Abstract
Purpose
Although several prescriptions and techniques exist for comprehensive fixed appliance treatment, their treatment effects have not yet been adequately assessed in an evidence-based manner. The aim of this systematic review was to assess the therapeutic and adverse effects of various prescriptions or techniques for orthodontic appliances from randomized clinical trials on human patients.
Methods
Eight databases were searched up to July 2016 for randomized trials assessing any orthodontic prescriptions or techniques in human patients. After elimination of duplicate studies, data extraction, and risk of bias assessment according to the Cochrane guidelines, random effects meta-analyses with mean differences (MD) and their 95% confidence intervals (CIs) were performed.
Results
Compared to Roth preadjusted appliances, both Begg and modified Begg appliances were associated with statistically significantly worse occlusal outcome assessed with Peer Assessment Review (PAR) scores (1 trial, MD 3.1 points, 95% CI 1.9–4.3 points and 1 trial, MD 2.4 points, 95% CI 1.2–3.6 points, respectively) with low quality of evidence, due to bias and imprecision. Compared to a partially programmed fixed orthodontic appliance, a fully programmed appliance was associated with a statistically significant, but clinically irrelevant increase in treatment duration (1 trial, MD 2.4 months, 95% CI 0.6–4.2 months), supported by high quality of evidence. However, caution is needed in the interpretation of these results as only a limited number of small trials with methodological issues were available.
Conclusions
Based on existing trials, there is limited evidence to support any robust clinical recommendation regarding the prescriptions or techniques for fixed orthodontic appliances.
Registration: PROSPERO (CRD42016042727).
Funding: None.
Zusammenfassung
Zielsetzung
Zwar gibt es etliche Systeme und Techniken für eine umfassende Behandlung mit festsitzenden kieferorthopädischen Apparaturen, doch ihre Effekte sind noch nicht angemessen evidenzbasiert erforscht worden. Ziel dieses systematischen Reviews war die Untersuchung von sowohl therapeutisch erwünschten als auch unerwünschten Auswirkungen unterschiedlicher Systeme bzw. Techniken für kieferorthopädische Apparaturen mittels randomisierter klinischer Studien an menschlichen Patienten.
Methoden
In 8 Datenbanken wurde nach randomisierten klinischen Humanstudien zu kieferorthopädischen Systemen oder Techniken recherchiert. Nach Eliminierung von Duplikaten, Datenextraktion und Einsatz des Risk-of-Bias-Tools der Cochrane Collaboration wurden Metaanalysen unter Anwendung eines random effect model sowie von mittleren Differenzen (mean differences, MDs) und deren 95% Konfidenzintervallen (KI) durchgeführt.
Ergebnisse
Im Vergleich mit den Roth-Apparaturen zeigten sowohl die Begg- als auch die modifizierten Begg-Apparaturen nach PAR(“peer assessement review”)-Scores (eine Studie, MD 3,1 Punkte, 95%-KI 1,9-4,3; eine Studie, MD 2,4 Punkte, 95%-KI 1,2-3,6) ein hinsichtlich der Okklusion statistisch signifikant ungünstigeres Outcome, allerdings mit geringer Evidenzqualität bedingt durch Bias und mangende Präzision. Verglichen mit einer teilweise programmierten festsitzenden kieferorthopädischen Apparatur war eine vollständig programmierte Apparatur assoziiert mit einer statistisch signifikanten, klinisch jedoch weitgehend irrelevanten Verlängerung der Behandlungsdauer (eine Studie, MD 2,4, 95%-KI 0,6-4,2 Monate), unterstützt durch eine hohe Evidenz-Qualität. Da nur eine begrenzte Anzahl kleiner, methodisch nicht unproblematischer Studien zur Verfügung stand, sind diese Ergebnisse allerdings mit Vorsicht zu interpretieren.
