Abstract
Purpose
We aimed to compare the short-term effects of alternate rapid maxillary expansion and constriction (Alt-RAMEC) with conventional rapid maxillary expansion (RME) followed by facemask (FM) therapy.
Methods
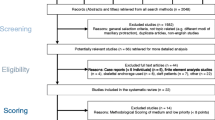
A total of 30 patients who had received facemask therapy after RME or Alt-RAMEC protocols were included in the study. The Alt-RAMEC/FM and RME/FM groups were created to be well-matched regarding cervical vertebral maturation stage and sex. In the Alt-RAMEC group (10 males and 5 females, 10.99 ± 1.80 years), expansion screws were activated for a week (two turns/day), then deactivated in the following week (two turns/day). The activation–deactivation protocol continued for 6 or 7 weeks. In the RME/FM group (10 males and 5 females, 11.61 ± 1.20 years), screw activation was performed according to the patients’ requirements. Lateral cephalograms which had been taken at the beginning of treatment and at the end of the facemask therapy were analyzed. Intragroup and intergroup differences were statistically analyzed.
Results
Both groups showed a significant sagittal advancement of the maxilla. However, the Alt-RAMEC/FM group showed statistically greater improvements than the RME/FM group for SNA (3.11 ± 1.79 vs. 1.45 ± 1.34, p = 0.008), ANB (4.29 ± 1.80 vs. 2.95 ± 1.19, p = 0.023), convexity (8.91 ± 4.29 vs. 5.61 ± 2.51, p = 0.016), and overjet (5.86 ± 2.29 vs. 4.61 ± 2.10, p < 0.001). The sagittal mandibular, vertical skeletal, dental, and soft tissue changes were similar between the groups (p > 0.05).
Conclusion
The Alt-RAMEC protocol was found to be more effective in the correction of skeletal class III malocclusion in the short term.
Zusammenfassung
Ziel
Unser Ziel war es, die Kurzzeiteffekte einer alternierenden schnellen Gaumennahtexpansion und -konstriktion (Alt-RAMEC) mit einer konventionellen schnellen Gaumennahtexpansion (RME) mit anschließender Gesichtsmaskenbehandlung (FM) zu vergleichen.
Methoden
In die Studie wurden insgesamt 30 Patienten aufgenommen, die nach RME- oder Alt-RAMEC-Protokollen eine Gesichtsmaskenbehandlung erhalten hatten. Die Gruppen Alt-RAMEC/FM und RME/FM wurden so zusammengestellt, dass sie hinsichtlich des Reifungsgrads der Halswirbel und des Geschlechts gut übereinstimmten. In der Alt-RAMEC-Gruppe (10 Jungen, 5 Mädchen, 10,99 ± 1,80 Jahre) wurden die Dehnschrauben eine Woche lang aktiviert (2 Umdrehungen/Tag) und in der darauf folgenden Woche deaktiviert (2 Umdrehungen/Tag). Das Aktivierungs‑/Deaktivierungsprotokoll wurde für 6 oder 7 Wochen fortgesetzt. In der RME/FM-Gruppe (10 Jungen, 5 Mädchen, 11,61 ± 1,20 Jahre) wurde die Schraubenaktivierung entsprechend den Anforderungen der Patienten durchgeführt. Die zu Beginn der Behandlung und am Ende der Gesichtsmaskenbehandlung angefertigten seitlichen Kephalogramme wurden analysiert. Die Unterschiede zwischen den einzelnen Gruppen wurden statistisch ausgewertet.
Ergebnisse
Beide Gruppen zeigten eine signifikante sagittale Vorverlagerung des Oberkiefers. Die Alt-RAMEC/FM-Gruppe zeigte jedoch statistisch größere Verbesserungen als die RME/FM-Gruppe für SNA (3,11 ± 1,79 vs. 1,45 ± 1,34, p = 0,008), ANB (4,29 ± 1,80 vs. 2,95 ± 1,19, p = 0,023), Konvexität (8,91 ± 4,29 vs. 5,61 ± 2,51, p = 0,016) und Overjet (5,86 ± 2,29 vs. 4,61 ± 2,10, p < 0,001). Die sagittalen mandibulären, vertikalen skelettalen, dentalen und Weichgewebeveränderungen waren zwischen den Gruppen ähnlich (p > 0,05).
