Abstract
Objectives
The purpose of this work was to evaluate the influence of insertion depth on the stability of orthodontic mini-implants. Sensitivity of three different methods to measure implant stability based on differences in insertion depth were determined.
Methods
A total of 82 mini-implants (2 × 9 mm) were inserted into pelvic bone of Swabian Hall pigs. Each implant was inserted stepwise to depths of 4, 5, 6, 7, and 8 mm. At each of these depths, three different methods were used to measure implant stability, including maximum insertion torque (MIT), resonance frequency analysis (RFA), and Periotest®. Differences between the recorded values were statistically analyzed and the methods tested for correlations.
Results
Almost linear changes from each insertion depth were measured with the values of RFA [implant stability quotient (ISQ) values range from 1–100], which increased from 6.95 ± 2.85 ISQ at 4 mm to 34.63 ± 5.51 ISQ at 8 mm, and with those of Periotest® [periotest values (PTV) range from −8 to 50], which decreased from 13.24 ± 4.03 PTV to −2.89 ± 1.87 PTV. Both methods were found to record highly significant (p < 0.0001) changes for each additional millimeter of insertion depth. The MIT increased significantly (p < 0.0001) from 153.67 ± 69.32 Nmm to 261 ± 103.73 Nmm between 4 and 5 mm of insertion depth but no further significant changes were observed as the implants were driven deeper. The RFA and Periotest® values were highly correlated (r = −0.907).
Conclusions
Mini-implant stability varies significantly with insertion depth. The RFA and the Periotest® yielded a linear relationship between stability and insertion depth. MIT does not appear to be an adequate method to determine implant stability based on insertion depth.
Zusammenfassung
Zielsetzung
Ziel der Arbeit war es, den Einfluss der Insertionstiefe auf die Stabilität orthodontischer Mini-Implantate zu untersuchen und die Sensitivität verschiedener Stabilitätsmessmethoden in Hinblick auf den Parameter Insertionstiefe zu ermitteln.
Methoden
Insgesamt 82 Mini-Implantate (2 × 9 mm) wurden in den Beckenknochen vom Landschwein inseriert. Bei Insertionstiefen (ID) von 4, 5, 6, 7 und 8 mm wurden jeweils das maximale Eindrehmoment (MIT) gemessen sowie der Periotest® und die Resonanzfrequenzanalyse (RFA) durchgeführt. Die Ergebnisse für die verschiedenen ID wurden statistisch auf signifikante Unterschiede untersucht und die Messmethoden hinsichtlich ihrer Korrelation zueinander überprüft.
Ergebnisse
Die Werte für RFA stiegen mit zunehmender ID nahezu linear an [6,95 ± 2,85 ISQ (“implant stability quotient”) bei ID 4 mm auf 34,63 ± 5,51 ISQ bei ID 8 mm) und fielen für den Periotest® fast linear ab [13,24 ± 4,03 PTV (“periotest values”) auf −2,89 ± 1,87 PTV]. Die Änderungen waren für RFA und Periotest® bei jedem Millimeterschritt der Insertion hoch signifikant (p < 0,0001). Die MIT-Werte stiegen von 4 auf 5 mm ID an (153,67 ± 69,32 auf 261 ± 103,73 Nmm, p < 0,0001) und änderten sich von da an nicht mehr signifikant. RFA und Periotest® zeigten eine hohe Korrelation (r = −0,907).
Schlussfolgerung
Die ID hat einen signifikanten Einfluss auf die Stabilität der Mini-Implantate; der Zusammenhang scheint linearer Natur zu sein. Im Gegensatz zum MIT sind die RFA und der Periotest® dazu geeignet, die Stabilität in Bezug auf den Parameter der Insertionstiefe zu ermitteln.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High primary stability is a basic requirement for the successful use of both dental and orthodontic implants. It appears plausible that implant stability should increase with insertion depth, given the larger bone-to-implant contact area. Orthodontic implants are usually loaded by a constant lateral force. Smaller insertion depths will create a longer lever arm that will increase the tipping moment. In conjunction with the smaller bone-to-implant contact area, this results in higher compressive stresses that may be detrimental to long-term stability [5]. Although these biomechanical considerations do suggest that insertion depth should significantly influence implant stability, no exact information is currently available—and particularly not for mini-implants—about how stability and depth are interrelated.
