysis is accepted as an effective method for evaluating trabecular bone changes in the dental literature, it has some limitations. The use of different methods for calculating the FD makes it difficult to compare the results of different studies effectively [35]. This is supported by the fact that different studies on the FD of normal maxillary bone demonstrated different normal values [7]. The lack of optimal FD reference values for different ROIs calculated with a single method can be considered a limitation. Therefore, comparing the FD values with the values obtained from a specific reference point or an untreated control group may provide more accurate results instead of comparing individuals as has been done in the present study. Since there was no untreated control group, it was also not possible to definitively ascribe the FD changes to the appliance usage in the present study, as growth could also have influenced these variables. This was also a limitation of the present study.
Conclusions
-
Mandibular advancement was obtained and mandibular length increased with functional appliance treatment in growing class II patients.
-
Functional orthopedic forces did not change the fractal dimension (FD) values in the region of the mandibular condyle, but significant changes were observed in the FD values of the mandibular corpus region.
-
Results of the present study indicate that changes in the occlusal forces and local force applications may be more effective influencing the FD values of mandibular trabecular structure.
-
Functional orthopedic appliance treatment was an effective method for the correction of skeletal class II malocclusions, but its effect on the mandibular trabecular structure was not clearly without ambiguity.
References
Geraets WG, Van Der Stelt PF (2000) Fractal properties of bone. Dentomaxillofac Radiol 29(3):144–153. https://doi.org/10.1038/sj/dmfr/4600524
Sánchez I, Uzcátegui G (2011) Fractals in dentistry. J Dent 39(4):273–292. https://doi.org/10.1016/j.jdent.2011.01.010
Demirbaş AK, Ergün S, Güneri P, Aktener BO, Boyacıoğlu H (2008) Mandibular bone changes in sickle cell anemia: fractal analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106(1):e41–e48. https://doi.org/10.1016/j.tripleo.2008.03.007
Yasar F, Akgunlu F (2005) Fractal dimension and lacunarity analysis of dental radiographs. Dentomaxillofac Radiol 34(5):261–267. https://doi.org/10.1259/dmfr/85149245
Bollen AM, Taguchi A, Hujoel PP, Hollender LG (2001) Fractal dimension on dental radiographs. Dentomaxillofac Radiol 30(5):270–275. https://doi.org/10.1038/sj/dmfr/4600630
Ergün S, Saraçoglu A, Güneri P, Ozpınar B (2009) Application of fractal analysis in hyperparathyroidism. Dentomaxillofac Radiol 38(5):281–288. https://doi.org/10.1259/dmfr/24986192
Southard TE, Southard KA, Jakobsen JR, Hillis SL, Najim CA (1996) Fractal dimension in radiographic analysis of alveolar process bone. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 82(5):569–576. https://doi.org/10.1016/s1079-2104(96)80205-8
Shrout MK, Potter BJ, Hildebolt CF (1997) The effect of image variations on fractal dimension calculations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 84(1):96–100. https://doi.org/10.1016/s1079-2104(97)90303-6
Huang CC, Chen JC, Chang YC, Jeng JH, Chen CM (2013) A fractal dimensional approach to successful evaluation of apical healing. Int Endod J 46(6):523–529. https://doi.org/10.1111/iej.12020
Updike SX, Nowzari H (2008) Fractal analysis of dental radiographs to detect periodontitis-induced trabecular changes. J Periodontal Res 43(6):658–664. https://doi.org/10.1111/j.1600-0765.2007.01056.x
Sansare K, Singh D, Karjodkar F (2012) Changes in the fractal dimension on pre-and post-implant panoramic radiographs. Oral Radiol 28(1):15–23. https://doi.org/10.1007/s11282-011-0075-8
Arsan B, Köse TE, Çene E, Özcan İ (2017) Assessment of the trabecular structure of mandibular condyles in patients with temporomandibular disorders using fractal analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 123(3):382–391. https://doi.org/10.1016/j.oooo.2016.11.005
Yasar F, Akgunlu F (2006) The differences in panoramic mandibular indices and fractal dimension between patients with and without spinal osteoporosis. Dentomaxillofac Radiol 35(1):1–9. https://doi.org/10.1259/dmfr/97652136
Coşgunarslan A, Canger EM, Soydan Çabuk D, Kış HC (2020) The evaluation of the mandibular bone structure changes related to lactation with fractal analysis. Oral Radiol 36(3):238–247. https://doi.org/10.1007/s11282-019-00400-6
Gulec M, Tassoker M, Ozcan S, Orhan K (2020) Evaluation of the mandibular trabecular bone in patients with bruxism using fractal analysis. Oral Radiol 37(1):36–45. https://doi.org/10.1007/s11282-020-00422-5
Gelgor IE, Karaman AI, Ercan E (2007) Prevalence of malocclusion among adolescents in central anatolia. Eur J Dent 1:125–131
Mossey PA (1999) The heritability of malocclusion: part 2. The influence of genetics in malocclusion. Br J Orthod 26(3):195–203. https://doi.org/10.1093/ortho/26.3.195