Schlussfolgerung
Das Alt-RAMEC-Protokoll erwies sich bei der kurzfristigen Korrektur von skelettalen Klasse-III-Malokklusionen als wirksamer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Skeletal class III malocclusion is characterized by maxillary retrusion, mandibular protrusion, or both. Facemask (FM) therapy is commonly used for the early correction of class III malocclusions. The primary purpose of facemask therapy is to protract the retrusive maxilla anteriorly by modifying sutural growth [1].
Rapid maxillary expansion (RME) is a recommended treatment adjunction with maxillary protraction therapy for mobilization of the circummaxillary sutures [2]. However, the amount of rapid maxillary expansion for a patient without maxillary transversal deficiency is often limited and may not provide sufficient sutural mobilization for the anterior movement of the maxilla. In 2005, as a solution to this limitation, Liou and Tsai [3] announced the alternate maxillary expansion and constriction (Alt-RAMEC) procedure with the hypothesis that opening and closing the sutures within a distinct course would result in more mobilization in the sutures, and they reported this method to be more effective than conventional RME. In 2008, Wang et al. [4] histologically demonstrated that the Alt-RAMEC procedure opens sutures more than conventional RME in a study with inbred cats.
There is a limited number of studies comparing treatment results between Alt-RAMEC and conventional RME followed by facemask therapy, and their results include some contradictions. While Isci et al. [5] found the Alt-RAMEC/FM procedure led to two times more anterior movement of point A than the conventional method (4.13 vs 2.33), Liu et al. [6] reported that the Alt-RAMEC/FM protocol produced differences of less than 1 mm or 1°, which was not clinically significant. Masucci et al. [7] suggested that the Alt-RAMEC/FM protocol was more effective than the conventional RME/FM therapy. However, Da Luz Vieira et al. [8], Do-deLatour et al. [9], Ozbilen et al. [10], and Fisher et al. [11] did not find a statistical difference between Alt-RAMEC/FM and RME/FM groups. Also, in a recent systematic review [12], the evidence regarding the Alt-RAMEC protocol was stated to be based on only low to moderate certainty.
In the majority of previous studies [5, 6, 8, 10], groups with matched chronological ages were compared. On the other hand, in assessing the skeletal response of growing patients to treatment, it might be more logical to consider skeletal maturation and sex of the patients [13, 14]. Therefore, the present study aimed to reveal the differences in skeletal, dental, and soft tissue changes between Alt-RAMEC/FM and RME/FM treatment modalities by comparing well-matched groups in terms of skeletal maturation and sex.
Materials and methods
Ethical approval was obtained from the clinical research ethics committee of Tokat Gaziosmanpasa University (Study number: 20-KAEK-191). Patients who were treated with 6 or 7 weeks of Alt-RAMEC protocol (with twice daily activation of the expander) followed by facemask therapy at the Orthodontics Departments of Tokat Gaziosmanpasa and Erciyes Universities between the years 2013 and 2020 were recruited. Informed consent was obtained from the parents of all participants included in the study. The inclusion criteria were growing patients with negative Wits values, class III malocclusion, and 0 mm or less overjet. Patients with any craniofacial anomaly such as cleft lip and palate, poor cooperation (who wear the FM for less than 12 h a day), or missing records were excluded.