Different methods of measuring the stability of implants are available in dentistry. The most widely reported approach has been to measure the maximum insertion torque (MIT) during insertion [9, 23, 24]. Tools to this end have included dedicated surgical motors in clinical practice [8] and more precise torque sensors in laboratory experiments [25]. Another principle of measuring stability, represented by the Periotest® device [12], is to capture the damping characteristics of an implant. This is accomplished by percussing the implant head with a small pestle that will rebound at a specific speed depending on implant stability. During contact, a piezoelectric crystal inside the head of the pestle is deformed, thus, creating an electric impulse that reveals the duration of contact. This time-based information is converted to stability expressed as Periotest values (PTV), which range from −8 to +50. This method, first developed to measure tooth mobility, was introduced to implant dentistry by Brägger et al. [1]. A third method widely used is resonance frequency analysis (RFA) [13]. In this case, a SmartPeg with a permanent magnet is tightened into the implant. A handpiece emits electromagnetic impulses of 5–15 kHz against the peg to record the resonance frequencies, which are converted to stability expressed as “implant stability quotient” (ISQ) values ranging from 0–100.
These three methods to measure implant stability were used in the present study to investigate (1) what difference the variable of insertion depth makes, independently of bone quality, to the stability of orthodontic mini-implants and (2) how sensitively the various measuring methods would respond to differences in insertion depth.
Materials and methods
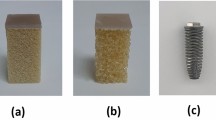
In the present study, experiments were performed using pelvic bone of five Swabian Hall pigs. A hand saw was used to obtain a bone block of 30 × 60 mm from each animal. This bone features a density similar to human jawbone and a cortical thickness varying between approximately 0.5 and 2.5 mm, which is appropriate for simulation of a human maxilla and mandible [14]. All measurements described below were performed immediately after creating the bone blocks on the day of slaughter. There was no storage in medium and no embedding of specimens. After drawing a 5-mm grid for the insertion sites on the bone surface, a drill press was used for pilot drillings 1.5 mm in diameter and 4 mm in depth.
Experiments were performed to test the stability of 82 almost cylindrical mini-implants 2 mm in diameter and 9 mm in length, featuring a thread pitch of 0.75 mm, a taper of 0.1 mm over the 9 mm length of the threaded implant segment, and a core diameter of 1.35 mm (Benefit; PSM Medical Solutions, Tuttlingen, Germany). Implant stability was repeatedly measured at different insertion depths by using various spacer sleeves (5, 4, 3, 2, 1 mm) to define the distance of the implant shoulder to the bone surface. Using a manual driver, we first inserted each implant to 5 mm from the bone. Then the insertion torque was recorded with a sensor (8625-5001; Burster Präzisionsmesstechnik, Gernsbach, Germany) attached to the specimen holder (Fig. 1a). A precision robot (RX60; StäubliTec-Systems, Bayreuth, Germany) inserted the mini-implant by another full turn (360°), equaling an insertion depth of 0.75 mm as defined by the thread pitch (Fig. 1b). Vertical insertion movements were executed by the robot as required. The insertion torques were captured with RMS (Robotic Measurement System) software.
