Abstract
Background
Colorectal cancer is associated with considerable impairment of quality of life as well as disease-specific symptoms and functional limitations. These can be assessed using standardized patient-reported outcome (PRO) instruments such as the EORTC QLQ-C30 and CR29 questionnaires. To date, no systematic investigation exists regarding which of the total 35 symptoms and functional limitations captured by the EORTC questionnaires are relevant to clinicians. This study aimed to identify the dimensions of the EORTC questionnaires most relevant to clinicians in the pretherapeutic assessment of colorectal cancer patients.
Methods
An online survey was conducted (February–March 2021) in which clinicians from certified colorectal cancer centers were asked to rate the five most relevant scales (for colon and rectal cancer, respectively). The contacted cancer centers all participated in the EDIUM study, in which the PRO instruments were already used. The survey results were analyzed descriptively.
Result
Of 203 respondents, 96 took part in the survey (83 surgeons, 9 internists, 4 not specified/others). For colon, the scales “quality of life” (n = 80), “pain” (40), “physical function” (36), “constipation” (33), and “abdominal pain” (31) were most frequently reported; for rectum, these were the scales “quality of life” (74), “fecal incontinence” (62), “pain” (27), “physical function” (25), and “constipation” (25).
Conclusion
The results show that in the pretherapeutic assessment of colorectal patients, the clinicians’ interest mainly focuses on the self-reported quality of life. However, in addition, colorectal cancer-specific symptoms are perceived as important, such as fecal incontinence (for rectum). The results can be used to select specific scales of PROs that are relevant in practice and for further development of these instruments.
Zusammenfassung
Hintergrund
Darmkrebs ist mit einer erheblichen Beeinträchtigung der Lebensqualität sowie mit krankheitsspezifischen Symptomen und Funktionseinschränkungen verbunden. Diese lassen sich gut mit standardisierten patient-reported-outcomes(PRO)-Instrumenten, wie den EORTC QLQ-C30- und -CR29-Fragebogen, erfassen. Bislang wurde nicht systematisch untersucht, welche der insgesamt 35 Symptome und Funktionseinschränkungen, die mit den EORTC-Fragebogen erfasst werden, für Kliniker*innen relevant sind. Ziel dieser Studie war es zu untersuchen, welche der in den EORTC-Fragebogen erfassten Dimensionen für Kliniker*innen bei der prätherapeutischen Beurteilung der Darmkrebspatienten am relevantesten sind.
Methoden
Eine Onlineumfrage wurde durchgeführt (Februar/März 2021), bei der Kliniker aus zertifizierten Darmkrebszentren gebeten wurden, die fünf relevantesten Skalen (für das Kolon- bzw. Rektumkarzinom) anzugeben. Alle kontaktierten Darmkrebszentren nahmen an der EDIUM-Studie teil, in der die PRO-Instrumente bereits verwendet wurden. Die Umfrageergebnisse wurden deskriptiv ausgewertet.
Ergebnis
96 von 203 Befragten nahmen an der Umfrage teil (83 Chirurg*innen, 9 Internist*innen, 4 nicht angegeben/sonstige). Für Kolon wurden die Skalen „Lebensqualität“ (n = 80), „Schmerzen“ (40), „Verstopfung“ (33) und „Bauchschmerzen“ (31) am häufigsten genannt; für Rektum die Skalen „Lebensqualität“ (74), „Stuhlinkontinenz“ (62), „Schmerzen“ (27), „körperliche Funktion“ (25) und „Verstopfung“ (25).