Schlussfolgerungen
Auf der Basis verfügbarer Studien besteht nur eine sehr limitierte Datenlage, anhand derer sich klinische Empfehlungen hinsichtlich Systeme bzw. Techniken für festsitzende kieferorthopädische Apparaturen evidenzbasiert unterstützen ließen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fixed appliances have become an integral part of comprehensive orthodontic treatment, as a versatile tool for three-dimensional controlled tooth movement. Through the years, great developments in orthodontic appliances and their torque/tip prescription have been seen since the initial appliance designed by E.H. Angle and the introduction of the preadjusted (“straight wire”) edgewise appliance by Andrews [4] including the Roth prescription [35], the MacLaughlin–Bennet–Trevisi (MBT) [18], and several other bracket prescriptions or techniques like the Tweed–Merrifield, Begg lightwire, Tip-Edge, and bioefficient technique [2, 6, 8, 9, 15, 19, 33, 34, 41, 43]. Among these, the straight wire concept revolutionized orthodontic treatment with fixed appliances and was founded on the universality of tooth-type shapes and positions, when an exemplary occlusion is present. This enables the incorporation of information about the ideal position of each tooth in the three planes (“prescription”) into the brackets that, when rightly prescribed and placed on the tooth surface, enable the correction of malpositioned teeth and dental arches without any bends inserted in the wire.
Over the years, several studies have attempted to assess the treatment effects of existing prescriptions or techniques for fixed orthodontic appliances in terms of occlusal outcome, control of tooth movement, treatment duration, pain, and discomfort [13, 14, 20, 21, 42]. However, to date, the therapeutic and adverse effects of prescriptions or techniques used in comprehensive fixed appliance treatment have not been systematically appraised, according to standard procedures of evidence-based orthodontics [29].
The aim of the present systematic review is to critically assess the available evidence from randomized clinical trials on humans investigating any prescription or technique used for fixed orthodontic appliances and, if possible, to pool evidence from existing trials together in a meta-analysis.
Materials and methods
Protocol and registration
The protocol for this systematic review was made a priori based on the PRISMA-P statement [37], registered in PROSPERO (CRD42016042727), and all post hoc changes were appropriately noted. This systematic review is conducted and reported according to the Cochrane Handbook [12] and PRISMA statement [16], respectively.
Eligibility criteria
According to the Participants–Intervention–Comparison–Outcome Study design (PICOS) schema, we included parallel randomized and quasi-randomized prospective controlled trials on human patients comparing any two prescriptions or techniques for fixed orthodontic appliances and assessing therapeutic effects (both effectiveness and efficacy) or adverse effects (Supplementary Appendix 1). Excluded were nonclinical studies, retrospective studies, animal studies, and studies with partial, self-ligating, or lingual appliances.
Information sources and literature search
A total of seven electronic databases (MEDLINE through PubMed, Cochrane Database of Systematic Reviews, Cochrane Database of Abstracts of Reviews of Effects, Cochrane Central Register of Controlled Trials, Virtual Health Library, Web of Knowledge, and Scopus) were searched systematically by two authors (SM, SNP) without any limitations for publication year, language, or status from inception up to 21 July 2016 (Supplementary Appendix 2). Two additional sources (Google Scholar and ISRCTN registry) were manually searched for additional trials or protocols by the same authors. Authors of included trials were contacted for additional missed or ongoing trials. The reference lists and citation lists of the included trials and relevant reviews were also manually searched.
Study selection and data extraction
Titles identified from the search were screened by one author (SM) with a subsequent duplicate independent checking of their abstracts/full texts against the eligibility criteria by a second author (SNP), while conflicts were resolved by a third author (TE). Characteristics of included trials and quantitative data were extracted in duplicate by two authors (SM, SNP) using predetermined and piloted extraction forms. Missing or unclear information was requested by the trials’ authors.
Risk of bias in individual trials
The risk of bias of the included trials was assessed using Cochrane’s risk of bias tool [12] after initial calibration. A main risk of bias assessment was included in the systematic review pertaining to each trial’s primary outcome.