Dolce C, McGorray SP, Brazeau L, King GJ, Wheeler TT (2007) Timing of Class II treatment: skeletal changes comparing 1‑phase and 2‑phase treatment. Am J Orthod Dentofacial Orthop 132(4):481–489. https://doi.org/10.1016/j.ajodo.2005.08.046
Rakosi TR, Graber TM, Petrovic AG (1985) Dentofacial orthopedics with functional appliances. Mosby, St Louis
Ahmad S, Kamble RH, Shrivastav S, Sharma N, Patil R, Goyal A (2015) Assesment of bony trabecular patternchanges seen in growing skeletal Class II malocclusion treated with twin block therapy. Int J Cur Res Rev 7(21):59–65
Wagle N, Do NN, Yu J, Borke JL (2005) Fractal analysis of the PDL-bone interface and implications for orthodontic tooth movement. Am J Orthod Dentofacial Orthop 127(6):655–661. https://doi.org/10.1016/j.ajodo.2004.02.022
Kang HJ, Jeong SW, Jo BH, Kim YD, Kim SS (2012) Observation of trabecular changes of the mandible after orthognathic surgery using fractal analysis. J Korean Assoc Oral Maxillofac Surg 38(2):96–100. https://doi.org/10.5125/jkaoms.2012.38.2.96
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav Res Methods 41(4):1149–1160. https://doi.org/10.3758/BRM.41.4.1149
White SC, Rudolph DJ (1999) Alterations of the trabecular pattern of the jaws in patients with osteoporosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 88(5):628–635. https://doi.org/10.1016/s1079-2104(99)70097-1
McNamara JA Jr, Bryan FA (1987) Long-term mandibular adaptations to protrusive function: an experimental study in Macaca mulatta. Am J Orthod Dentofacial Orthop 92(2):98–108. https://doi.org/10.1016/0889-5406(87)90364-7
Hirzel HC, Grewe JM (1974) Activators: a practical approach. Am J Orthod 66(5):557–570. https://doi.org/10.1016/0002-9416(74)90114-6
Tulley WJ (1972) The scope and limitations of treatment with the activator. Am J Orthod 61(6):562–577. https://doi.org/10.1016/0002-9416(72)90107-8
Shrout MK, Farley BA, Patt SM, Potter BJ, Hildebolt CF, Pilgram TK et al (1999) The effect of region of interest variations on morphologic operations data and gray-level values extracted from digitized dental radiographs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 88(5):636–639. https://doi.org/10.1016/s1079-2104(99)70098-3
Weibel ER (1991) Fractal geometry: a design principle for living organisms. Am J Physiol 261(6 Pt 1):L361–L369. https://doi.org/10.1152/ajplung.1991.261.6.l361
Ruttimann UE, Webber RL, Hazelrig JB (1992) Fractal dimension from radiographs of peridental alveolar bone: a possible diagnostic indicator of osteoporosis. Oral Surg Oral Med Oral Pathol 74(1):98–110. https://doi.org/10.1016/0030-4220(92)90222-c
Aktuna Belgin C, Serindere G (2020) Evaluation of trabecular bone changes in patients with periodontitis using fractal analysis: a periapical radiography study. J Periodontol 91(7):933–937. https://doi.org/10.1002/jper.19-0452
Tümer N, Gültan AS (1999) Comparison of the effects of monoblock and twin-block appliances on the skeletal and dentoalveolar structures. Am J Orthod Dentofacial Orthop 116(4):460–468. https://doi.org/10.1016/s0889-5406(99)70233-7
Amer ME, Heo MS, Brooks SL, Benavides E (2012) Anatomical variations of trabecular bone structure in intraoral radiographs using fractal and particles count analyses. Imaging Sci Dent 42(1):5–12. https://doi.org/10.5624/isd.2012.42.1.5
McNamara JA Jr, Carlson DS (1979) Quantitative analysis of temporomandibular joint adaptations to protrusive function. Am J Orthod 76(6):593–611. https://doi.org/10.1016/0002-9416(79)90206-9
Kwak KH, Kim SS, Kim YI, Kim YD (2016) Quantitative evaluation of midpalatal suture maturation via fractal analysis. Korean J Orthod 46(5):323–330. https://doi.org/10.4041/kjod.2016.46.5.323
Acknowledgements
The authors would like to thank Başak Oğuz for the statistical analysis.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by E. Bolat Gümüş, E. Yavuz, and C. Tufekci. The first draft of the manuscript was written by E. Bolat Gümüş and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. Conceptualization and Methodology: E. Bolat Gümüş; Formal analysis and investigation: E. Bolat Gümüş, E. Yavuz, C. Tufekci; Writing—original draft preparation: E. Bolat Gümüş, E. Yavuz, C. Tufekci; Writing—review and editing: E. Bolat Gümüş, E. Yavuz, C. Tufekci; Supervision: E. Bolat Gümüş.
Corresponding author
Ethics declarations
Conflict of interest
E. Bolat Gümüş, E. Yavuz and C. Tufekci declare that they have no competing interests.
Ethical standards
This retrospective study was approved by the Ethics Committee of the Akdeniz University Faculty of Medicine (Approval Date and No.: 08 July 2020, 508). The study material was selected from the archives of the Akdeniz University Faculty of Dentistry, Department of Orthodontics. Informed consent: Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bolat Gümüş, E., Yavuz, E. & Tufekci, C. Effects of functional orthopedic treatment on mandibular trabecular bone in class II patients using fractal analysis. J Orofac Orthop 84 (Suppl 3), 155–164 (2023). https://doi.org/10.1007/s00056-022-00397-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00056-022-00397-4