Schlussfolgerung
Die Ergebnisse zeigen, dass sich das Interesse der Kliniker*innen bei der prätherapeutischen Beurteilung von Darmkrebspatient*innen v. a. auf die selbstberichtete Lebensqualität konzentriert. Darüber hinaus werden auch krankheitsspezifische Symptome als wichtig empfunden, wie z. B. Stuhlinkontinenz (für Rektum). Die Ergebnisse können für die Auswahl spezifischer Skalen von PROs, die für die klinische Praxis relevant sind, und für die Weiterentwicklung dieser Instrumente genutzt werden.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Colon cancer is the third most common cancer worldwide [2]. Diagnosis and subsequent treatment decisions are usually dependent on “hard” clinical factors such as tumor stage or comorbidities of the patient [3]. There is an increasing demand to include self-reported symptoms and functional limitations not only as an outcome after treatment, but also before and during therapy [10]. The tools of choice to measure such symptoms and functional limitations are patient-reported outcomes (PRO). These are standardized questionnaires that patients answer themselves and thus provide information about patients’ own assessment of their health status and the symptoms and functional limitations they encounter. In oncology, the European Organisation for Research and Treatment of Cancer Core Quality of Life Questionnaire (EORTC QLQ-C30) is widely used [1], which can be combined with a disease-specific module; for colorectal cancer, this is EORTC QLQ-CR29 [12]. Pioneering work by Bash et al. was able to show that early inclusion of PROs into treatment planning and monitoring leads to a statistically significant increase in life expectancy [4]. Nevertheless, patient-reported outcomes are still very rarely used in colorectal oncologic care [9]. This seems to partly be due to the fact that the questionnaires are very long and thus perceived as impractical for clinical routine (taking the generic module together with the colorectal cancer-specific form, a total of 35 different symptoms and functional scores are captured by the EORTC QLQ questionnaires) [5]. Therefore, it seems to be of high clinical relevance to select those scores that are particularly important from the point of view of the treating clinicians in the pretherapeutic assessment of colorectal cancer patients.
Materials and methods
The CHERRIES framework for reporting online surveys was used for this study [7].
Design, participants, and recruitment process
Coordinators and directors of certified colorectal cancer centers which participated in a PRO study using the EOTRC QLQ-C30 and CR29 questionnaires (EDIUM centersFootnote 1) were asked to participate in a closed online survey. The survey was hosted on the platform sosci-survey.de between February and March 2021.
All participants gave their informed consent based on information regarding the time required for the survey (approximately 5 min), contact information to study group, and the pseudonymization process before accessing the online survey.
Directors and coordinators of all EDIUM centers were contacted via mail with information about the survey and study purposes. If they were willing to participate, they could access a personalized link. All eligible directors and coordinators were reminded biweekly three times. There were no additional incentives. The study group set up an internal trust office led by SS for contacting and reminding the eligible directors and coordinators. SS did not take part in any data analysis for pseudonymization purposes.
The survey was part of the evaluation process of the EDIUM study and as such has an ethical approval by the Ethics Committees of the Berlin Chamber of Physicians (Eth-19/18).
Questionnaire
The questionnaire was developed by NTS. A first pre-test was performed by CB and CK, both investigators of the EDIUM study group. The questionnaire was then pre-tested by two clinicians of the independent scientific board of the EDIUM study. Any ambiguities relating to the survey questions were revised afterwards and reworded by NTS, if necessary. The final questionnaire consisted of three main questions followed by two optional fields for any additional comments on the survey or the EDIUM study in general.
The first two questions were (translated) “Which of the following dimensions (disease-specific symptoms and function) of the EORTC questionnaires QLQ-C30 and CR29 are most relevant regarding clinical assessment, treatment preparation, and discussion before a definitive treatment (e.g., surgery) of COLON carcinoma?”Footnote 2 and “Which of the following dimensions (disease-specific symptoms and function) of the EORTC questionnaires QLQ-C30 and CR29 are most relevant regarding clinical assessment, treatment preparation, and discussion before a definitive treatment (e.g., surgery) of RECTAL carcinoma?”Footnote 3. Both main questions had 35 response options—the number of EORTC QLQ-C30 and CR29 dimensions—and the participants were asked to choose the five most relevant dimensions for them. Afterwards, the participants were to indicate which specialty (internal medicine, surgery, other) they work in.