Records of 15 patients (10 males and 5 females, mean age of 10.99 ± 1.80 years) who met the inclusion criteria were collected. Then, cervical vertebral maturation stages (CVMS) were determined according to the method of Hassel and Farman [10] from the pretreatment lateral cephalometric radiographs of these patients by an orthodontist with 4 years of experience (SY), and the data were recorded in an Excel file (Microsoft, Redmond, WA, USA): 8 of the 15 patients were at stage CVMS1, 6 were at CVMS2, and 1 of them was at CVMS3. Another 15 patients (10 males and 5 females, mean age of 11.61 ± 1.20 years) who received RME/FM therapy and matched well in terms of CVMS and sex were recruited from the archives. The same inclusion and exclusion criteria were applied to this group. Pretreatment chronological ages, total facemask usage times, and the cooperation levels of the patients were recorded from the files of the patients.
An acrylic bonded Hyrax appliance (Fig. 1) and a Petit-type facemask (FM; Fig. 2) were used in both the Alt-RAMEC/FM and RME/FM groups. In the Alt-RAMEC/FM group, the expansion screw was activated twice daily (0.4 mm per day) in the first week and deactivated in the following week. This course was continued for 6 or 7 weeks depending on the patient’s requirement. In patients with a narrow maxilla, the course was terminated by activating the screw in the seventh week. In those who did not need maxillary expansion, the course was terminated after deactivating the screw in week 6. After carrying out this protocol, facemasks that implement a total force of 700–800 cN (350–400 cN per side) were applied. In the RME/FM group, the screw was activated twice daily for 2 weeks, and then additional activations were applied according to the patient’s requirement. Then, the facemasks were applied to the patients with a total force of 700–800 cN.
The protraction hooks were in the canine region of the appliances, and the protraction forces were applied via protraction elastics, with an angle of 30–45° downward to the occlusal plane. The patients were instructed to wear facemasks for 16–18 hours a day and change their elastics daily. The treatment was terminated when a minimum of 2 mm positive overjet was reached.
The lateral cephalometric radiographs of the patients taken just before the treatment and at the end of the facemask therapy were traced using Dolphin® Imaging software (version 11.5, Patterson Dental Supply, Chatsworth, CA, USA) by a single, blinded examiner (SY). In all, 10 angular and 13 linear measurements were performed to evaluate the skeletal, dental, and soft tissue changes.
Two months later, to assess the repeatability of the measurements, 10 randomly selected cephalograms were retraced by the same researcher (SY).
Statistical analysis
The statistical analysis of the data was carried out using Sigmastat 3.5 (Statcon© Witzenhausen, Germany). The means and standard deviations of the changes between the pre- and posttreatment measurements were calculated. Shapiro–Wilks test was used for evaluating the normality of the data. Then, paired-samples T‑test for normally distributed and Wilcoxon test for nonnormally distributed data were used. Intergroup differences were tested with independent samples T‑test or Mann–Whitney U test. Pearson correlation was used to assess the intraexaminer reliability. The level of significance was set at p < 0.05. A post hoc power analysis was conducted using G*Power 3.1.9.6.
Results
The post power of the present study, when assessing treatment differences between the groups (for the SNA variable), was calculated as 80%. The intraexaminer reliability was high with the Pearson coefficient varying between 0.731 and 0.989.
The severity of the sagittal and vertical skeletal malocclusions, chronological age of the patients, sex distribution, and skeletal maturation stages were similar between the groups, at the beginning of treatment (p > 0.05). Also, the facemask usage durations were also found to be similar (8.24 ± 2.94 months in the Alt-RAMEC/FM and 7.81 ± 1.95 months in the RME/FM group; p > 0.05; Table 1).
Statistically significant improvements were found for some skeletal measurements in both groups (Tables 2 and 3). The SNA angle increased by 3.11 ± 1.79° and 1.45 ± 1.34° in the Alt-RAMEC/FH and RME/FM groups, respectively (Table 4). Both groups showed a significant decrease of the SNB (1.2 ± 1.03°, 1.5 ± 0.99°) and a significant increase of the vertical skeletal measurements which indicates a posterior rotation of the mandible. As a result, the overbite was found to be reduced by 1.51 ± 2.34 and 1.71 ± 2.09 mm in the Alt-RAMEC/FH and RME/FM groups, respectively (Table 4). There was no statistically significant change in the dental measurements, the nasolabial angle, and the lower lip position for both groups (p > 0.05). The upper lip was found to be protruded in both groups (Tables 2 and 3).