Data analysis
The mean difference (MD) and the relative risk (RR) with their corresponding 95% confidence intervals (CI) were chosen as effect measures for continuous and binary outcomes, respectively. As the outcome of fixed appliance treatment is bound to be affected by characteristics of the used brackets, archwires, and auxiliaries [26–28], a random effects model according to DerSimonian and Laird [10] was deemed clinically and statistically appropriate for meta-analysis [24]. However, no meta-analyses of two or more studies, assessment of between trial heterogeneity, and additional analyses (subgroup or metaregression analyses, and sensitivity analyses) could be conducted due to the limited number of included studies, which are presented descriptively. All analyses were run using Stata SE 10.0 (StataCorp, College Station, TX, USA) by one author (SNP). A two-tailed P value of 0.05 was considered significant for hypothesis testing.
Risk of bias across studies
The overall quality of evidence (confidence in effect estimates) for each of the main outcomes was rated using the GRADE approach [11]. For this assessment, the risk of bias of each included trial was re-assessed separately at outcome level.
The minimal clinical important, large, and very large effects were conventionally defined [22] as half, one, and two standard deviations, respectively. The standard deviation for an outcome was averaged from control groups of the existing trials. Conventional cut-offs of 1.5, 2.5, and 4.3 were adopted for the relative risk (RR). Finally, the optimal information size (i.e., required meta-analysis sample size) was calculated for each outcome independently for α = 5% and β = 20%.
Results
Study selection
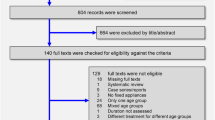
A total of 580 papers from electronic and 7 papers from manual searches were identified (Fig. 1; Supplementary Appendix 2). After removal of duplicates and initial screening, 54 papers were assessed for eligibility according to established inclusion criteria and finally 6 papers (5 published and one unpublished) remained for the final analysis (Fig. 1; Supplementary Appendix 3) [3, 23, 31, 32, 38, 40]. In one instance, duplicate publications (one thesis and one journal paper) pertaining to the same trial were grouped together; thus, a total of 5 trials was finally included in the systematic review.
Study characteristics
The characteristics of the trials included are shown in Table 1. All five included studies were parallel randomized clinical trials conducted in four different countries. They included a total of 370 patients (with at least 82 male and 103 female patients) with mean ages ranging between 12.3 and 15.3 years. A wide variety of interventions were used to treat different types of malocclusions depending on the eligibility criteria and protocols set in each trial. The Roth prescription was compared to either standard edgewise (one trial) [32], Begg and modified Begg appliances (one trial) [38], or to the MBT prescription (one trial) [40]. One unpublished trial [23] compared a standard edgewise appliance (Andrews prescription) group to a Tip-Edge appliance. Finally, one study [3] assigned patients to two groups, where maxillary distalization was performed with either three-dimensional bimetric arches (3D-BMDA) or a modified Begg system (MBIDS).
After the start of the active treatment, patients were followed for periods ranging from 8 weeks [40] to 6.5 months [3] and the investigated outcomes included among others treatment duration (3 trials [3, 23, 31]), chairside time (3 trials [23, 31, 38]), number of appointments (1 trial [23]), occlusal outcome (3 trials [23, 31, 38]), space closure (1 trial [31]), radiographic outcomes of tooth position/inclination (5 trials [3, 23, 31, 38, 40]), oral health (1 trial [31]), cost effectiveness (1 trial [23]), root resorption (1 trial [31]), and patient discomfort (1 trial [31]) (Table 1). The corresponding authors of included trials were contacted in several instances to request additional data. However, apart from one unpublished study [23], where the corresponding author provided a draft of the unpublished paper, no additional data could be retrieved.
Risk of bias within studies
A summary of the risk of bias for all studies is shown in Fig. 2. The detailed risk of bias assessment for the included trials can be found in Supplementary Appendix 4. High risk of bias was found in three trials (60%) for at least one bias domain. The most problematic domains were the blinding of outcome assessment (problematic in 60% of the trials), followed by incomplete outcome data (found in 20% of the trials).
Results of individual studies and data analysis
The retrieved results for all reported outcomes of all individual studies are quantitatively represented in Table 2. Substantial differences in the implemented interventions, participants’ characteristics, observational periods, and investigated outcomes among studies were observed, making them incompatible. Thus, no meta-analysis was attempted.