The survey offered completeness checks and reminded the participants if any question was not yet answered. However, completeness was not compulsory for submitting the survey. After submitting, the respondents were not able to re-submit the questionnaire or change their responses.
Data analysis
Data were descriptively analyzed using R version 4.0.2 (2020.06.22; R Core Team (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/). A summarizing, qualitative analysis of the two “further comments” sections (text fields) was also performed.
Results
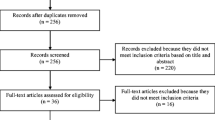
Participants and response rates
A total of 203 directors and coordinators of 103 EDIUM centers were asked to participate in the survey. After three biweekly reminders, 96 of the contacted persons submitted the questionnaire, resulting in a response rate of 45.8%. Most of the respondents were surgeons (83 in total, 86%). The frequencies of the different specialities can be found in Table 1.
On average, respondents needed 3.6 min (standard deviation 1.9 min) to answer the survey.
Relevant EORTC QLQ-C30 and CR29 items
Colon cancer
For colon carcinoma, the “quality of life” score was most often chosen to be one of the five most relevant scores (70 of 83 surgeons, 8 of 9 specialists for internal medicine). The other four most frequently chosen scores were: “pain” (36 surgeons, 2 specialists for internal medicine), “physical function” (30 surgeons, 5 specialists for internal medicine), “constipation” (30 surgeons, 1 specialist for internal medicine), and “abdominal pain” (27 surgeons, 4 specialists for internal medicine). The scores “dry mouth,” “dysuria,” “hair loss,” “trouble with taste,” and “urinary frequency” were not chosen by any participants. For the exact frequencies, compare Fig. 1 and the supplementary Appendix.
Rectal cancer
For rectal cancer, the “quality of life” score was most often chosen to be one of the five most relevant scores (65 of 83 surgeons, 7 of 9 specialists for internal medicine). The other four most frequently chosen scores were: “fecal incontinence” (54 surgeons, 6 specialists for internal medicine), “pain” (23 surgeons, 3 specialists for internal medicine), “constipation” (22 surgeons, 1 specialist for internal medicine), and “physical function” (20 surgeons, 4 specialists for internal medicine). The scores “dry mouth,” “hair loss,” “insomnia,” and “trouble with taste” were not chosen by any of the respondents. For the exact frequencies, compare Fig. 2 or the Appendix.
Additional remarks
The participants had the possibility to fill out a text field if they had any additional remarks. Two participants highlighted the importance of the patients’ perception of stomal therapy:
“How stressful do patients find a stoma depending on their age and life situation?” (Specialist for internal medicine)
Another participant doubted that any dimensions of EORTC QLQ-C30 and -CR29 should be regarded on their own, as the overall picture of the patient is most relevant:
“I find the selection problematic. We actually want to have an overall picture. Many of the individual factors listed must be evaluated by the patient and then discussed, whereas others require direct action.” (Surgeon)
Moreover, one participant named “sexual life” as an important additional piece of information about the patients, another “psychiatric comorbidities.”
Discussion
To the authors’ knowledge, this is the first summary and presentation of clinicians’ assessment of the relevance of the EORTC QLQ-C30 and -CR29 scores for treatment planning in colorectal cancer patients. First, it should be emphasized that a general summary score such as the quality of life score is most relevant for both rectal and colon cancer from the clinicians’ perspective. Differences in the localization of these tumors explain why fecal incontinence is mentioned in second place for rectal cancer (seventh place for colon cancer). Dyspareunia and impotence, which are frequently mentioned in rectal cancer, can also be explained by the location of the tumor. Symptoms occurring after cancer treatment (e.g., chemotherapy) were not reported at all or rarely (e.g., “trouble with taste” or “hair loss” in both entities).
Our results underline the importance of standardized recording of symptoms and functions in patients with colorectal cancer. However, based on our survey and other findings, it is recommended to make an appropriate selection of EORTC-QLQ scores in order to not overburden patients or clinicians with unnecessary information [8, 11]. The clinicians’ particularly strong focus on quality of life also underscores this information’s relevance for treatment planning.