The Alt-RAMEC/FM group was found to be more effective in the correction of the class III malocclusion than the RME/FM group, with greater improvements of SNA (3.11° vs 1.45°, p = 0.008), ANB (4.29° vs 2.95°, p = 0.023), convexity (8.91° vs 5.61°, p = 0.016), and overjet (5.86 mm vs 4.61 mm, p < 0.001). The sagittal mandibular, the vertical skeletal, the dental, and the soft tissue changes were similar between the groups (Table 4).
Discussion
The studies in the literature vary considerably in terms of the applied protraction force (700–1000 cN), the activation rate of the expander (2 or 4 times a day), the Alt-RAMEC duration (4–9 weeks or throughout the entire course of maxillary protraction) [15, 16], the screw design (Hyrax, Haas [15], double-hinged [3, 10], bone-anchored [17,18,19]), the chronological ages of the patients treated (5.6–13.3 years), the existence of cleft lip and palate anomaly, and the protraction appliance used (noncompliance intraoral springs [3], bone-anchored class III elastics [20], or facemasks). Similarly, the presented results of these studies are quite different.
The results of the current study revealed that Alt-RAMEC/FM therapy led to a small but greater advancement of the maxilla than RME/FM (with a 1.66° greater increase of the SNA angle) in non-cleft patients. The findings of our study support some related studies [5,6,7, 12]. Masucci et al. [7] reported that the increase of the SNA angle in their Alt-RAMEC/FM group was 1.2° greater than in the RME/FM group. Similarly, Isci et al. [5] found a 1.23° greater increase of the SNA angle and 1.17 mm more advancement at A point in their Alt-RAMEC/FM group in the short term. Liu et al. [6] reported 0.74° more increase of the SNA and 0.93 mm more advancement of point A in their Alt-RAMEC/FM group but stated that this difference being less than 1° would not be of clinical significance. In a recent study [16], even with simultaneous application of a facemask and the Alt-RAMEC protocol, only 0.88° more increase of the SNA and 0.83 mm more advancement of point A was found in the Alt-RAMEC/FM group compared to the RME/FM group. In light of these findings, long-term results would be most important. However, as far as we know, there are very few studies in the literature in which long-term results were analyzed.
In the study of Liou and Tsai [3], the observed difference in the amount of maxillary advancement obtained with Alt-RAMEC compared to conventional RME was reported to be significantly higher than that in the above-mentioned studies (3.2 mm more maxillary advancement in the Alt-RAMEC group, 5.8 mm vs 2.6 mm). Similarly, Meazzini et al. reported 5.7 mm sagittal advancement of point A in cleft patients [20] and 5.4 mm in non-cleft patients [21]. However, unlike other related studies, they [3, 20, 21] used noncompliance intraoral springs for maxillary protraction instead of a removable facemask and a double-hinged expander instead of a Hyrax. In addition, Meazzini et al. [20, 21] used miniscrews for distributing the traction forces to the bones. In light of these limited findings, the reason for the greater amounts of advancements can mainly be attributed to the expander type and daytime application of the protraction forces.
Based on Biederman’s theory [22], Liou and Tsai [3] claimed that in cleft patients the Alt-RAMEC protocol alone (without applying a maxillary protraction force), carried out with a double-hinged expander, results in more sagittal advancement of the maxilla than RME alone. They reported 3 mm forward movement at point A following an Alt-RAMEC protocol alone for 9 weeks. On the other hand, in non-cleft patients in a CBCT study, the forward movement of point A was reported to be only 0.89 mm [23] after following the same Alt-RAMEC protocol and the same type expander as Liou and Tsai [3]. The difference in results might be due to the use of different imaging modalities (2D cephalograms versus CBCT) and the different maxillary morphology of cleft patients.