a Specimen of pelvic bone from a Swabian Hall pig following insertion of mini-implants. b A precision robot was used to insert the mini-implants and to record the maximum insertion torque on reaching each of the five defined insertion depths
Abb. 1 a Beckenknochenprobe eines Schwäbisch-Hällischen Landschweins mit Mini-Implantaten. b Einbringen der Implantate und Registrierung des maximalen Eindrehmoments bei Erreichen der jeweiligen Insertionstiefe erfolgten durch einen Präzisionsroboter
Resonance frequency analysis was then tested, using an ISQ device by Ostell (Gothenburg, Sweden) and type 1 SmartPegs that had been optimized, in collaboration with Ostell, for a perfect fit with the internal thread of the mini-implant. Using a torque ratchet, the SmartPegs were tightened to 4–6 Ncm into the mini-implants. This modified technique of resonance frequency analysis has been used, and its accuracy and reproducibility investigated in previous studies [14–17]. Three longitudinal and three transverse stability measurements were performed relative to the bone fibers, followed by calculating the longitudinal, transverse, and total mean values. The Periotest® device (Medzintechnik Gulden e. K., Modautal, Germany) was applied last, again three times in both orientations followed by calculation of mean values. After advancing the mini-implant to the next insertion depth, using the next spacer sleeve in the series, the three measurement procedures were repeated. Given a threaded implant segment of 9 mm in length, stability values were obtained at a total of five insertion depths (4, 5, 6, 7, and 8 mm).
Statistical analysis
First, the mean values and standard deviations were calculated for all results of resonance frequency analysis, Periotest, and maximum insertion torque. For resonance frequency analysis and Periotest, total values were determined per screw per insertion depth from the values measured longitudinally and transversely to the superficial bone fibers. In addition, 95 % confidence intervals were calculated for each insertion depth. Appropriate statistical tests were selected after an initial Shapiro–Wilk test to check for the presence of a normal distribution. Wilcoxon’s test was applied to evaluate the different values measured longitudinally and transversely to the superficial bone fibers by resonance frequency analysis and the Periotest. Friedman’s test followed by Wilcoxon’s test were used to compare mini-implant stability as recorded by resonance frequency analysis and the Periotest at each insertion depth. Analysis of variance (ANOVA) was applied with Duncan post hoc tests to the values of maximum insertion torque. Finally, the three methods of implant stability measurement were compared to each other using a Pearson correlation test and regression analysis. All statistical calculations were performed with statistical software (SPSS®, v. 22; IBM, Armonk, NY, USA).
Results
No significant differences were seen between the resonance frequency data (expressed in ISQ) measured longitudinally or transversely to the superficial bone fibers. The increase in the ISQ values from 6.95 ± 2.85 at 4 mm to 34.63 ± 5.51 at 8 mm of insertion depth is shown in Fig. 2a. The values changed significantly with each additional millimeter of insertion, without overlapping of the 95 % confidence intervals (Tables 1, 2). In Fig. 3b, the Periotest results (expressed in PTV) decreased from 13.24 ± 4.03 to −2.89 ± 1.87, again indicating progressive increases of implant stability with insertion depth (Fig. 2b). Like the values of resonance frequency analysis, the Periotest values changed significantly with each additional millimeter of insertion and involved no overlapping of the 95 % confidence intervals (Tables 1, 2). The changes indicated by the two methods were fairly constant from each insertion depth to the next.