Often, however, quality of life is not recorded in a standardized way, but may only be taken into account during the medical history taking. In the interests of equal treatment of all patients and quality assurance in oncologic care, it is advisable to query patients in a structured and thus binding manner before the start of a therapy rather than to rely on an unstructured anamnesis. If collected in a standardized way, information can only not be lost less easily, but it can also be used by the entire treatment team instead of by a single physician who talked to the patient. Here, too, it seems particularly relevant to restrict oneself to the clinically important scores, in order to promote acceptance among clinicians beforehand—even though one participant strengthened the importance of non-restriction as an additional remark.
Moreover, if patients are actively involved during treatment planning and treatment decision-making by contributing information about their disease burden themselves, and thus by being able to control what is particularly important to them for treatment, the communication between clinicians and patients is strengthened. This contributes to an improvement of colorectal cancer treatment [6].
These results may help to select relevant scores to be queried in one’s own care unit. Due to the low level of participating specialists in internal medicine, conclusions can be drawn from the current survey mainly for surgical departments. However, since colorectal cancer patients often first encounter surgeons, it seems reasonable to set a main focus on surgically important PROs. Since the EORTC-QLQ instruments were only introduced in many participating centers during the EDIUM study, it is possible that responders are comparably inexperienced in the use of PROs. Further research may investigate whether responses differ in samples with more PRO experience. Moreover, the authors strongly encourage further research in patient-relevant symptoms and functions, which might be others than those important to clinicians. Nevertheless, this is the first listing and survey of the most relevant symptoms and functions—which can be self-reported by the patient—for the treatment decision in colorectal cancer and, as such, should also be included in the clinical oncology daily routine.
Notes
EDIUM study: “Ergebnisqualität bei Darmkrebs: Identifikation von Unterschieden und Maßnahmen zur flächendeckenden Qualitätsentwicklung”; https://www.edium-studie.de.
Original German question: Welche der folgenden Dimensionen (krankheitsspezifische Symptome und Funktionen) aus den EORTC-Fragebogen QLQ-C30 und -CR29 finden Sie für die Behandlungsvorbereitung und -besprechung sowie zur klinischen Beurteilung vor Beginn einer definitiven Therapie (z. B. Operation) für das KOLONKARZINOM besonders relevant?
Original German question: Welche der folgenden Dimensionen (krankheitsspezifische Symptome und Funktionen) aus den EORTC-Fragebogen QLQ-C30 und -CR29 finden Sie für die Behandlungsvorbereitung und -besprechung sowie zur klinischen Beurteilung vor Beginn einer definitiven Therapie (z. B. Operation) für das REKTUMKARZINOM besonders relevant?
References
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376
Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Niksic M, Bonaventure A, Valkov M, Johnson CJ, Esteve J, Ogunbiyi OJ, Azevedo ESG, Chen WQ, Eser S, Engholm G, Stiller CA, Monnereau A, Woods RR, Visser O, Lim GH, Aitken J, Weir HK, Coleman MP (2018) Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 391(10125):1023–1075. https://doi.org/10.1016/s0140-6736(17)33326-3
Argilés G, Tabernero J, Labianca R, Hochhauser D, Salazar R, Iveson T, Laurent-Puig P, Quirke P, Yoshino T, Taieb J, Martinelli E, Arnold D (2020) Localised colon cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 31(10):1291–1305. https://doi.org/10.1016/j.annonc.2020.06.022
Basch E, Deal AM, Kris MG, Scher HI, Hudis CA, Sabbatini P, Rogak L, Bennett AV, Dueck AC, Atkinson TM, Chou JF, Dulko D, Sit L, Barz A, Novotny P, Fruscione M, Sloan JA, Schrag D (2015) Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol. https://doi.org/10.1200/jco.2015.63.0830