Some researchers [8,9,10,11, 20] did not find any statistically significant difference between their Alt-RAMEC/FM and RME/FM groups. The inconsistency between the results may be attributed to individual variables such as inhomogeneous cooperation level and/or skeletal maturation of the groups. As there are only small differences between the two treatment protocols, even minor differences related to the variables mentioned above may affect the results. To our knowledge, this is the first study comparing non-cleft Alt-RAMEC/FM and RME/FM groups that match well in terms of skeletal maturation and sex. In most of the former studies, the investigated groups were created based on chronological age [5, 6, 8, 10]. However, the correlation between chronological age and skeletal maturation was found to be quite low [13]. Treatment applied at different maturation stages can induce different amounts of skeletal response, and this can affect the outcome. To overcome this bias, the groups of the current study were created from patients who were matched regarding skeletal maturation and sex.
Exactly determining the facemask wearing time is another critical point when comparing different clinical studies. Except for the study of Liou and Tsai [3], generally, wearing time was determined according to the patients’ statements, or the patients were asked to compile a list of daily use. Especially in the case of children, these statements might be unreliable. Thus, it might not be possible to determine the differences in cooperation between the groups. The same limitation exists in the current study. Since the current study was retrospective, the facemask wearing times of the patients were collected from the treatment forms which were filled out according to patients’ statements. For future prospective studies, using noncompliance appliances or technologies [24] that measure the duration of facemask use can increase the reliability of the results.
The present study also showed that Alt-RAMEC/FM and RME/FM therapies did not cause any significant change of the lower and upper incisor positions or inclinations. These findings are consistent with the results of Isci et al. [5], Do-deLatour et al. [9], Liu et al. [6], and Maino et al. [25]. However, Liou and Tsai [3] reported a significant protrusion of the upper incisors and a significant retrusion of the lower incisors in both Alt-RAMEC and RME groups. This difference might be explained by the diversity of the maxillary protraction appliances used. In Liou and Tsai’s study design, the protraction force was applied to banded upper canines and maxillary first molars while an acrylic bonded expander which comprised all posterior maxillary teeth was used in the present study. In addition, Liou and Tsai used the lower arch for anchorage, while the chin and forehead were used in our study. The intraoral maxillary protraction springs might have caused more dental effects than a facemask combined with a bonded expander. These undesirable dental effects were also reported after facemask therapy combined with banded RME appliances [26, 27]. On the other hand, although it is more invasive, using bone-anchored appliances could also be another option to eliminate the dental side effects of the treatment, especially in older patients [19, 28, 29].
According to the current study, both treatment modalities caused an increase in the vertical skeletal dimension, but these effects were similar between the groups. These results are consistent with the literature [5, 7, 9, 10, 30]. This effect is believed to be caused by the facemask putting a retrusive force on the chin and forcing the mandible to rotate posteriorly. Based on these findings, it might be more reasonable to apply the facemask especially on patients with lower vertical facial height.
This retrospective study presents evidence without being affected by inhomogeneous group bias that Alt-RAMEC/FM therapy leads to slightly more favorable skeletal effects than RME/FM. However, there are some limitations. The retrospective design of the study, not considering the growth pattern of the patients, the absence of an untreated control group, and the relatively small sample size can be listed as limitations. Also, this study includes only short-term results.
Conclusions
With some limitations, the present study supports that, at least in the short term, class III treatment following the Alt-RAMEC/FM protocol is slightly but more effective than that following the RME/FM protocol. Nevertheless, randomized controlled studies evaluating long-term results with larger sample sizes are needed before the Alt-RAMEC protocol becomes a routine treatment method for the early correction of skeletal class III malocclusion.