The statistically significant (P < 0.05) effects reported from the included studies can be summarized as follows. The Roth appliance was associated with a lower Peer Assessment Rating (PAR) score (better occlusal outcome), but also an increase in total chairside time compared to the Begg appliance. The Roth appliance was also associated with a lower PAR score (better occlusal outcome) compared to a modified Begg appliance. Significant short-term differences in the inclination of the upper and lower incisors and the upper canines were also found between Roth and MBT appliances. When a fully programmed fixed orthodontic appliance was compared to a partially programmed appliance, a statistically significant, but clinically irrelevant, increase in treatment duration by 2.4 months was reported. Finally, several cephalometric differences were found between the 3D-BMDA and the modified Begg distalization technique, but these were only minor and short-term.
Risk of bias across studies—GRADE assessment
The outcomes that were selected for assessment in the GRADE analysis were total treatment duration or chairtime, occlusal outcome (PAR score), upper incisor inclination, lower incisor inclination, and root resorption.
Roth vs. Begg and modified Begg fixed orthodontic appliances
Compared to the Roth appliance, use of the Begg appliance could probably decrease total chairtime, while the time saving with the use of a modified Begg appliance was statistically insignificant (moderate quality evidence for both). Additionally, based on low quality evidence use of either the Begg or the modified Begg appliance may slightly deteriorate the final occlusal outcome of treatment. Finally, no considerable differences in the inclination of the upper or lower incisors were found between Roth, Begg, and modified Begg appliances (low quality of evidence). The main reasons for downgrading the quality of existing evidence were risk of bias due to methodological inadequacies and imprecision due to the small sample of the included trial (Table 3).
Fully vs. partially programmed fixed orthodontic appliances
Based on existing high-quality evidence coming from a single trial, the use of a fully programmed appliance slightly increases treatment duration (by about 2.4 months) compared to a partially programmed appliance, but seems to have little or no effect on occlusal outcome, incisor inclination, or the prevalence of root resorption after treatment (Table 4).
Discussion
Summary of evidence
The present systematic review included five parallel, randomized clinical trials and a total of 370 patients. Interestingly, although most of the prescriptions/techniques in question have existed for several decades, there is a considerable lack of clinical evidence regarding both the therapeutic and adverse effects that could enable the formulation of robust clinical recommendations for their use. This is mainly due to the small number of trials with limited sample sizes that were identified, which implemented different protocols and assessed diverse outcomes, making overall data analysis difficult.
Nevertheless, data analysis was considered feasible in the following two instances: in the comparison of comprehensive orthodontic treatment with a Roth versus treatment with a Begg or modified Begg appliance and in the comparison of a fully versus a partially programmed appliance where clinically important outcomes were reported. Use of a Begg appliance was associated with reduced chairside time compared to the use of a Roth appliance, which might imply more efficient treatment. On the other hand, the Begg appliance was associated with a worse occlusal outcome at the end of treatment as indicated by PAR, when compared to the Roth appliance. Therefore, no clear recommendations about treatment effectiveness with Roth or Begg appliances can be made. Additionally, these findings should be interpreted with caution, due to the observed moderate to high risk of bias and imprecision.
As for the outcomes obtained with the use of a fully programmed appliance (straight wire concept) compared to a partially programmed one (conventional full edgewise concept) [32], limited high-quality evidence indicates that no considerable differences exist in occlusal outcome, final inclination of the upper or lower incisors, or prevalence of root resorption after treatment. The only statistically significant difference was a slight decrease in treatment duration with the partially programmed appliance (2.4 months), which is probably irrelevant to the clinician. Therefore, both appliance types could, theoretically, be equally effective in treating malocclusions and appliance choice still remains, mainly, with the personal preference of the clinician.
Beyond the aforementioned findings, a considerable number of retrospective studies concerning the clinical assessment of various prescriptions and techniques for fixed orthodontic appliances are also available in the literature [13, 14, 20, 21, 42]. In the study of Kattner and Schneider [14], no differences in the ideal tooth relationship index were found when study models of patients treated with a Roth prescription preadjusted edgewise appliance were compared to those of patients treated with a standard edgewise appliance. In addition, Ugur and Yukay [42] found no differences in torque values between cases treated with standard edgewise and Roth prescription appliances by implementing an accurate method for the evaluation of faciolingual tooth inclination, as described by Andrews [4].