Breidenbach C, Kowalski C, Wesselmann S, Sibert NT (2021) Could existing infrastructure for using patient-reported outcomes as quality measures also be used for individual care in patients with colorectal cancer? BMC Health Serv Res 21(1):448. https://doi.org/10.1186/s12913-021-06457-6
Cranley NM, Curbow B, George TJ, Christie J (2017) Influential factors on treatment decision making among patients with colorectal cancer: a scoping review. Support Care Cancer 25(9):2943–2951. https://doi.org/10.1007/s00520-017-3763-z
Eysenbach G (2004) Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E‑Surveys (CHERRIES). J Med Internet Res 6(3):e34. https://doi.org/10.2196/jmir.6.3.e34
Foster A, Croot L, Brazier J, Harris J, O’Cathain A (2018) The facilitators and barriers to implementing patient reported outcome measures in organisations delivering health related services: a systematic review of reviews. J Patient Rep Outcomes 2(1):46
Rutherford C, Campbell R, White K, King M (2019) Patient-reported outcomes as predictors of survival in patients with bowel cancer: a systematic review. Qual Life Res 28(11):2871–2887. https://doi.org/10.1007/s11136-019-02255-0
Sibert NT, Kowalski C, Pfaff H, Wesselmann S, Breidenbach C (2021) Clinicians’ knowledge and attitudes towards patient reported outcomes in colorectal cancer care—insights from qualitative interviews. BMC Health Serv Res 21(1):366. https://doi.org/10.1186/s12913-021-06361-z
Stover AM, Haverman L, van Oers HA, Greenhalgh J, Potter CM, Ahmed S, Greenhalgh J, Gibbons E, Haverman L, Manalili K, Potter C, Roberts N, Santana M, Stover AM, van Oers H (2020) Using an implementation science approach to implement and evaluate patient-reported outcome measures (PROM) initiatives in routine care settings. Qual Life Res. https://doi.org/10.1007/s11136-020-02564-9
Whistance RN, Conroy T, Chie W, Costantini A, Sezer O, Koller M, Johnson CD, Pilkington SA, Arraras J, Ben-Josef E, Pullyblank AM, Fayers P, Blazeby JM (2009) Clinical and psychometric validation of the EORTC QLQ-CR29 questionnaire module to assess health-related quality of life in patients with colorectal cancer. Eur J Cancer 45(17):3017–3026. https://doi.org/10.1016/j.ejca.2009.08.014
Acknowledgements
We would like to thank all study participants for their time and effort. We are grateful to the Innovation Fund of the Federal Joint Committee (G-BA) for funding this research.
Funding
EDIUM was funded by the Innovation Fund of the Federal Joint Committee (Innovationsausschuss beim Gemeinsamen Bundesausschuss, G‑BA).
Author information
Authors and Affiliations
Contributions
NTS planned the online survey and analyzed and interpreted the data. The online questionnaire was developed with the aid of NTS, CB and CK. CK and SW lead the EDIUM study. CB, NTS and CK coordinate the EDIUM study. SS led the internal trust office for this online survey. NTS wrote the first draft of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
N.T. Sibert, C. Breidenbach, S. Wesselmann, C. Kowalski, and S. Schult are employees of the German Cancer Society, the institution in charge of the EDIUM study. T. Seufferlein is honorary president of the German Cancer Society. S.R. Benz, S. Post, and P. Schloss declare that they have no competing interests.
As part of the EDIUM study evaluation, this online survey was approved by the Ethics Committees of the Berlin Chamber of Physicians (Eth-19/18). Informed consent was given by the participants.
Additional information
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.

Scan QR code & read article online
Supplementary Information
Rights and permissions
About this article
Cite this article
Sibert, N.T., Breidenbach, C., Wesselmann, S. et al. Which EORTC QLQ-C30 and -CR29 scores are relevant for clinicians for therapy planning and decisions?. coloproctology 43, 411–416 (2021). https://doi.org/10.1007/s00053-021-00560-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00053-021-00560-2
Keywords
- Patient-reported outcome measures
- Colorectal neoplasms
- Quality of life
- Cancer care facilities
- Questionnaires