References
Tanne K, Sakuda M (1991) Biomechanical and clinical changes of the craniofacial complex from orthopedic maxillary protraction. Angle Orthod 61(2):145–152
Foersch M, Jacobs C, Wriedt S, Hechtner M, Wehrbein H (2015) Effectiveness of maxillary protraction using facemask with or without maxillary expansion: a systematic review and meta-analysis. Clin Oral Investig 19(6):1181–1192
Liou EJ, Tsai WC (2005) A new protocol for maxillary protraction in cleft patients: repetitive weekly protocol of alternate rapid maxillary expansions and constrictions. Cleft Palate Craniofac J 42(2):121–127
Wang YC, Chang PM, Liou EJ (2009) Opening of circumaxillary sutures by alternate rapid maxillary expansions and constrictions. Angle Orthod 79(2):230–234
Isci D, Turk T, Elekdag-Turk S (2010) Activation-deactivation rapid palatal expansion and reverse headgear in class III cases. Eur J Orthod 32(6):706–715
Liu W, Zhou Y, Wang X, Liu D, Zhou S (2015) Effect of maxillary protraction with alternating rapid palatal expansion and constriction vs expansion alone in maxillary retrusive patients: a single-center, randomized controlled trial. Am J Orthod Dentofacial Orthop 148(4):641–651
Masucci C, Franchi L, Giuntini V, Defraia E (2014) Short-term effects of a modified Alt-RAMEC protocol for early treatment of class III malocclusion: a controlled study. Orthod Craniofac Res 17(4):259–269
da Luz Vieira G, de Menezes LM, de Lima EM, Rizzatto S (2009) Dentoskeletal effects of maxillary protraction in cleft patients with repetitive weekly protocol of alternate rapid maxillary expansions and constrictions. Cleft Palate Craniofac J 46(4):391–398
Do-deLatour TB, Ngan P, Martin C, Razmus T, Gunel E (2009) Effect of alternate maxillary expansion and contraction on protraction of the maxilla: a pilot study. Hong Kong Dent J 6(2):72–82
Onem Ozbilen E, Yilmaz HN, Kucukkeles N (2019) Comparison of the effects of rapid maxillary expansion and alternate rapid maxillary expansion and constriction protocols followed by facemask therapy. Korean J Orthod 49(1):49–58
Fischer B, Masucci C, Ruellas A et al (2018) Three-dimensional evaluation of the maxillary effects of two orthopaedic protocols for the treatment of class III malocclusion: a prospective study. Orthod Craniofac Res 21(4):248–257
Zhao T, Hua F, He H (2020) Alternate rapid maxillary expansion and constriction (Alt-RAMEC) may be more effective than rapid maxillary expansion alone for protraction facial mask treatment. J Evid Based Dent Pract 20(2):101408
Alkhal HA, Wong RW, Rabie AB (2008) Correlation between chronological age, cervical vertebral maturation and Fishman’s skeletal maturity indicators in southern Chinese. Angle Orthod 78(4):591–596
Almeida M, Laurent MR, Dubois V et al (2017) Estrogens and androgens in skeletal physiology and pathophysiology. Physiol Rev 97(1):135–187
Celikoglu M, Buyukcavus MH (2017) Evaluation of the effects of two different Alt-RAMEC procedures: five weeks versus nine weeks. Aust Orthod J 33(2):249
Liu Y, Hou R, Jin H et al (2021) Relative effectiveness of facemask therapy with alternate maxillary expansion and constriction in the early treatment of class III malocclusion. Am J Orthod Dentofacial Orthop 159(3):321–332
Al-Mozany SA, Dalci O, Almuzian M, Gonzalez C, Tarraf NE, Darendeliler AM (2017) A novel method for treatment of class III malocclusion in growing patients. Prog Orthod 18(1):40
Wilmes B, Ngan P, Liou EJ, Franchi L, Drescher D (2014) Early class III facemask treatment with the hybrid hyrax and Alt-RAMEC protocol. J Clin Orthod 48(2):84–93
Kaya D, Kocadereli I, Kan B, Tasar F (2011) Effects of facemask treatment anchored with miniplates after alternate rapid maxillary expansions and constrictions; a pilot study. Angle Orthod 81(4):639–646