Mean values and standard deviations plotted against insertion depth. Each graph illustrates the values recorded with one of the three methods of implant stability measurement, including a resonance frequency analysis (RFA), b the Periotest, and c maximum insertion torque (MIT). Asterisks indicate significant changes (p < 0.0001) from one insertion depth to the next, n.s. nonsignificant changes (p > 0.05)
Abb. 2 Plot der Durchschnittswerte und Standardabweichung gegen die Insertionstiefe. Jeder Graph stellt die Werte dar, die mit einer der 3 Methoden zur Messung der Implantatstabilität generiert wurden, einschließlich a Resonanzfrequenzanalyse (RFA), b Periotest und c maximalem Eindrehmoment (MIT). Signifikante Änderungen (p < 0,0001) von einer Insertionsstufe zur nächsten sind mit Sternchen (*), nichtsignifikante (p > 0,05) mit n.s. gekennzeichnet
Correlations between methods. Each graph illustrates a pattern between two methods of implant stability measurement, including the correlation of a maximum insertion torque (MIT) with resonance frequency analysis (RFA); b MIT with the Periotest; and c RFA with the Periotest, the latter including a regression line
Abb. 3 Korrelation zwischen den Methoden. Jeder Graph illustriert ein Pattern zwischen 2 Stabilitätsmessmethoden, einschließlich der Korrelation des a maximalen Eindrehmoments (MIT; Resonanzfrequenzanalyse, RFA); b MIT mit Periotest; c RFA mit Periotest, letzter mit einer Regressionsgeraden
A different pattern of values was obtained for maximum insertion torque. Insertion to the initial depth of 4 mm yielded a mean value of 153.67 ± 69.32 Nmm (Table 1; Fig. 2c), which increased by a 108.13 Nmm to 261 ± 103.73 Nmm (significant; Table 2) as the implants were driven deeper to 5 mm. Past that point, however, no significant changes with the insertion torque values were observed. Following a slight increase from 5 to 6 mm, they decreased, during the last two insertion steps, to 248.78 ± 95.88 Nmm at 8 mm. The Pearson correlation test confirmed these patterns. As listed in Table 3 and shown in Fig. 3a, b, the values for maximum insertion torque did not correlate closely with those of the resonance frequency analysis (r = 0.301) or Periotest (r = −0.283). As shown in Fig. 3c, however, a strong negative correlation did emerge between resonance frequency analysis and the Periotest (r = −0.907; p < 0.0001). The equation applied for the regression line in this context yielded “y = −0.55 · x + 15.34”.
Discussion
The 95 % confidence intervals, which did not overlap for two of the three methods, indicate that the number of mini-implants was adequate for representative results. The bone model used in this study was previously proven useful in simulating human jawbone of all cortical thicknesses [14]. We created the bone blocks immediately after the animals had been slaughtered, avoiding any storage or embedding to ensure that the mechanical properties remained unchanged. The use of a precision robot enabled us to determine the maximum implant torques based on highly reproducible tightening of the implants during insertion. Our in vitro setup allowed the Periotest probe to be precisely angulated as per the manufacturer’s recommendations. The protocol used for resonance frequency analysis was also evaluated previously for coupling stability, reproducibility, and plausibility of results [14]. The statistical tests employed were selected after an initial Shapiro–Wilk test for normal distribution in small samples.
Both with resonance frequency analysis and with the Periotest method, linear associations were observed between insertion depth and stability. In addition, a close correlation was apparent between these two methods (r = −0.901). One reason for this latter finding might have been the perpendicular orientation of measurements relative to the implant axis. Given the lateral loading of orthodontic implants, their clinical success will greatly depend on the leverage involved, i.e., on the distance between the point of force application and the center of resistance [5]. Hence, it appears plausible that stability, as a function of resistance to lateral forces, should strongly depend on insertion depth. Close correlation between resonance frequency analysis and the Periotest in measuring the stability of dental and orthodontic implants have been previously reported [10, 14]. Moreover, resonance frequency analysis is currently regarded as the gold standard for clinical assessment of implant stability [11]. Periotest values were also found to be highly prognostic for implant loss [18].
Several studies have confirmed the importance of the bone-to-implant contact area [3, 4, 6, 21, 22]. Of particular important, however, is the contact with cortical bone [2]. Insertion depths being equal, the results of resonance frequency analysis were found to correlate with cortical bone thickness [14]. The aim in our study was to evaluate how implant stability differs as a specific function of insertion depth across the whole range of cortical bone thicknesses. The mini-implants were distributed for this purpose across the bone specimens—with cortical thickness ranging from 0.45 to 2.65 mm [14] —which also accounts for the expectedly high standard deviations of the values measured. The results are informative because the implants were advanced deeper in a stepwise manner, so that stability values at different insertion depths could be obtained for each single implant, thus, enabling the use of statistical tests for paired samples. Thus, our results reliably demonstrate that the associations shown are true for almost all bone configurations encountered in human maxillae and mandibles.