Comparisons between various techniques have been also performed in previous retrospective clinical studies, which were excluded from the present review due to their high risk of bias. Jain et al. [13] retrospectively assessed the occlusal outcome with the Objective Grading System (OGS) of the American Board of Orthodontists (ABO) after treatment with a Roth or an MBT appliance. They reported that the use of the MBT appliance was associated with a significantly better occlusal outcome than the Roth appliance (MD −2.7 OGS points; 95% CI −1.0 to −4.3 OGS points; P < 0.05). However, if we look at the baseline malocclusion severity of the two groups, we can see that the MBT group included patients with significantly “easier” malocclusions than the Roth group, as assessed with the ABO Discrepancy Index (DI; MD −3.8 points; 95% CI −0.4 to −7.2 points; P < 0.05). This can be better illustrated if we divide the mean OGS score with the mean DI score in each group, which would result in 1.49 and 1.74 for the Roth and MBT appliance, respectively. This means that given similar conditions, the Roth appliance is more efficient than the MBT appliance (both the OGS and the DI are scored negatively, meaning that less is better). Bias by confounding, as can be seen in this example, is just one of the several inherent limitations of retrospective study designs [30], which make them potentially inappropriate to base clinical recommendations upon. Additionally, Moesi et al. [21] found that bracket prescription had no effect on the subjective aesthetic outcome after treatment with either a Roth or MBT appliances. Furthermore, Mittal et al. [20] reported several tooth alignment outcomes after treatment with Roth or MBT appliances.
As far as straight wire versus standard edgewise appliances are concerned, Soltani et al. [39] reported that treatment with an MBT straight wire or a standard edgewise appliance resulted in similar occlusal outcomes (mean OGS of 20.0 and 20.4, respectively), but treatment with the MBT straight wire appliance was slightly shorter than with the standard edgewise appliance (24.0 and 26.0 months, respectively). In the study of Beg [5], a Roth straight wire appliance was compared with a standard edgewise appliance in the treatment of Class I malocclusion. Reanalysis of the provided raw data with multivariable regression indicated that Roth appliances were associated with slightly greater effectiveness (PAR 1.49 points more) and slightly greater treatment duration (2.69 months more) compared to standard edgewise appliance, although both differences were not statistically significant (P values of 0.104 and 0.180, respectively).
Additionally, Wu et al. [44] reported that MBT appliances were better to control the mesial inclination of molars, the vertical movement, and torque of anterior teeth during treatment than standard edgewise appliances. Mavragani et al. [17] systematically compared straight wire and standard edgewise appliances, both in 0.018-inch slots, in extraction treatment and found that straight wire appliances were associated with statistically significant less root resorption of the incisors than standard edgewise appliances, which was attributed to more efficient force control with this technique. Finally, Akhoundi et al. [1] reported that significantly more patients treated with straight wire appliances demonstrated canine guidance on laterotrusion and mutually protected occlusion posttreatment compared to patients treated with standard edgewise appliances. However, these results should be interpreted with caution, since they originate from retrospective studies that are inherently associated with high risk of bias.
Strengths and limitations
This systematic review provides a succinct summary of existing evidence with its main strengths being its a priori registration in PROSPERO [7], the extensive unrestricted literature search, the inclusion of unpublished data, the use of robust methodology pertaining to the qualitative and quantitative synthesis of data [25], the exclusion of biased study designs [30], transparent reporting of quantitative data for all outcomes from included studies, assessment of the quality of evidence with the GRADE approach [11], and the clear reporting of any deviations from the review’s protocol (Supplementary Appendix 8). However, this systematic review also has some limitations, like the limited number of included trials, which precluded the assessments of heterogeneity, subgroup analyses, small-study effects, and reporting biases for most of the outcomes. Although this could not be formally assessed as only a limited number of studies were included, the risk of publication bias might be considered minimal due to the extensive literature search which was not limited to publications in scientific journals. Furthermore, despite our efforts, no response was obtained from most contacted authors, apart from one author who provided an unpublished study [23].