Meazzini MC, Zappia LB, Tortora C, Autelitano L, Tintinelli R (2019) Short- and long-term effects of late maxillary advancement with the Liou-Alt-RAMEC protocol in unilateral cleft lip and palate. Cleft Palate Craniofac J 56(2):159–167
Meazzini MC, Torre C, Cappello A, Tintinelli R, De Ponti E, Mazzoleni F (2021) Long-term follow-up of late maxillary orthopedic advancement with the Liou-alternate rapid maxillary expansion-constriction technique in patients with skeletal class III malocclusion. Am J Orthod Dentofacial Orthop 160(2):221–230
Biederman W (1973) Rapid correction of class III malocclusion by midpalatal expansion. Am J Orthod 63(1):47–55
Yilmaz BS, Kucukkeles N (2014) Skeletal, soft tissue, and airway changes following the alternate maxillary expansions and constrictions protocol. Angle Orthod 84(5):868–877
Stocker B, Willmann JH, Wilmes B, Vasudavan S, Drescher D (2016) Wear-time recording during early class III facemask treatment using Theramon chip technology. Am J Orthod Dentofacial Orthop 150(3):533–540
Maino G, Turci Y, Arreghini A, Paoletto E, Siciliani G, Lombardo L (2018) Skeletal and dentoalveolar effects of hybrid rapid palatal expansion and facemask treatment in growing skeletal class III patients. Am J Orthod Dentofacial Orthop 153(2):262–268
Miranda F, da Cunha Bastos JC, Magno Dos Santos A, Janson G, Lauris JRP, Garib D (2021) Dentoskeletal comparison of miniscrew-anchored maxillary protraction with hybrid and conventional hyrax expanders: a randomized clinical trial. Am J Orthod Dentofacial Orthop 160(6):774–783
Ngan P, Wilmes B, Drescher D, Martin C, Weaver B, Gunel E (2015) Comparison of two maxillary protraction protocols: tooth-borne versus bone-anchored protraction facemask treatment. Prog Orthod 16(1):1–11
Nienkemper M, Wilmes B, Franchi L, Drescher D (2014) Effectiveness of maxillary protraction using a hybrid hyrax-facemask combination: a controlled clinical study. Angle Orthod 85(5):764–770
Gandedkar NH, Liou EJ (2018) The immediate effect of alternate rapid maxillary expansions and constrictions on the alveolus: a retrospective cone beam computed tomography study. Prog Orthod 19(1):40
Kama JD, Ozer T, Baran S (2006) Orthodontic and orthopaedic changes associated with treatment in subjects with class III malocclusions. Eur J Orthod 28(5):496–502
Author information
Authors and Affiliations
Contributions
Sibel Akbulut: Conceptualization, Methodology, Resources, Writing—Original Draft, Visualization; Sema Yilmaz: Resources, Formal analysis, Validation, Investigation, Data Curation; Ahmet Yagci: Conceptualization, Methodology, Resources, Writing—Review and Editing, Supervision.
Corresponding author
Ethics declarations
Conflict of interest
S. Akbulut, S. Yilmaz and A. Yagci declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval for the study was obtained from the clinical research ethics committee of Tokat Gaziosmanpasa University (study number: 20-KAEK-191). Informed consent was obtained from all individual participants included in the study. Patients signed informed consent regarding publishing their data and photographs.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Akbulut, S., Yilmaz, S. & Yagci, A. Comparison of the short-term effects of facemask therapy preceded by conventional rapid maxillary expansion or by an alternate rapid maxillary expansions and constrictions protocol. J Orofac Orthop 84, 278–286 (2023). https://doi.org/10.1007/s00056-022-00380-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00056-022-00380-z
Keywords
- Dentofacial orthopedics
- Skeletal class III malocclusion
- Maxillary retrusion
- Mandibular protrusion
- Circummaxillary sutures