Laboratory and clinical studies have shown that—insertion depths being equal—implants of greater total length will not yield better resonance frequency results or resistance to lateral forces [17, 20]. In addition, Chatzigianni et al. [7] did not find a correlation between total length and displacement of implants on applying a lateral force in the clinically relevant range. Pan et al. [19] did hypothesize that resistance to lateral forces would depend on the ratio of insertion depth to total implant length. Our data and those in the literature suggest that resistance to lateral forces is significantly determined by the ratio of extrabony implant length to cortical bone thickness. As the main clinical implication, care should be taken to select insertion sites which, in addition to the requirement of offering high bone quality, are characterized by a thin mucosal layer to minimize the length of the biomechanically relevant extrabony implant segment.
Unlike resonance frequency analysis and the Periotest, in which steady increases in implant stability were observed to the final insertion depth of 8 mm, the maximum insertion torques did not reveal significant changes past an insertion depth of 5 mm. They even decreased slightly during the last two insertion steps (6–7 mm and 7–8 mm). Other authors [26], by contrast, reported continuous increases in maximum insertion torque during insertion. Resistance to insertion torque is due to external friction between the contact surfaces of two solid objects (i.e., bone and implant). This frictional force (F R), as predicted by Amonton’s law, increases almost linearly with the normal force (F N) but is independent of the contact surface (F R ≤ µ · F N, where µ is the friction coefficient associated with the surface characteristics of the solid objects). This means that the frictional force and with it the insertion torque will not increase further along with the contact surface area as the implant is driven deeper. The slight decrease in maximum insertion torque of the last few millimeters of insertion may be attributed to a decrease in normal force. In other words, following self-drilling of the implant screw into the first few millimeters of cortical bone, its almost cylindrical shape will cause slight widening of the cortical bone at deeper levels. As a result, the pressure of bone against the implant will slightly decrease, and so will the normal force. Against this background, it becomes easy to understand why the method of maximum insertion torque should be less sensitive to insertion depth. Therefore, in clinical practice the methods of resonance frequency analysis and the Periotest appear better suited for stability measurement of orthodontic mini-implants.
Conclusions
Mini-implant stability varies significantly with insertion depth. Using the present experimental setup, a linear association between implant stability and insertion depth was observed. Since all screws in the study were identical in length, there was a direct inverse relationship between insertion depth and extrabony implant length. Thus, it may be concluded that extrabony implant length is a codeterminant of implant stability in addition to cortical bone thickness. It follows that, in clinical practice, attention should be paid to selecting insertion sites characterized by mucosa that is as thin as possible. Resonance frequency analysis and the Periotest use lateral loading consistent with the biomechanics of clinical application. The fact that their values reflect the effective tipping moments explains their high sensitivity relative to insertion depth/extrabony length.
References
Brägger U, Hugel-Pisoni C, Burgin W et al (1996) Correlations between radiographic, clinical and mobility parameters after loading of oral implants with fixed partial dentures. A 2-year longitudinal study. Clin Oral Implants Res 7(3):230–239
Buchter A, Kleinheinz J, Wiesmann HP et al (2004) Peri-implant bone formation around cylindrical and conical implant systems. Mund Kiefer Gesichtschir 8(5):282–288
Buchter A, Kleinheinz J, Wiesmann HP et al (2005) Interface reaction at dental implants inserted in condensed bone. Clin Oral Implants Res 16(5):509–517
Buchter A, Kleinheinz J, Wiesmann HP et al (2005) Biological and biomechanical evaluation of bone remodelling and implant stability after using an osteotome technique. Clin Oral Implants Res 16(1):1–8