Recommendations for clinical practice
There is insufficient evidence at present to make robust recommendations about any prescriptions or techniques for the fixed orthodontic appliance in terms of therapeutic or adverse effects. Existing evidence indicates that only minor differences can be directly attributed to the choice of prescription/technique, which are clinically irrelevant and our confidence in these estimates is very poor.
Recommendations for further research
Parallel randomized clinical trials or well-designed prospective trials with blinded outcome assessment are needed in order to form robust clinical recommendations. These should ideally be carried out according to the Consolidated Standards of Reporting Trials (CONSORT) statement [36] and adequately report on objective outcomes of treatment effectiveness and efficiency. These could include several therapeutic effects (like treatment duration, occlusal outcome with OGS, patient satisfaction/quality of life, and relapse) or adverse effects (including root resorption, white spot lesions, gingival recessions, oral pain, oral discomfort, functional impairment, and cost of treatment) so that reliable conclusions can be reached.
Conclusions
The present systematic review suggests that there is currently insufficient data to support the evidence-based clinical use of any particular prescription or technique for fixed orthodontic appliances over another in terms of efficiency, effectiveness, or side effects.
References
Akhoundi MS, Hashem A, Noroozi H (2009) Comparison of occlusal balance contacts in patients treated with standard edgewise and preadjusted straight-wire appliances. World J Orthod 10:216–219
Alexander RG (2001) The principles of the alexander discipline. Semin Orthod 7:62–66
Altug-Atac AT, Erdem D, Arat ZM (2008) Three-dimensional bimetric maxillary distalization arches compared with a modified Begg intraoral distalization system. Eur J Orthod 30:73–79
Andrews LF (1979) The straight-wire appliance. Br J Orthod 6:125–143
Beg Z (2002) Assessment of straightwire vs standard edgewise orthodontic treatment using the Par Index. Oregon Health & Science University, Master thesis
Begg PR (1961) Light-wire technique: employing the principles of differential force. Am J Orthod 47:30–48
Booth A, Clarke M, Ghersi D, Moher D, Petticrew M, Stewart L (2011) An international registry of systematic-review protocols. Lancet 377:108–109
Burstone CJ (1981) Variable-modulus orthodontics. Am J Orthod 80:1–16
Creekmore TD, Kunik RL (1993) Straight wire: the next generation. Am J Orthod Dentofac Orthop 104:8–20
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A (2011) GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol 64:380–382
Higgins JPT, Green S (2016) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. http://www.cochrane-handbook.org. Accessed 10 Aug 2016
Jain M, Varghese J, Mascarenhas R, Mogra S, Shetty S, Dhakar N (2013) Assessment of clinical outcomes of Roth and MBT bracket prescription using the American Board of Orthodontics objective grading system. Contemp Clin Dent 4:307–312
Kattner PF, Schneider BJ (1993) Comparison of Roth appliance and standard edgewise appliance treatment results. Am J Orthod Dentofac Orthop 103:24–32
Kesling CK (1992) The Tip-Edge concept: eliminating unnecessary anchorage strain. J Clin Orthod 26:165–178
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–e34
Mavragani M, Vergari A, Selliseth NJ, Bøe OE, Wisth PL (2000) A radiographic comparison of apical root resorption after orthodontic treatment with a standard edgewise and a straight-wire edgewise technique. Eur J Orthod 22:665–674
Mclaughlin R, Bennett J, Trevisi H (1997) A clinical review of the MBT orthodontic treatment program. Orthod Perspect 4:14
Merrifield L (1982) The systems of directional force. J Charles H. Tweed Int Found 10:15e29
Mittal M, Thiruvenkatachari B, Sandler PJ, Benson PE (2015) A three-dimensional comparison of torque achieved with a preadjusted edgewise appliance using a Roth or MBT prescription. Angle Orthod 85:292–297
Moesi B, Dyer F, Benson PE (2013) Roth versus MBT: does bracket prescription have an effect on the subjective outcome of pre-adjusted edgewise treatment? Eur J Orthod 35:236–243