Buchter A, Wiechmann D, Koerdt S et al (2005) Load-related implant reaction of mini-implants used for orthodontic anchorage. Clin Oral Implants Res 16(4):473–479
Buchter A, Wiechmann D, Gaertner C et al (2006) Load-related bone modelling at the interface of orthodontic micro-implants. Clin Oral Implants Res 17(6):714–722
Chatzigianni A, Keilig L, Reimann S et al (2011) Effect of mini-implant length and diameter on primary stability under loading with two force levels. Eur J Orthod 33(4):381–387
Grandi T, Guazzi P, Samarani R et al (2013) Clinical outcome and bone healing of implants placed with high insertion torque: 12-month results from a multicenter controlled cohort study. Int J Oral Maxillofac Surg 42(4):516–520
Javed F, Almas K, Crespi R et al (2011) Implant surface morphology and primary stability: is there a connection? Implant Dent 20(1):40–46
Lachmann S, Jager B, Axmann D et al (2006) Resonance frequency analysis and damping capacity assessment. Part I: an in vitro study on measurement reliability and a method of comparison in the determination of primary dental implant stability. Clin Oral Implants Res 17(1):75–79
Lachmann S, Laval JY, Jager B et al (2006) Resonance frequency analysis and damping capacity assessment. Part 2: peri-implant bone loss follow-up. An in vitro study with the Periotest and Osstell instruments. Clin Oral Implants Res 17(1):80–84
Lukas D, Schulte W (1990) Periotest–a dynamic procedure for the diagnosis of the human periodontium. Clin Phys Physiol Meas 11(1):65–75
Meredith N, Alleyne D, Cawley P (1996) Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin Oral Implants Res 7(3):261–267
Nienkemper M, Wilmes B, Panayotidis A et al (2012) Measurement of mini-implant stability using resonance frequency analysis. Angle Orthod 83(2):230–238
Nienkemper M, Pauls A, Ludwig B et al (2013) Stability of paramedian inserted palatal mini-implants at the initial healing period: a controlled clinical study. Clin Oral Implants Res. 26(8):870–875
Nienkemper M, Wilmes B, Pauls A et al (2013) Mini-implant stability at the initial healing period. Angle Orthod. Epub ahead of print
Nienkemper M, Wilmes B, Pauls A et al (2013) Impact of mini-implant length on stability at the initial healing period: a controlled clinical study. Head Face Med 20(9):30
Noguerol B, Munoz R, Mesa F et al (2006) Early implant failure. Prognostic capacity of Periotest: retrospective study of a large sample. Clin Oral Implants Res 17(4):459–464
Pan CY, Chou ST, Tseng YC et al (2012) Influence of different implant materials on the primary stability of orthodontic mini-implants. Kaohsiung J Med Sci 28(12):673–678
Pithon MM, Figueiredo DS, Oliveira DD (2013) Mechanical evaluation of orthodontic mini-implants of different lengths. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg 71(3):479–486
Schwarz F, Sager M, Kadelka I et al (2010) Influence of titanium implant surface characteristics on bone regeneration in dehiscence-type defects: an experimental study in dogs. J Clin Periodontol 37(5):466–473
Schwarz F, Sahm N, Iglhaut G et al (2011) Impact of the method of surface debridement and decontamination on the clinical outcome following combined surgical therapy of peri-implantitis: a randomized controlled clinical study. J Clin Periodontol 38(3):276–284
Su YY (2009) Primary stability of orthodontic mini-implants: analysis of biomechanical properties and clinical relevance. Doctoral thesis, Department of Orthodotnics Heinrich-Heine-Universität, Düsseldorf
Wilmes B, Rademacher C, Olthoff G et al (2006) Parameters affecting primary stability of orthodontic mini-implants. J Orofac Orthop 67(3):162–174
Wilmes B, Su YY, Drescher D (2008) Insertion angle impact on primary stability of orthodontic mini-implants. Angle Orthod 78(6):1065–1070
Wilmes B, Drescher D (2009) Impact of insertion depth and predrilling diameter on primary stability of orthodontic mini-implants. Angle Orthod 79(4):609–614
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Nienkemper, N. Santel, R. Hönscheid, and D. Drescher state that there are no conflicts of interest.
The accompanying manuscript does not include studies on humans or living animals.
Additional information
PD Dr. Manuel Nienkemper.
Rights and permissions
About this article
Cite this article
Nienkemper, M., Santel, N., Hönscheid, R. et al. Orthodontic mini-implant stability at different insertion depths. J Orofac Orthop 77, 296–303 (2016). https://doi.org/10.1007/s00056-016-0036-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00056-016-0036-2