Norman GR, Sloan JA, Wyrwich KW (2003) Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 41:582–592
O’Neill J (2003) Straight-wire versus tip-edge: a randomized controlled trial. In: 32nd meeting of the annual angle society of Europe, 2003, Going
Papageorgiou SN (2014) Meta-analysis for orthodontists: part I—how to choose effect measure and statistical model. J Orthod 41:317–326
Papageorgiou SN (2014) Meta-analysis for orthodontists: part II—is all that glitters gold? J Orthod 41:327–336
Papageorgiou SN, Gölz L, Jäger A, Eliades T, Bourauel C (2016) Lingual vs. labial fixed orthodontic appliances: systematic review and meta-analysis of treatment effects. Eur J Oral Sci 124:105–118
Papageorgiou SN, Konstantinidis I, Papadopoulou K, Jager A, Bourauel C (2014) Clinical effects of pre-adjusted edgewise orthodontic brackets: a systematic review and meta-analysis. Eur J Orthod 36:350–363
Papageorgiou SN, Konstantinidis I, Papadopoulou K, Jäger A, Bourauel C (2014) A systematic review and meta-analysis of experimental clinical evidence on initial aligning archwires and archwire sequences. Orthod Craniofac Res 17:197–215
Papageorgiou SN, Papadopoulos MA, Athanasiou AE (2014) Reporting characteristics of meta-analyses in orthodontics: methodological assessment and statistical recommendations. Eur J Orthod 36:74–85
Papageorgiou SN, Xavier GM, Cobourne MT (2015) Basic study design influences the results of orthodontic clinical investigations. J Clin Epidemiol 68:1512–1522
Reukers EA, Sanderink GC, Kuijpers-Jagtman AM, van’t Hof MA (1989) Radiographic evaluation of apical root resorption with 2 different types of edgewise appliances. Results of a randomized clinical trial. J Orofac Orthop 59:100–109
Reukers HAJ (1997) Straight wire appliance versus conventional full edgewise: a prospective clinical trial. Radboud University, Doctoral thesis
Ricketts RM, Bench RW, Hilgers JJ (1972) Mandibular utility arch. The basic arch in the light progressive technique. Proc Found Orthod Res 120–5
Root TL (1981) The level anchorage system for correction of orthodontic malocclusions. Am J Orthod 80:395–410
Roth RH (1982) The straight wire appliance 17 years later. J Clin Orthod 21:632–642
Schulz KF, Altman DG, Moher D, CONSORT Group (2010) CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 63:834–840
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P GROUP (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 349:g7647
Sharma V, Sengupta J (2009) Modifications to increase efficiency of the Begg orthodontic technique. Med J Armed Forces India 2:118–122
Soltani M, Saedi B, Mohammadi Z (2012) Outcome of MBT and standard edgewise techniques in treating Cl I malocclusion. Avicenna J Dent Res 4(2):61–65
Talapaneni AK, Supraja G, Prasad M, Kommi PB (2012) Comparison of sagittal and vertical dental changes during first phase of orthodontic treatment with MBT vs ROTH prescription. Indian J Dent Res 23:182–186
Tweed CH (1945) A philosophy of orthodontic treatment. Am J Orthod 31:74–103
Ugur T, Yukay F (1997) Normal faciolingual inclinations of tooth crowns compared with treatment groups of standard and pretorqued brackets. Am J Orthod Dentofac Orthop 112:50–57
Viazis AD (1995) Orthodontic seminar syllabus. University of South California
Wu L, Zhang M, Shao P (2007) Comparative study of anchorage loss between straight wire appliance and standard edgewise appliance. Stomatology 27(8):396–398
Acknowledgements
The authors would like to thank J. O’Neil (Kettering General Hospital, UK) for providing unpublished data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S Mousoulea, S.N. Papageorgiou, and T. Eliades state that they have no competing interests.
Additional information
Prof. Theodore Eliades.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mousoulea, S., Papageorgiou, S.N. & Eliades, T. Treatment effects of various prescriptions and techniques for fixed orthodontic appliances. J Orofac Orthop 78, 403–414 (2017). https://doi.org/10.1007/s00056-017-0094-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00056-017-0094-0